Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-109
Complex High Risk Percutaneous Coronary Intervention: Imaging-Guided Rotational Atherectomy and Intravascular Lithotripsy for In-Stent Restenosis of Multiple Overlapping Stents With Severe Calcifications
By Bryan Rene Toledano, Jeffrey Chua
Presenter
Bryan Rene Toledano
Authors
Bryan Rene Toledano1, Jeffrey Chua1
Affiliation
The Medical City, Philippines1,
View Study Report
TCTAP C-109
Coronary - Complex PCI - In-Stent Restenosis
Complex High Risk Percutaneous Coronary Intervention: Imaging-Guided Rotational Atherectomy and Intravascular Lithotripsy for In-Stent Restenosis of Multiple Overlapping Stents With Severe Calcifications
Bryan Rene Toledano1, Jeffrey Chua1
The Medical City, Philippines1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 62-year-old male presented with worsening chest pain radiating to the jaw and left arm over 6 months, relieved by isosorbide dinitrate. He has two-vessel coronary artery disease with LAD involvement and chronic RCA occlusion since 2003. He underwent PCI to the LAD in 2003 for unstable angina, and in 2009 and 2012 for in-stent restenosis. His history also includes hypertension, type II diabetes, anxiety disorder and failed bilateral peripheral angioplasty of the superficial femoral arteries
Relevant Test Results Prior to Catheterization
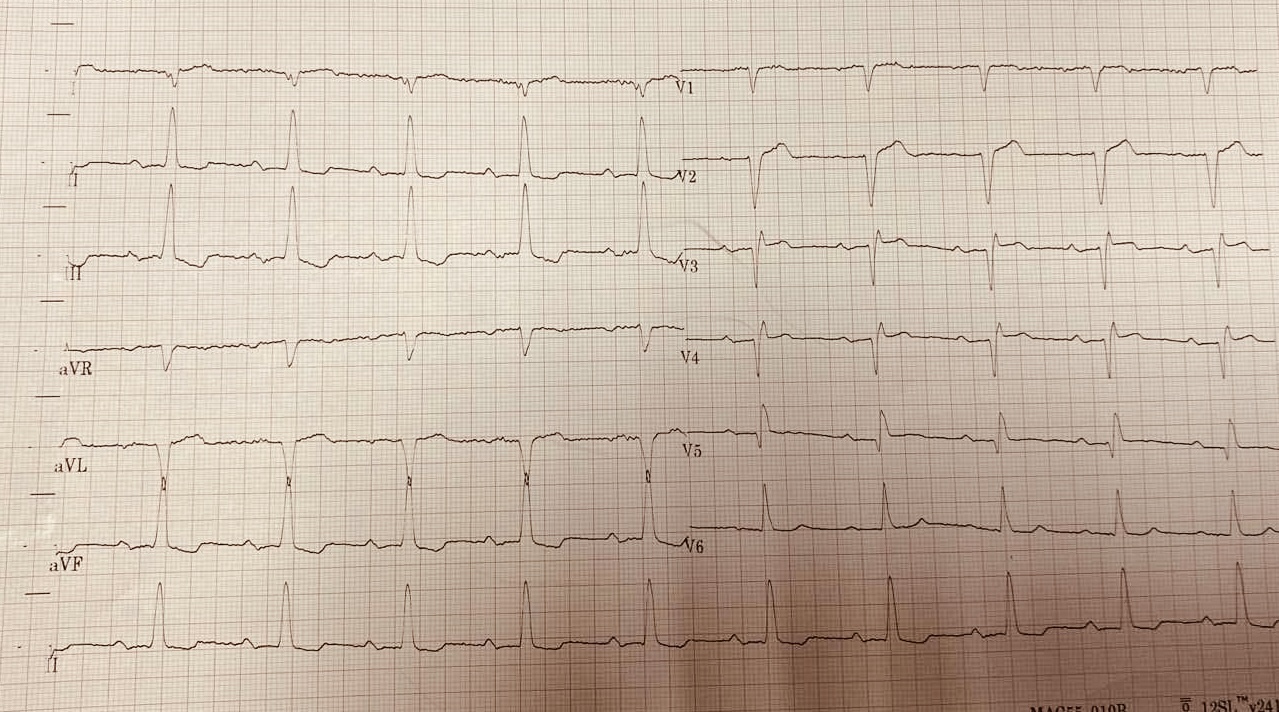
His 12-lead ECG showed sinus rhythm, inferior wall ischemia, and anteroseptal infarct of indeterminate age (Figure 1). Troponin I was mildly elevated. A 2D echocardiogram revealed severe hypokinesia in the LAD distribution and reduced systolic function at 37% (Simpsons). Incomplete PCI records indicate Cypher and Velocity stents in the proximal to mid LAD (2003), Taxus stents (2.5 × 8 mm, 3.0 × 20 mm) in the proximal and mid LAD (2009), and a Veriflex 3.5 × 8 mm stent in the proximal LAD (2012).
