Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-150
Case Report of a Rare Complication: The IVUS Dislodgement
By Piyoros Lertsanguansinchai
Presenter
Piyoros Lertsanguansinchai
Authors
Piyoros Lertsanguansinchai1
Affiliation
King Chulalongkorn Memorial Hospital, Thailand1,
View Study Report
TCTAP C-150
Coronary - Complication Management
Case Report of a Rare Complication: The IVUS Dislodgement
Piyoros Lertsanguansinchai1
King Chulalongkorn Memorial Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 78-year-old female with a history of hypertension, dyslipidemia, and diabetes mellitus was admitted with non-ST elevation acute coronary syndrome to the provincial hospital. His blood pressure was 145/85 mmHg, his heart rate was 80 beats per minute, his respiration rate was 22 breaths per minute, and her temperature was 36.5 oC. The angiography at the provincial hospital showed TVD. The patient was advised to undergo CABG, but he strongly refused. He was referred for PCI at our institution.






Relevant Test Results Prior to Catheterization
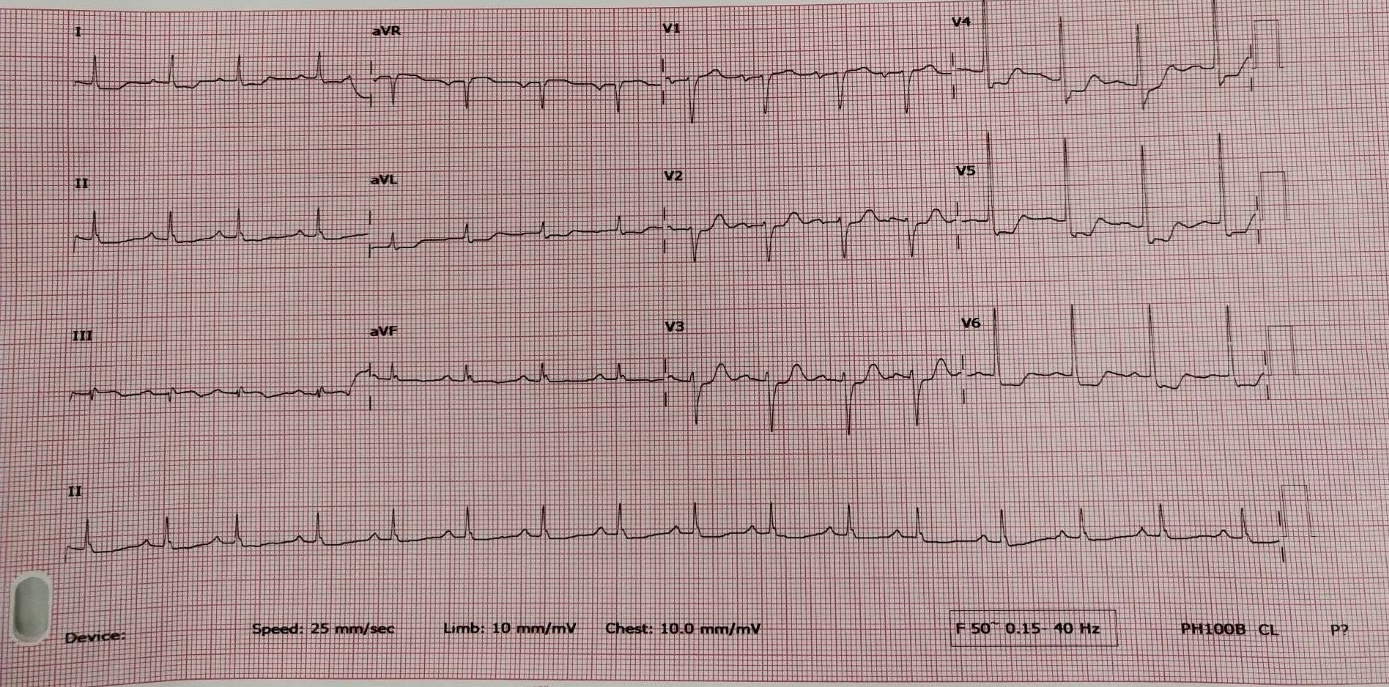
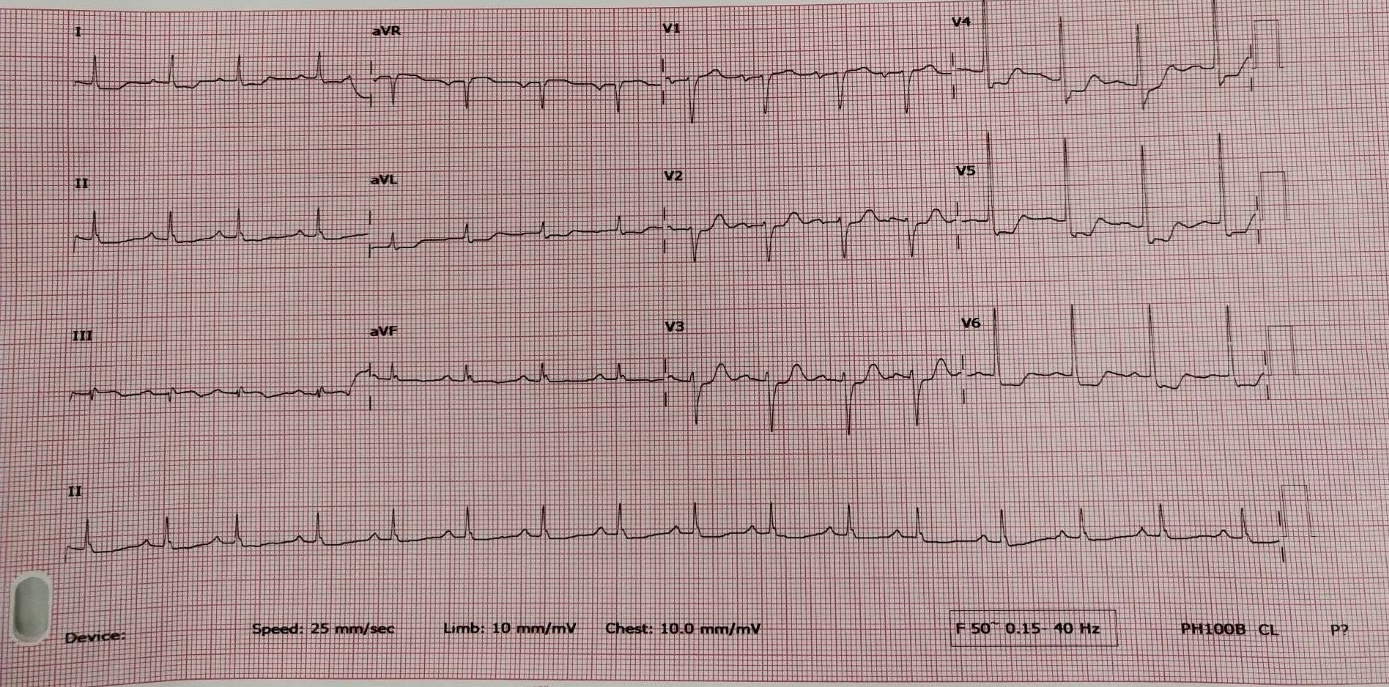
The initial electrocardiogram showed a sinus rhythm rate of 70 bpm with ST segment elevation
