Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-218
Mitral Intentional Neo-Skirt Left Ventricular Outflow Tract Optimization via Antegrade Upscaling Balloon-Facilitated Leaflet Razing (MINOTAUR) for Valve-in-Valve Transcatheter Mitral Valve Replacement - A Case Series of a Novel Technique to Prevent LVOT Obstruction
By Christina Mew, Ganeev Malhotra, Christopher Cole, Arun Dahiya, Adrian Chong, Danielle Harrop, Samual Hayman, Yash Singbal, Jordan Ross, Stephen Cox, David Trappett, Gemma Duncan, Kellee Korver, Anthony Camuglia
Presenter
Christina Mew
Authors
Christina Mew1, Ganeev Malhotra1, Christopher Cole1, Arun Dahiya1, Adrian Chong1, Danielle Harrop1, Samual Hayman2, Yash Singbal1, Jordan Ross1, Stephen Cox1, David Trappett1, Gemma Duncan1, Kellee Korver1, Anthony Camuglia1
Affiliation
Princess Alexandra Hospital, Australia1, Royal Brisbane and Women's Hospital, Australia2,
View Study Report
TCTAP C-218
Structural - Mitral Valve Intervention - Transcatheter MV Replacement
Mitral Intentional Neo-Skirt Left Ventricular Outflow Tract Optimization via Antegrade Upscaling Balloon-Facilitated Leaflet Razing (MINOTAUR) for Valve-in-Valve Transcatheter Mitral Valve Replacement - A Case Series of a Novel Technique to Prevent LVOT Obstruction
Christina Mew1, Ganeev Malhotra1, Christopher Cole1, Arun Dahiya1, Adrian Chong1, Danielle Harrop1, Samual Hayman2, Yash Singbal1, Jordan Ross1, Stephen Cox1, David Trappett1, Gemma Duncan1, Kellee Korver1, Anthony Camuglia1
Princess Alexandra Hospital, Australia1, Royal Brisbane and Women's Hospital, Australia2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
We present MINOTAUR, a novel technique to mitigate neo-LVOT obstruction (LVOTO) risk in valve-in-valve (VIV) transcatheter mitral valve replacement (TMVR). Our transvenous transseptal approach combines prior methods, and involves precise leaflet penetration using an electrified wire, followed by sequential balloon dilatation and implantation of balloon expandable prostheses through the modified mitral intraleaflet tract to achieve maximal leaflet splaying.
Relevant Test Results Prior to Catheterization
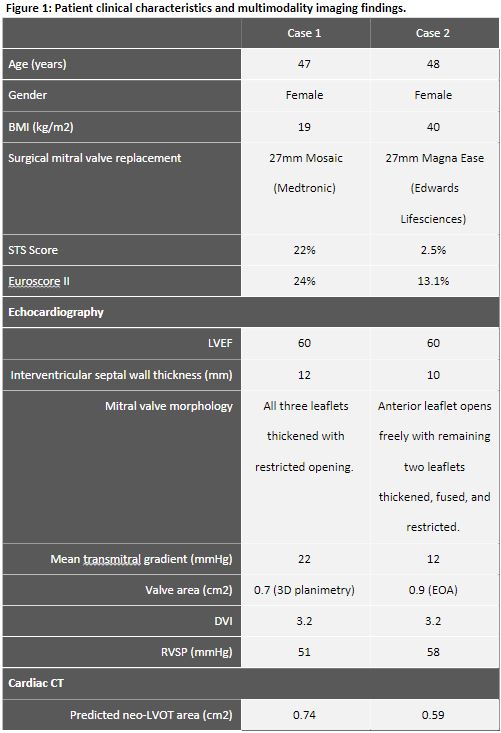
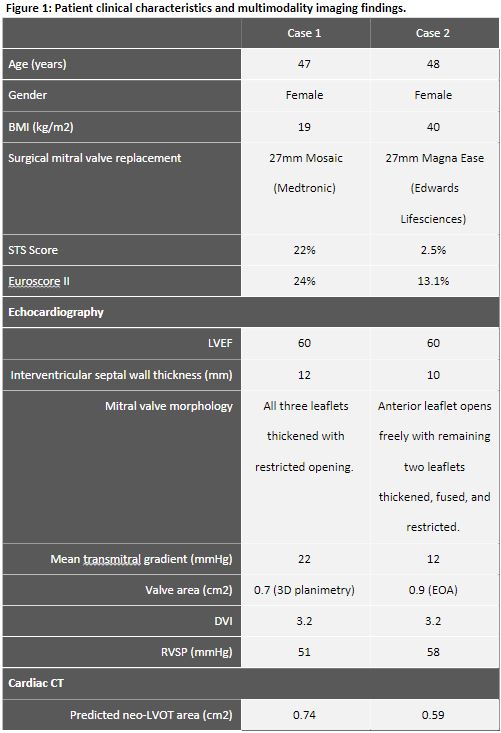
Patient 1 is a 47yo with NYHA class IV medically refractory pulmonary oedema with right heart failure and pulmonary hypertension due to stenotic degeneration of a 27mm Mosaic prosthesis. Patient 2 is a 48yo with NYHA class III heart failure and pulmonary hypertension due to stenotic degeneration of a 27mm Magna Ease prosthesis. Both had cardiac CT predicting extreme neo-LVOTO risk and deemed prohibitive risk for conventional redo surgeries by Heart Team consensus. See figure 1.
