Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-011
Coronary Perforation During Primary PCI: Does Intrapericardial Tranexamic Acid Work?
By Dileep Tiwari
Presenter
Dileep Tiwari
Authors
Dileep Tiwari1
Affiliation
Baderia Metro Prime Hospital, India1,
View Study Report
TCTAP C-011
Coronary - Complication Management
Coronary Perforation During Primary PCI: Does Intrapericardial Tranexamic Acid Work?
Dileep Tiwari1
Baderia Metro Prime Hospital, India1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 58-year-old female with no prior history of diabetes Mellitus and hypertension, presented to the emergency room with a history of retrosternal chest pain, which was radiating to both shoulders for the last 10 hours duration. The pain was associated with profuse sweating and uneasiness. On examination, she was still in pain. She was conscious and oriented, her pulse rate was 70/min. BP was 114/70 mmHg, and SPO2 was 97% at room air. The systemic examination was unremarkable.
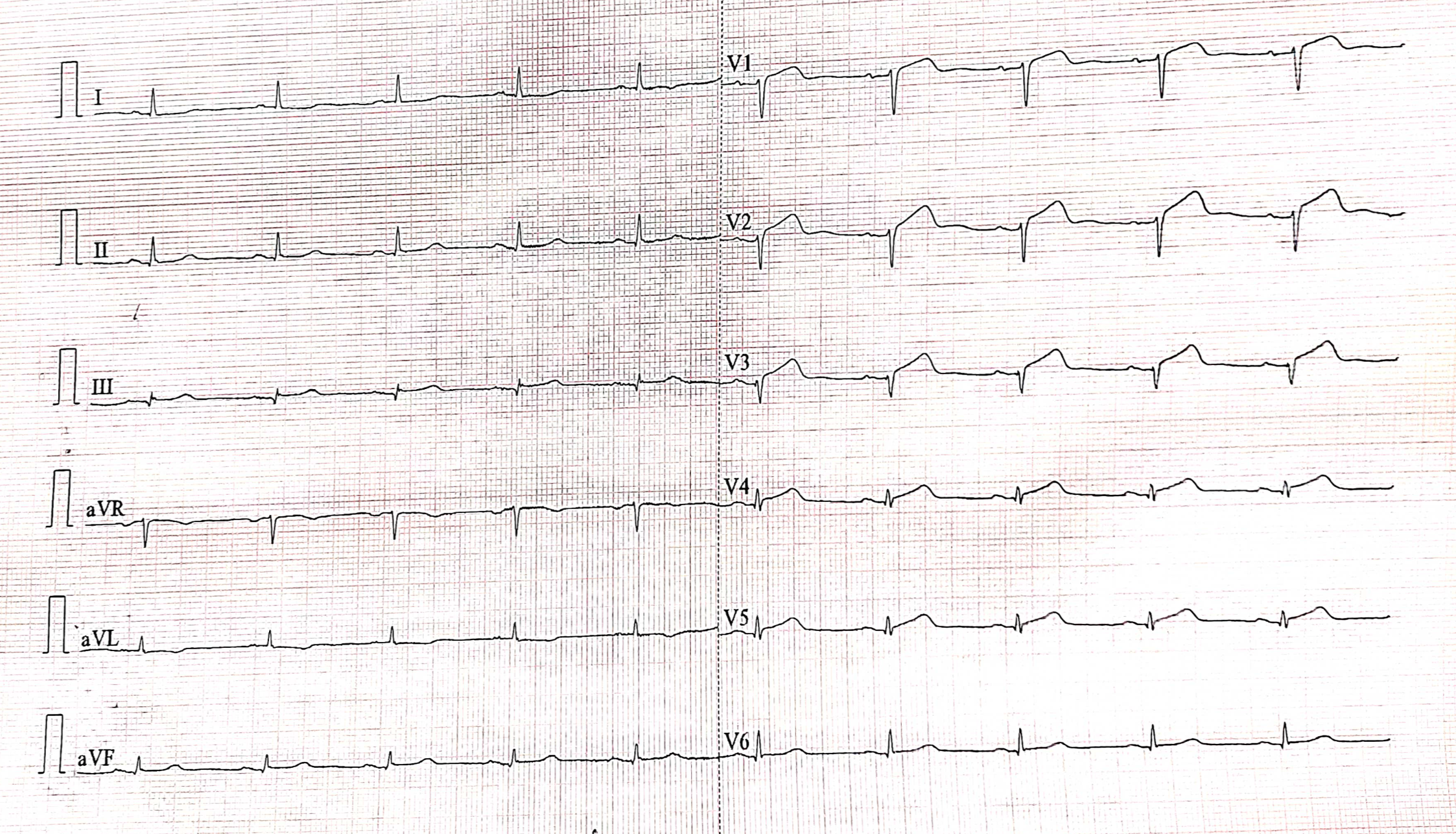
Relevant Test Results Prior to Catheterization
The ECG showed normal sinus rhythm with anterior wall STEMI. The echocardiogram revealed severely hypo-kinetic LAD territory and LVEF was 35%. All the laboratory parameters were within normal limits except troponin I, which was significantly raised. Other than the symptomatic treatment, the loading dose of Ticagrelor 180 mg, Disprin 325 mg, and Atorvastatin 80 mg was given in the emergency room. After taking written high-risk-informed consent, she was shifted to the catheterization laboratory.