Relevant Catheterization Findings
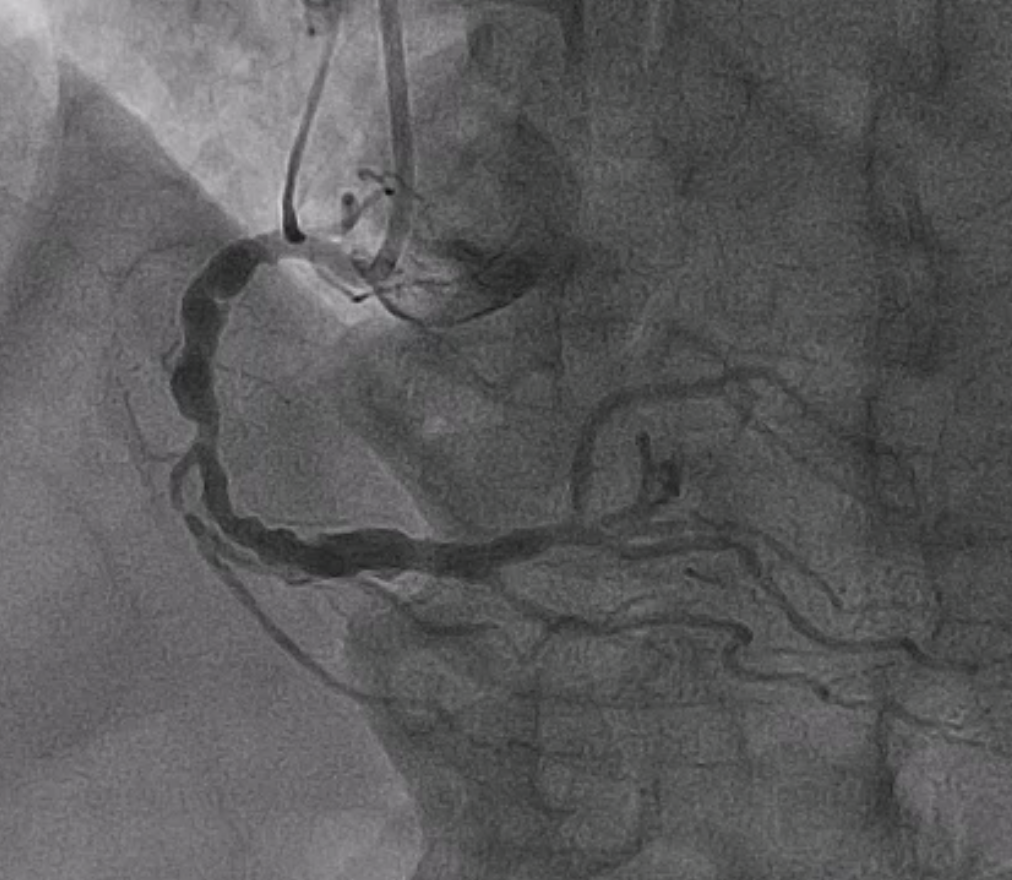
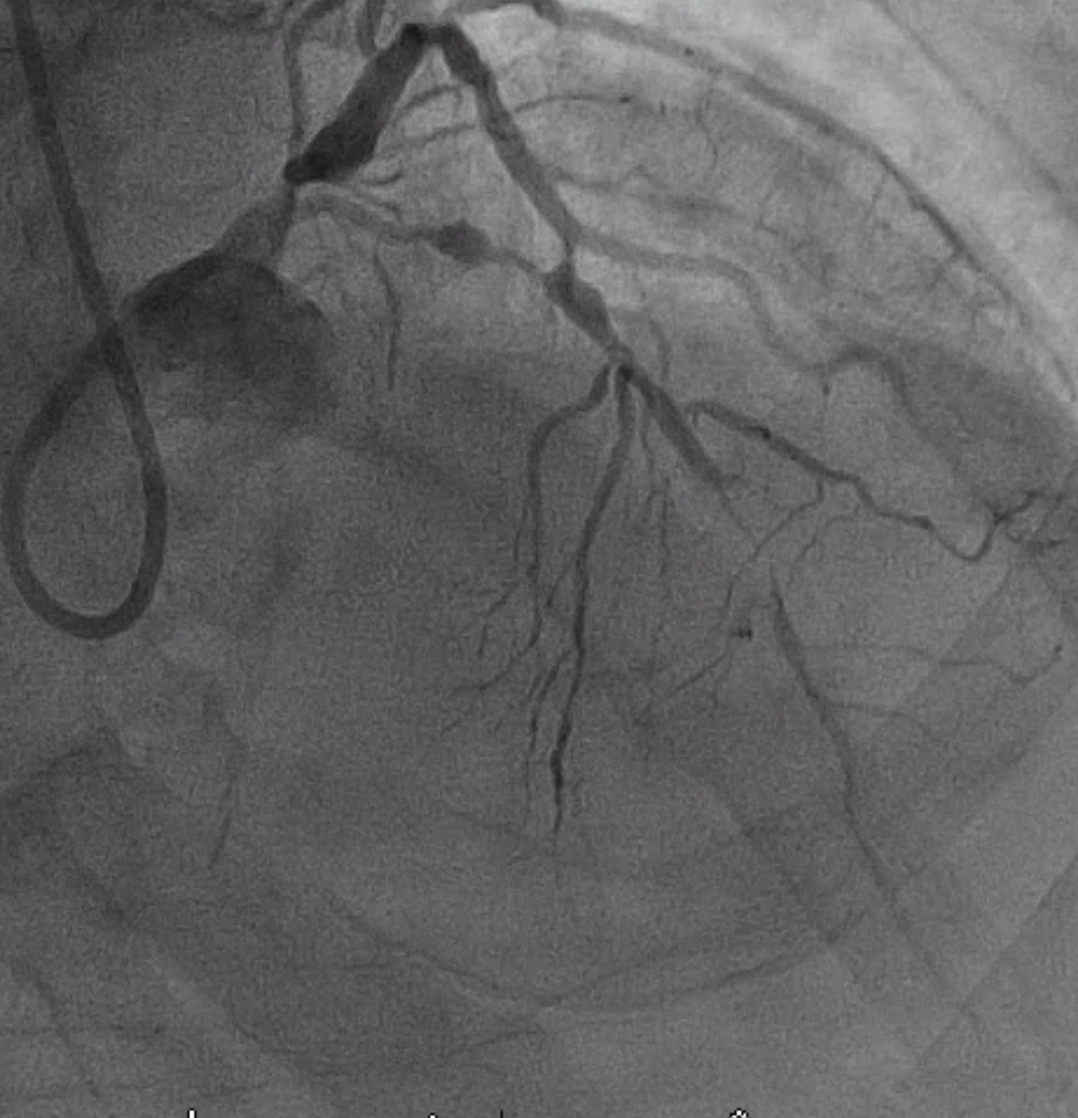
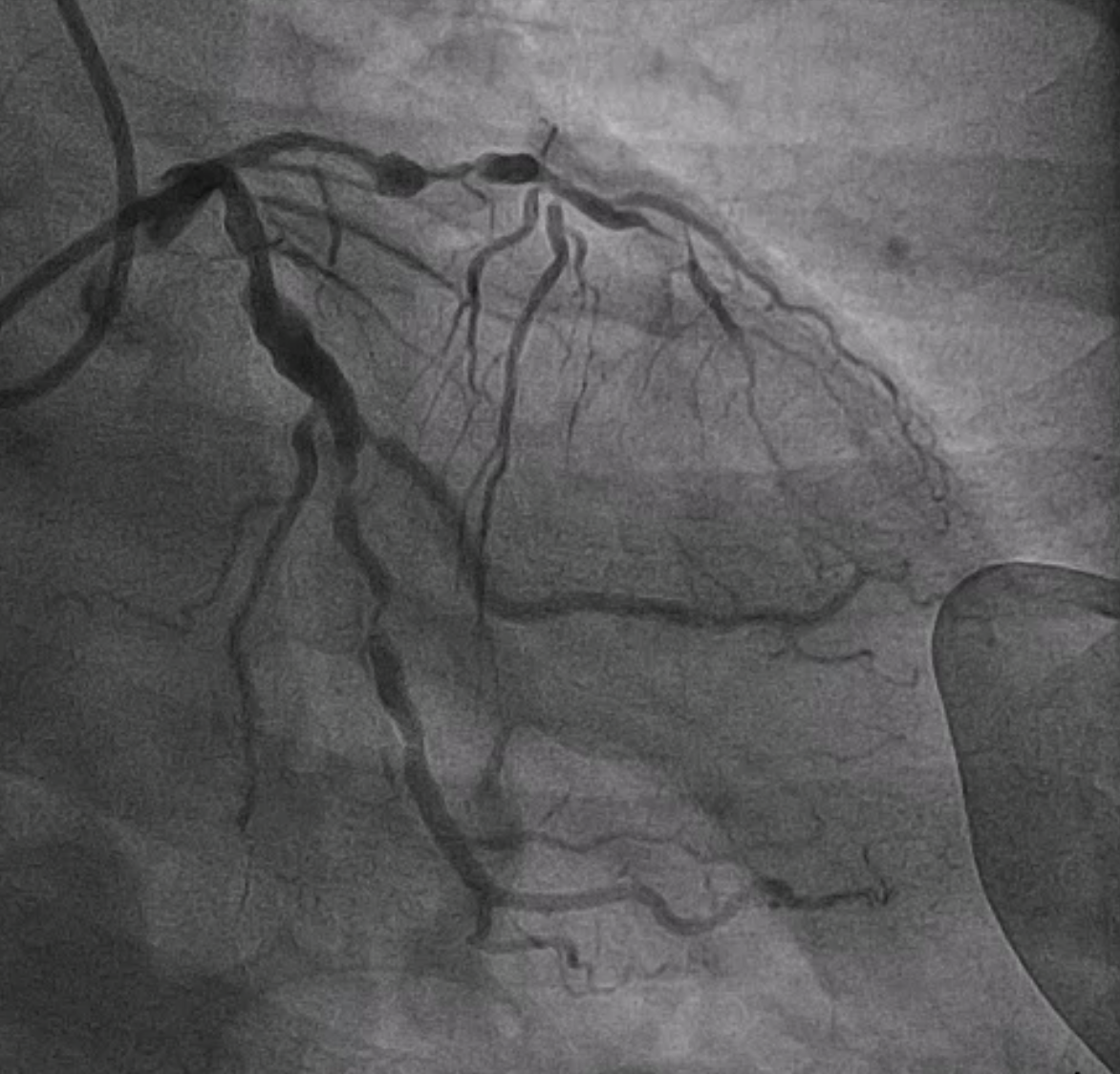
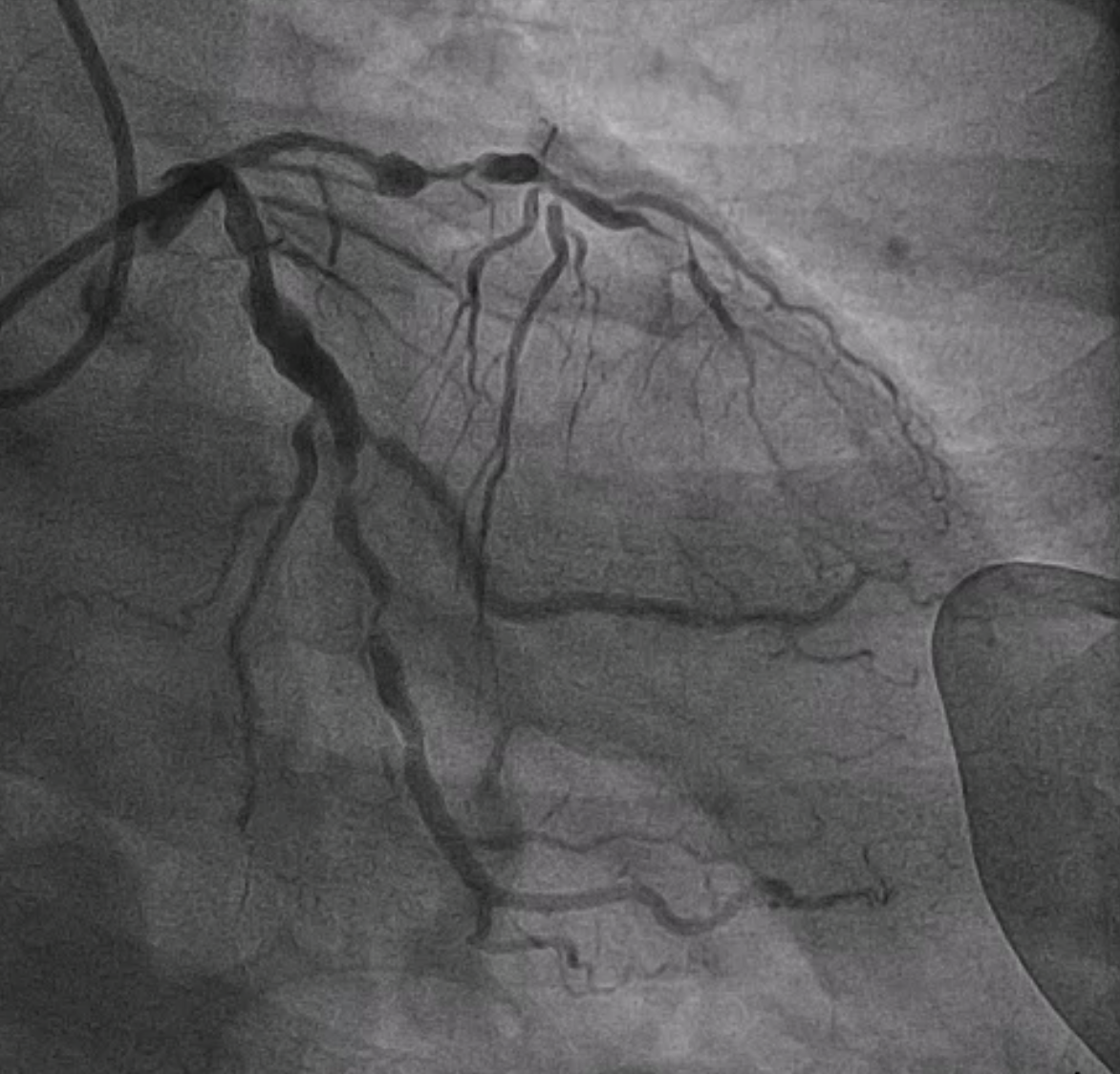
At our hospital, an urgent coronary angiography showed an aneurysmal change with significant stenosis at the proximal to mid LAD, an aneurysmal change at the proximal LCx with significant stenosis at the proximal to distal LCx, and an aneurysmal change with 70% stenosis at the proximal to mid RCA. The coronary angiography showed TVD with medina (0,1,1) and was compatible with a complex bifurcation lesion by definition criteria.
