Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-076
Complicated Road Block: Retrograde Chronic Total Occlusion Intervention via Occluded Saphenous Venous Graft
By Avik Karak, Shuvanan Ray
Presenter
Avik Karak
Authors
Avik Karak1, Shuvanan Ray1
Affiliation
Fortis Hospital, India1,
View Study Report
TCTAP C-076
Coronary - Complex PCI - CTO
Complicated Road Block: Retrograde Chronic Total Occlusion Intervention via Occluded Saphenous Venous Graft
Avik Karak1, Shuvanan Ray1
Fortis Hospital, India1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
65 years old male hypertensive, diabetic admitted with unstable angina. History of CABG in 2011. Patient had a history of progressively deteriorating angina over the last two months before admission. CT coronary angiography was done which showed 90% stenosis of the RSVG graft to Ramus to PLV. Patient was hemodynamically stable without any evidence of heart failure.
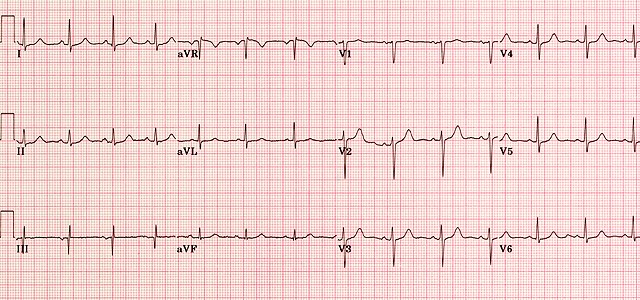
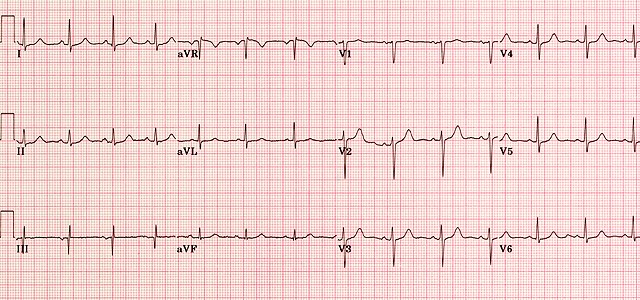
