Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-022
Recurrent Ventricular Tachycardia in Acute Inferior ST-Segment Elevation With Dominant Left Circumflex Artery Occlusion
By Evi Supriadi Sukardi, Hernina Oktaviani
Presenter
Evi Supriadi Sukardi
Authors
Evi Supriadi Sukardi1, Hernina Oktaviani2
Affiliation
RSUD Raden Mattaher Hospital, Indonesia1, RSUD H. Abdurrahman Sayoeti, Indonesia2,
View Study Report
TCTAP C-022
Coronary - ACS/AMI
Recurrent Ventricular Tachycardia in Acute Inferior ST-Segment Elevation With Dominant Left Circumflex Artery Occlusion
Evi Supriadi Sukardi1, Hernina Oktaviani2
RSUD Raden Mattaher Hospital, Indonesia1, RSUD H. Abdurrahman Sayoeti, Indonesia2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
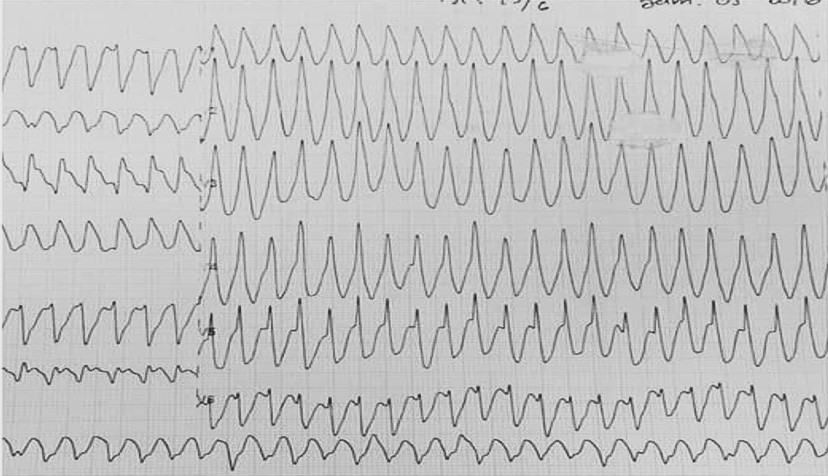
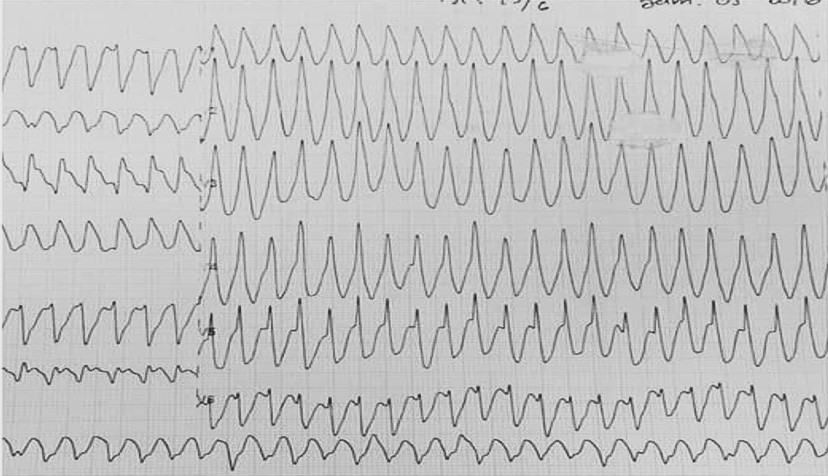
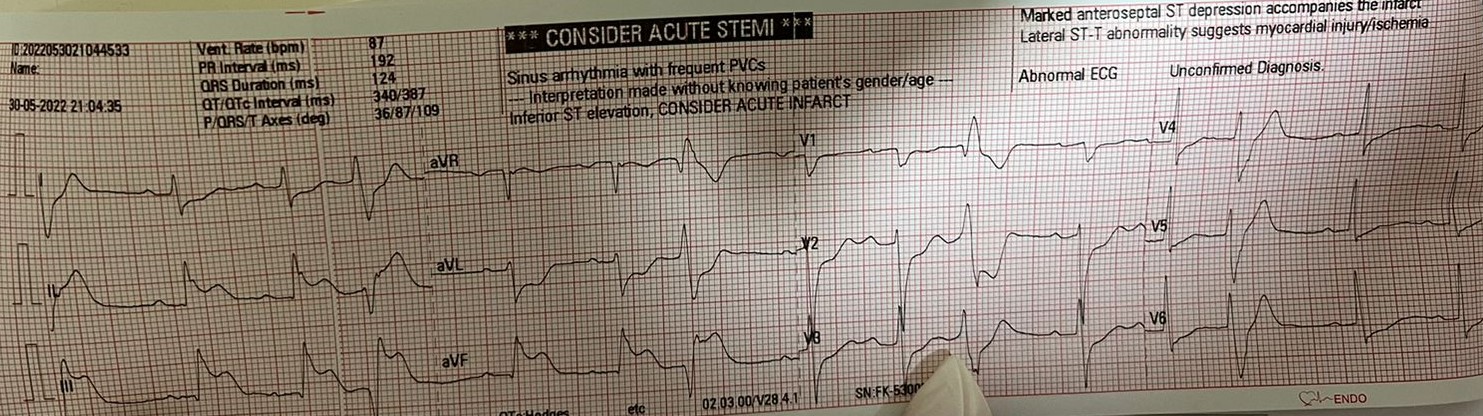
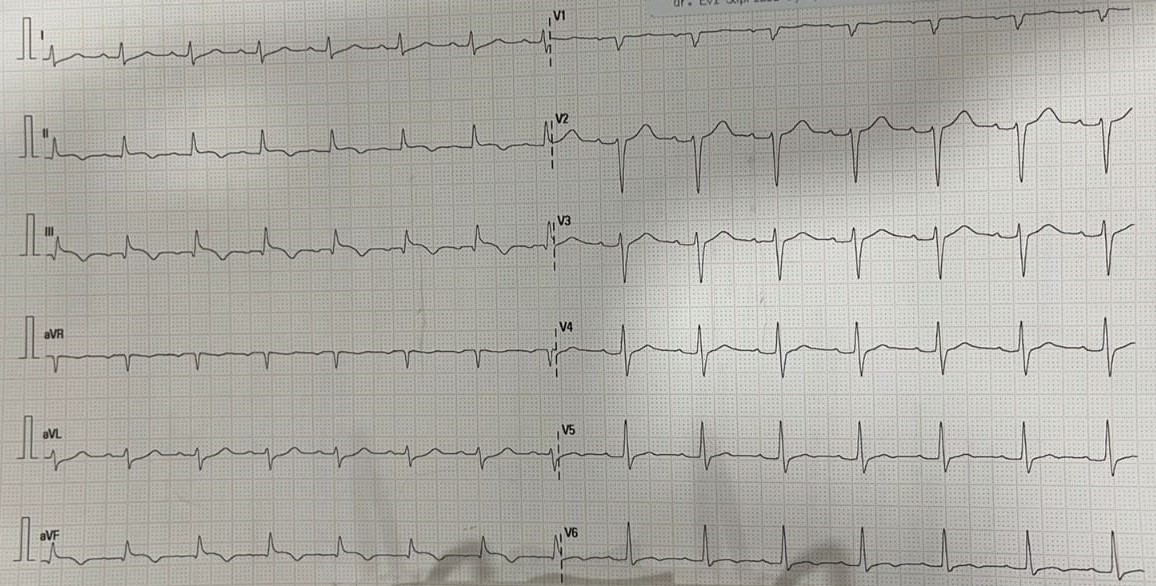
A 68-year-old man came to the emergency department with palpitation, chest pain and diaphoresis for more than 20 minutes. Six months previously he complained of chest pain triggered by exercise, subsided by rest. There is history of metabolic syndrome and smoking. Heart rate is 200 bpm, regular; respiration rate 28 breaths/minute, pulse oximetry 97% with room air and otherwise normal findings upon physical examination. ECG showed Ventricular tachycardia (VT).
