Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-124
Multivessel Revascularization in a Case With Absence of the Left Circumflex Artery and a Super-Dominant Right Coronary Artery
By Zhen Cheng Hwang, Lung-Ching Chen
Presenter
Zhen Cheng Hwang
Authors
Zhen Cheng Hwang1, Lung-Ching Chen1
Affiliation
Shin Kong Wu Ho-Su Memorial Hospital, Taiwan1,
View Study Report
TCTAP C-124
Coronary - Complex PCI - Multi-Vessel Disease
Multivessel Revascularization in a Case With Absence of the Left Circumflex Artery and a Super-Dominant Right Coronary Artery
Zhen Cheng Hwang1, Lung-Ching Chen1
Shin Kong Wu Ho-Su Memorial Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
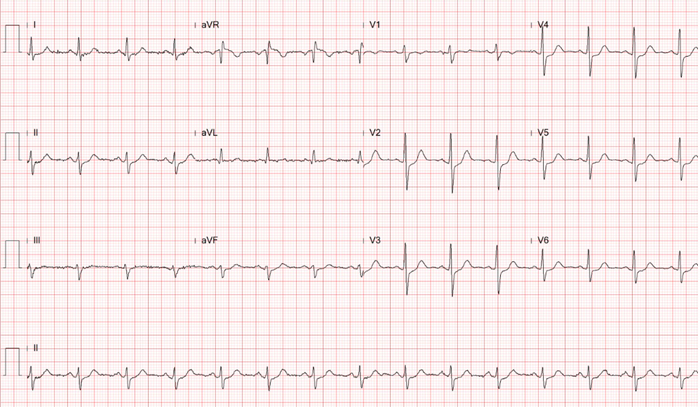
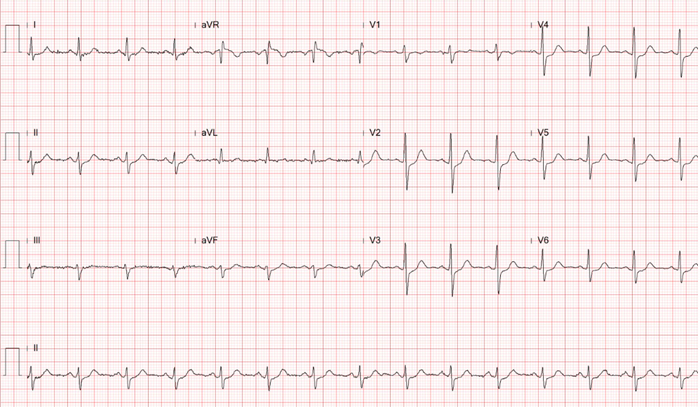
This 54-year-old businessman who had been experiencing intermittent chest pain for the past 6 months.The CCS score was II . He owns 6 factories,lives in high-stress life, combined with a smoking history of 0.5 pack per day for 10 years.Physical