Interventional Management
Procedural Step
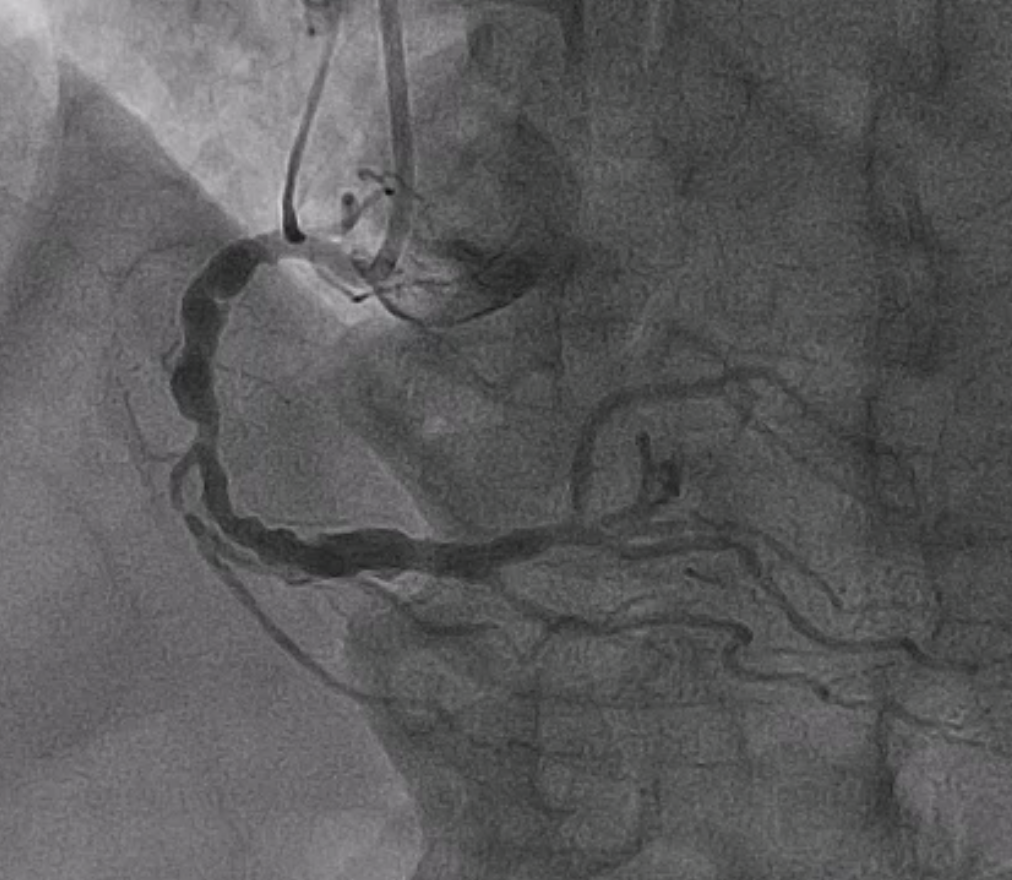
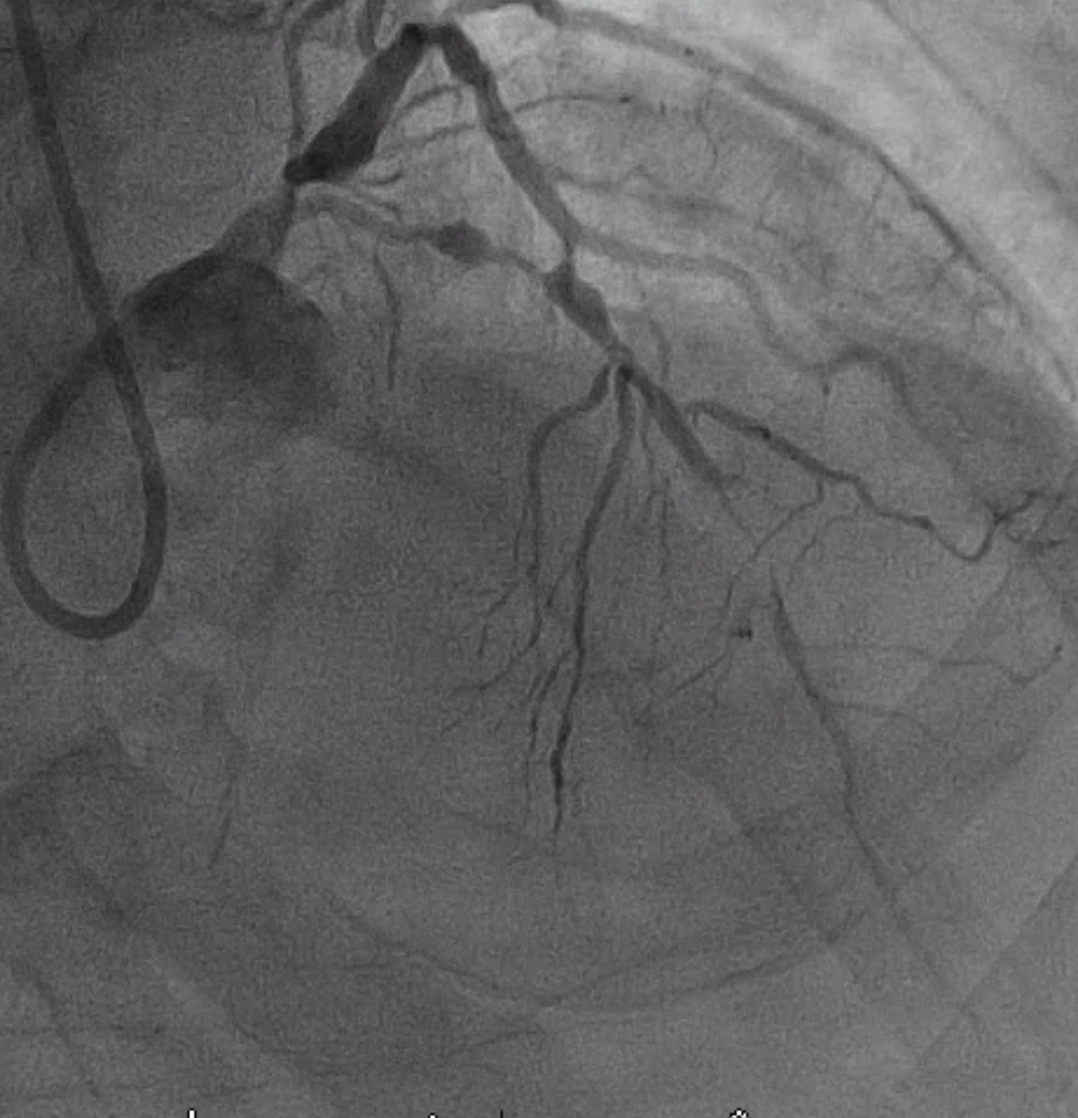
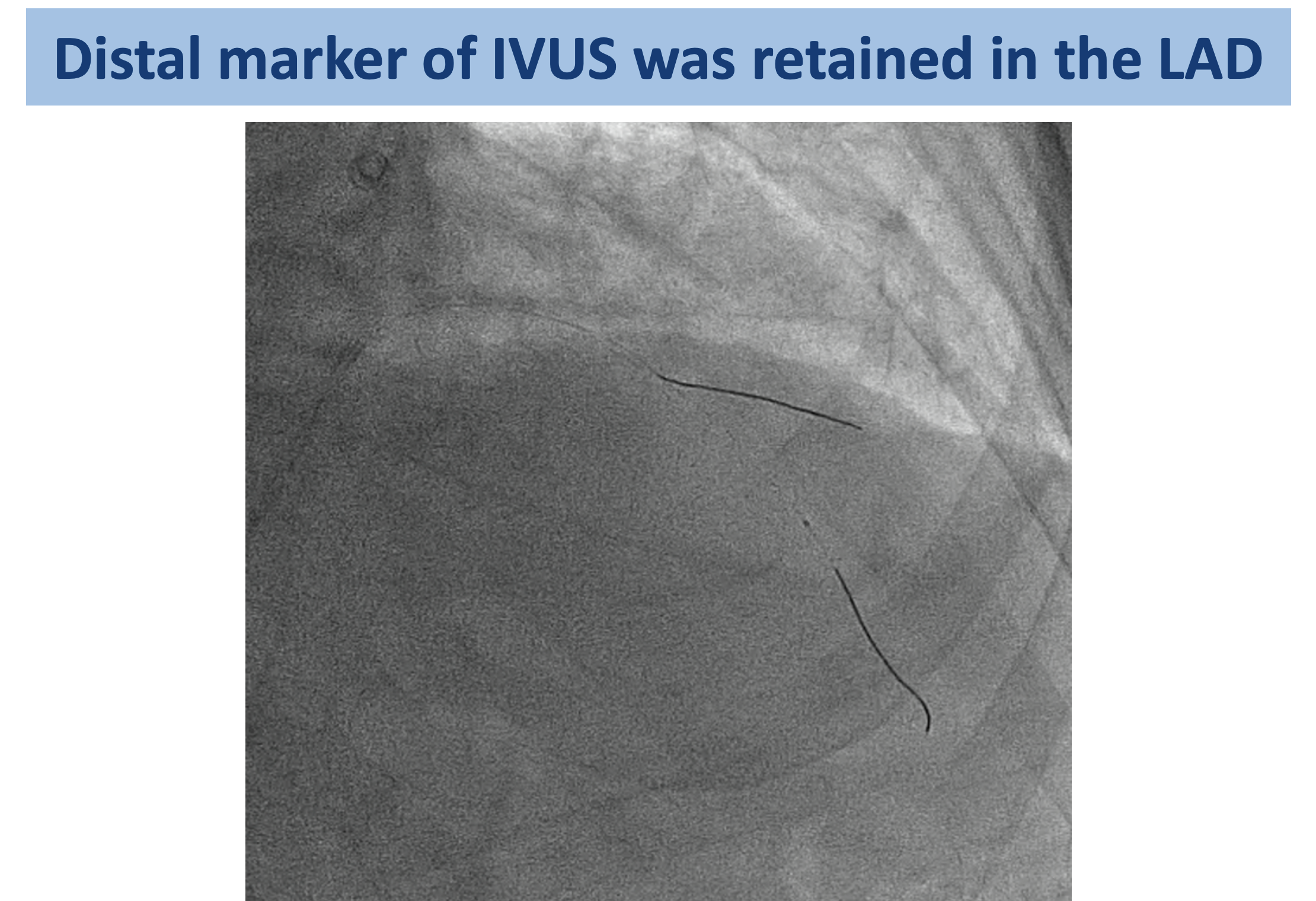
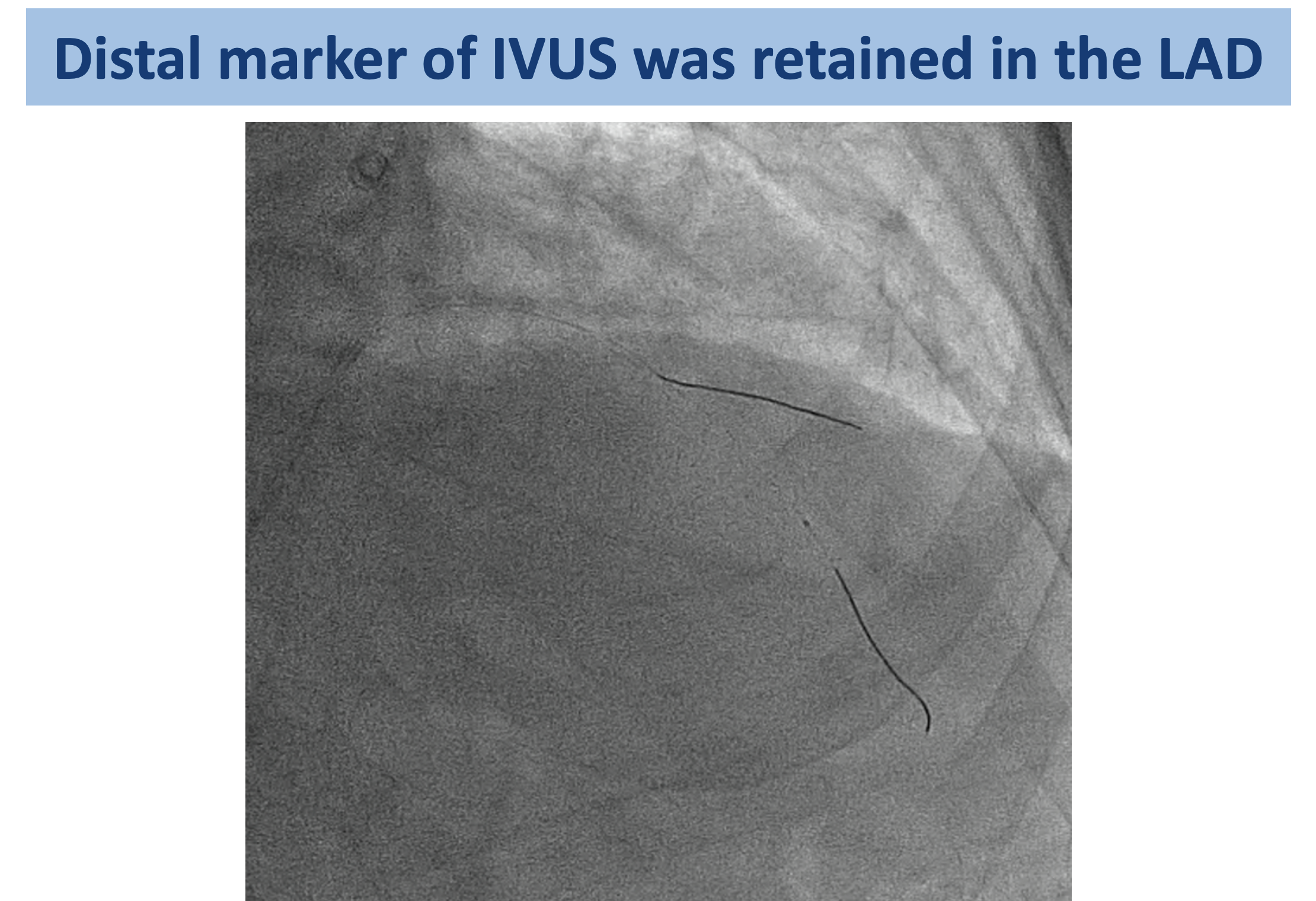
Due to a complex bifurcation lesion, we planned to perform PCI with a DK Culotte technique under IVUS guidance. We plan to perform PCI at the distal LCX and mid-LAD before proceeding with PCI at the LM bifurcation. We engaged LM with a 7Fr EBU via RFA. The mid- to distal LCx lesions were dilated with a