Relevant Test Results Prior to Catheterization
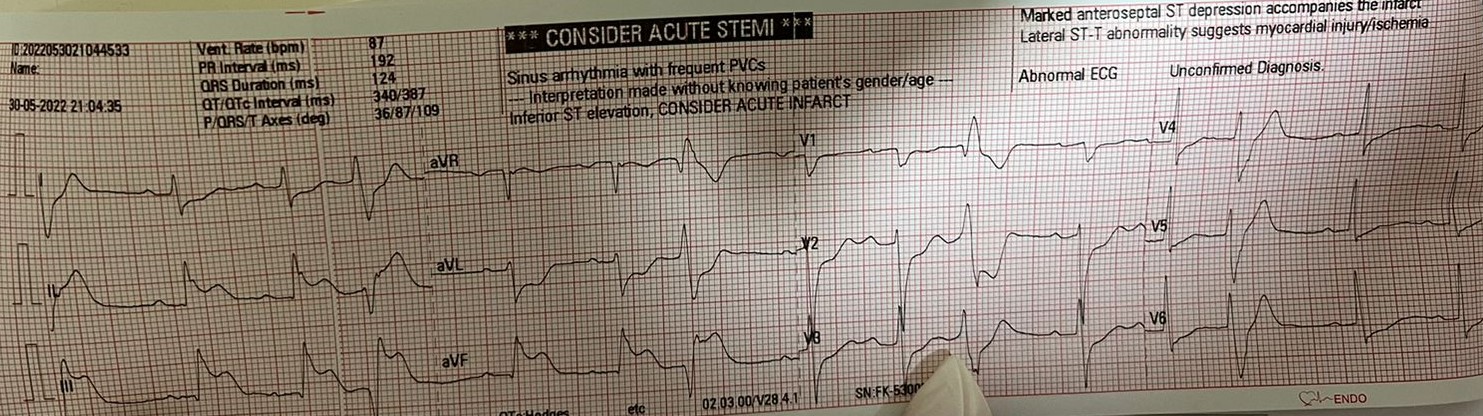
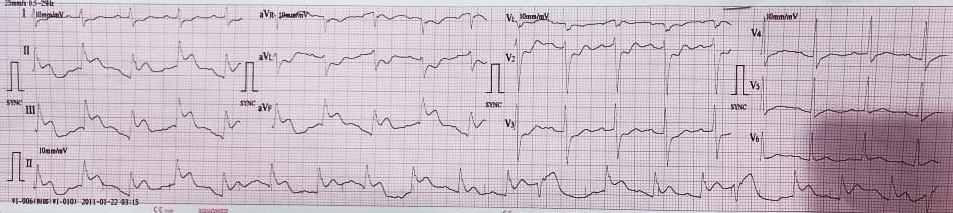
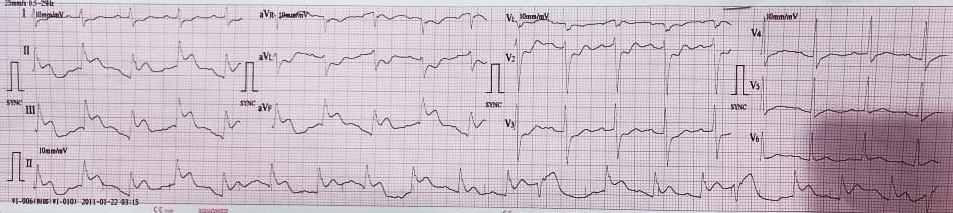
ECG showed VT, synchronized cardioversion of 100 joule was given. Follow-up ECG later showed ST segment elevation in inferior leads, more elevated in lead III than lead II. Loading Aspirin and P2Y12 inhibitor to initial management of STEACS. Shortly after, patient experienced seizures and ECG monitoring showed Ventricular Fibrillation (VF); DC shock of 200 joules was given. Patient was later treated for STEACS and prepared for primary percutaneous coronary intervention (PCI).