examination reveals chronically ill but shows neither abnormal heart sounds nor arrhythmias.Well perfusion of limbs and no pitting edema.Normal chest x-ray.EKG showed normal sinus rhythm without obvious ST changes


Relevant Test Results Prior to Catheterization
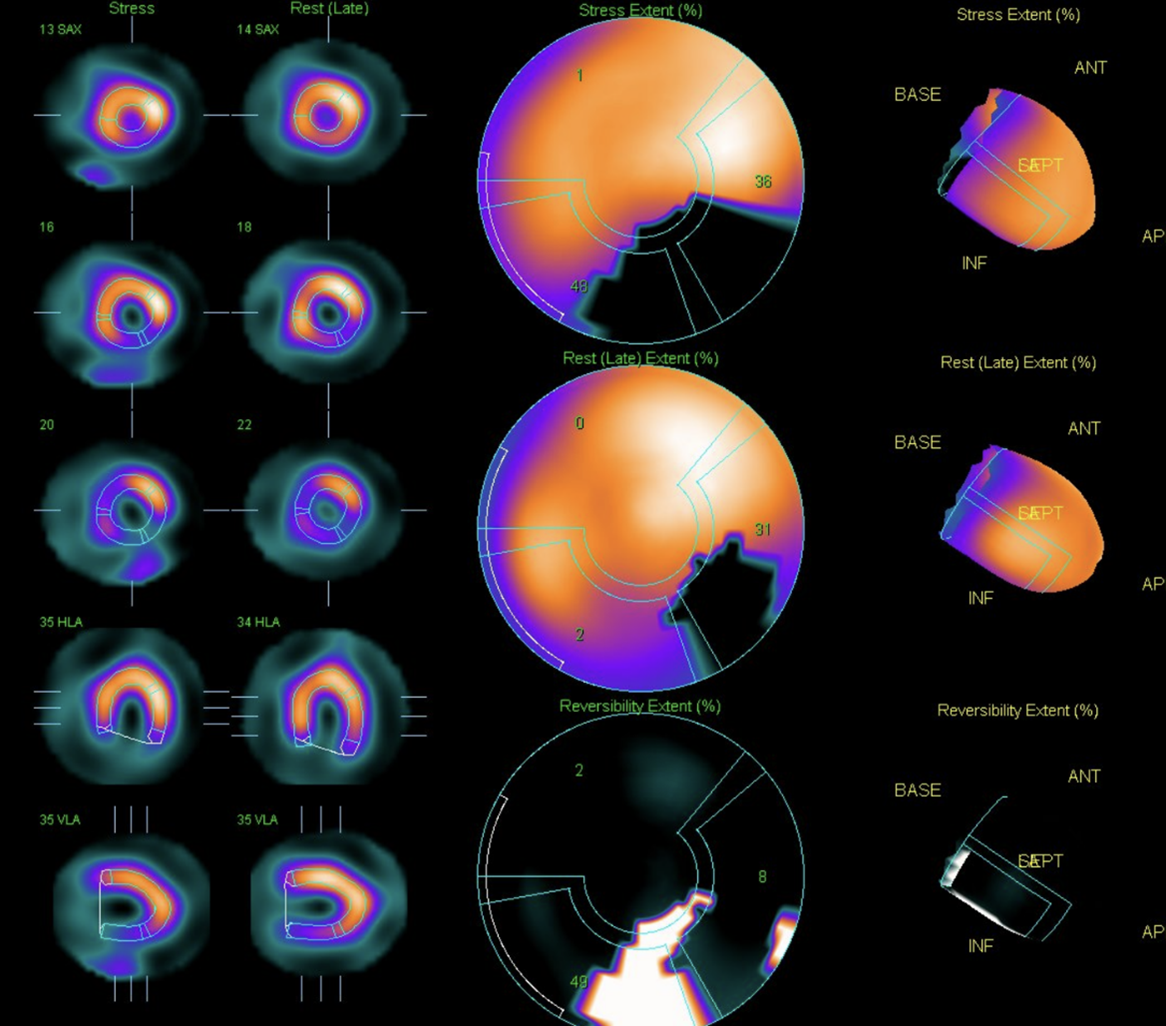
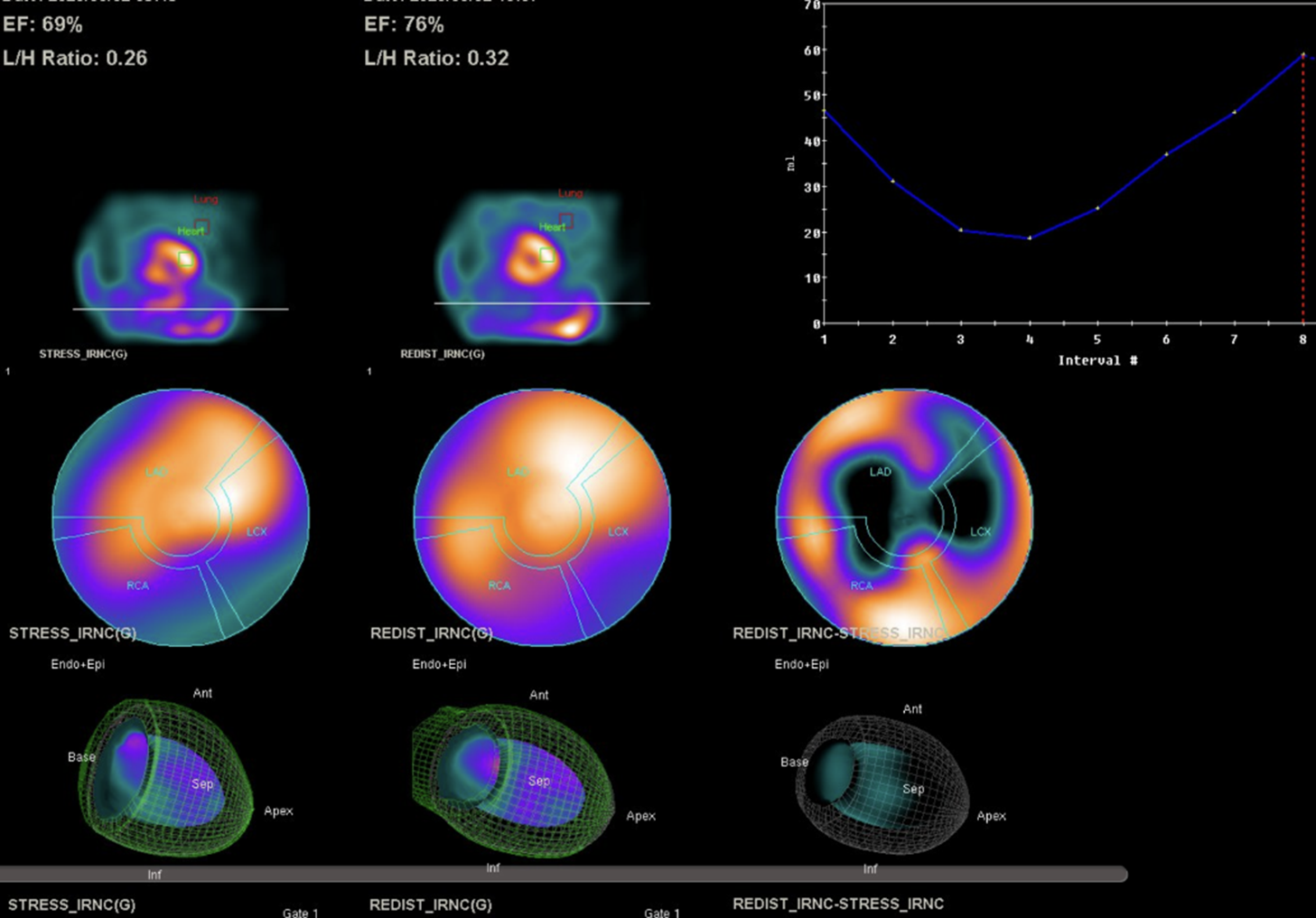
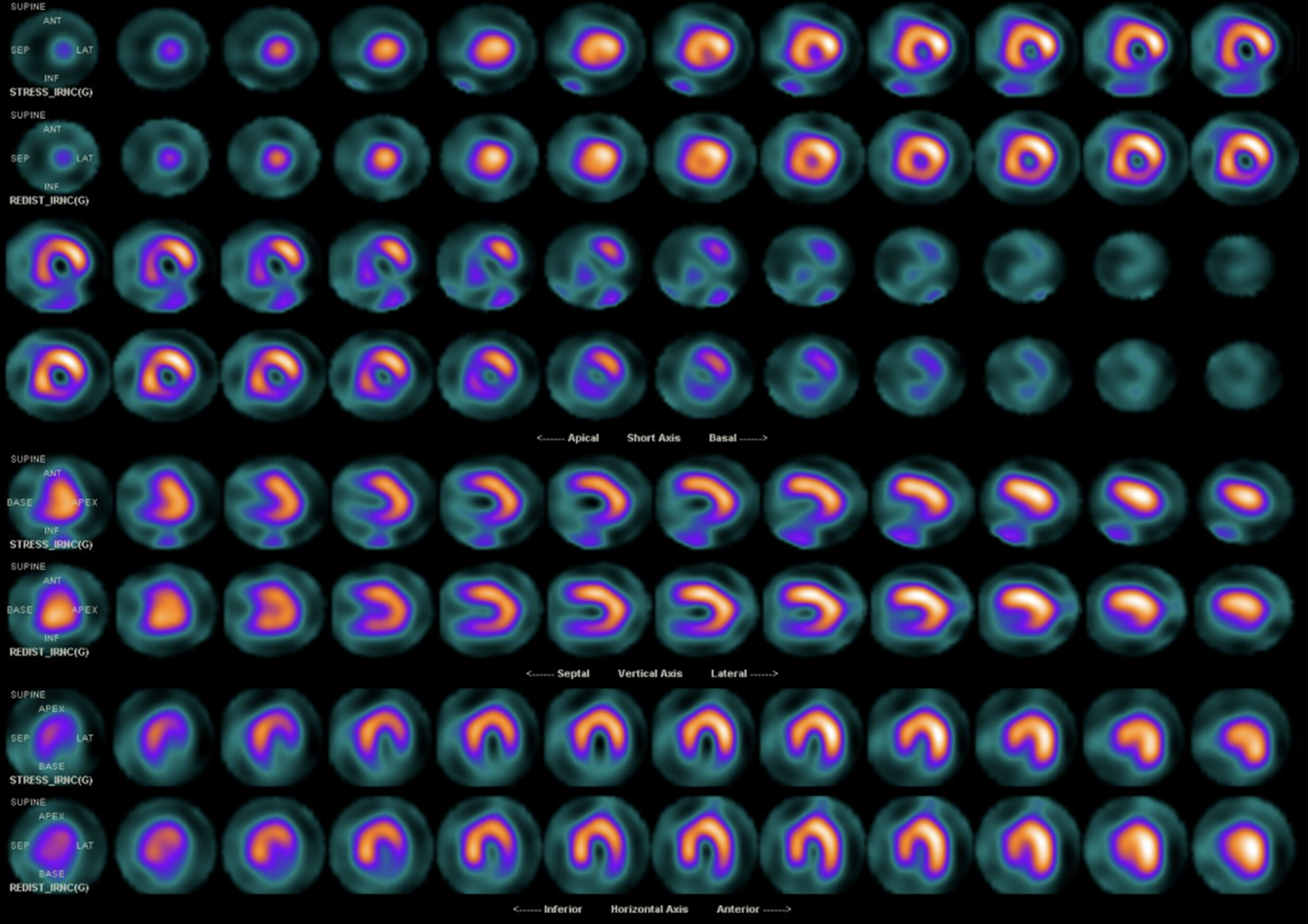
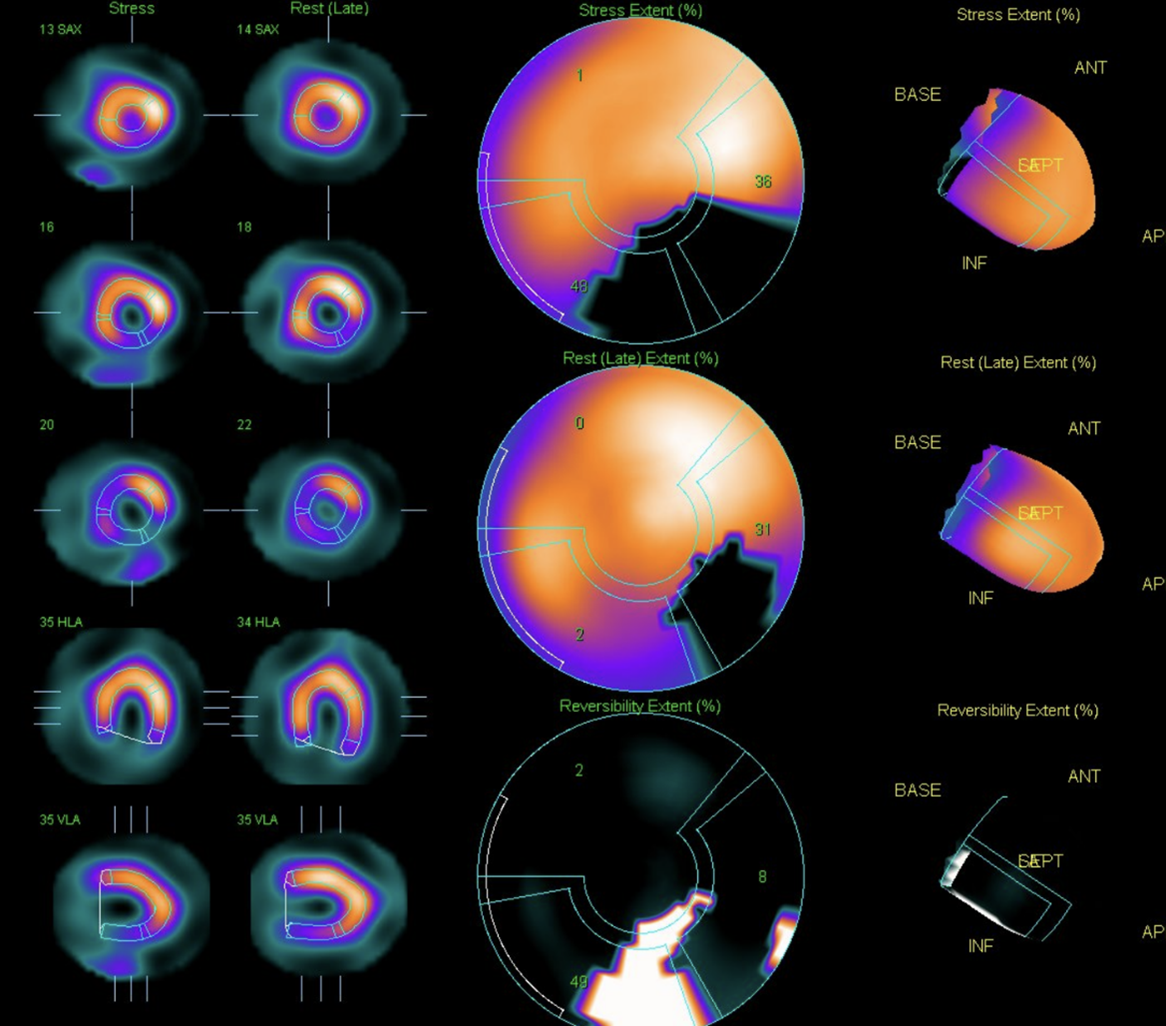
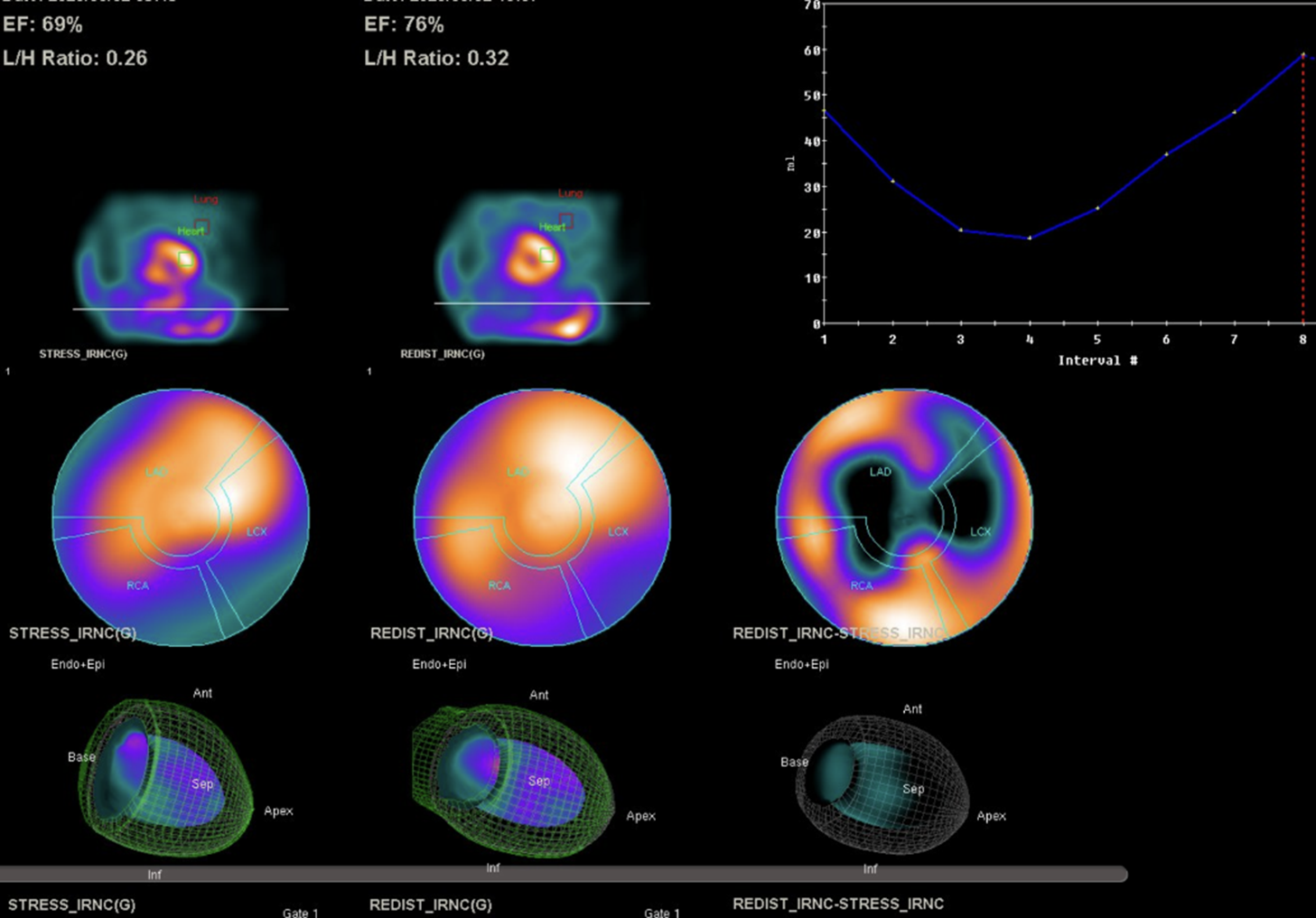
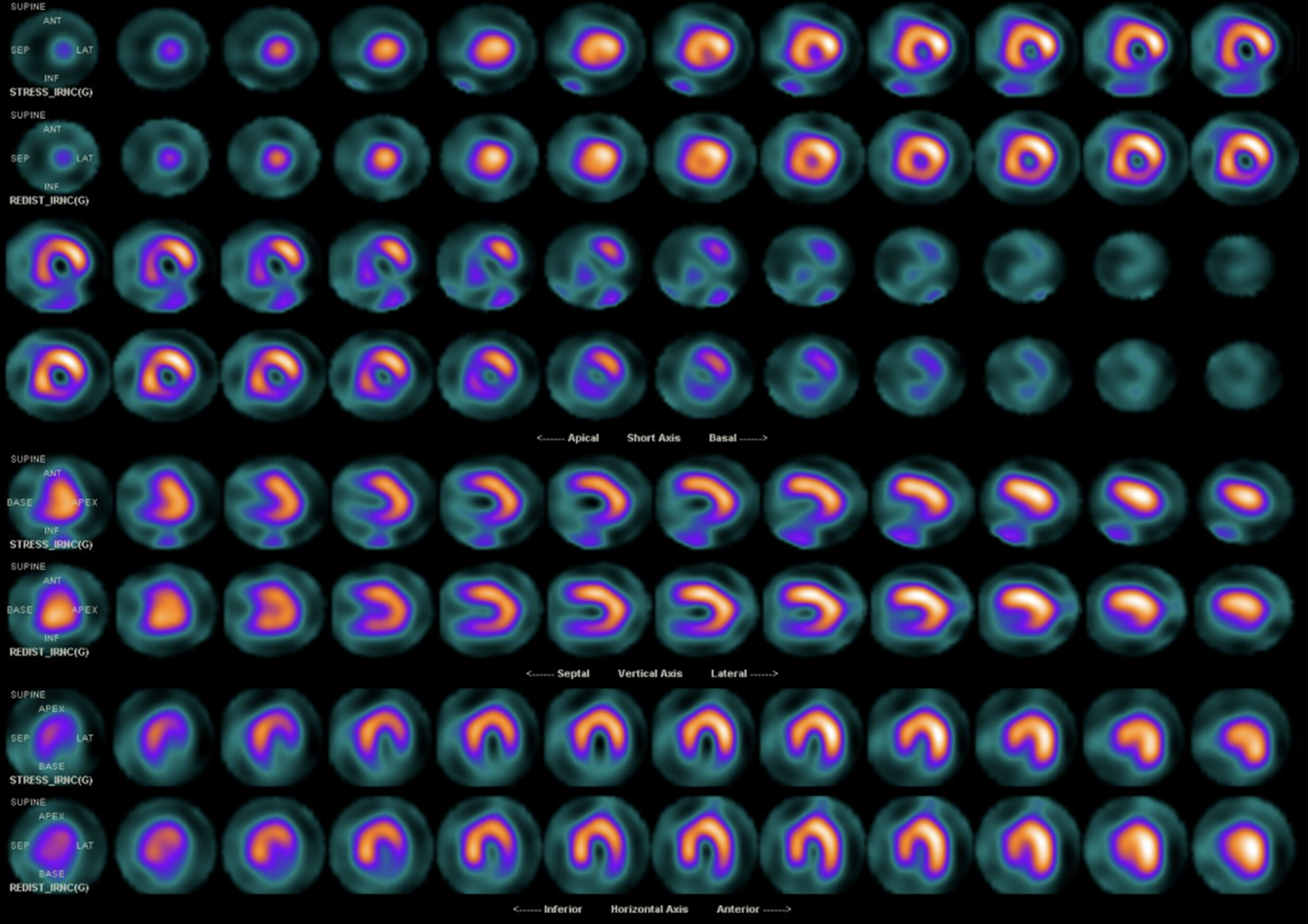
