Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-002
Intracoronary Imaging in Spontaneous Coronary Artery Dissection: Always?
By Nazim Megherbi
Presenter
Nazim Megherbi
Authors
Nazim Megherbi1
Affiliation
King Abdulaziz Specialist Hospital, Saudi Arabia1,
View Study Report
TCTAP C-002
Coronary - ACS/AMI
Intracoronary Imaging in Spontaneous Coronary Artery Dissection: Always?
Nazim Megherbi1
King Abdulaziz Specialist Hospital, Saudi Arabia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
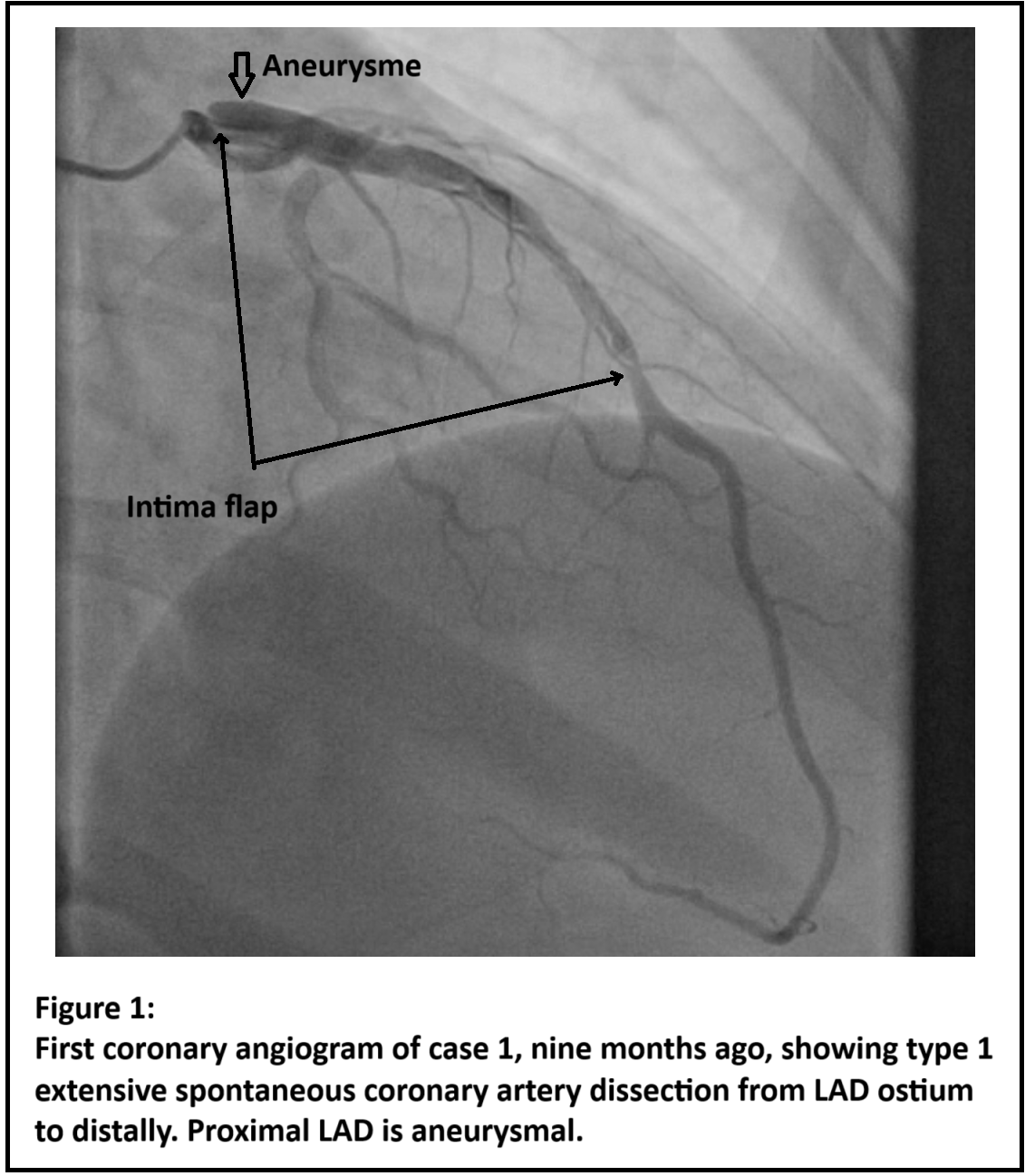
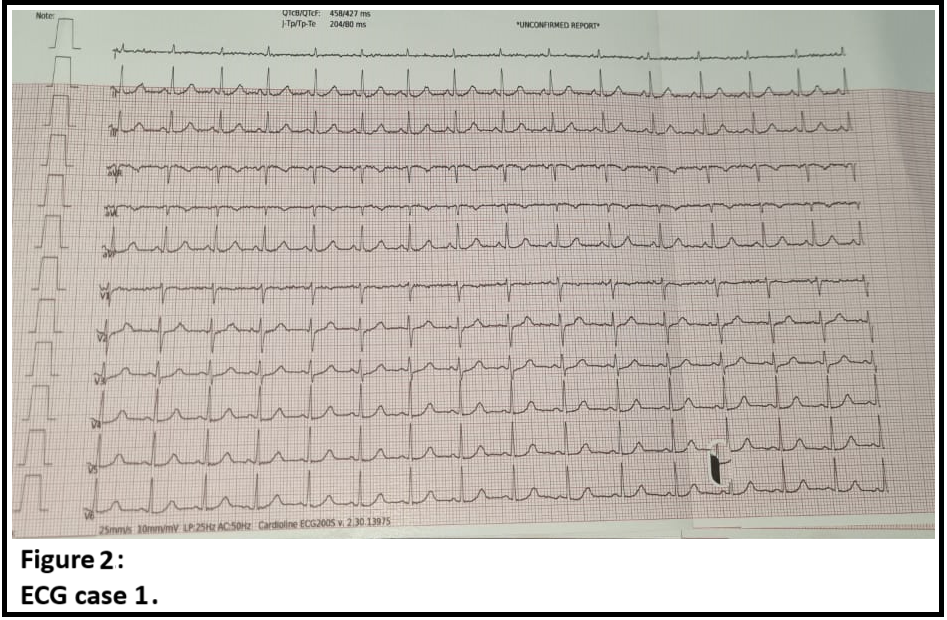
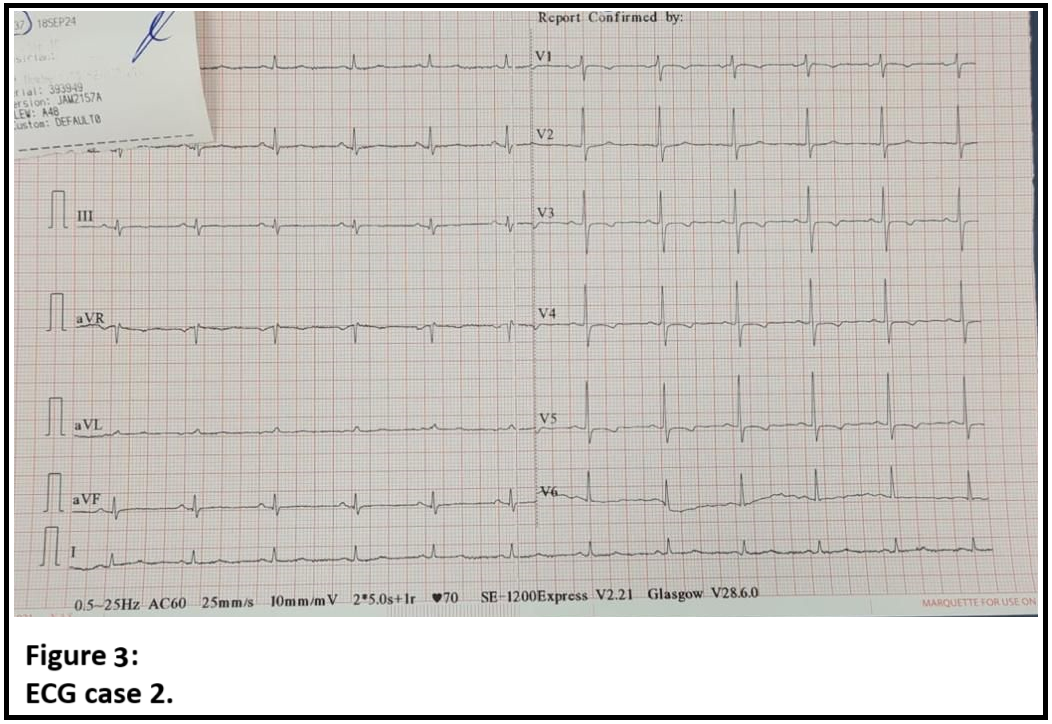
Case 1 :A 29-year-old woman without cardiovascular risk factors (CVRF) was admitted with CCS class III angina. Nine months previously, the patient had NSTEMI and coronary angiography then showed type 1 extensive spontaneous coronary artery dissection of the LAD with indication for medical treatment alone.Case 2 :A 38-year-old woman with no CVRF was admitted with high-risk NSTEMI.Case 3 :A 46-year-old man with no CVRF was admitted with very high-risk NSTEMI because of persistent chest pain.