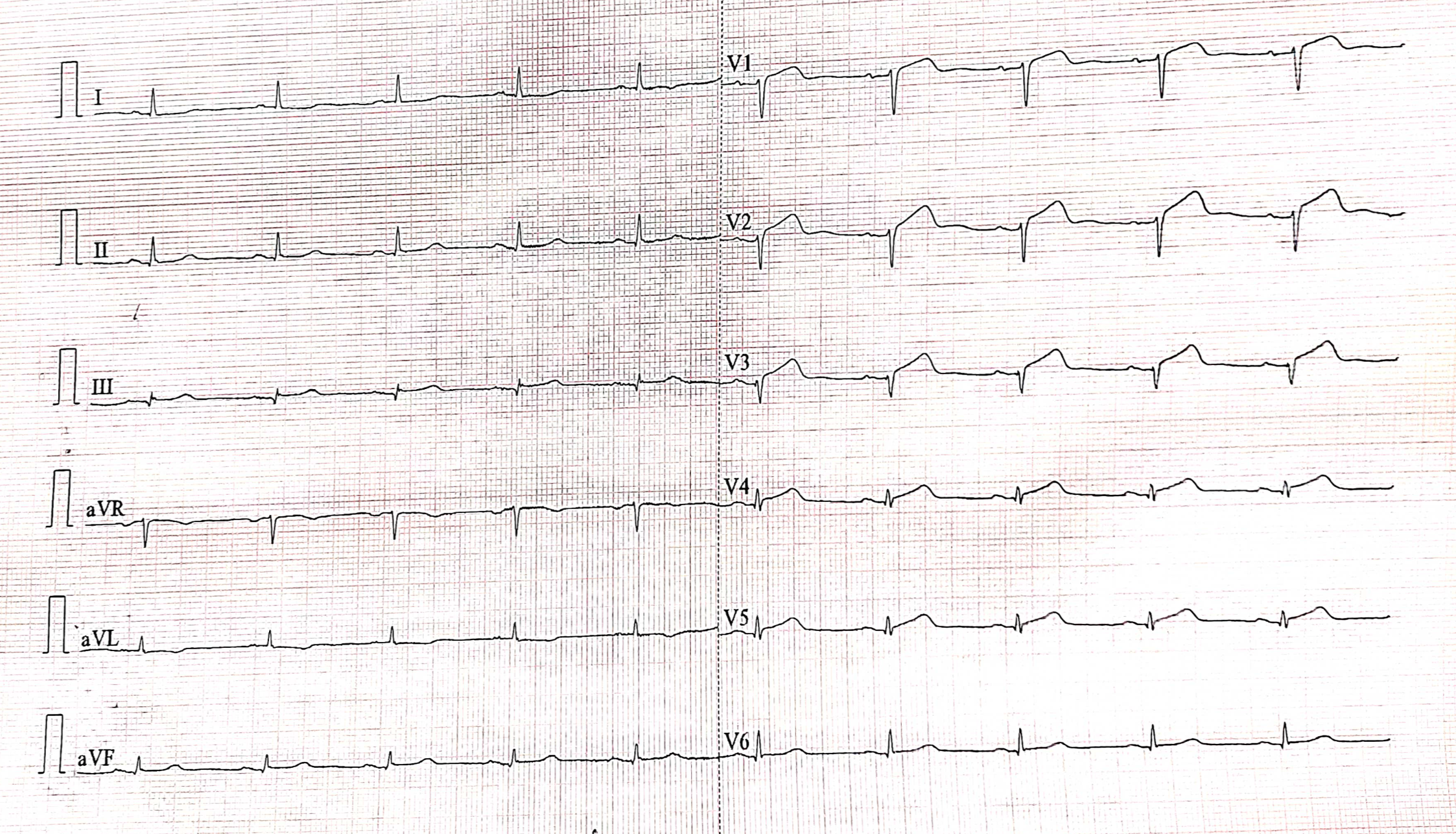
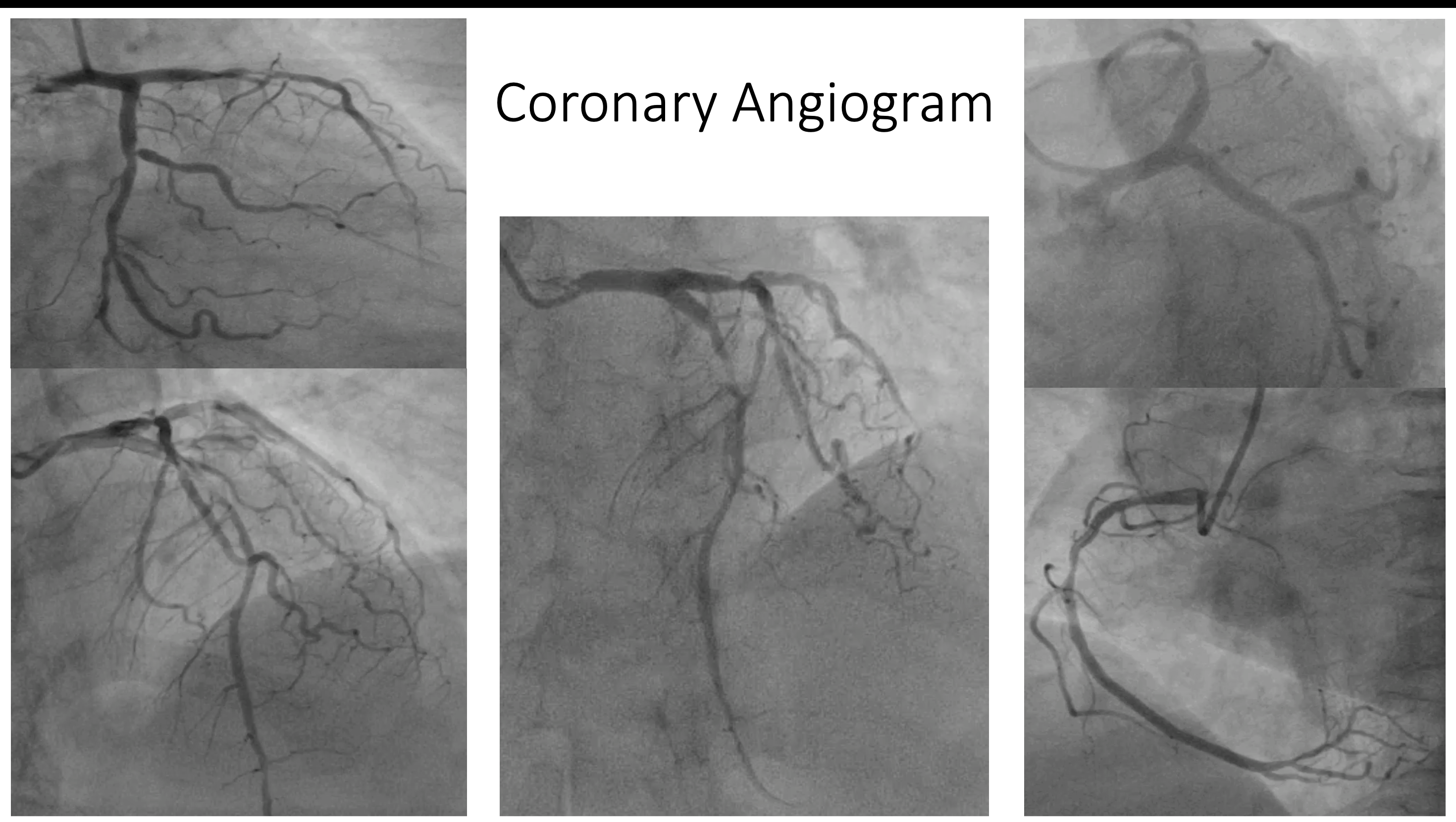
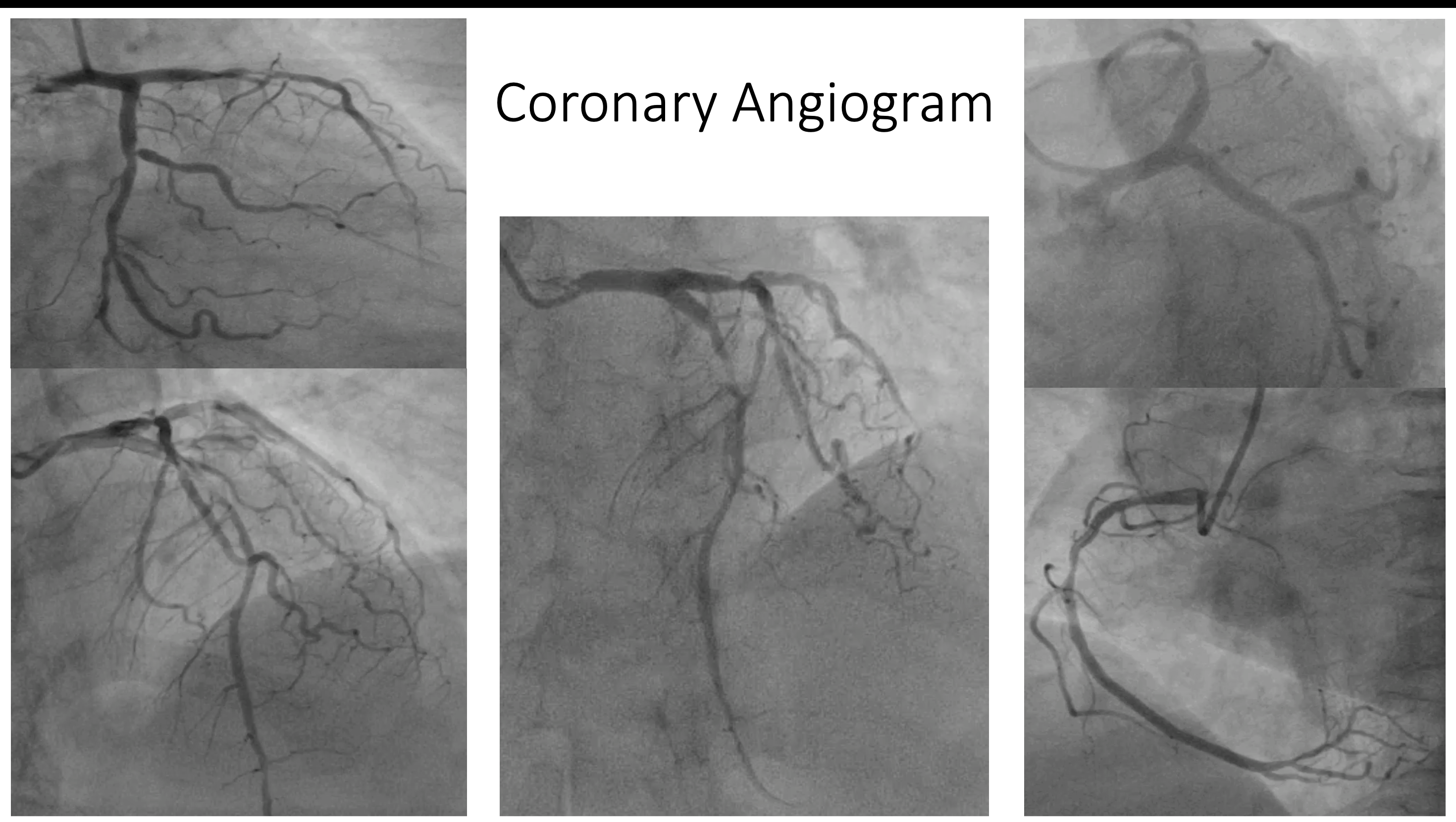
Relevant Catheterization Findings
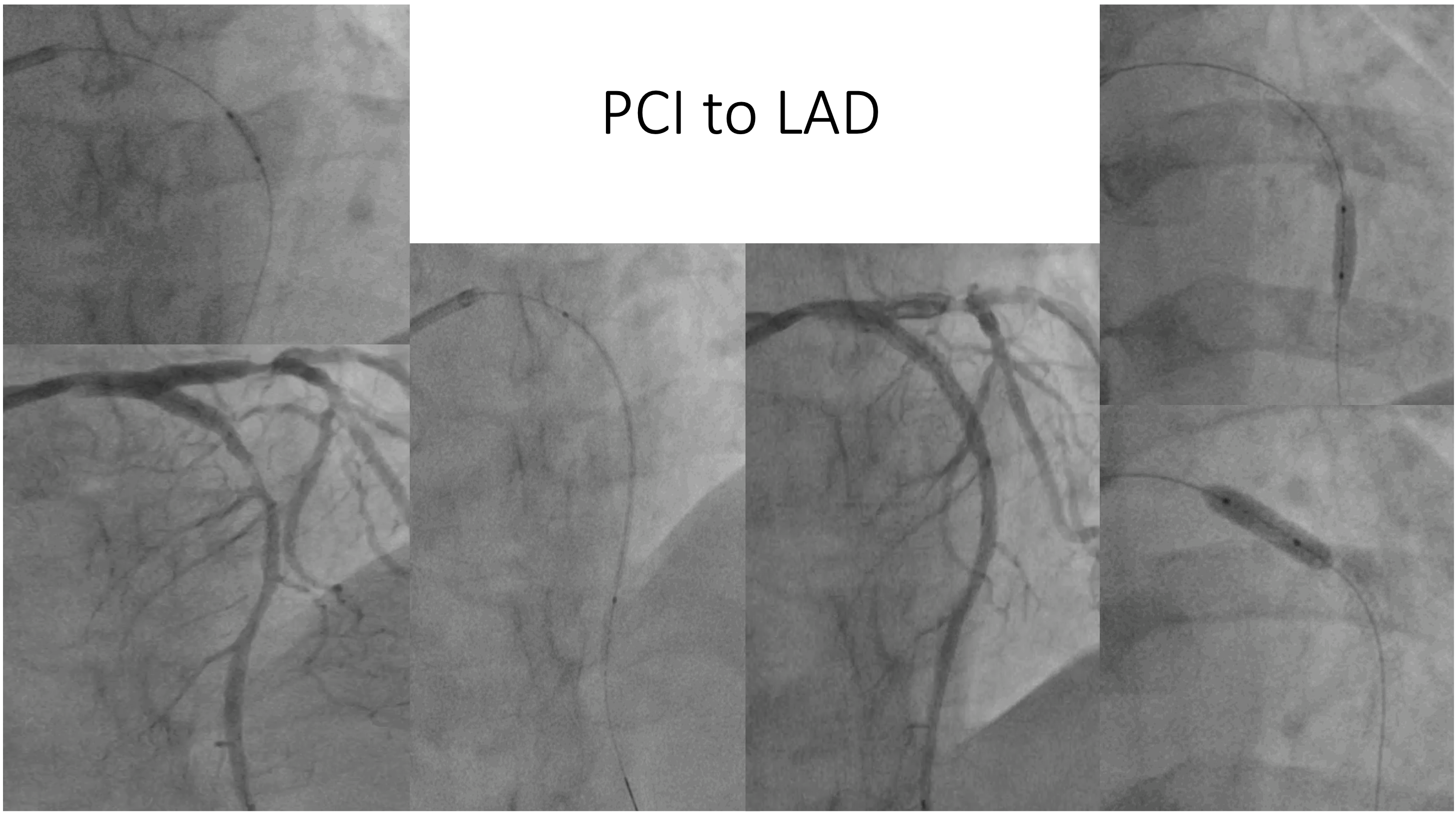
The coronary angiogram was performed via the right radial artery, which showed mid-LAD 95-99% stenosis, OM 1 had 90% ostial lesion and mid-RCA had 50-60% diffuse disease. Hence, the primary PCI to LAD was performed. During the PCI, the LAD lesion was pre-dilated