Relevant Catheterization Findings
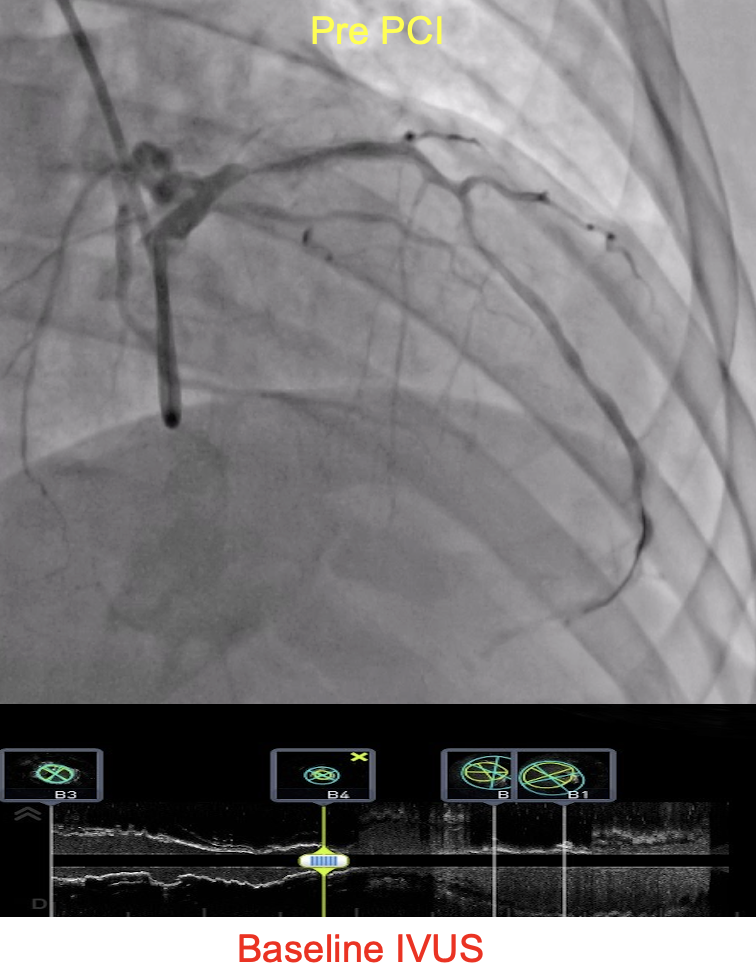
The right coronary artery is small, diffusely diseased, and totally occluded in the distal segment. The LAD is calcified, diffusely diseased, with 90-95% in-stent restenosis in the ostioproximal segment and 70-80% stenosis in the mid segment without prior stenting. The left main and circumflex arteries are free from significant disease. Coronary artery bypass grafting was advised, but the patient strongly refused.