Relevant Test Results Prior to Catheterization
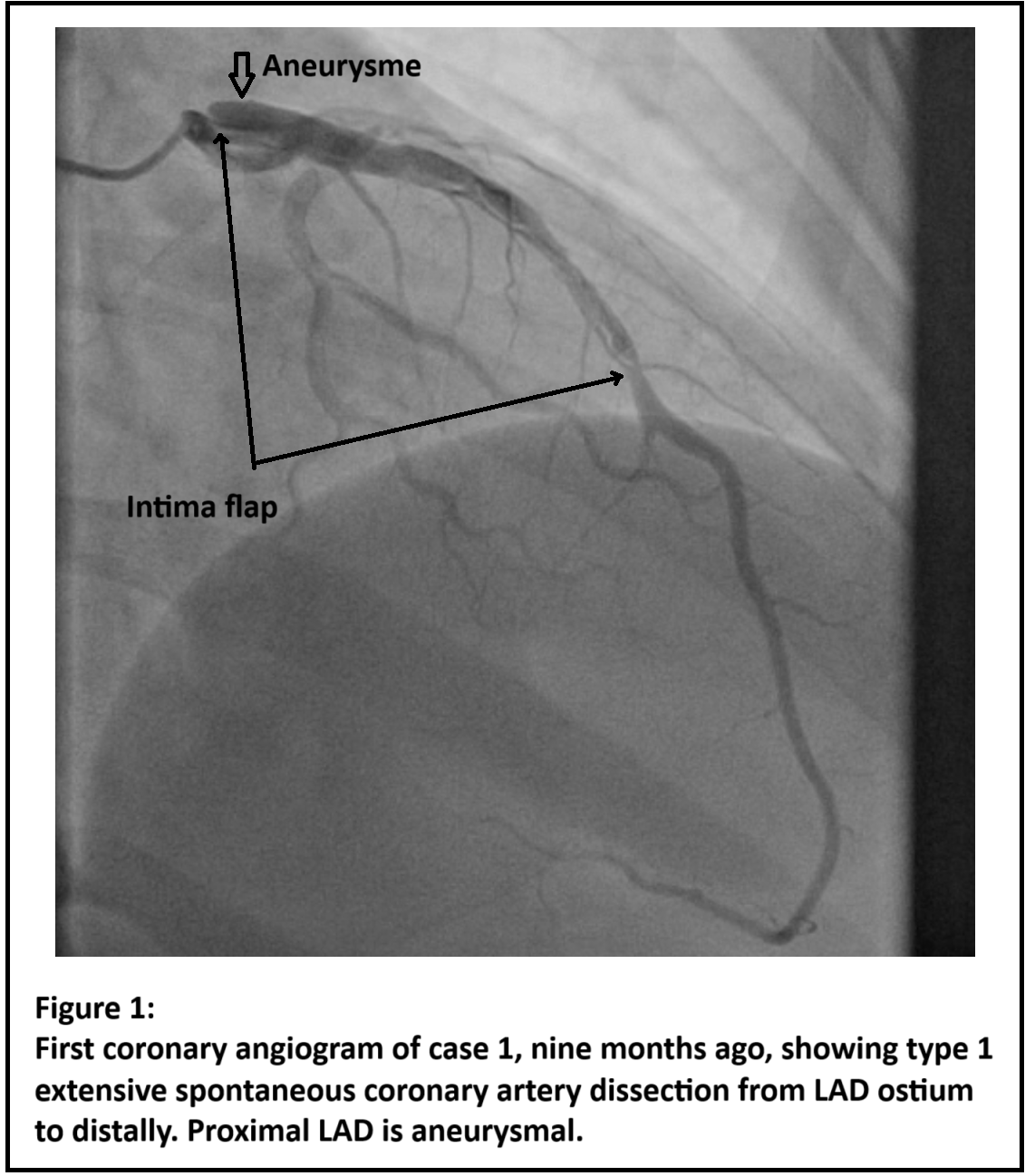
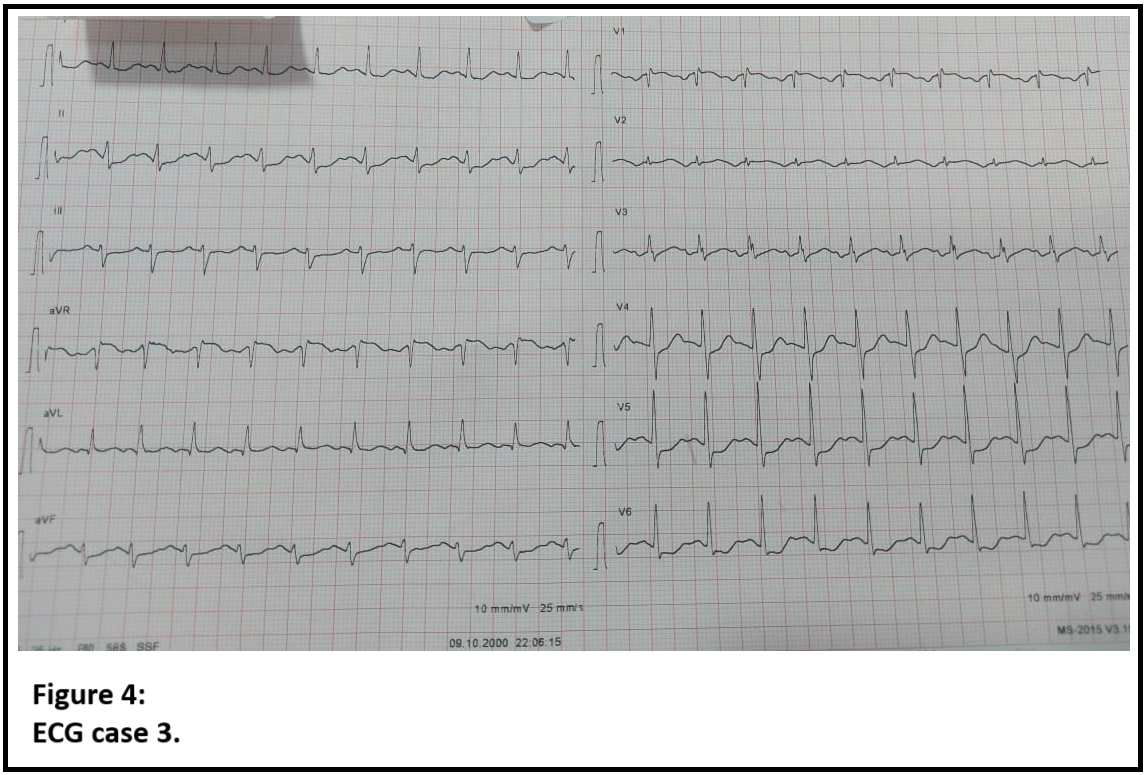
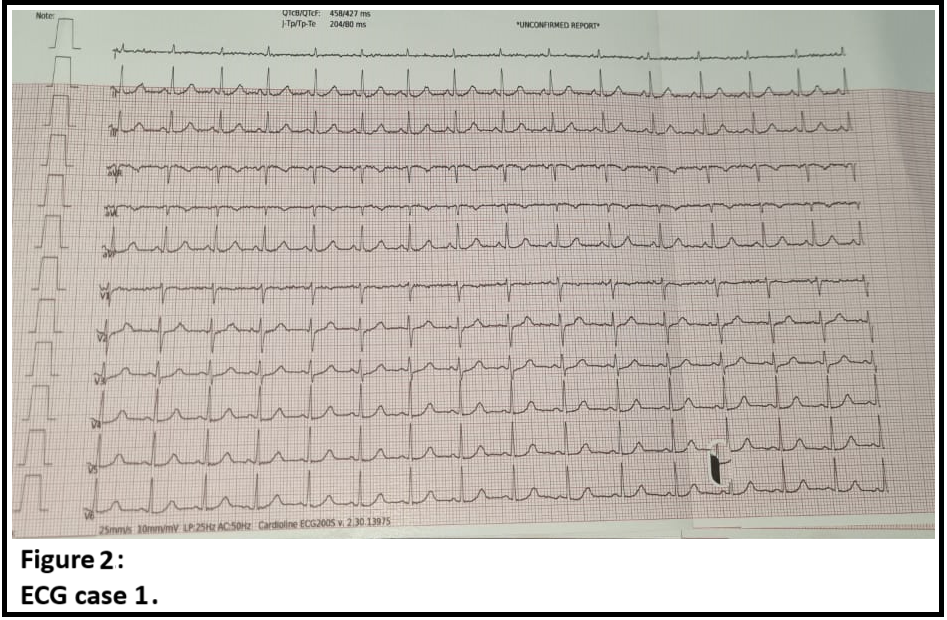
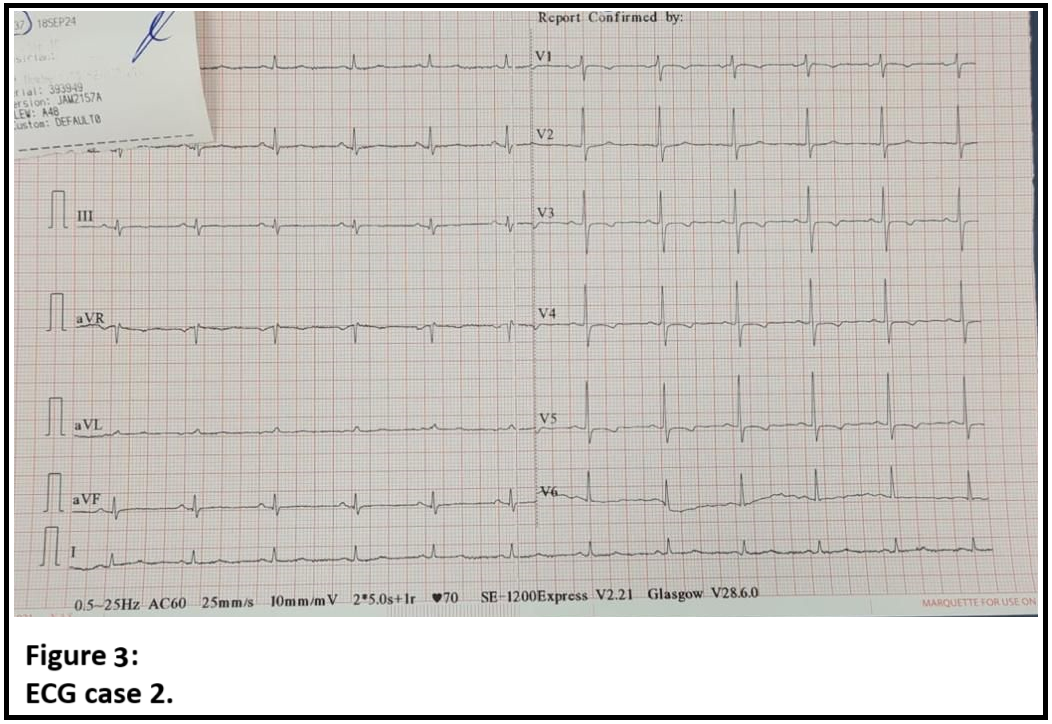
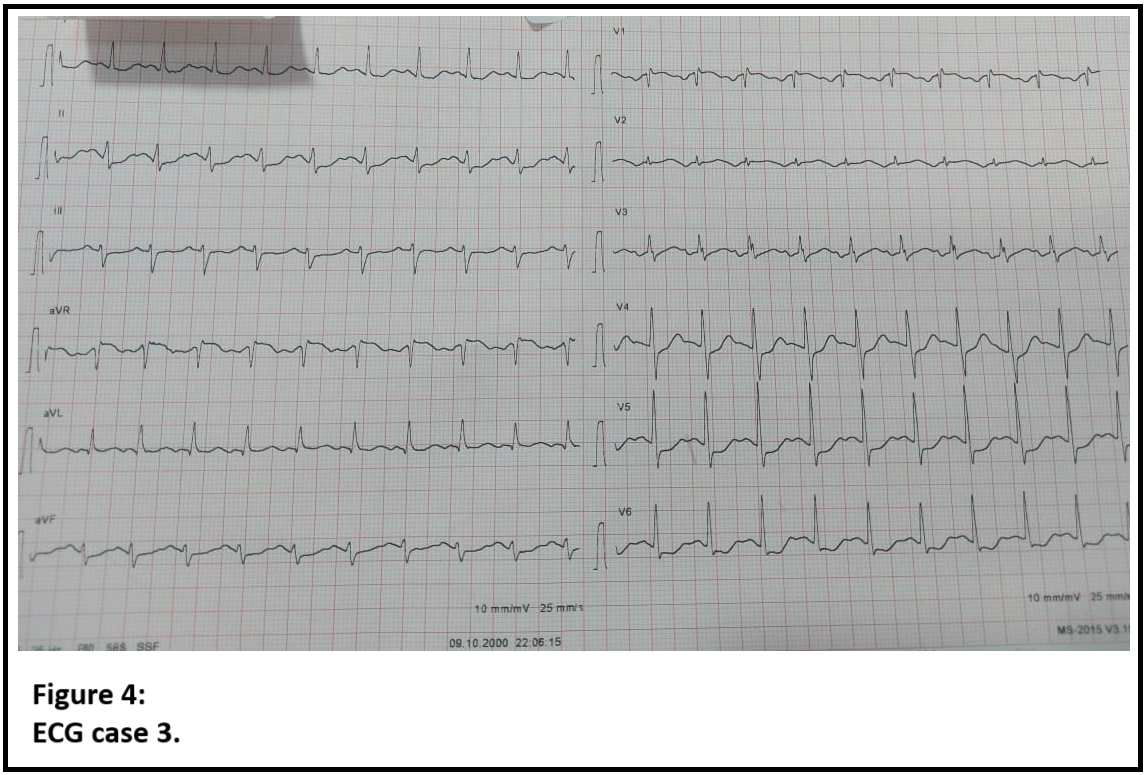
Case 1:Physical examination was normal with an unremarkabl ECG. Myocardial perfusion imaging showed severe ischemia in 5 segments, corresponding to LAD territory.Case 2:The patient presented with typical chest pain and T wave inversion on the anterior ECG leads. Troponin I levels increased from 0.12 ng/ml to 0.93 ng/ml within a 2-hour interval.Case 3:The patient presented with severe persistent chest pain. ECG showed ST segment elevation in aVR lead and ST segment depression in the other leads.