with a 2 x 10 mm balloon at 12 atm. Then 3.5 x 44 mm DES was deployed at 12 atm. and then post-dilated with a 3.5 x 10 mm NC balloon at 12 - 20 atm. But, during the post-dilatation, the Elis class III perforation had occurred.
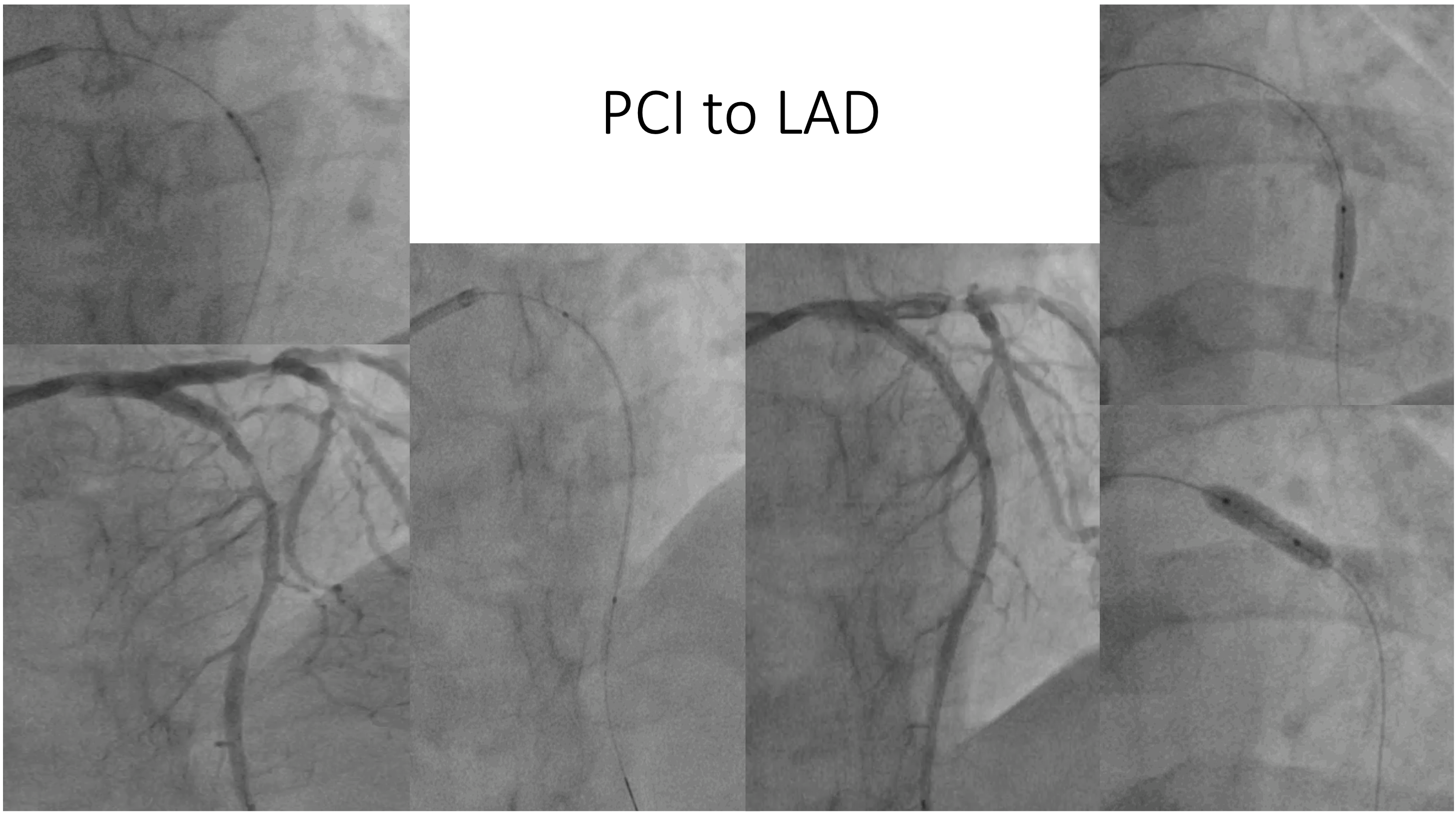


Interventional Management
Procedural Step
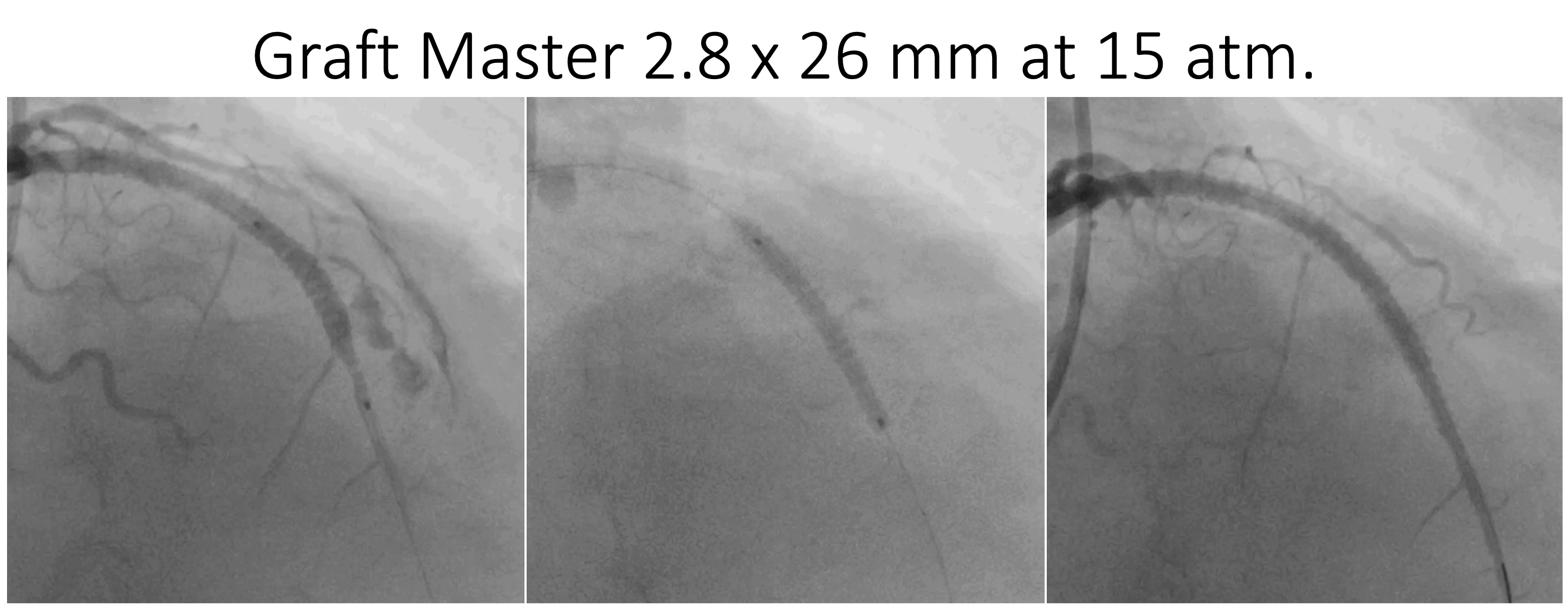
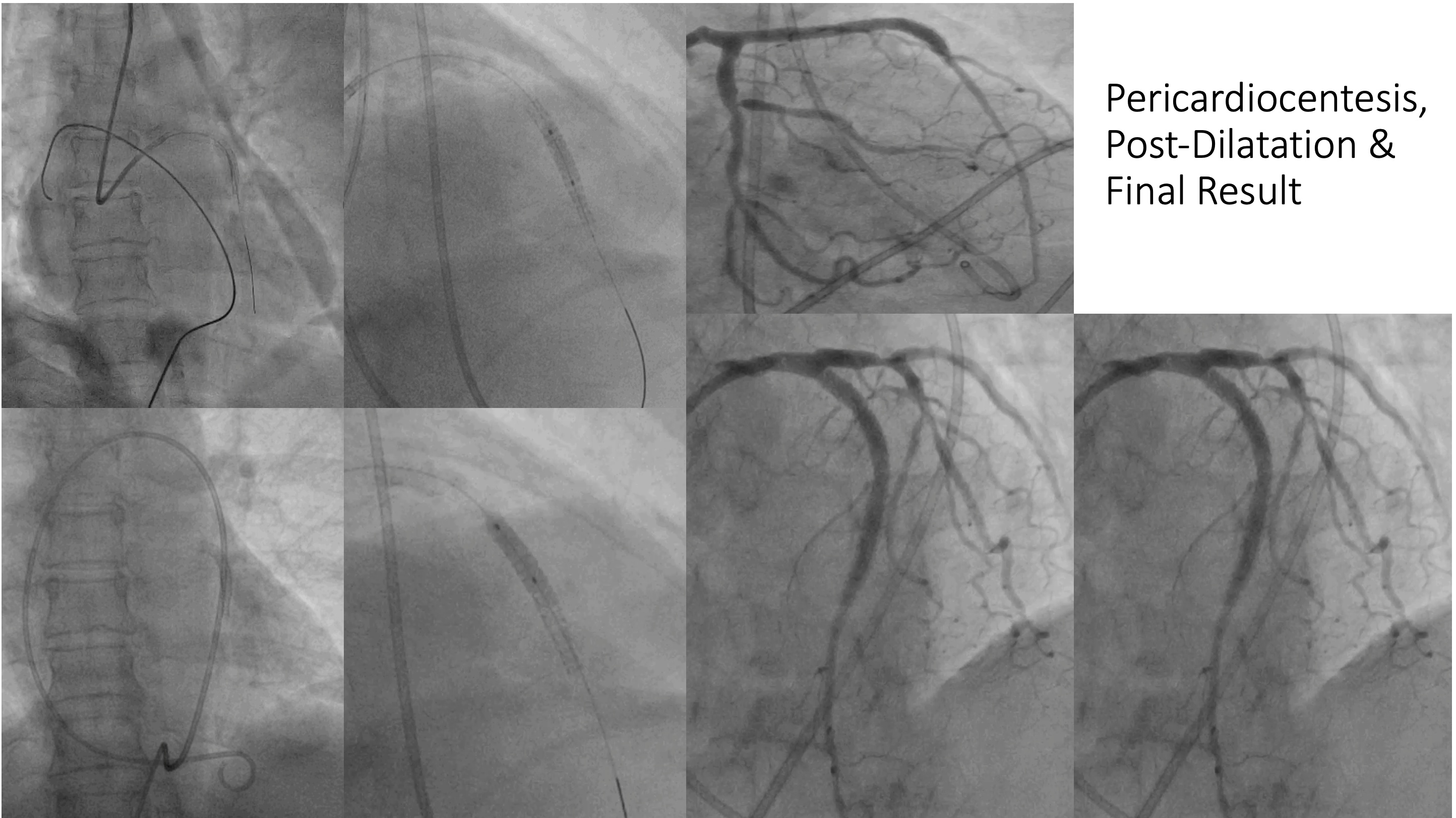
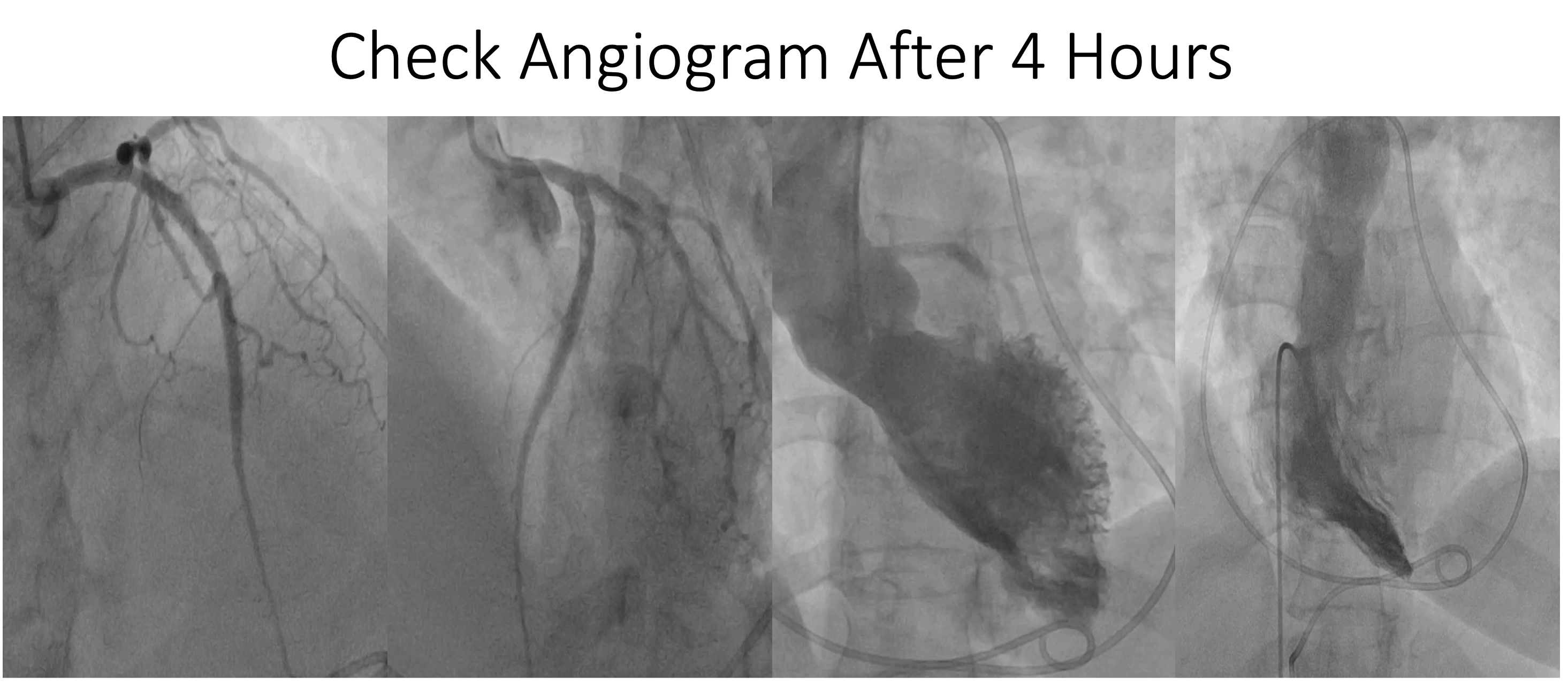
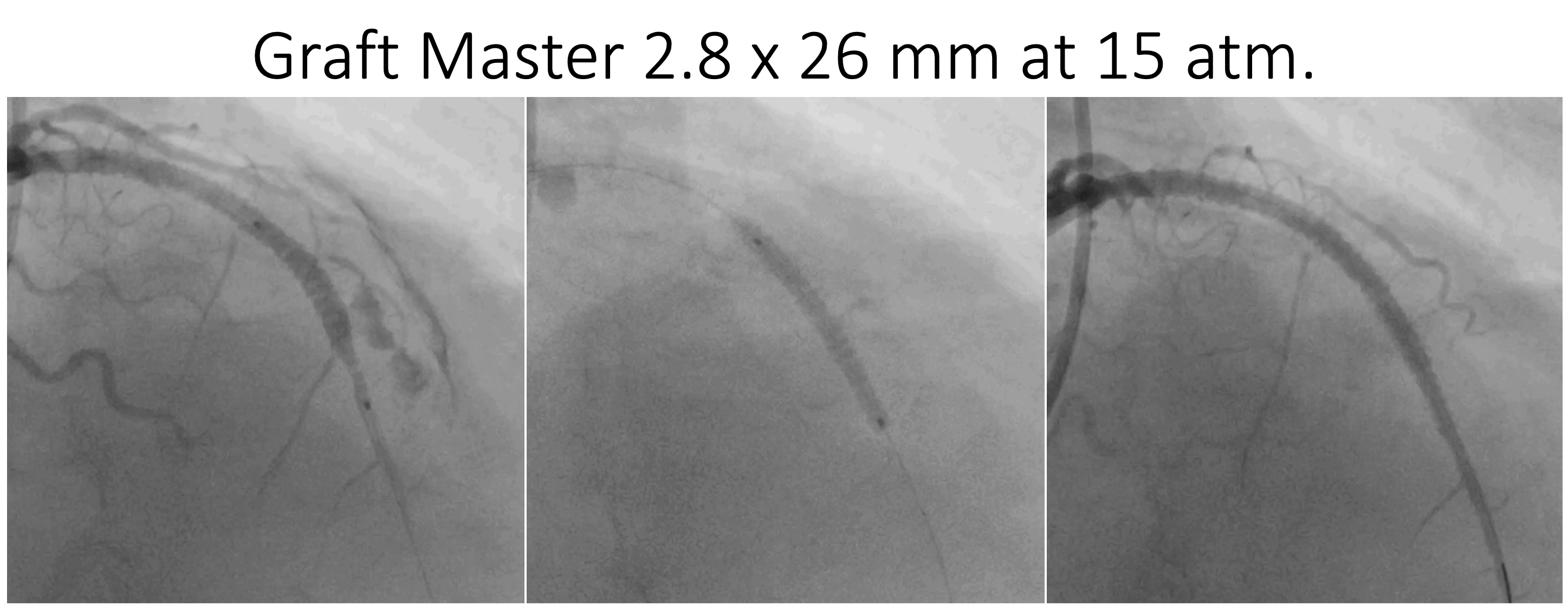