Interventional Management
Procedural Step
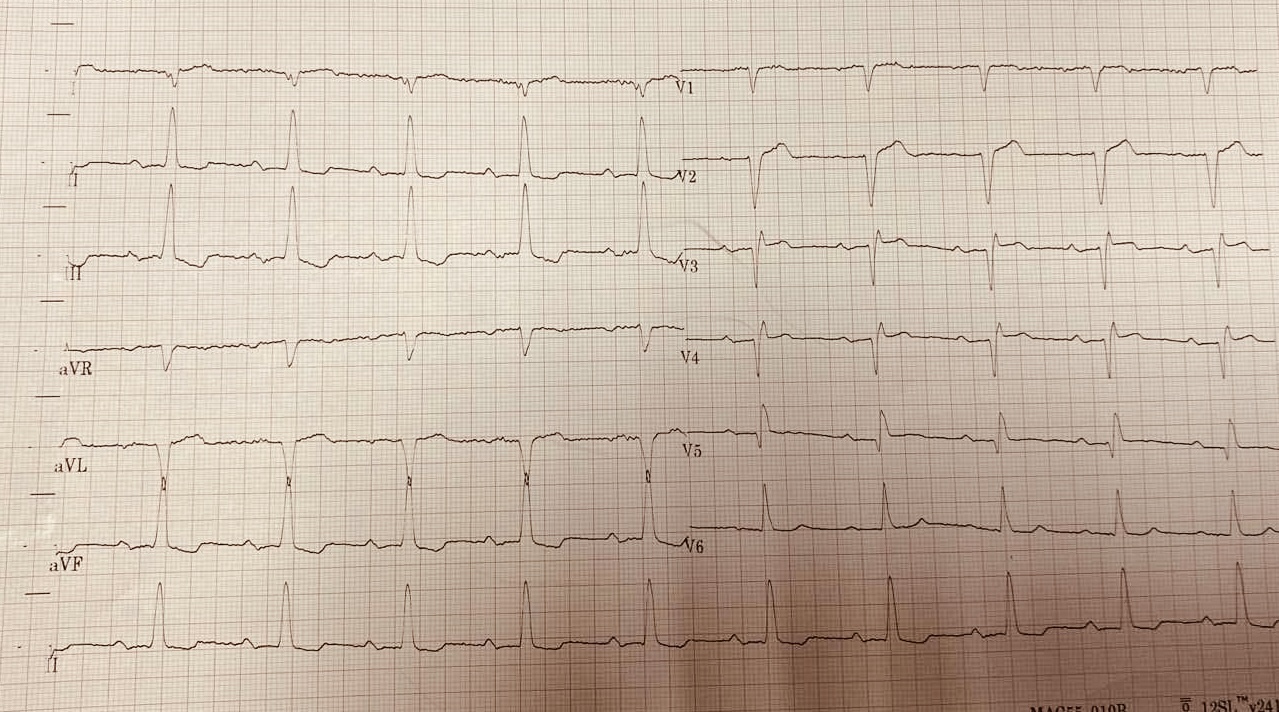
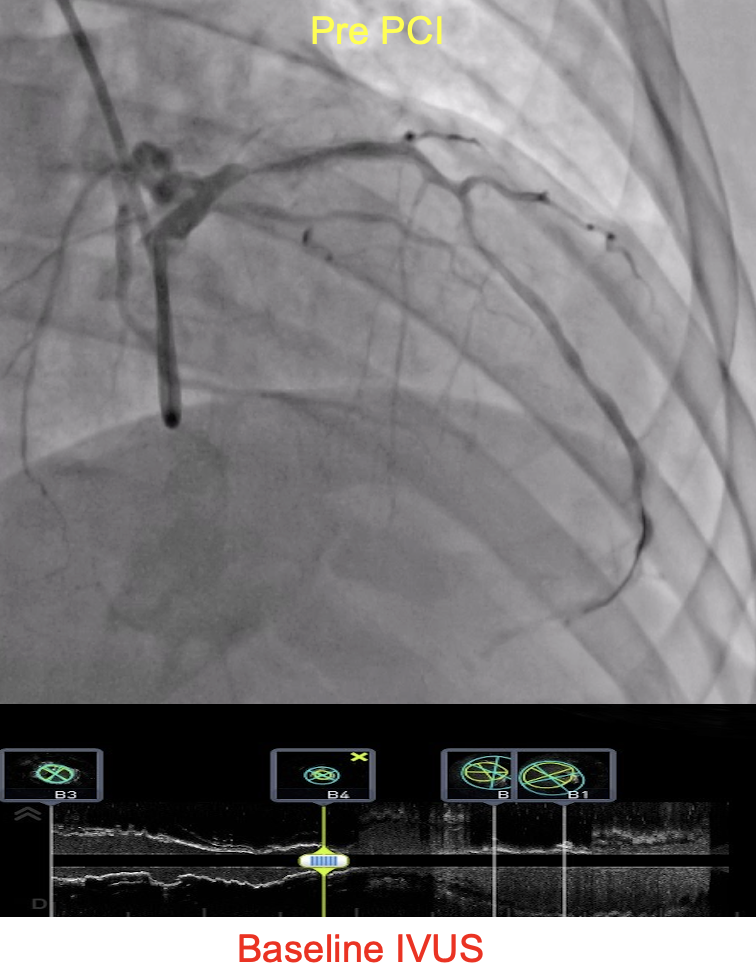
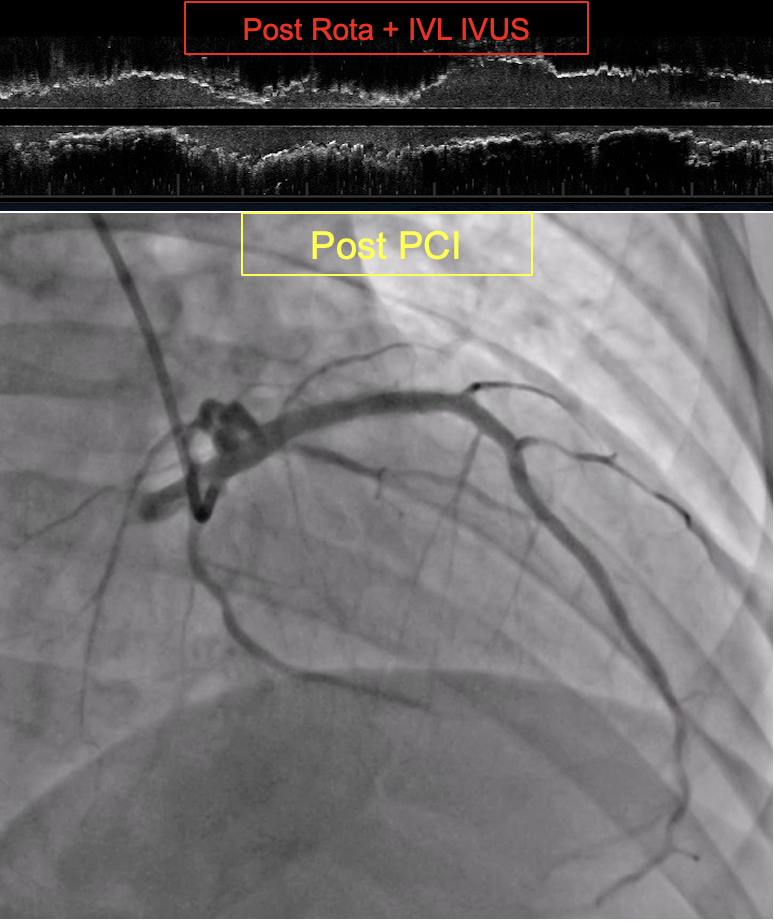
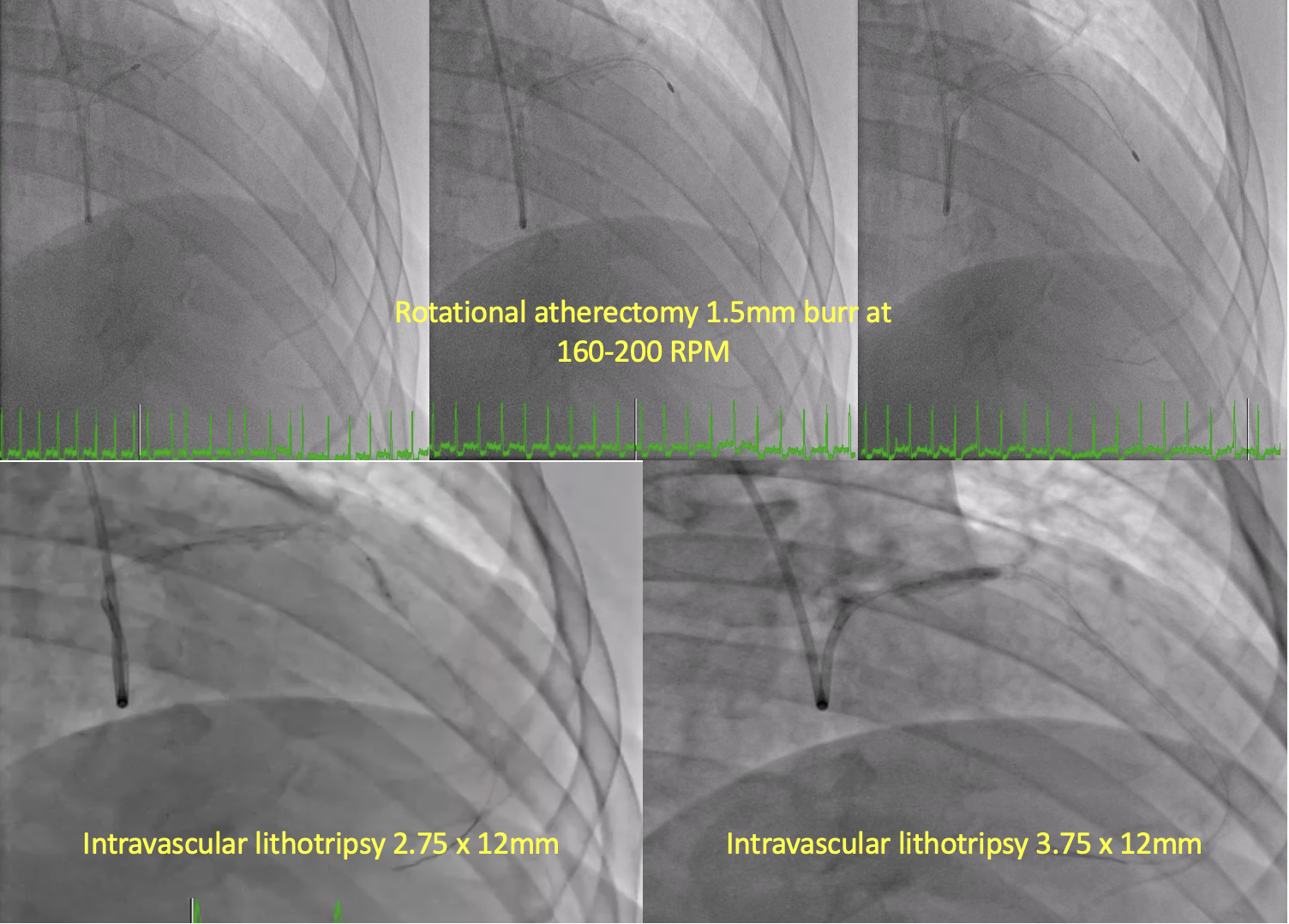
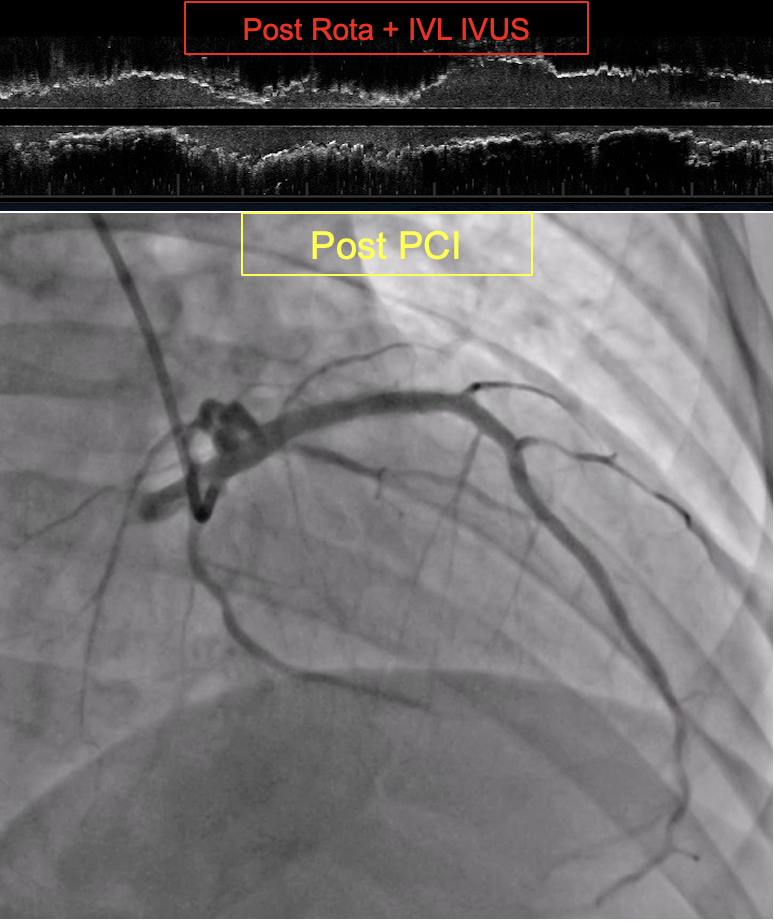
A 6-7F sheath via the right radial artery was used, with a 7F VL 3.5 guide catheter and a 7F Guidezilla II for support. IVUS crossed the proximal segment after predilation with 1.25x15 mm and 2.0x15 mm balloons. Pre-PCI IVUS revealed severe