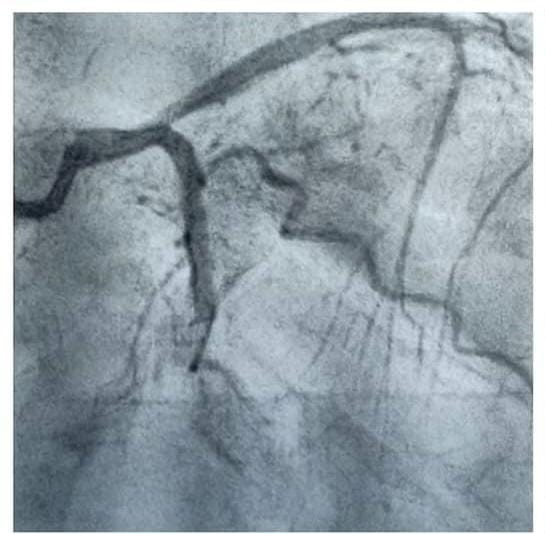
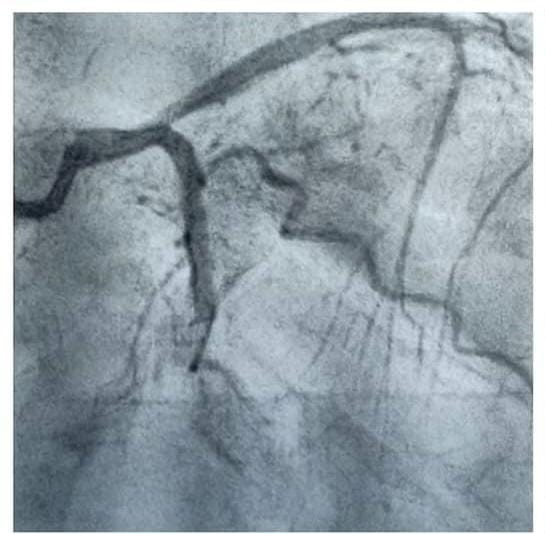
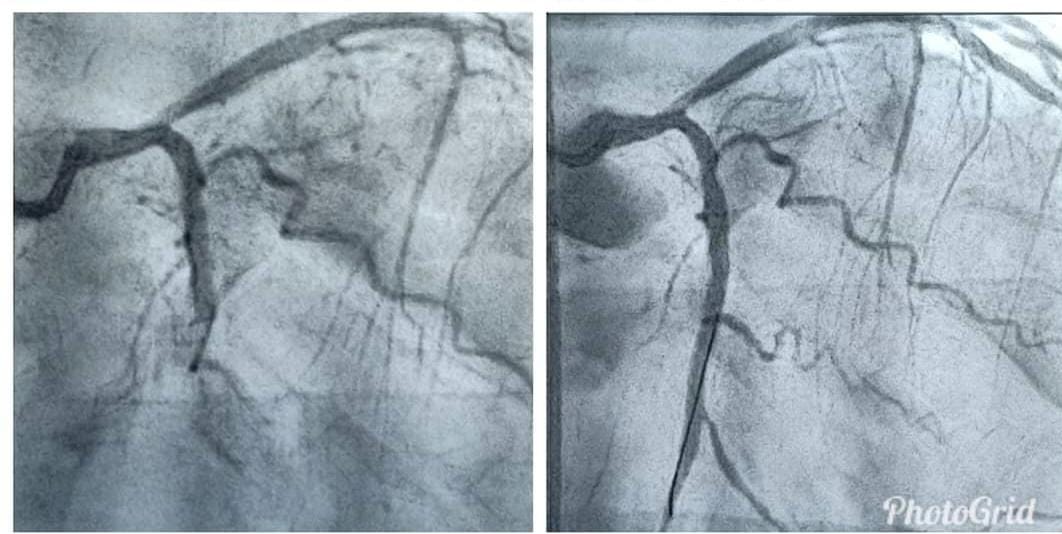
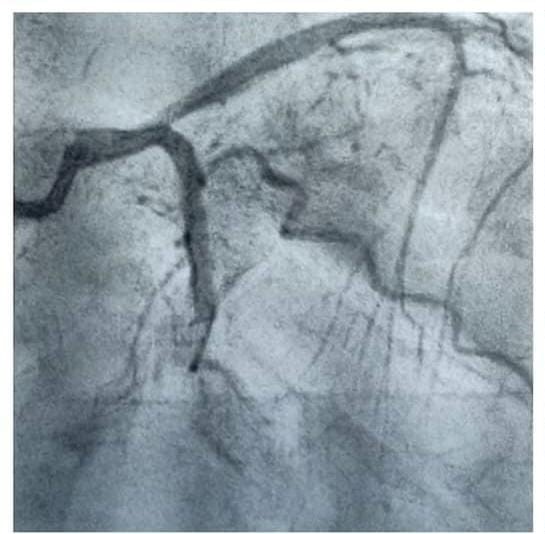
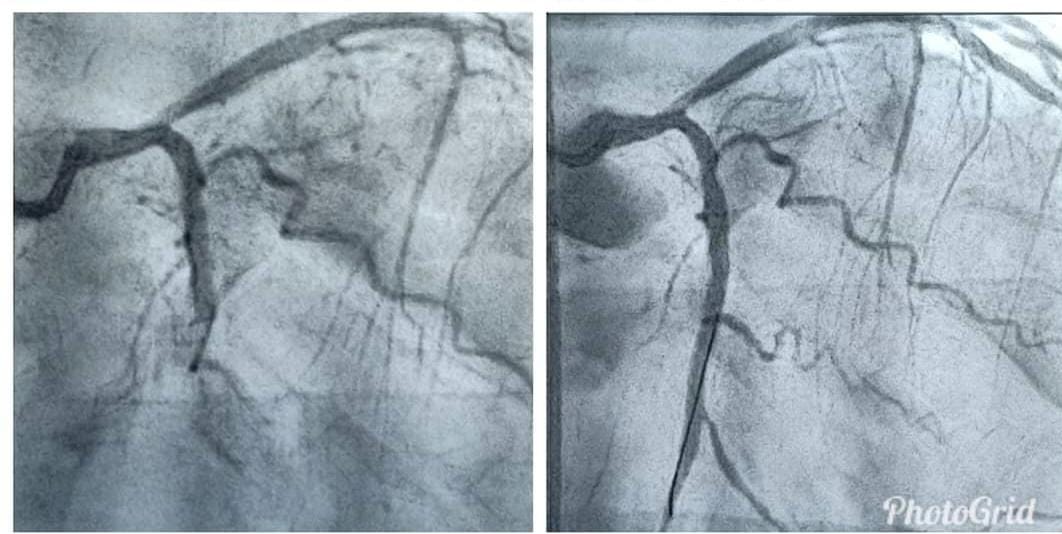
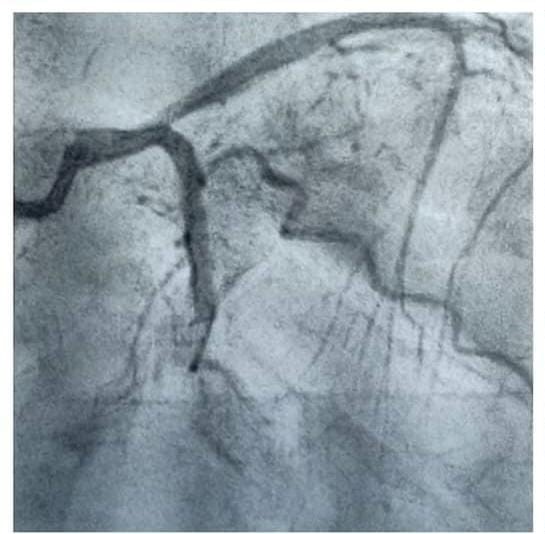
Relevant Catheterization Findings
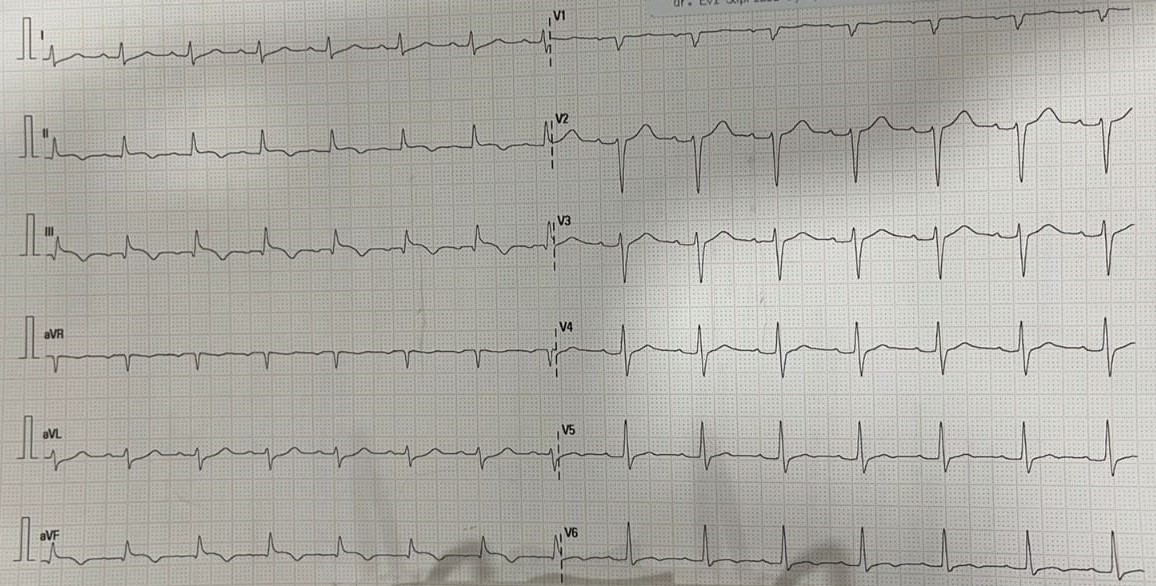
Total occlusion was found in LCx. RCA was normal. Synchronized cardioversion was subsequently performed seven times due to recurrent VT during intervention. After revascularization, patient had no symptoms, ECG revealed sinus rhythm. Echocardiography revealed LV dilatation, mild MR, EF 46% with hypokinetic in infero-posterior and akinesis in apical segment. After six days of optimal treatment in ICCU, patient was discharged with routine medication.