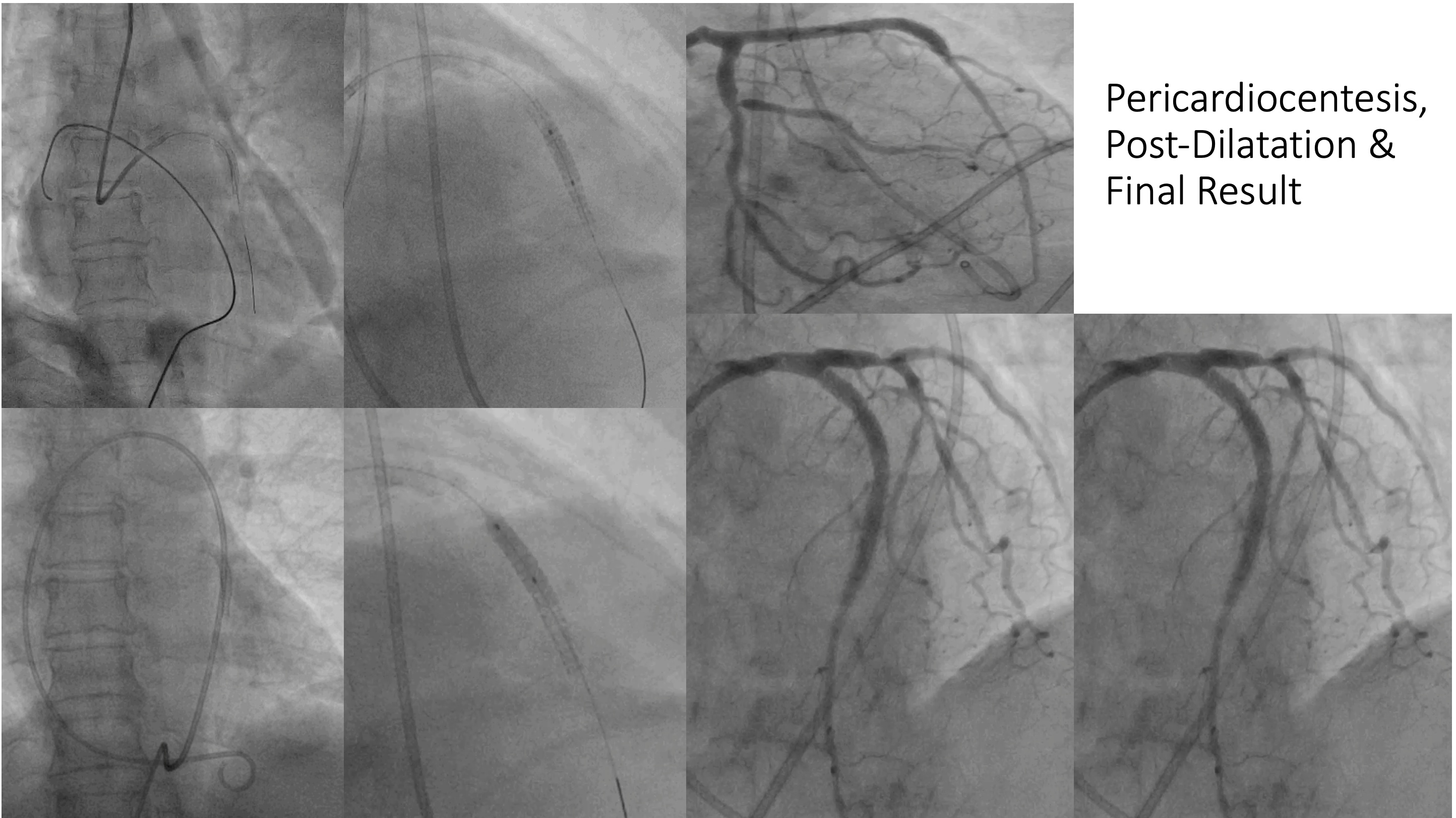
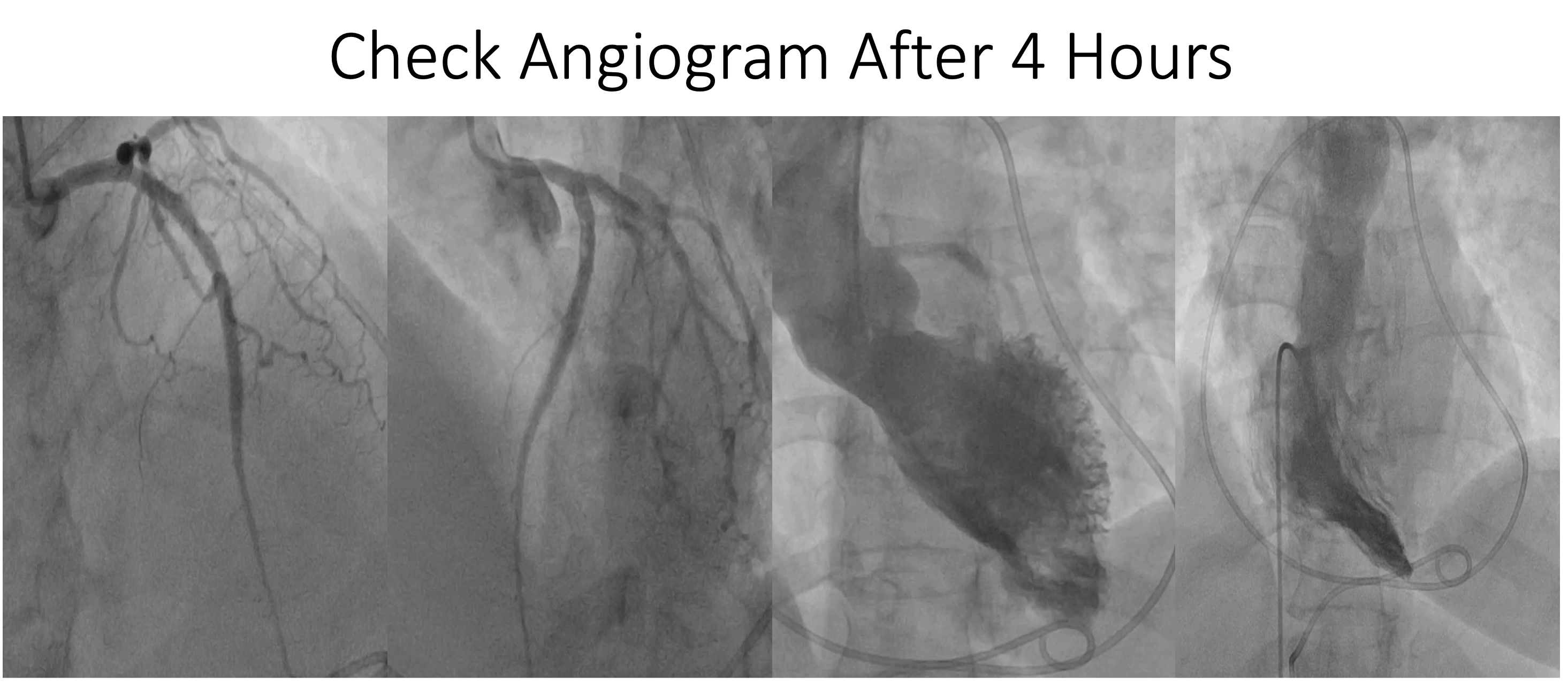
As we noticed perforation, the "Graftmaster" coronary stent graft (Abbott Vascular) 2.8 x 26 mm was immediately deployed. The patient was deteriorating hemodynamically, so the pericardiocentesis was done immediately, and about 140 ml of fresh blood was withdrawn. The 5F pigtail catheter was kept in the pericardial cavity. Then the stent graft was post-dilated