calcifications and neoatherosclerosis as the main cause of in-stent restenosis (Figure 2). A 1.5 mm Rotablator burr was used to modify plaques from the ostial to mid LAD. During atherectomy, the patient experienced severe chest pain and hypotension, which resolved with IV morphine and norepinephrine. An IVL catheter (2.75x12 mm) treated the mid segment with 6 cycles of 10 pulses, after stepwise predilation with cutting (2.25-2.5x10 mm) and NC (2.5-2.7x15 mm) balloons. Another IVL catheter (3.5x12 mm) treated the ostioproximal segment with 5 cycles of 10 pulses (Figure 3). Severe pain and hypotension recurred, and angiography showed no-reflow. A Corsair Pro XS delivered 2 mg of nicardipine distally, partially improving flow. Synergy DES (3.0x24 mm, 3.0x20 mm) were deployed in the mid LAD. IVUS revealed a flow-limiting distal hematoma, prompting a Synergy 2.75x24 mm DES deployment, restoring flow. The procedure concluded with Synergy 4.0x28 mm DES in the proximal segment and Synergy 5.0x28 mm DES in the LM-ostial segment. Post-dilation and Proximal Optimization with NC balloons (4.5x12 mm, 5.0x8 mm) achieved TIMI 3 flow, well-apposed and expanded stents with minimal stented area of 7.84mm2 in the proximal LAD (Figure 4)
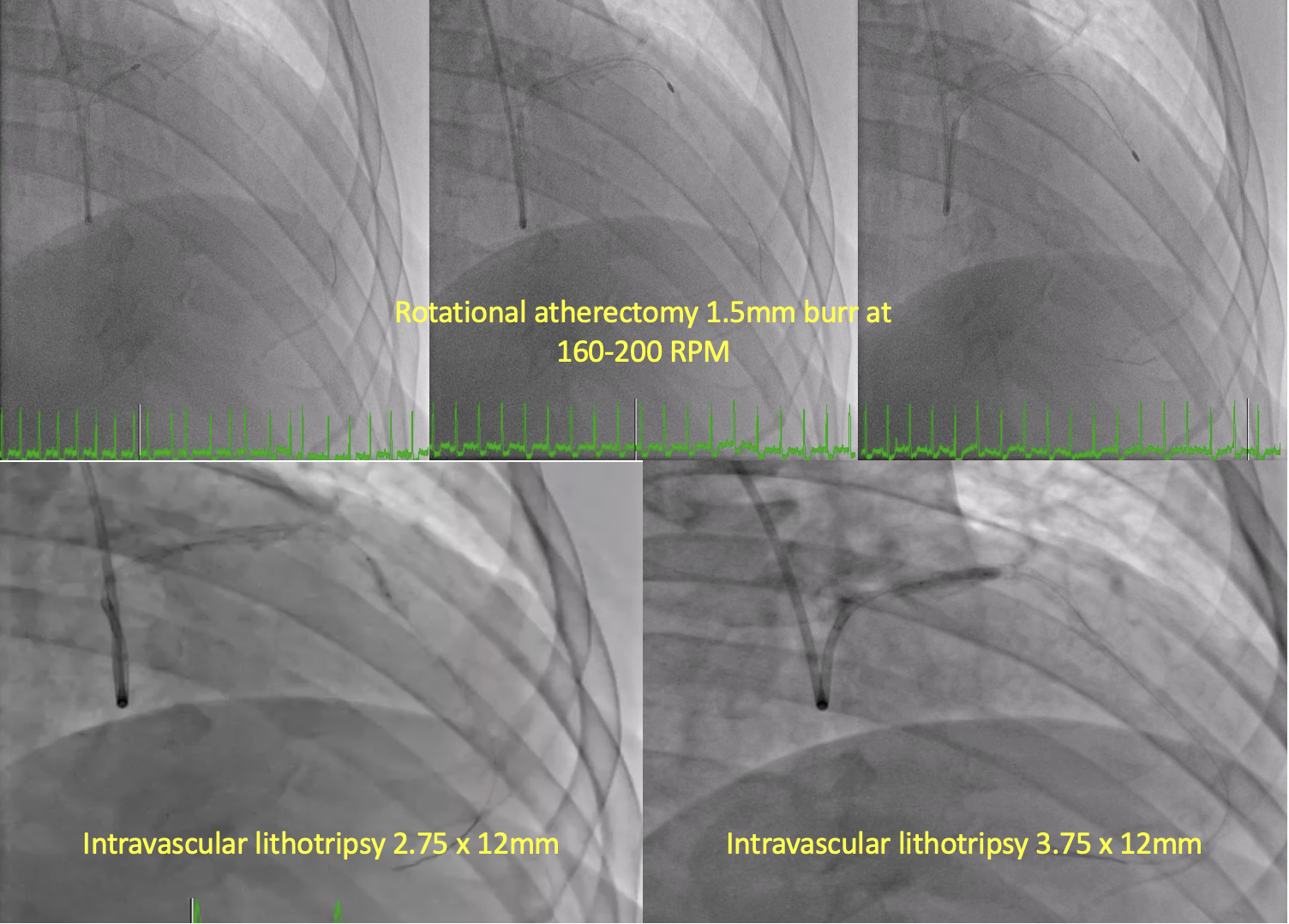
Case Summary
In this complex high-risk PCI case of NSTEMI with severely reduced ejection fraction, CABG refusal and infeasible access for mechanical circulatory support posed challenges. Severe in-stent restenosis involving multiple bare-metal and drug-eluting stents with heavily calcified lesions was successfully managed using imaging guidance with IVUS and a combination of calcium modification techniques, including cutting balloons, rotational atherectomy, and intravascular lithotripsy. No-reflow and distal hematoma formation should be anticipated and promptly managed in such interventions. In our knowledge this is the first Rotatripsy case in the Philippines, demonstrating its utility.


