Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-208
In Doubt of High-Risk Noncardiac Surgery Following Percutaneous Coronary Intervention (PCI) and Transcatheter Aortic Valve Replacement (TAVR): When Is the Best Time?
By Apichat Jansillapakorn, Kittipong Youpaniad, Anuruck Jeamanukoolkit, Wasant Soonfuang, Sukhum Tachasakunjaroen, Sakolwat Montrivade
Presenter
Apichat Jansillapakorn
Authors
Apichat Jansillapakorn1, Kittipong Youpaniad1, Anuruck Jeamanukoolkit1, Wasant Soonfuang1, Sukhum Tachasakunjaroen1, Sakolwat Montrivade1
Affiliation
Police General Hospital, Thailand1,
View Study Report
TCTAP C-208
Structural - Aortic Valve Intervention - Coronary Artery Protection / Access
In Doubt of High-Risk Noncardiac Surgery Following Percutaneous Coronary Intervention (PCI) and Transcatheter Aortic Valve Replacement (TAVR): When Is the Best Time?
Apichat Jansillapakorn1, Kittipong Youpaniad1, Anuruck Jeamanukoolkit1, Wasant Soonfuang1, Sukhum Tachasakunjaroen1, Sakolwat Montrivade1
Police General Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A Thai 85-year-old woman with history of prior myocardial infarction, AF, type 2 DM, HTN and DLP, presented with a 5-month history of exertional dyspnea. Physical examination revealed fine crepitations in both lower lung fields, irregularly irregular with lower volume of carotid pulse and grade 3 systolic ejection murmur at right upper parasternal border with sign of left ventricular hypertrophy.