The laboratory test showed white blood cell count (WBC) of 7.8x10^3/uL, hemoglobin (Hb) level of 15.1gm/dl, platelet count of 181x10^3/uL.The glucose level is 98mg/dL, The liver enzyme levels show GOT (AST) at 19 U/L and GPT (ALT) at 22 U/L. Lipid panel results include HDL-C at 44mg/dL, LDL-C at 62mg/dL, triglycerides at 101mg/dL.Creatinine level of 0.75 mg/dL (eGFR:108.53) Tl-201 myocardial perfusion scan showed abnormal uptake in inferior, inferolateral, and septal wall
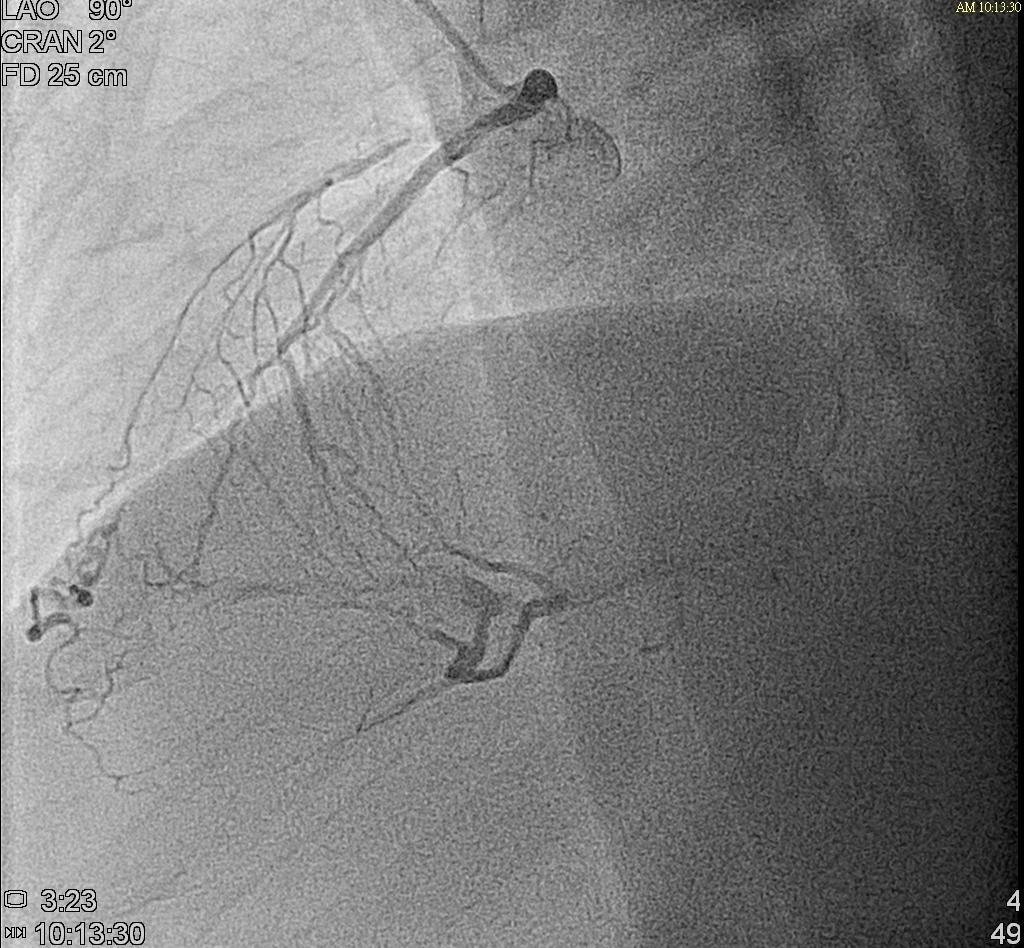
Relevant Catheterization Findings
Left main: 50% stenosis at distal left main
Left anterior descending artery: diffuse atherosclerotic plaque,proximal to middle total occlusion, with a big septal branch sending collaterals to distal LAD and distal RCA
Left circumflex artery: absence of LCX from angiography
Right coronary artery: very large, long dominant RCA, supplying inferior and lateral wall, middle segment total occlusionWe referred him to cardiovascular surgeon for CABG evaluation but he refused and preferred PCI