Relevant Catheterization Findings
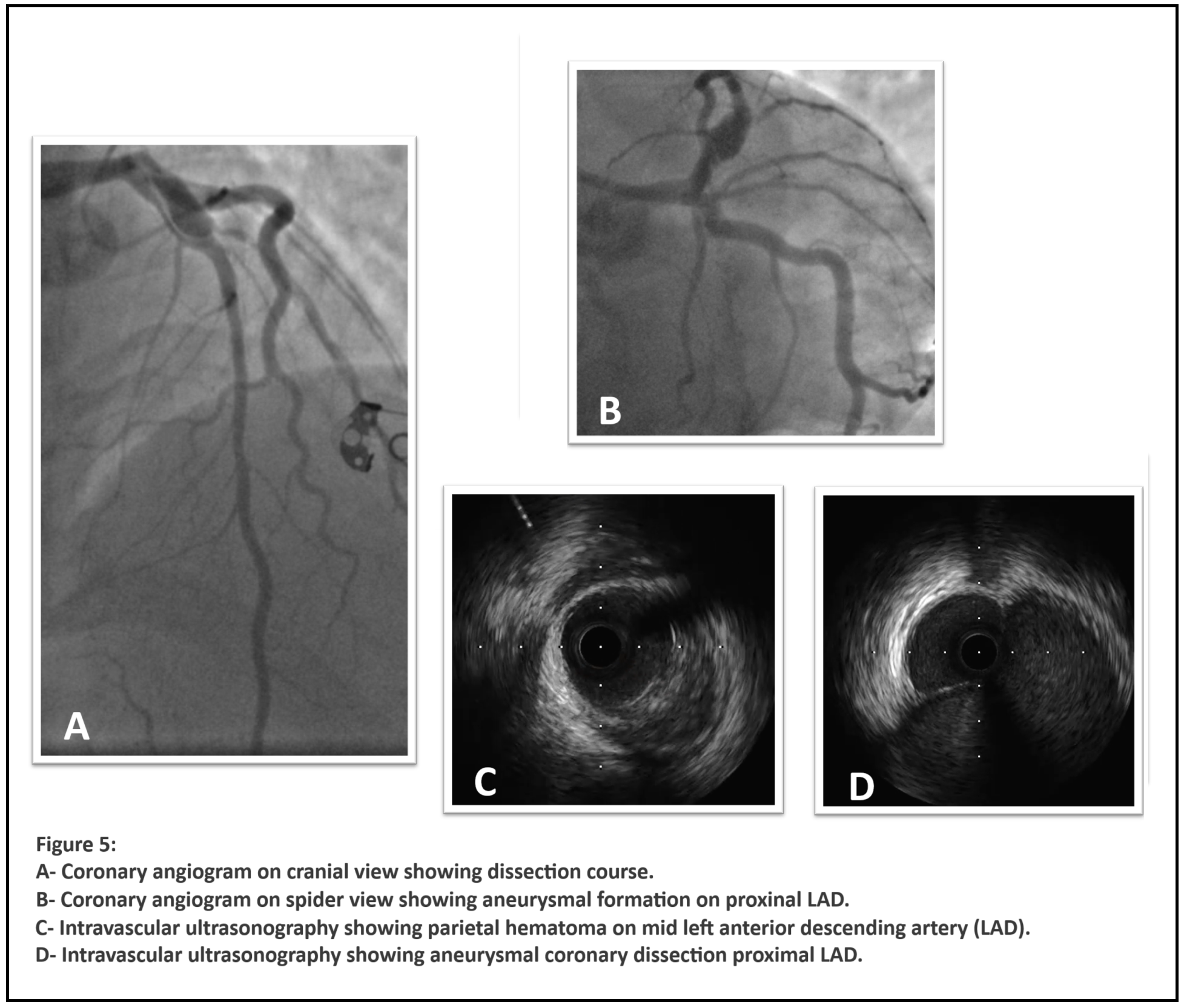
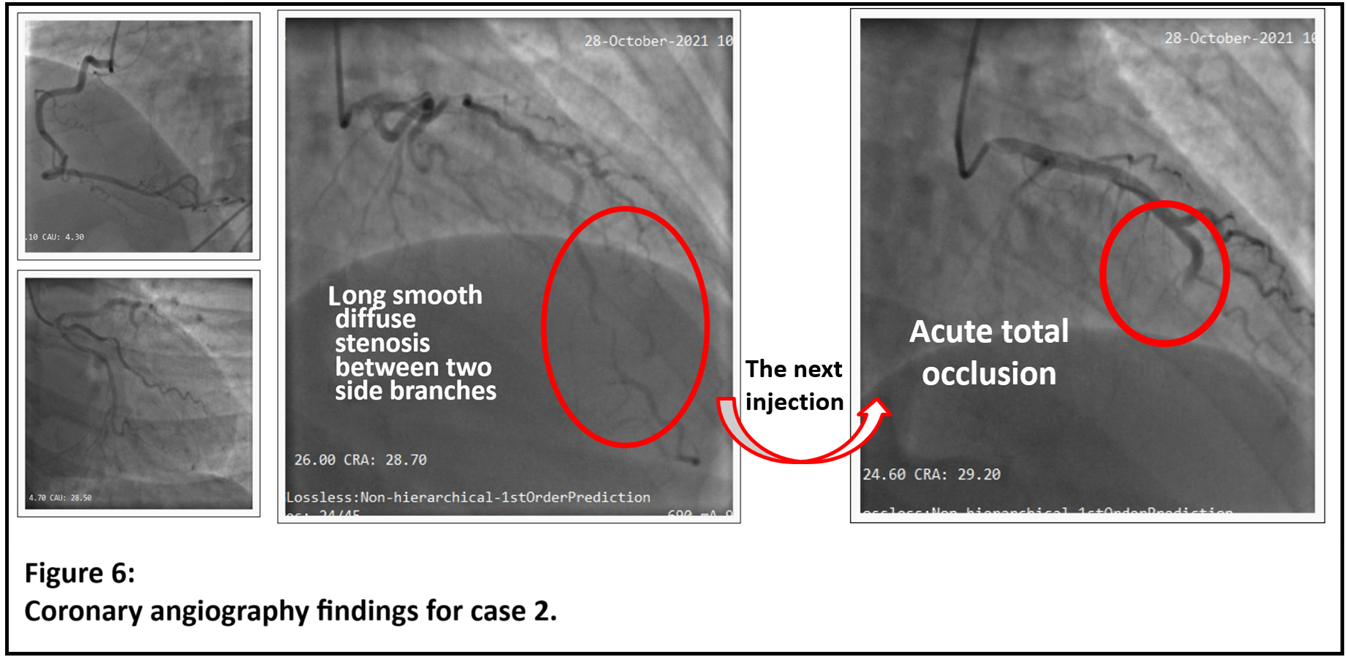
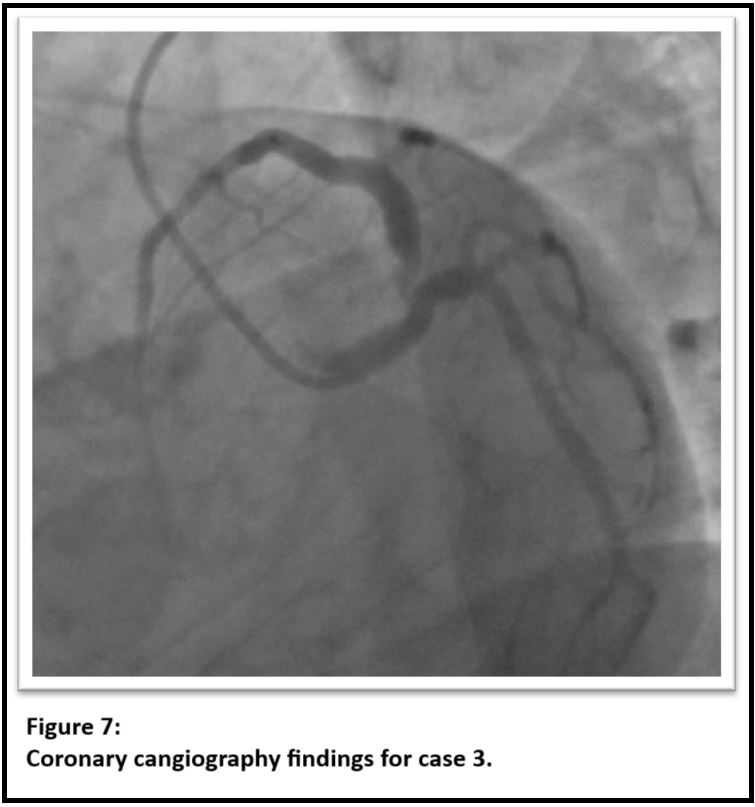
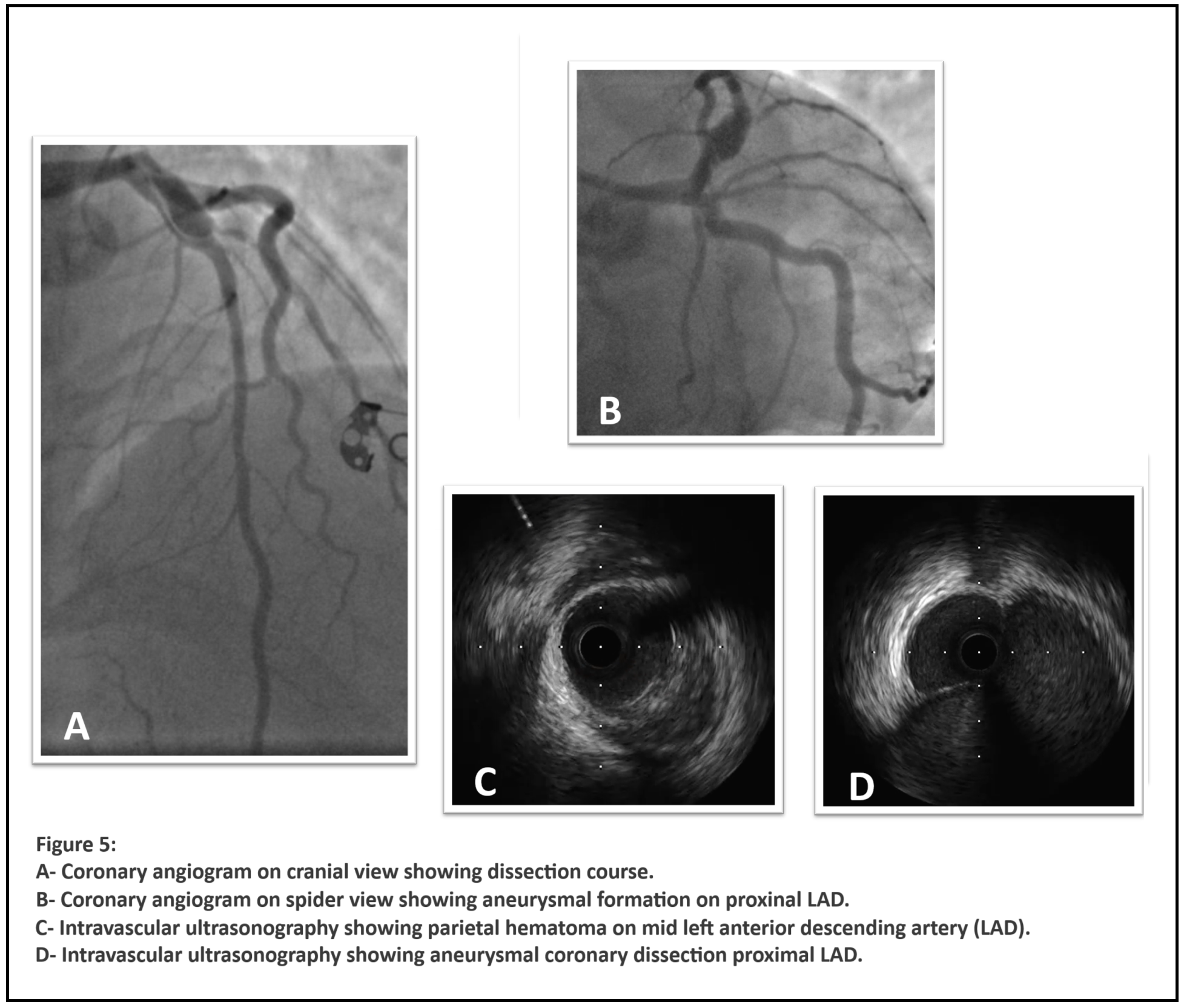
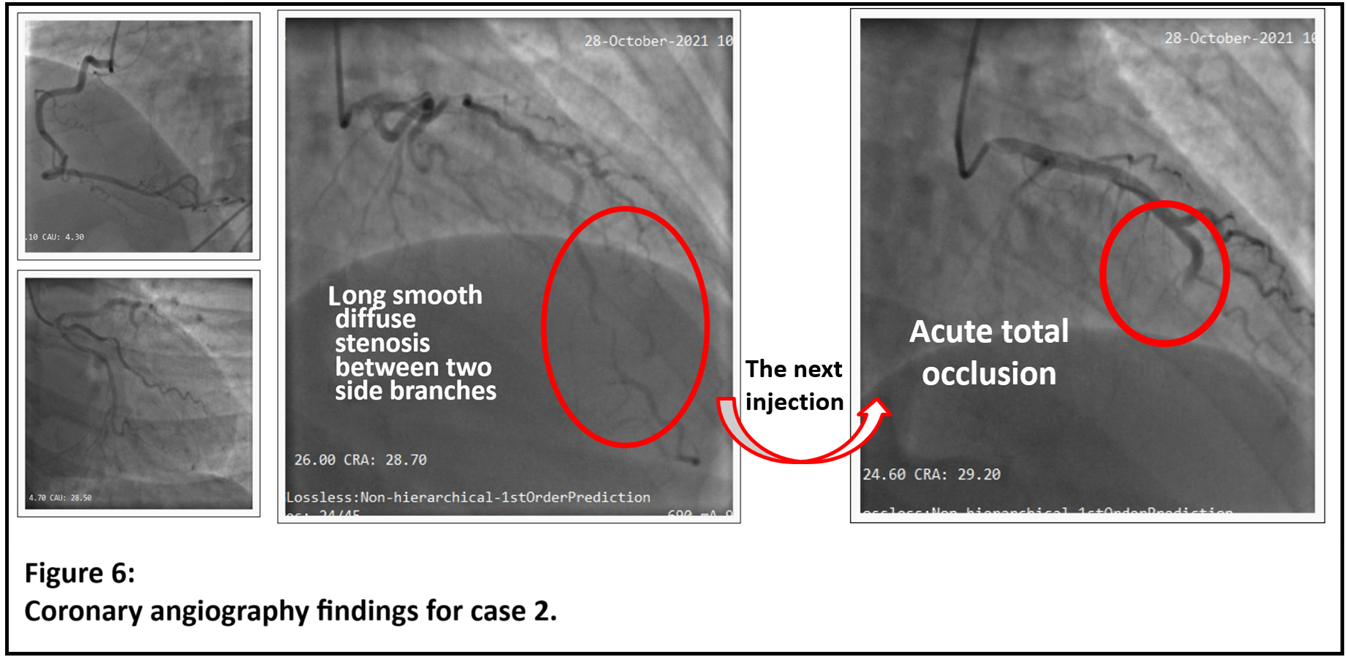
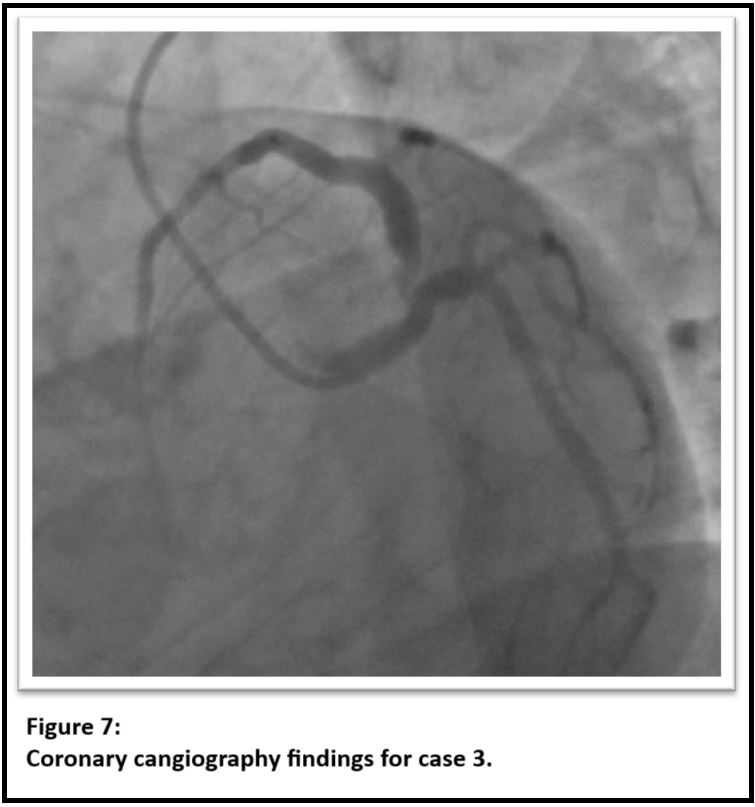
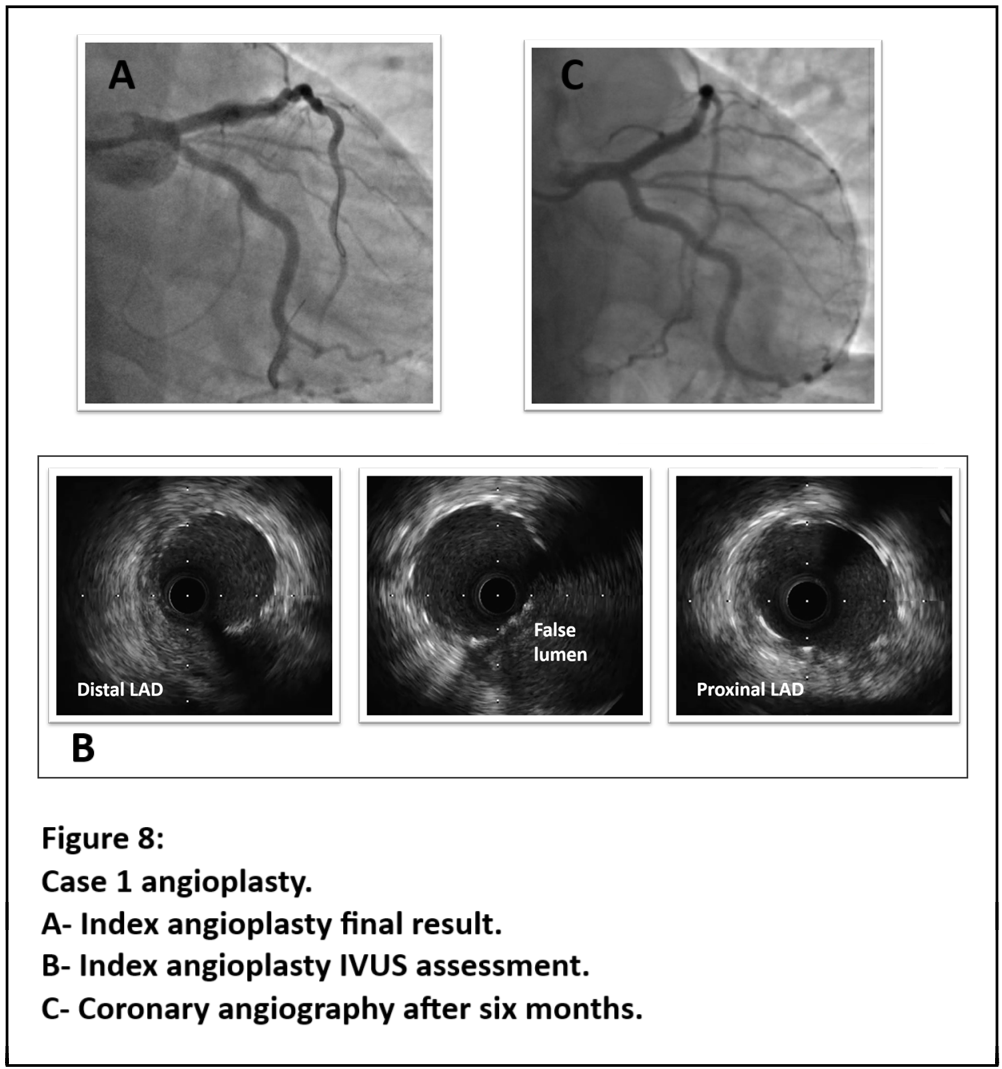
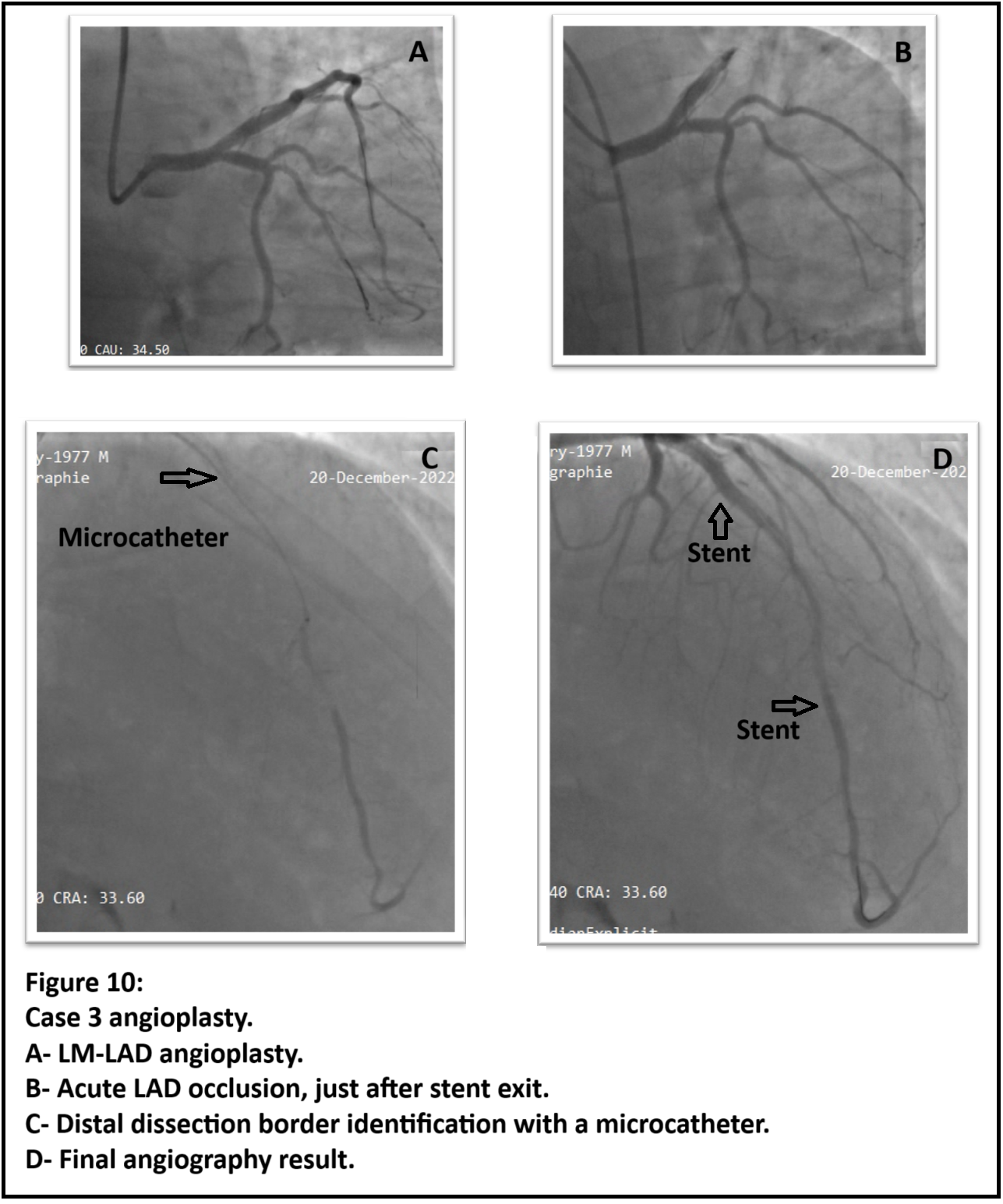
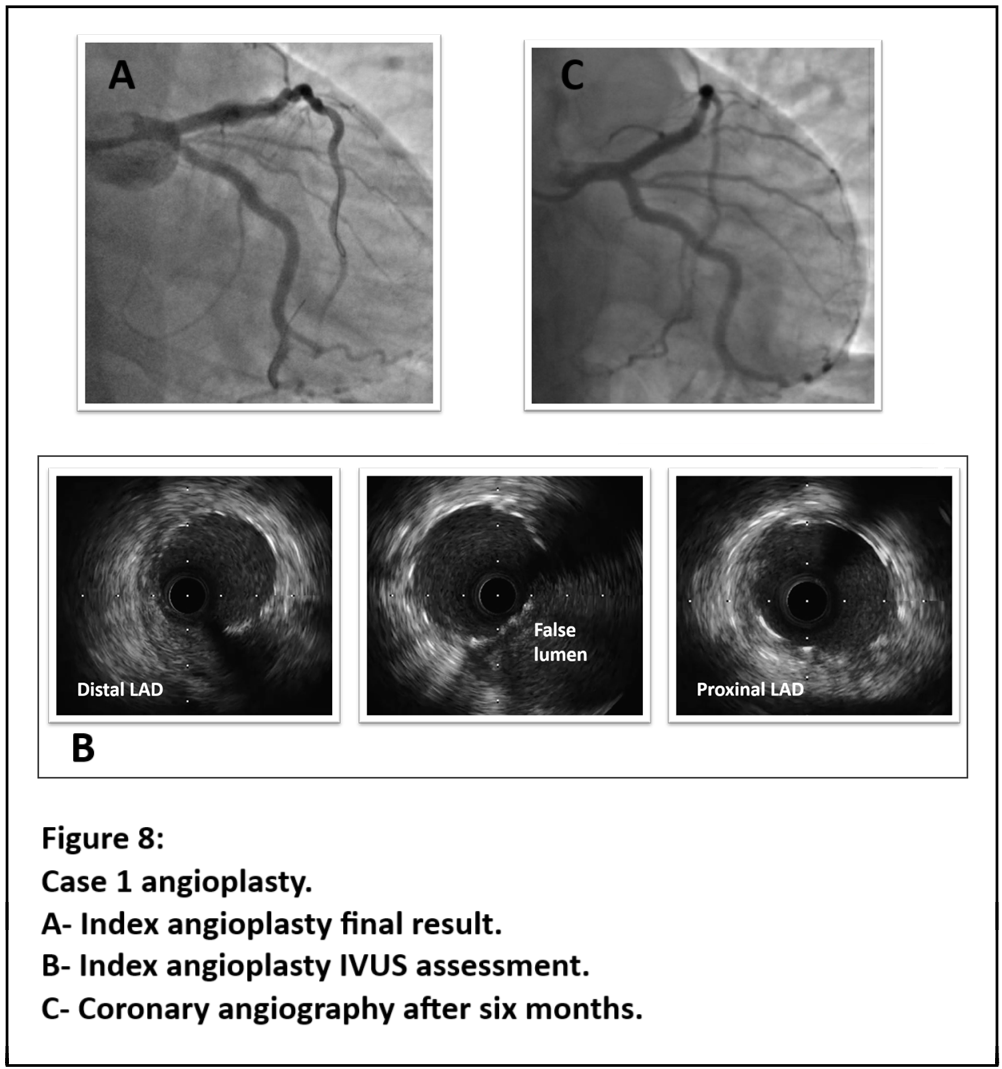
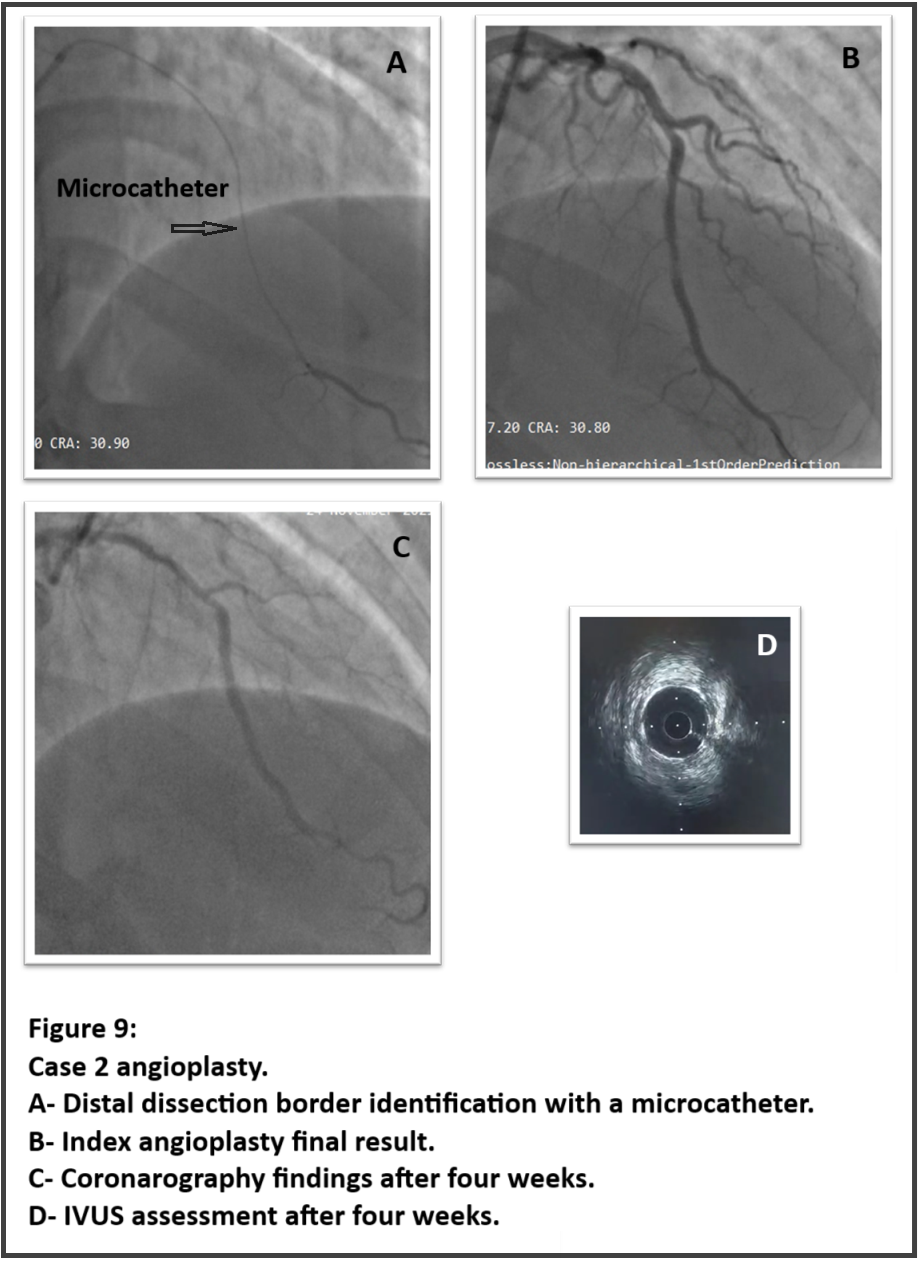
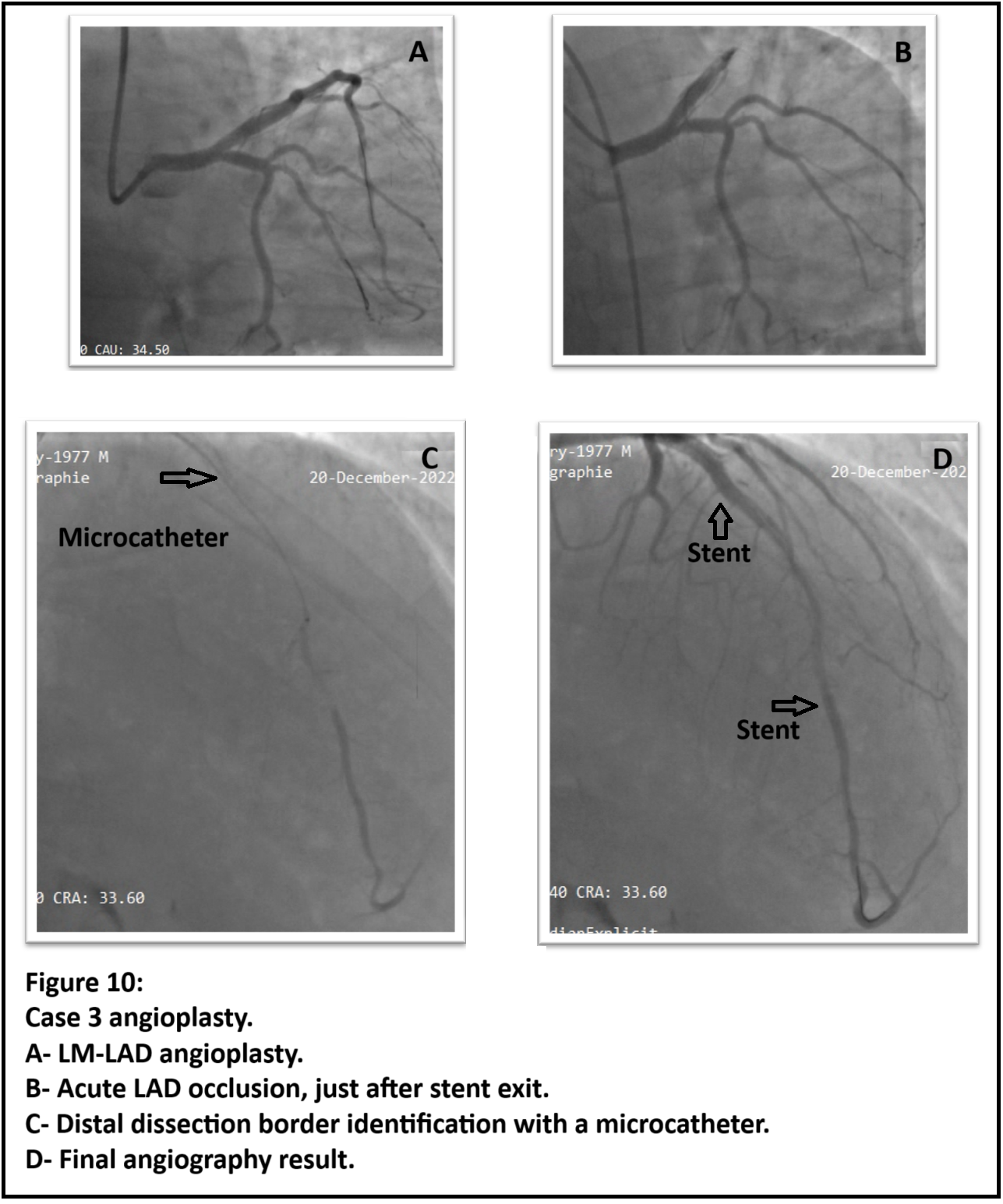
Case 1 :Dissection regression towards mid LAD. The proximal aneurysmal formation slightly increased with severe ture lumen compression.IVUS assessment showed