with a 3.5 x 10 mm NC balloon at 10 - 16 atm. After that, the patient was shifted to the intensive care unit in stable condition for further management. After three hours, the BP started to fall, hence around 60 ml of blood was aspirated from the pericardial cavity. The patient became stable again. But in the next hour, the BP again started to fall and around 60ml of blood aspirated again. Then, the patient was shifted to the cath lab and a check-angiogram of coronaries and heart cavities was done but no obvious source of bleeding was found. The repeat ACT was 130 seconds. We have no other options, so we decided to give intra-pericardial tranexamic acid instead of systemic infusion. After each aspiration, we infused 500 mg of tranexamic acid into the pericardial cavity through a pigtail catheter with 5 ml of normal saline. Even after the first dose of tranexamic acid, the amount of aspirate became lesser, and gradually, it became serous rather than the fresh blood. Then the patient remained stable; the Pigtail catheter was removed on the third day, and the patient was discharged on the fifth day.
Case Summary
Coronary artery perforation is rare but a serious complication during PCI. If not treated promptly, it may lead to a grave outcome including the death of the patient. Even after the successful treatment with the covered stent, continuous non-obvious oozing may persist. Systemic use of antifibrinolytic agents i.e. "Tranexamic Acid" is an effective therapy to prevent persistent oozing anywhere in the body. Still, it may be associated with an increased risk of thromboembolic events and seizures. Intrapericardial Tranexamic Acid may be an effective therapy to prevent continuous oozing after coronary perforation. Though the data are lacking, this may be a thought-provoking idea for further research.