semi-compliant 2.5/15 mm balloon at 16 atm. IVUS from LCx to LM showed fibrocalcific plaque along LCx with MLA 3.5 mm2 and 80% plaque burden. A 3.5/38 mm stent was deployed from mid to distal LCx. The mid LAD lesion was dilated with a semi-compliant 2.5/15 mm balloon at 16 atm. IVUS from LAD to LM showed fibrocalcific plaque along LAD with MLA 2.5 mm2 and 80% plaque burden at mid LAD. During withdrawing the IVUS from the LAD under fluoroscopy, we recognized that the distal tip of the IVUS catheter was broken off and retained in the LAD. Upon examining the IVUS catheter component of the IVUS catheter, we suspected that there was a guidewire exit port and a hydrophilic sheath retained in the LAD, which was approximately 10 cm in length. The patient developed chest pain; however, the hemodynamics were stable. The angiography showed worsening TIMI flow. We performed multiple twisted wires technique to remove the retained IVUS from the LAD. After removing the retained IVUS, we completed the procedure using the DK culotte technique, utilizing a 2.75/38 mm stent at the mid LAD, a 3.5/34 mm stent from the LM to the proximal LAD, and a 3.5/22 mm stent from the LM to the proximal LCx.
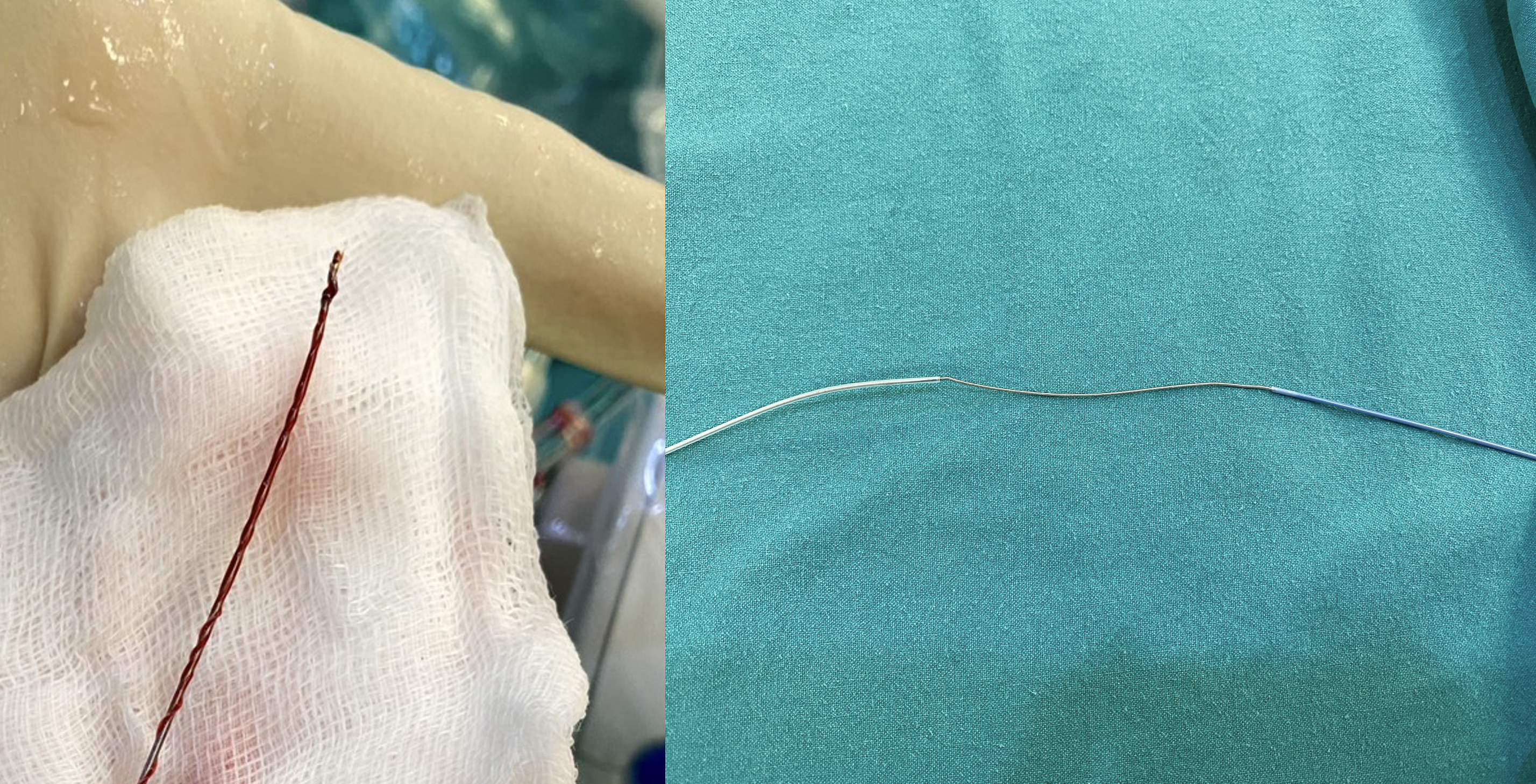
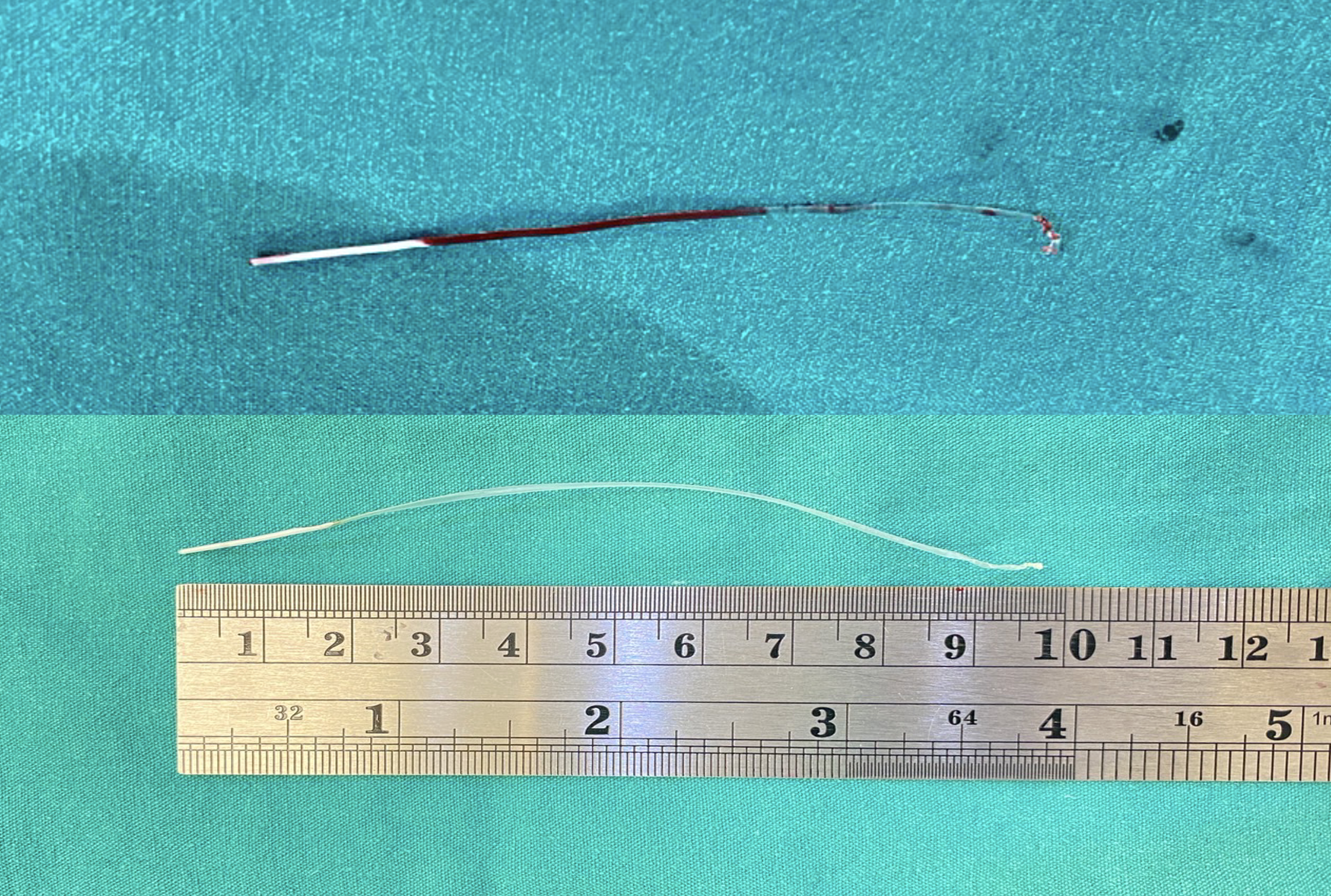
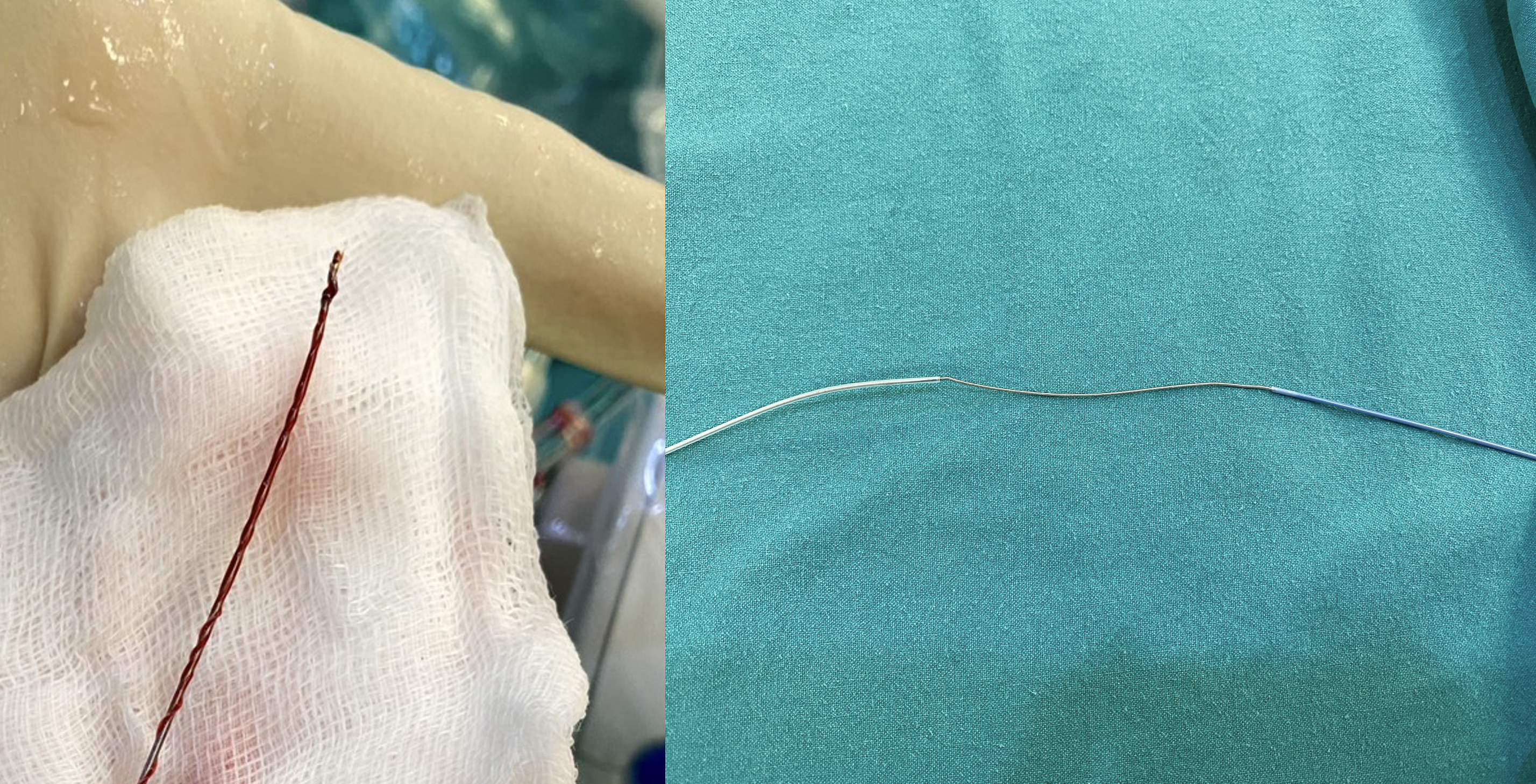
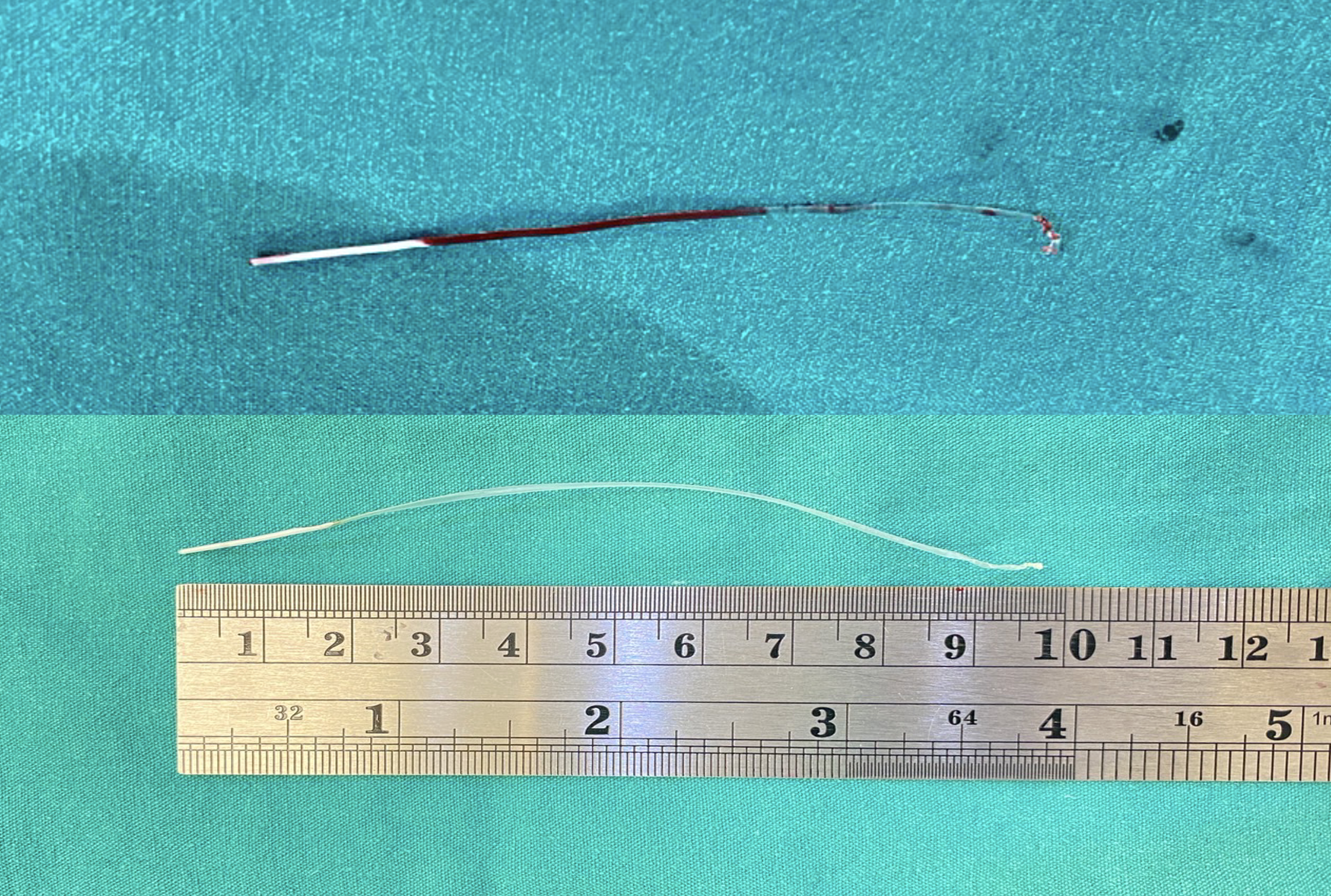
Case Summary
This case presents a significant challenge regarding IVUS dislodgement. We successfully retrieved 10 cm of retained IVUS from the LAD. When dealing with the IVUS dislodgement, it is necessary to identify the particular component of the IVUS that has become dislodged and to measure its length. If any part of the IVUS is partially within the guiding catheter, the trapping balloon technique may be used. In the absence of the IVUS within the guiding catheter, one may consider uses a loop snare, multiple twisted wire technique, or a distal embolic protection device. Contact the CVT standby for surgical removal or mechanical support in situations of hemodynamic instability.