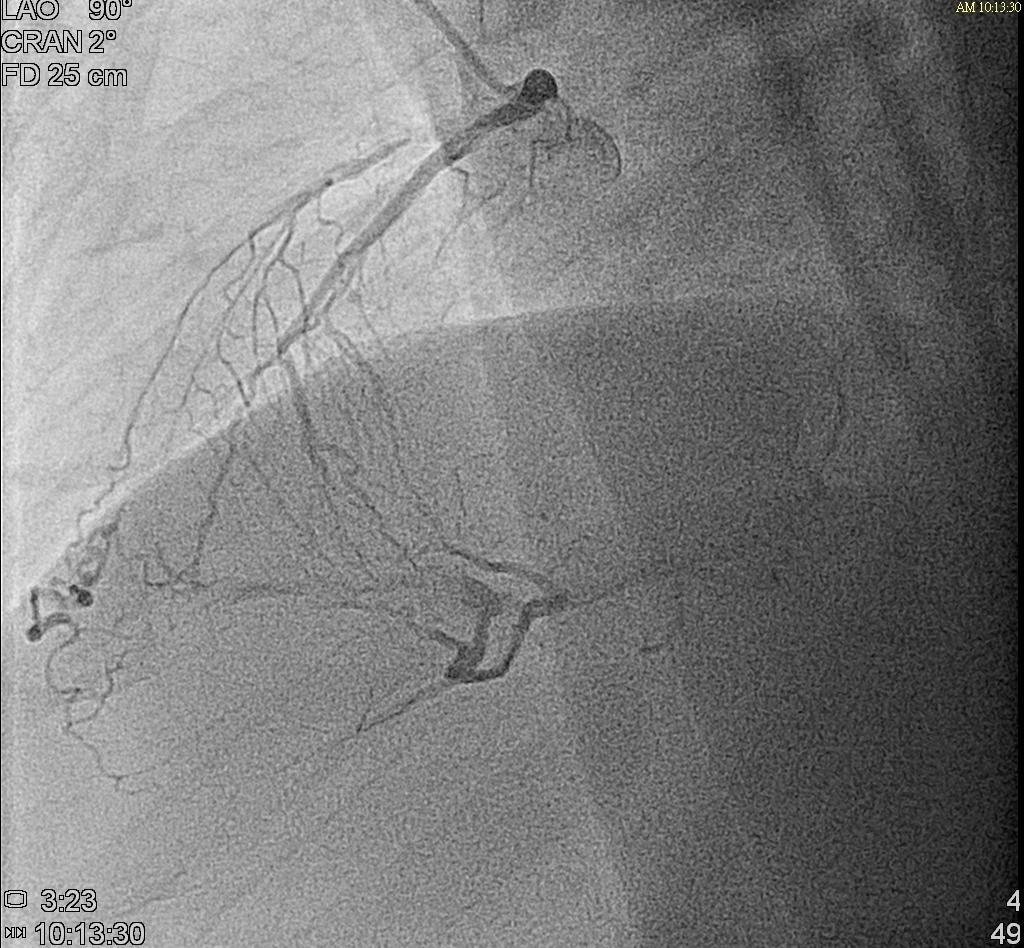

Left anterior descending artery: diffuse atherosclerotic plaque,proximal to middle total occlusion, with a big septal branch sending collaterals to distal LAD and distal RCA
Left circumflex artery: absence of LCX from angiography
Right coronary artery: very large, long dominant RCA, supplying inferior and lateral wall, middle segment total occlusionWe referred him to cardiovascular surgeon for CABG evaluation but he refused and preferred PCI