Relevant Test Results Prior to Catheterization
Resting ECG was normal. Normal resting LV function without RWMA.Renal function was normal.
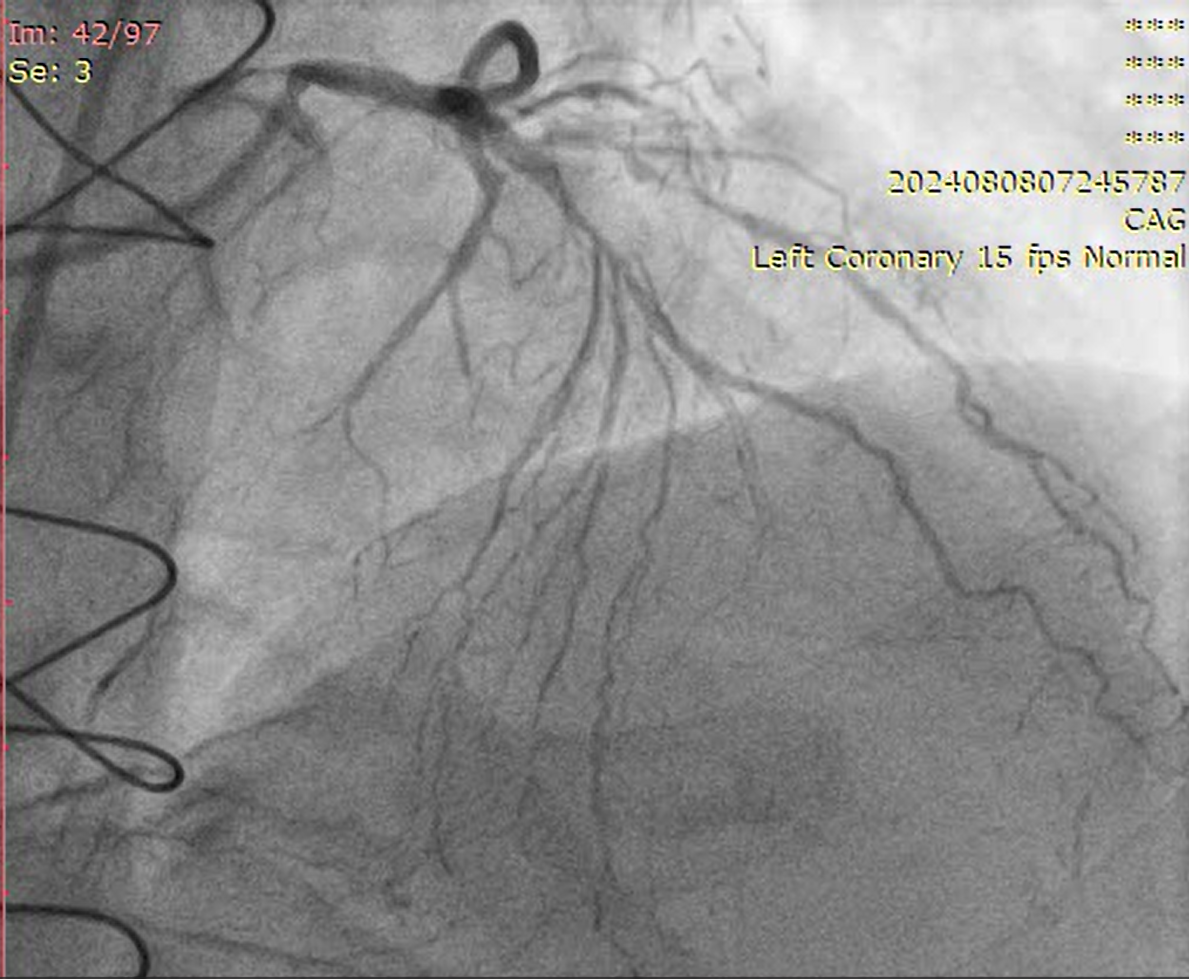
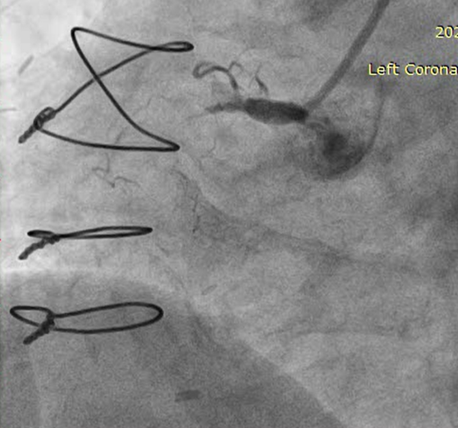
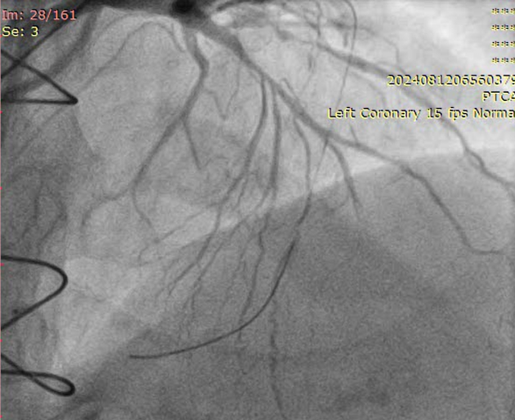
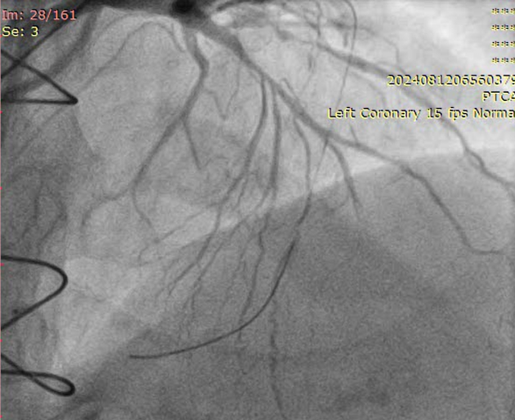
Relevant Catheterization Findings
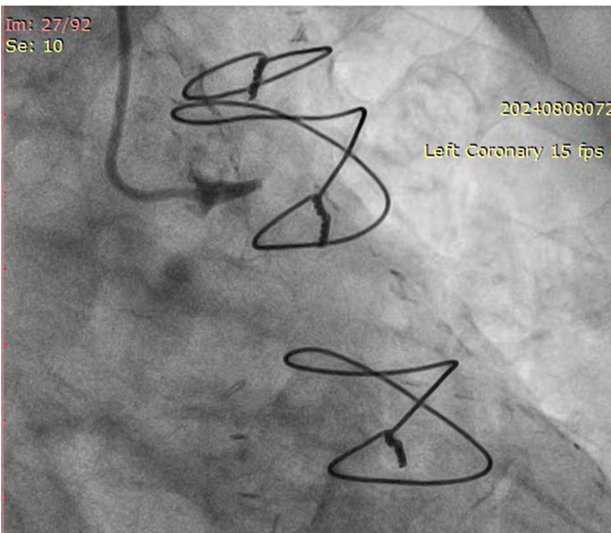
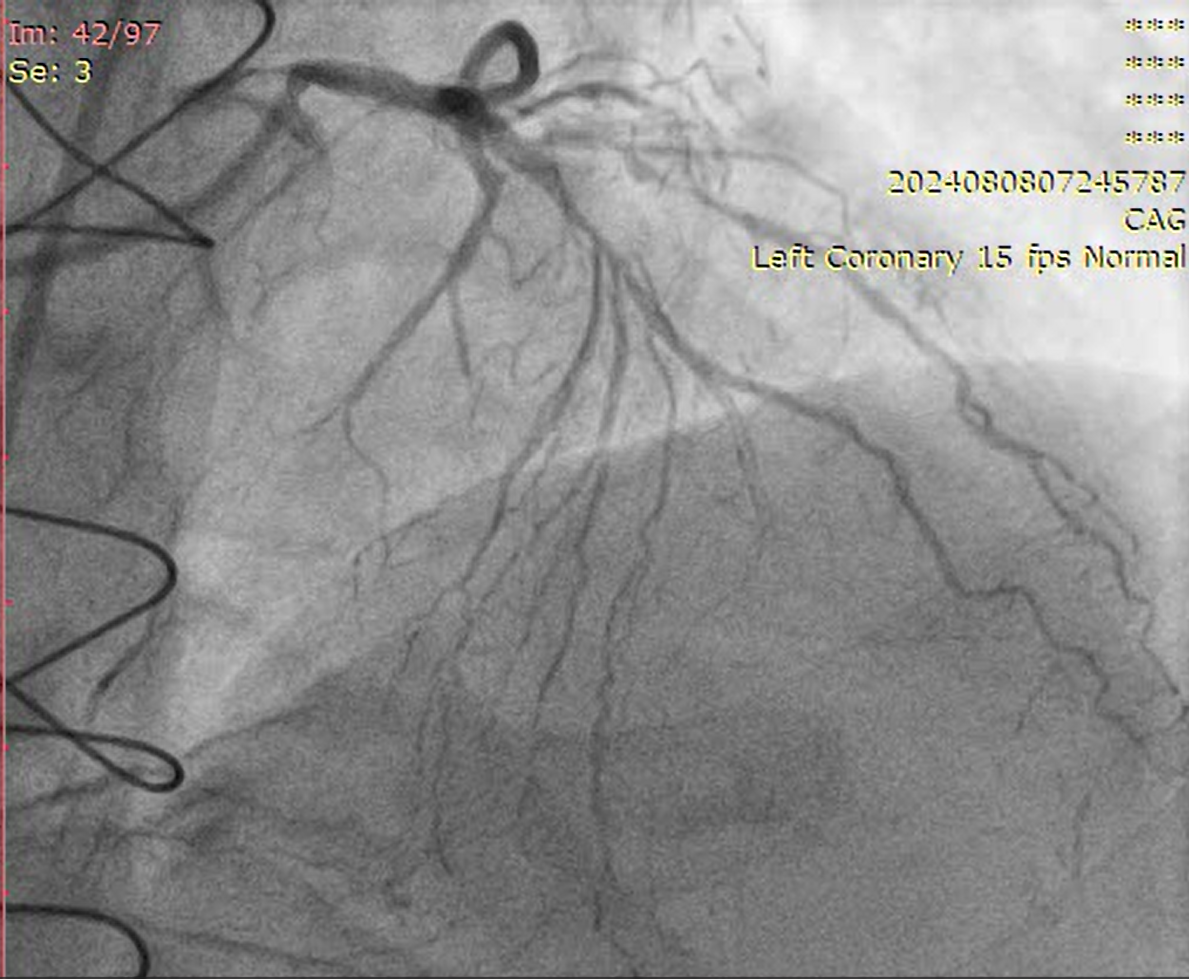
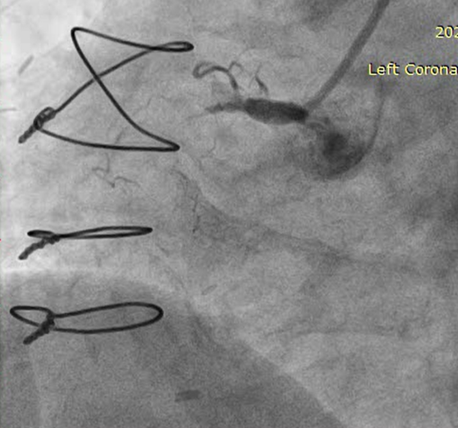
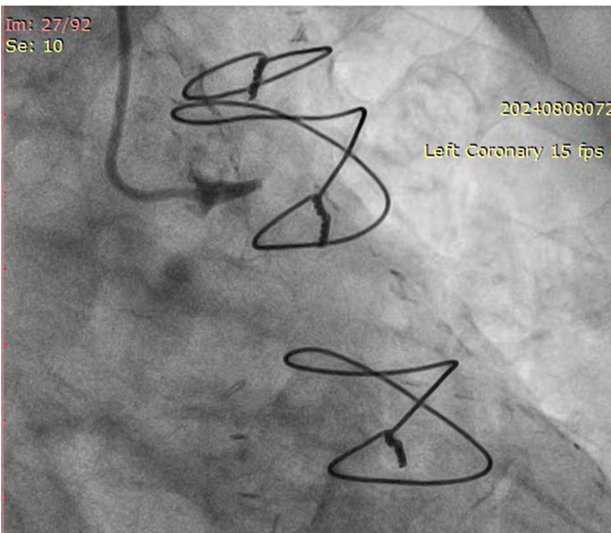
LMCA: distal mild stenosisLAD: diffusely disease from proximal part with total occlusion in mid part with competitive fillingD1, Ramus, OM1- total occlusionLCX: mild diffuse disease RCA: CTO from proximal part, retrograde filling from LADLIMA to LAD: patentSequential LIMA - RIMA “Y” to OM1 to PDA: occludedSequential RSVG to ramus to PLV branch of RCA- occluded
Interventional Management
Procedural Step