Relevant Test Results Prior to Catheterization
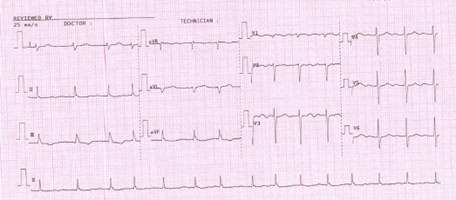
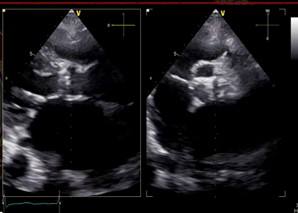
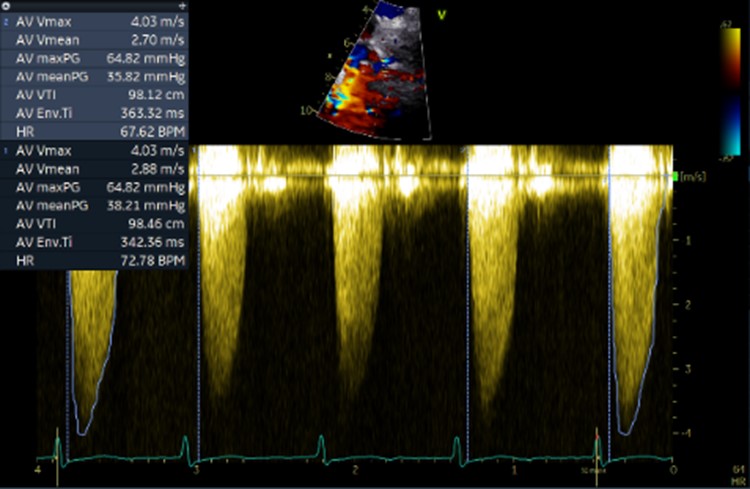
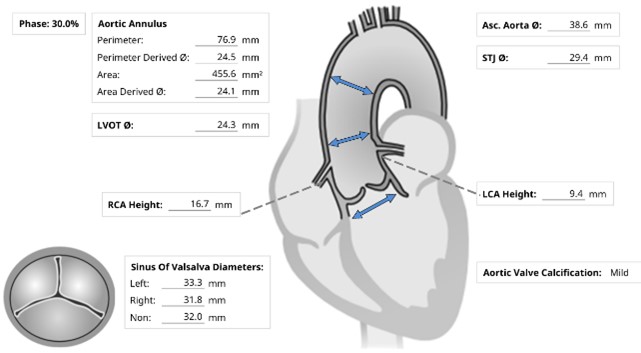
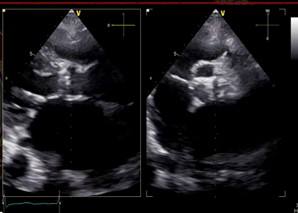
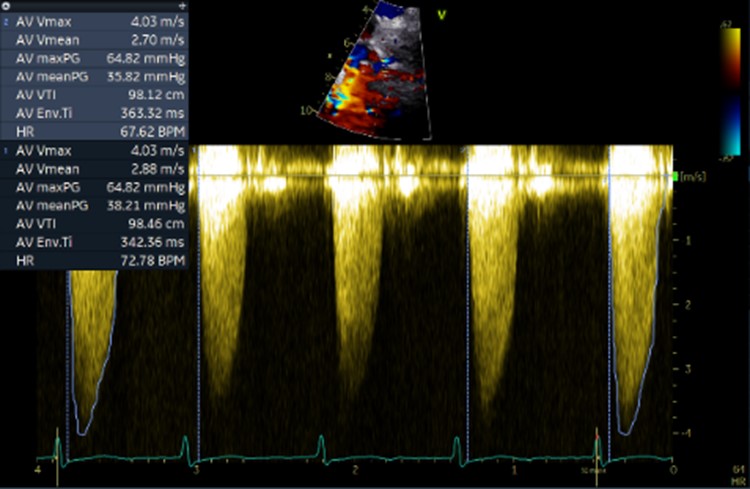
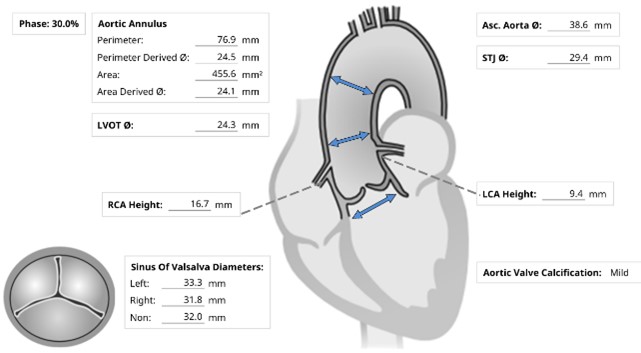
Initial ECG revealed AF. Transthoracic echocardiography revealed concentric LVH with a 70 % of left ventricular systolic function, normal right ventricular systolic function, bi-atrial enlargement and severe calcific aortic stenosis which classified as stage D1 (AVA 0.98 cm2 by AV VTI, AV Vmax 4.03 m/s, mean AV pressure gradient 38.21 mmHg). Following as the Heart Team discussion, Transcatheter Aortic Replacement (TAVR) following coronary angiography (CAG) was scheduled as the optimal choice.
Relevant Catheterization Findings
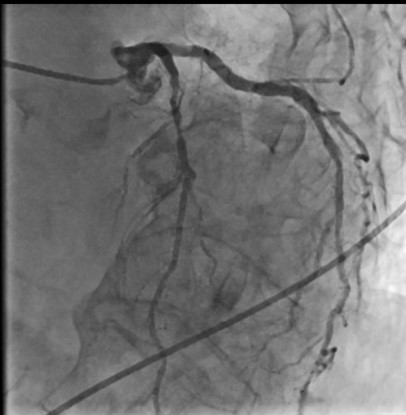
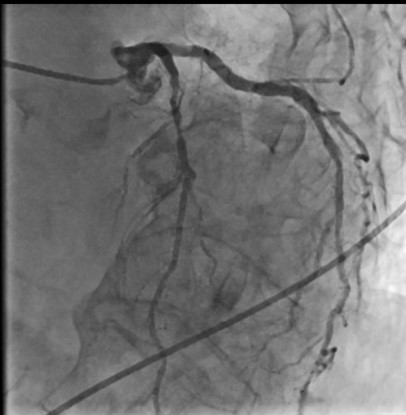
CACAG showed TVD without significant LM stenosis (90 % stenosis of prox-to-mid LAD, 70 % of DG1, 80 % of ostial LCX, 70 % of dis LCX, 90 % of mid RCA and 70 % of PDA). Consequently, the Heart Team's decision, lesion preparation and IVUS-guided stents implantation were completed for the mid RCA and prox-to-mid LAD. The patient was scheduled for TAVR on the next day. On that morning, she developed hematochezia with stable vital signs and hemoglobin. So, the TAVR was proceeded.




