Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-010
One Way Forward
By Choutchung Tinakorn Na Ayudhya
Presenter
Choutchung Tinakorn Na Ayudhya
Authors
Choutchung Tinakorn Na Ayudhya1
Affiliation
King Chulalongkorn Memorial Hospital, Thailand1,
View Study Report
TCTAP C-010
Coronary - ACS/AMI
One Way Forward
Choutchung Tinakorn Na Ayudhya1
King Chulalongkorn Memorial Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 67 year old man known case type II DM, HT, DLP presented to the ER with dyspnea on exertion for 3 days with worsening orthopnea and PND. He denied having chest discomfort or missing of medications. His current medications included Manidipine, Atorvastatin, Metformin, Losartan, HCTZ and Sitagliptin.
Relevant Test Results Prior to Catheterization
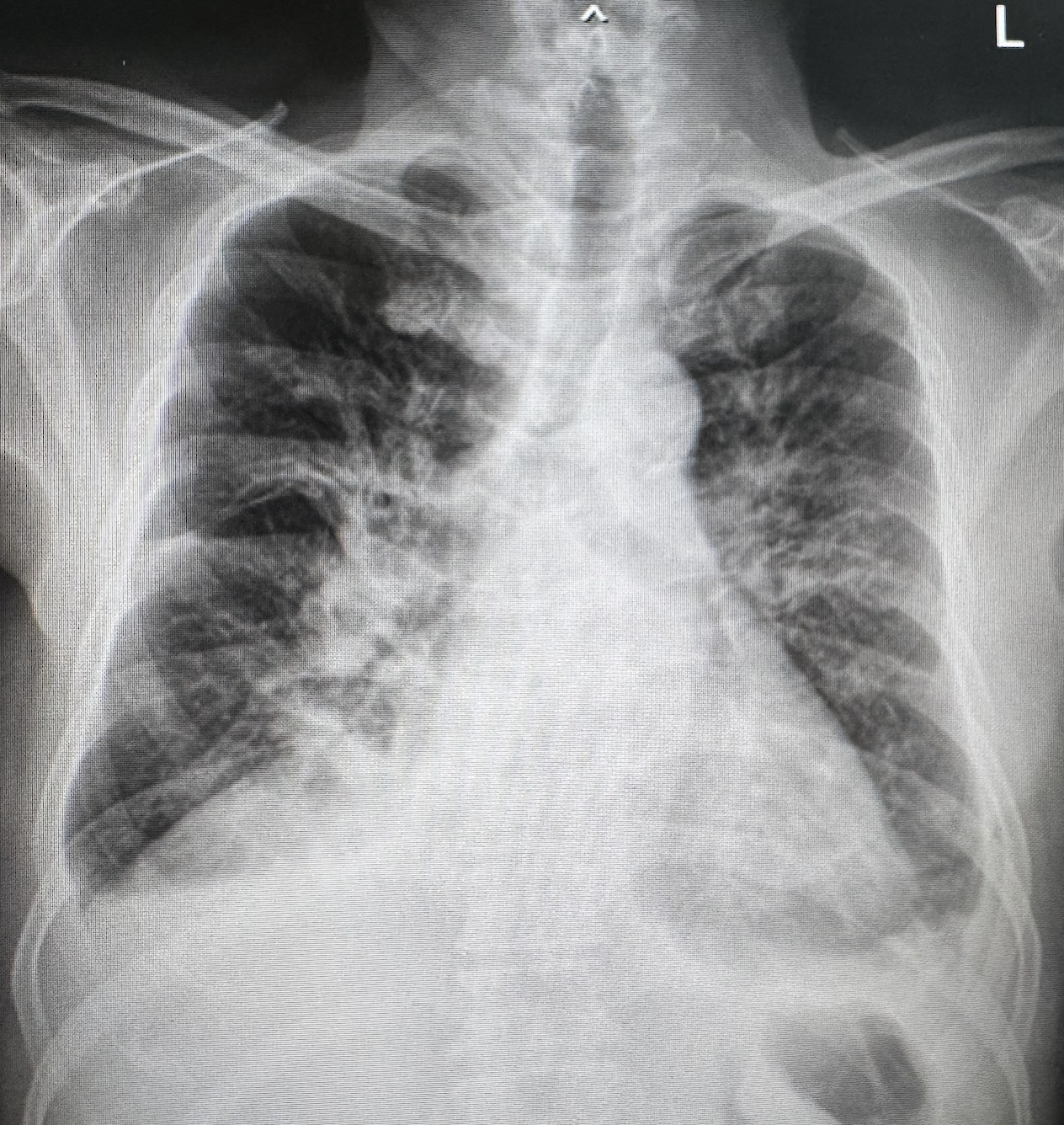
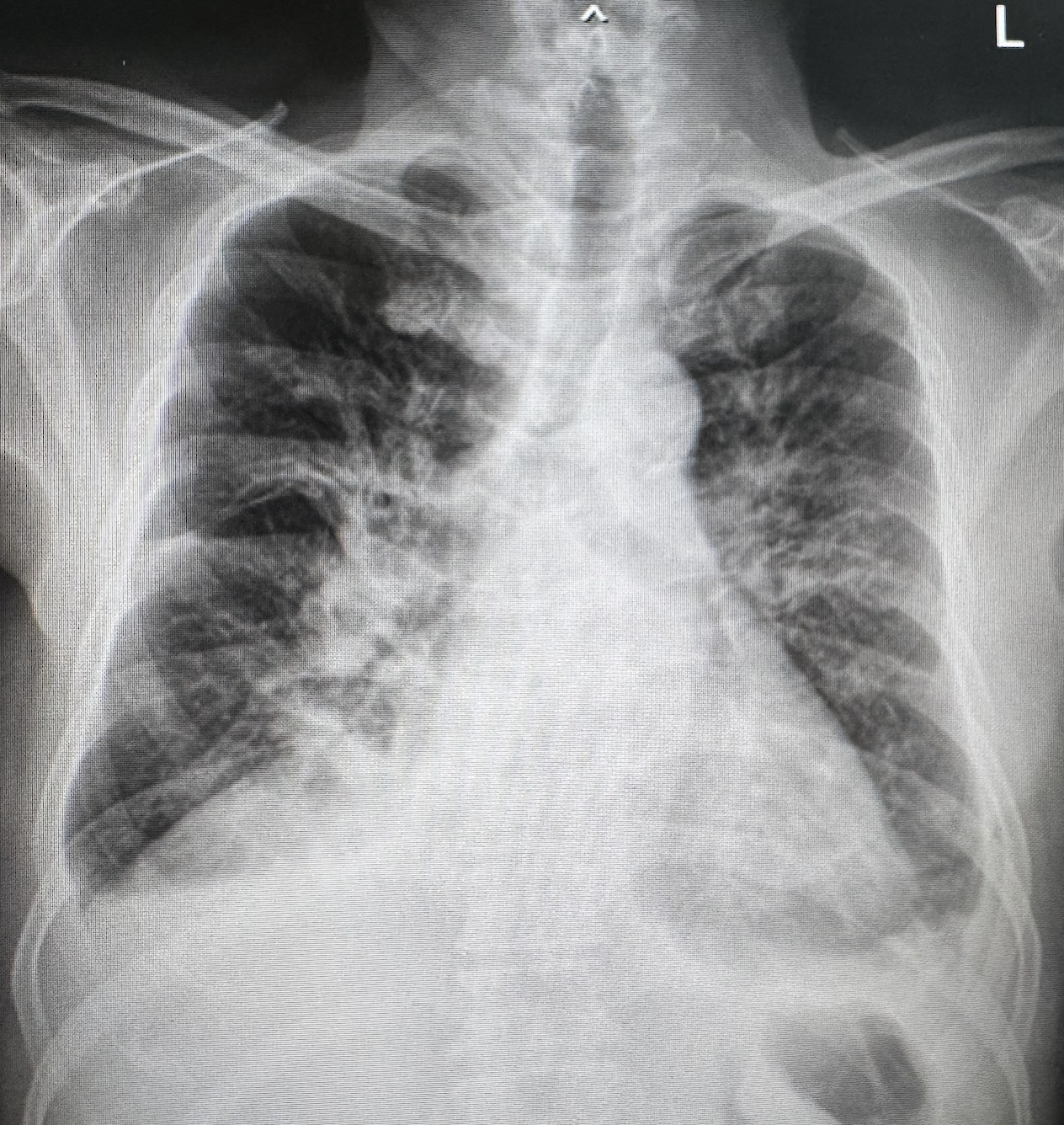
LAB Hct 30 Bun 65 Cr 3 Na 124 K 3.9 Cl 93 CO2 18 hsTnI 15,650
Relevant Catheterization Findings
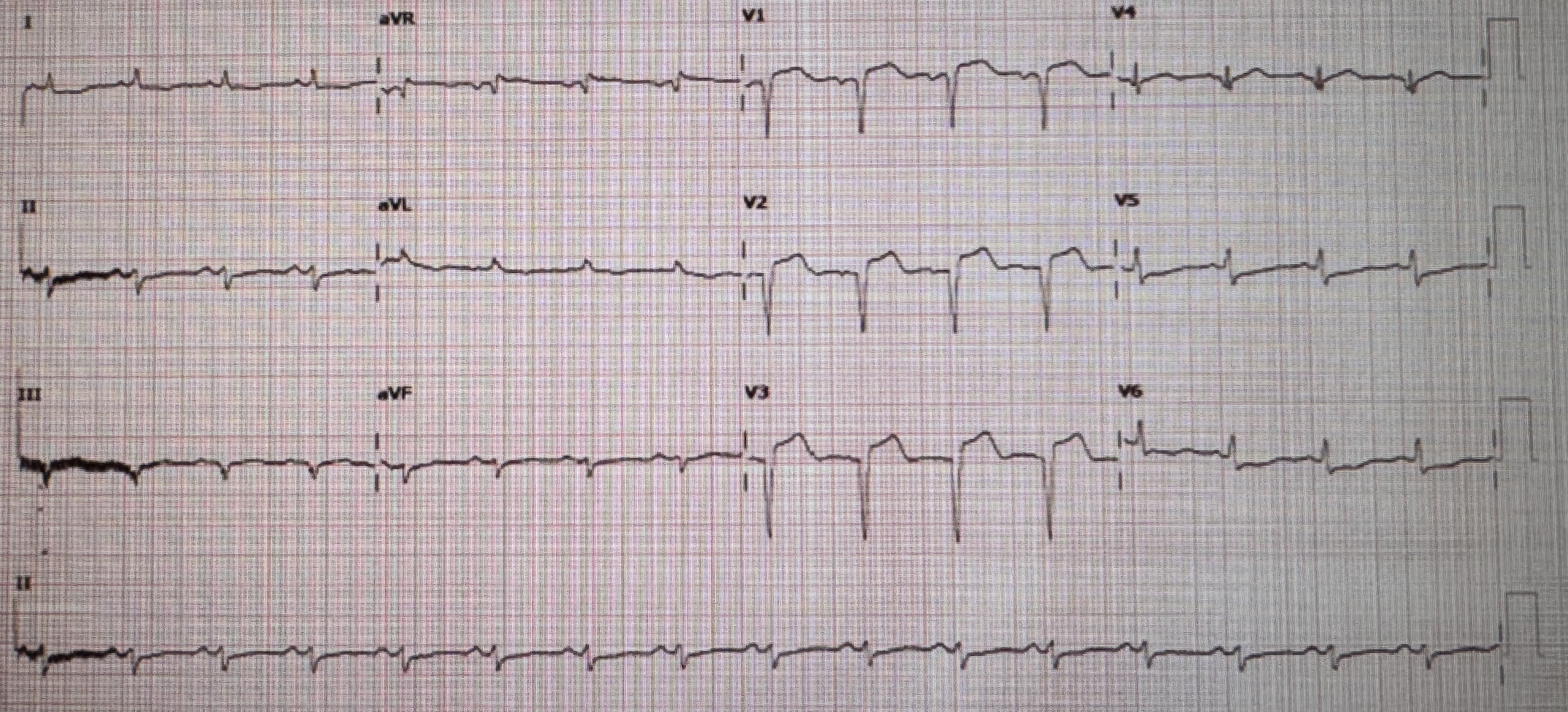
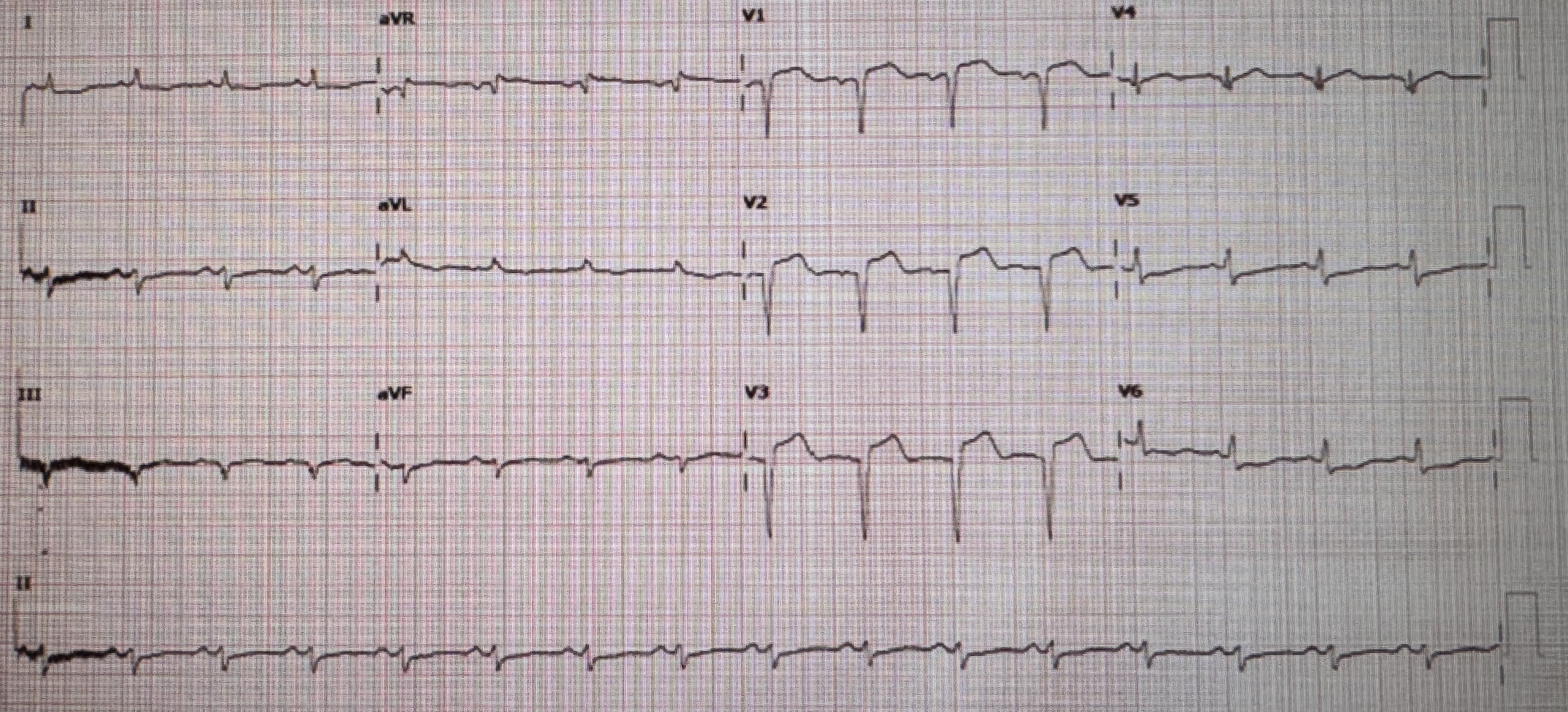
CAG showed 50% stenosis at mid to distal LM trifurcation Medina 1-1-1-1. 90% stenosis at proximal LAD with 100% stenosis at mid LAD with TIMI II flow likely from thrombus. There was collateral from RCA to mid to distal LAD seen. 80% stenosis at proximal RI. 90% stenosis at proximal Lcx. 90% stenosis at proximal RCA.