RSVG to Ramus to PLV was engaged with 7F AR-1 guide catheter. Occluded segment in RSVG crossed with Pilot-150 PTCA wire with Caravel micro-catheter and parked into distal RCA. Position of the wire and micro-catheter confirmed with retrograde injection from native LMCA. Retrograde wiring was attempted with Gaia NexT-2, Pilot-150, Pilot-200 PTCA guide wires, but was unsuccessful. Native RCA was engaged with 7F AL 0.75 guide catheter and antegrade wiring was attempted with micro-catheter support and Gaia NexT-2, Pilot-150 followed by Pilot-200 PTCA guide wires, but was unsuccessful. Balloon dilatation was done in proximal RCA with 2.0 x 10 mm SC balloon. Knuckle wire technique was used to cross the lesion from antegrade site but unsuccessful. Finally, lesion crossed with Asahi Gladius MG-14 wire from antegrade approach and wire parked into the RSVG. Micro-catheter exchanged. Serial predilatation was done with 0.75 x 8 mm SC balloon followed by 2.0 x 20 mm SC balloon. IVUS run was taken for vessel size estimation. 3.0 x 48mm DES was deployed from proximal RCA. Post dilatation was done with NC 3.5 x 8 mm balloon. Distal RCA was addressed with 2.75 x 30 mm DEB. Mid RCA was stented with DES 3.00 x 32 mm. Post-dilated with 3.0 x 10 mm NC balloon followed by 3.75 x 8 mm NC balloon. Post-stenting IVUS run showed good stent expansion and apposition. Distal TIMI-III flow was achieved.
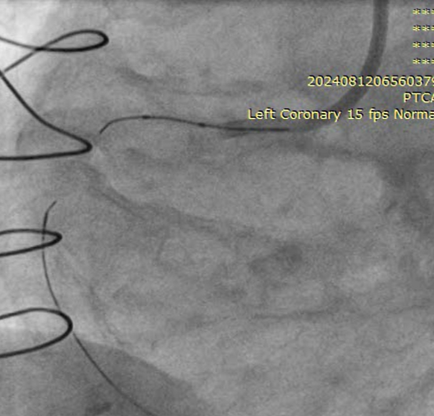

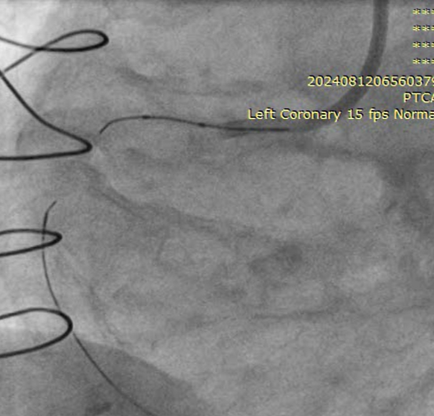

Case Summary
Occluded and degenerated venous grafts are better not to be intervened if not acute occlusion. Septal collaterals are best for retrograde CTO intervention but in our case the occluded SVG graft which was sequentially connected to ramus followed by the PLV branch of RCA proved to be a very good channel for the same. Appropriate wire escalations and sequential retrograde CTO techniques need to be carefully used. In our case Retrograde CART technique was successfully used followed by antegrade wire crossing. Ultimately the CTO lesion was treated thereafter antegradely. Intracoronary imaging is essential for such case and IVUS was used in our case.