Interventional Management
Procedural Step
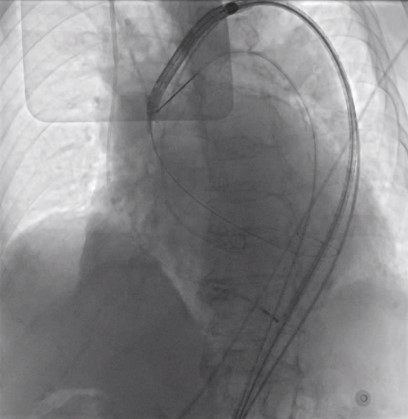
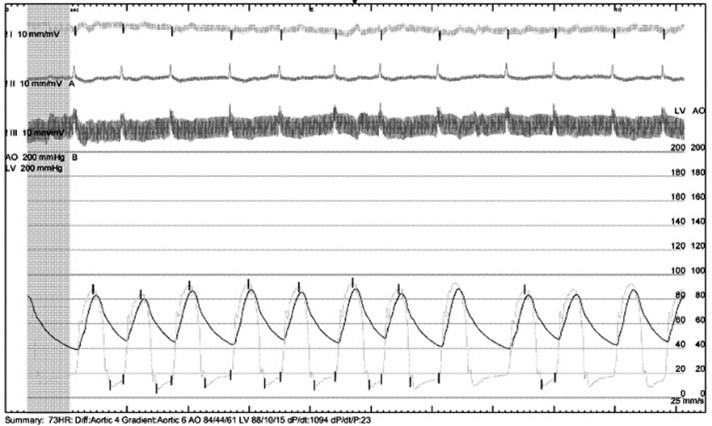
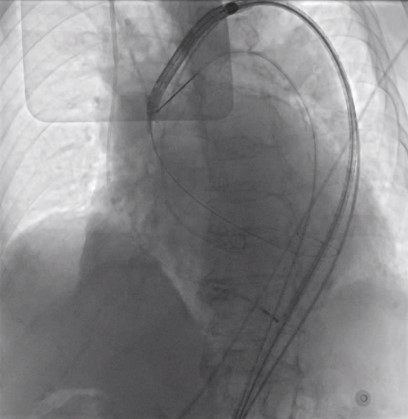
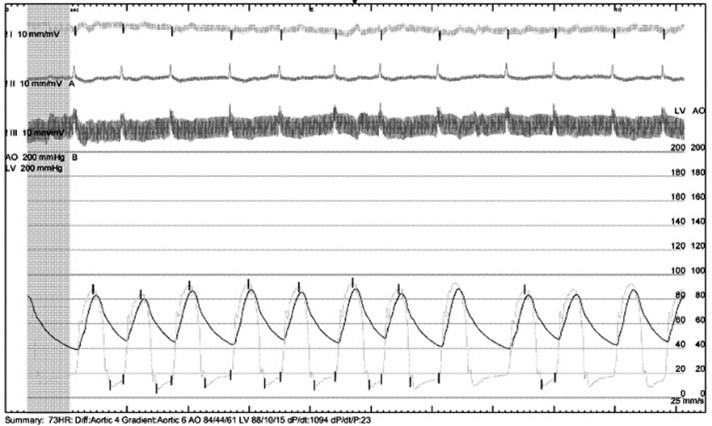
Under local anesthesia and conscious sedation, femoral arteries (FA) were accessed by 8-Fr sheath at right FA and two of 8-Fr sheaths at left FA for pigtail catheter and snare-assisted device. Aortography was conducted by pigtail catheter to locate aortic cusp. An Amplatz left catheter over a 0.035-inchJ-tip wire was placed at aortic cusp via the RFA which was then exchanged with an Amplatz Super Stiff wire to upsized 16-Fr Braidin sheath. The aortic valve was crossed with an Amplatz left catheter over a straight-tip wire under cuspoverlap views (LAO16, CAU 30), peak-to-peak gradient of 19 mmHg. During RV pacing, a Safari Extra Small guidewirewas positioned in LV and the AV was pre-dilated by an 18 × 40 mm Alwide balloon. Subsequently, a 27 mm VitaFlow valve was deployed in an optimal position under snare-assisted. Post-deployment aortography revealed mild AR, LVEDP of20 mmHg, and 4 mmHg of LVOT gradient. Post-dilation was performed by a 24 × 40mm VACC III balloon. The FA was closed by 6-Fr Proglide at the right and 8-Fr AngioSeal at the left. Post-TAVR TEE showed mild PVL without significant transvalvular gradient and preserved LVEF of 64%. One-month after the TAVR, she was diagnosed with early-stage colonic cancer. A laparoscopic hemicolectomy which completed pre-operative evaluation, coronary revascularization, TAVR and appropriated medication was performed as time-sensitive surgery following by CMT with curative intent.


Case Summary
Conclusion