intra parietal hematoma with positive remodeling up to mid LAD. False lumen was aneurysmal, compressing the true lumen. LAD ostium was unaffected.Case 2 :Smooth severe narrowing between two septal branches on mid LAD. Second contrast injection conducted to totale LAD occlusion.Case 3 :Isolated severe short subocclusion of ostial LAD.
Interventional Management
Procedural Step
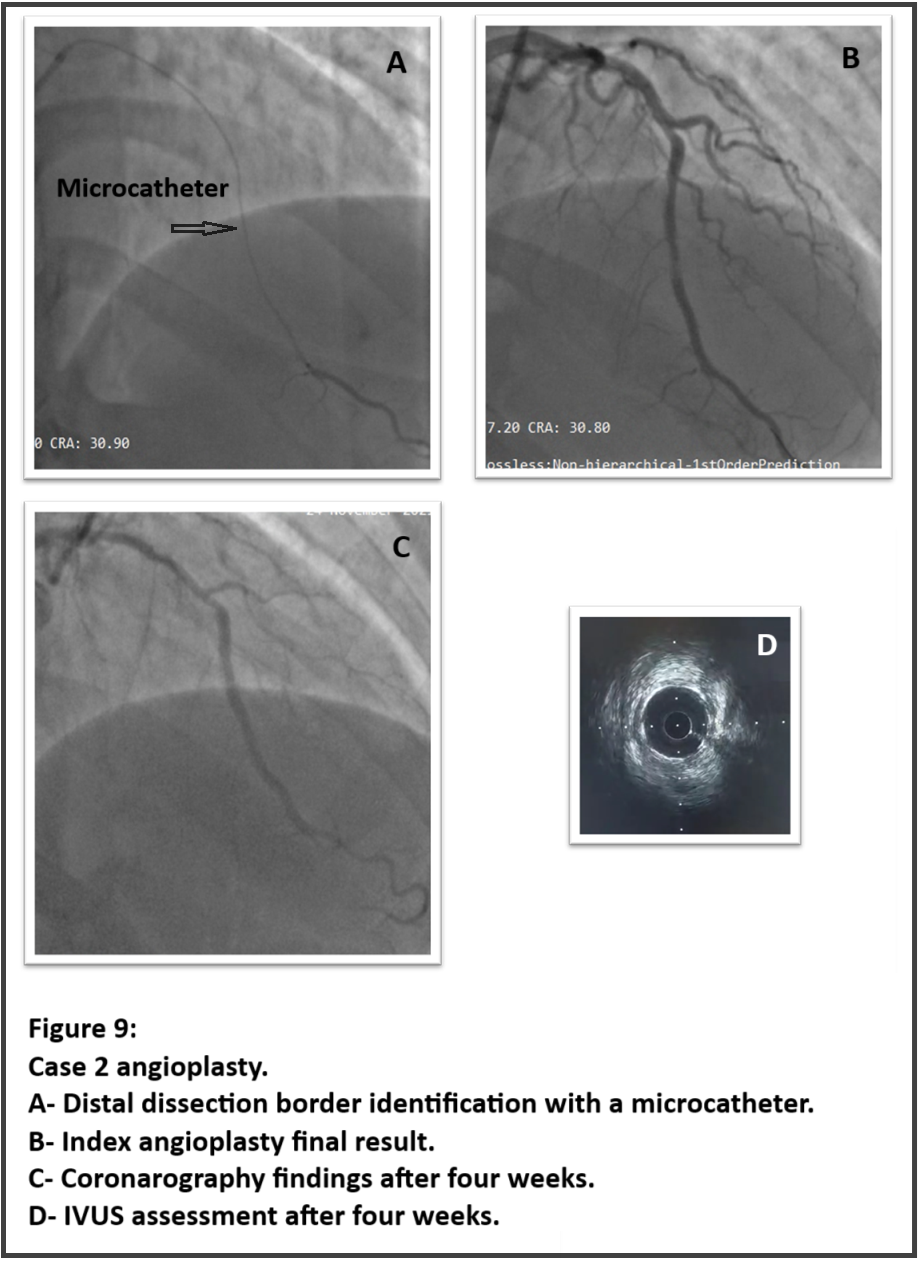
Case 1:An IVUS-guided stent was implanted on the proximal LAD. Final IVUS assessment showed good stent deployment with a reduced false lumen diameter suggesting filling restriction.After six months, an angiography control for