Interventional Management
Procedural Step
Patient suffered recurrent VT pre and durante intervention several times. Cardioversion was performed about 8 times to convert to sinus rhythm. PCI was performed using sheath 6F via trans-femoral dextra and showed tortuous Iliaca-femoral artery dextra. Second attempt of canulation was successfully performed using sheath 6F via trans-femoral sinistra to RCA. RCA was normal and non dominant. Canulation in LCx showed total occlusion. We use two wire floopy to distal LCx and distal OM2. Pre-dillation was performed with balloon 2.0/15 and DES stent 2.75/28 mm was inserted in distal LCx. Final result, stent well-apposed, no complication, stable vital sign, TIMI flow III, and no dissection and perforation during the procedures.


Case Summary
In few cases, inferior STEACS can be caused by LCx occlusion instead of RCA occlusion. The most common rhythm found in the acute phase is polymorphic VT that degenerates to VF. Inferior ST-Segment Elevation Acute Coronary Syndrome (STEACS) is usually the result of right coronary artery (RCA) occlusion. Left circumflex artery (LCx) occlusion can also manifest as inferior STEACS, although less frequently, and with differing electrocardiogram (ECG) patterns. In both cases, polymorphic Ventricular Tachycardia (VT) can occur, and develop into Ventricular Fibrillation (VF).