Relevant Catheterization Findings
Interventional Management
Procedural Step
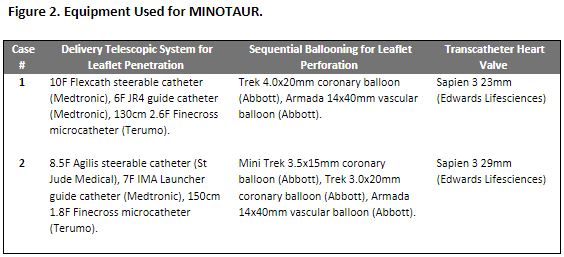
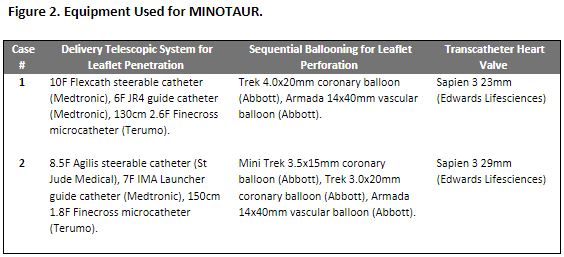
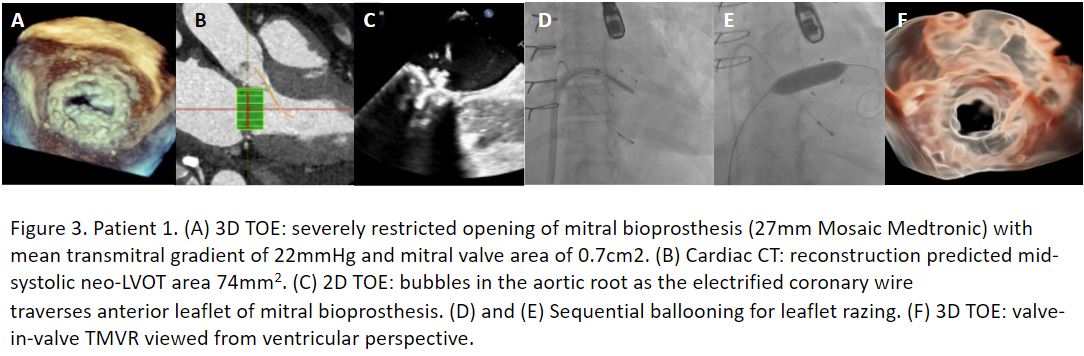
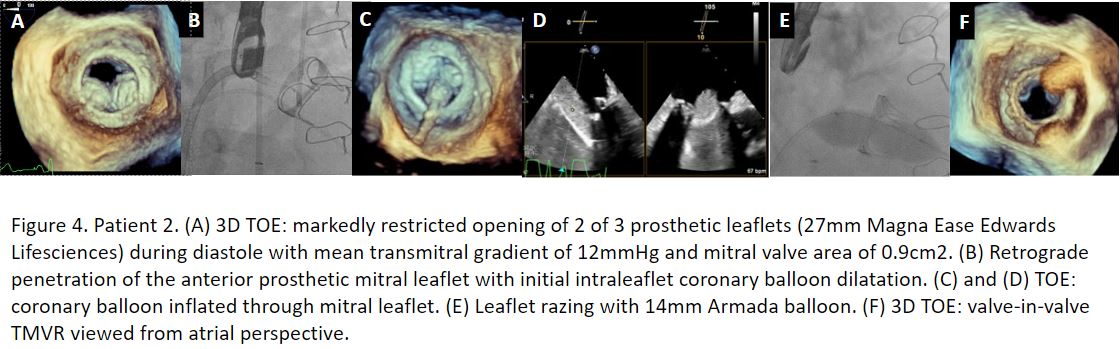
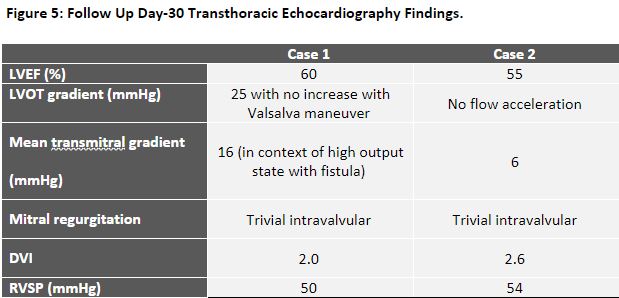
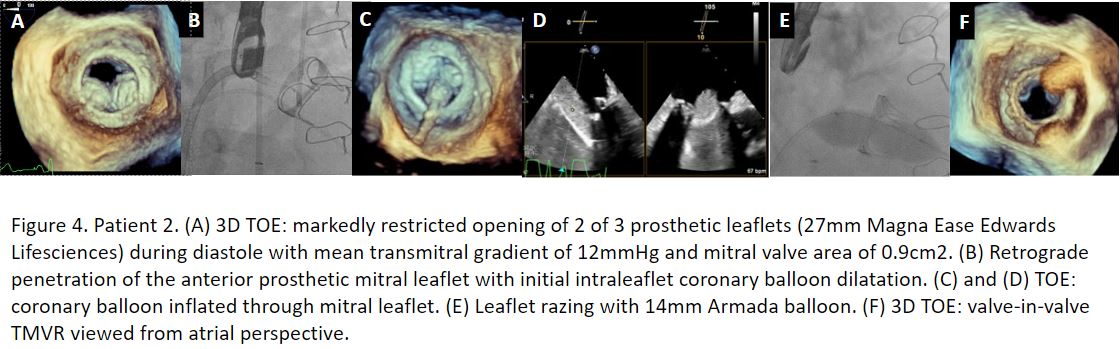
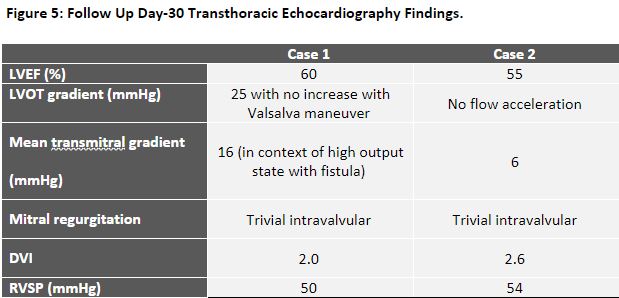
Procedures were performed via femoral venous access under general anaesthesia. Under TEE guidance mid to low-posterior transeptal punctures were made. Penetration of the anteromedial prosthetic mitral leaflet was achieved via an antegrade approach for case 1 and retrograde for case 2 with an Astato XS 40 300cm 0.014” wire with cautery on 100W pure-cut mode, delivered via a telescopic system outlined in figure 2. Following fluoroscopic and TEE confirmation of leaflet traversal, a 330 cm RG3 wire was exchanged via the microcatheter. Over this newly created veno-atrio-ventricular rail through the penetrated prosthetic mitral leaflet, sequential ballooning with coronary balloons was performed to achieve leaflet perforation. A 110 cm 5F pigtail catheter was then exchanged over the RG3 into the LV and further exchanged for a Safari2 guidewire. Further sequential ballooning was then performed through the penetrated leaflet with vascular balloons for inside-out leaflet annihilation (figure 3 and 4). Edwards Sapien 3 transcatheter heart valves were delivered through the intra-leaflet tract and deployed under rapid ventricular pacing to achieve VIV TMVR to complete the leaflet modification. There were no neurological or vascular complications and both patients had marked symptomatic and echocardiographic improvement (figure 5). Our findings suggest that MINOTAUR is a viable option for patients at high risk of neo-LVOTO from ViV TMVR who otherwise would have limited treatment options.
Case Summary
MINOTAUR is a feasible minimally invasive transcatheter percutaneous technique for the modification of degenerative mitral bioprosthetic valves being managed with VIV TMVR to mitigate the risk of neo-LVOTO. Investigation of the technique in larger patient cohorts is warranted.