atypical chest pain showed a patent stent and complete aneurysm resolution.Case 2:Balloon dilation failed to restore coronary flow. Rather than using endovascular imaging which might have worsened the situation, we injected contrast distally through a microcatheter. In doing so, we identified dissection extension and two stents were deployed with initial succes.One hour later, the patient was referred back to cath lab for acute stent thrombosis. TIMI III flow was achieved after balloon post-dilation and thromaspiration. Angiographic control with IVUS assessment four weeks later showed excellent stent deployment, no gap between the two stents and coronary healing.Case 3:Initially, we successfully implanted a stent from LM to LAD with provisional stenting technique.After two hours, the patient presented an acute thrombosis at the stent exit. After balloon dilation and a second stent implantation failed to restore flow, we used a microcatheter and had identified the LAD distally with angiographic aspect of coronary dissection. A short stent was deployed to seal the dissection distally and a SC balloon was used to fenestrate the hematoma. This successfully restored TIMI III flow.All three cases had excellent hospital outcomes with preserved EF at discharge.
Case Summary
PCI in patients with spontaneous coronary dissection carries several risks such as extension of hematoma and coronary dissection, false lumen wiring, acute vessel occlusion and stent thrombosis. The main objective of revascularization in spontaneous coronary artery dissection is not to restor coronary anatomy but rather to ensure adequate coronary flow. Reaching this goal, intravascular imaging remains the gold standard to identify coronary artery dissection, its extension, and guid eangioplasty. Careful injection through a microcatheter seems to be a good alternative achieving a secure guided angioplasty in such high risk situations.