Interventional Management
Procedural Step
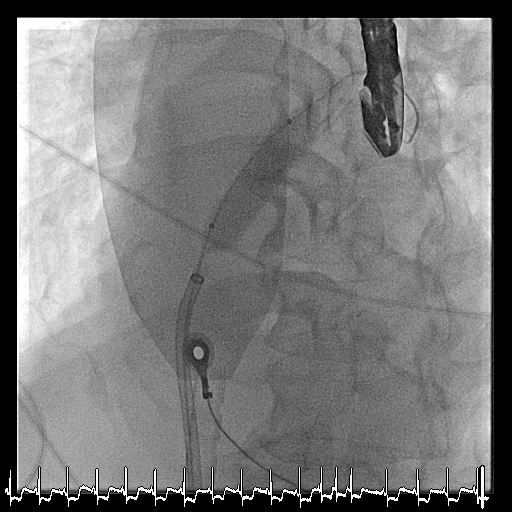
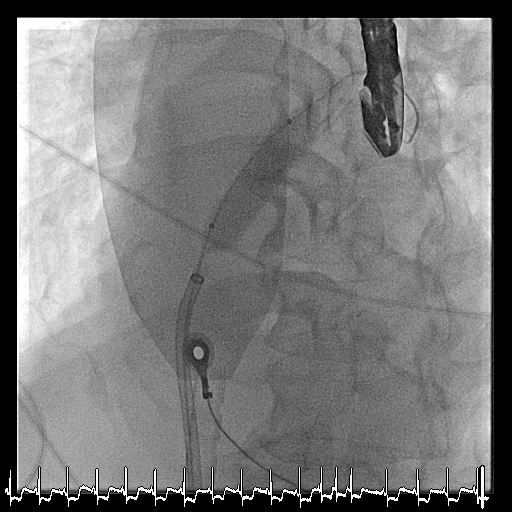
We consult CVT for CABG but patient developed VF arrest and VT storm not response to medication. IABP and VA ECMO was inserted. After ECMO patient developed pulmonary edema so interatrial septostomy using 12x40 mm balloon was done. Then PCI to RCA was done due to RCA giving collateral to LAD using 7Fr JR4 guiding catheter via right radial artery. Rotablator was done using 1.5 Burr at proximal RCA due to calcified lesion. Then pre dilatation with NC balloon and cutting balloon. DES 3.5x30 mm was deployed at proximal to mid RCA and post dilated with NC balloon 4.0x15 mm. patient could wean off VA ECMO but still had short run polymorphic VT despite amiodarone and lidocaine. Stage PCI to RI, Lcx and LM-LAD was done. Using 7 Fr XB3 guiding catheter. Direct stenting with DES 2.25x14 mm was done at proximal RI. Then TAP was perform at LM-LAD- Lcx bifurcation. Predilate was done at proximal Lcx with SC balloon 2.5x15 mm then DES 2.5x19 mm was deployed at proximal Lcx. Predilated was done at LM-proximal LAD with SC balloon 3.0x15 mm then 3.0x24 mm DES was deployed at LM to LAD and pot with NC 3.5 x12 mm at LM. Final angiogram showed good coronary blood flow in LAD, RI and Lcx.
Case Summary
Mechanical cardiac support remains crucial role in ACS patient with cardiogenic shock or significant cardiac arrhythmia even though never been beneficially proven in a randomize clinical trial. In this case we demonstrated a complex PCI in patient with recent STEMI with cardiogenic shock from VT storm using IABP and VA ECMO for cardiac support.