Interventional Management
Procedural Step
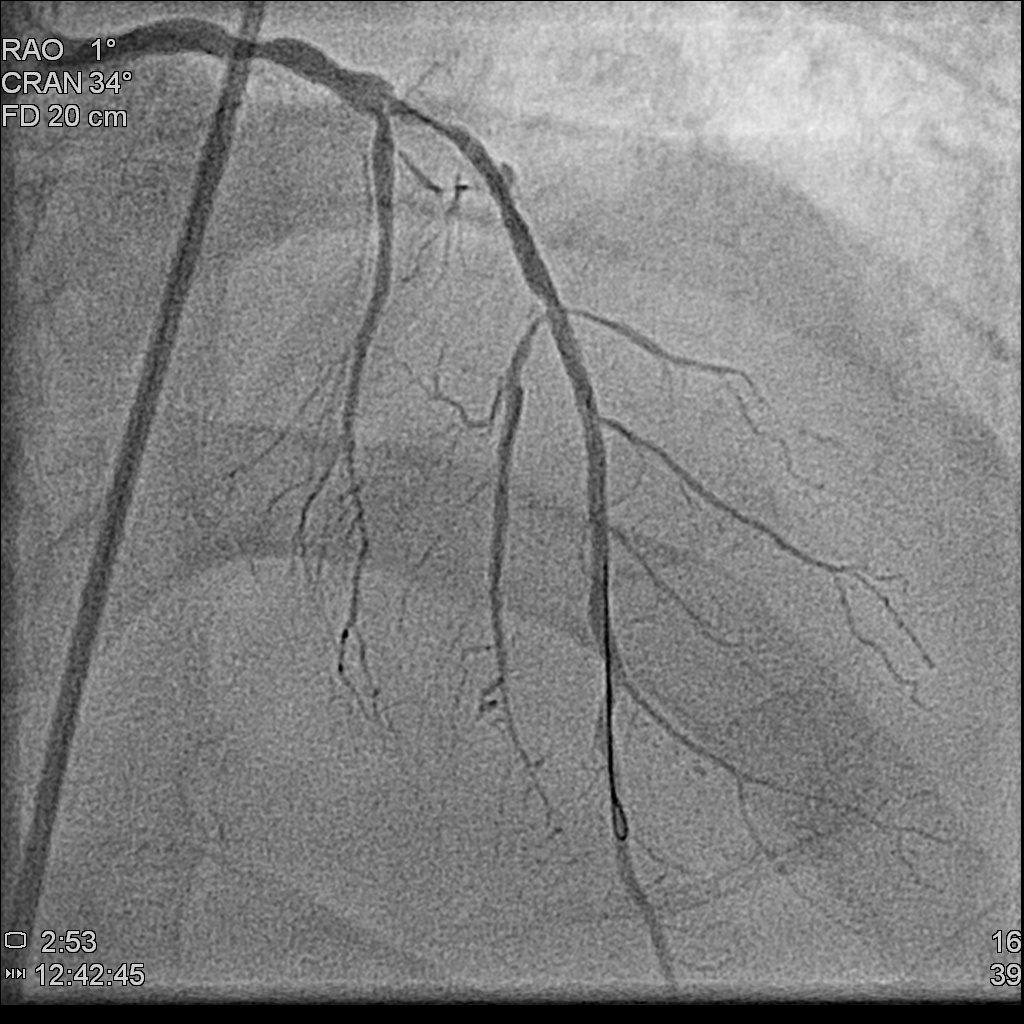
What is the optimal strategy revascularization for this patient? (1.CABG 2.PCI to left-main LAD lesion first then RCA ? 3.PCI to RCA lesion then left main-LAD ? Other options?)In 1st PCI procedure,we managed his RCA lesion first by antegrade approach.We used Miracle 6 guidewire and Conquest Pro guidewire.The microcatheter was successfully advanced into the lesion. The Fielder FC guidewire was then successfully navigated through the lesion.Dilatation with various sizes of PTCA balloon. 1.0x10mm, 2.5x15mm, 3.5x30mm).OptiCross IVUS showed vessel diameter ranging from 4.5 to 5mm over a length of 53mm. Two Synergy 4.0x38mm and 4.0x32mm drug-eluting stents (DES) were deployed at the middle to distal and proximal to middle RCA, respectively. Post-dilatated with 5.0x8mm NC Trek. The final IVUS confirmed excellent stent apposition and no residual stenosis.
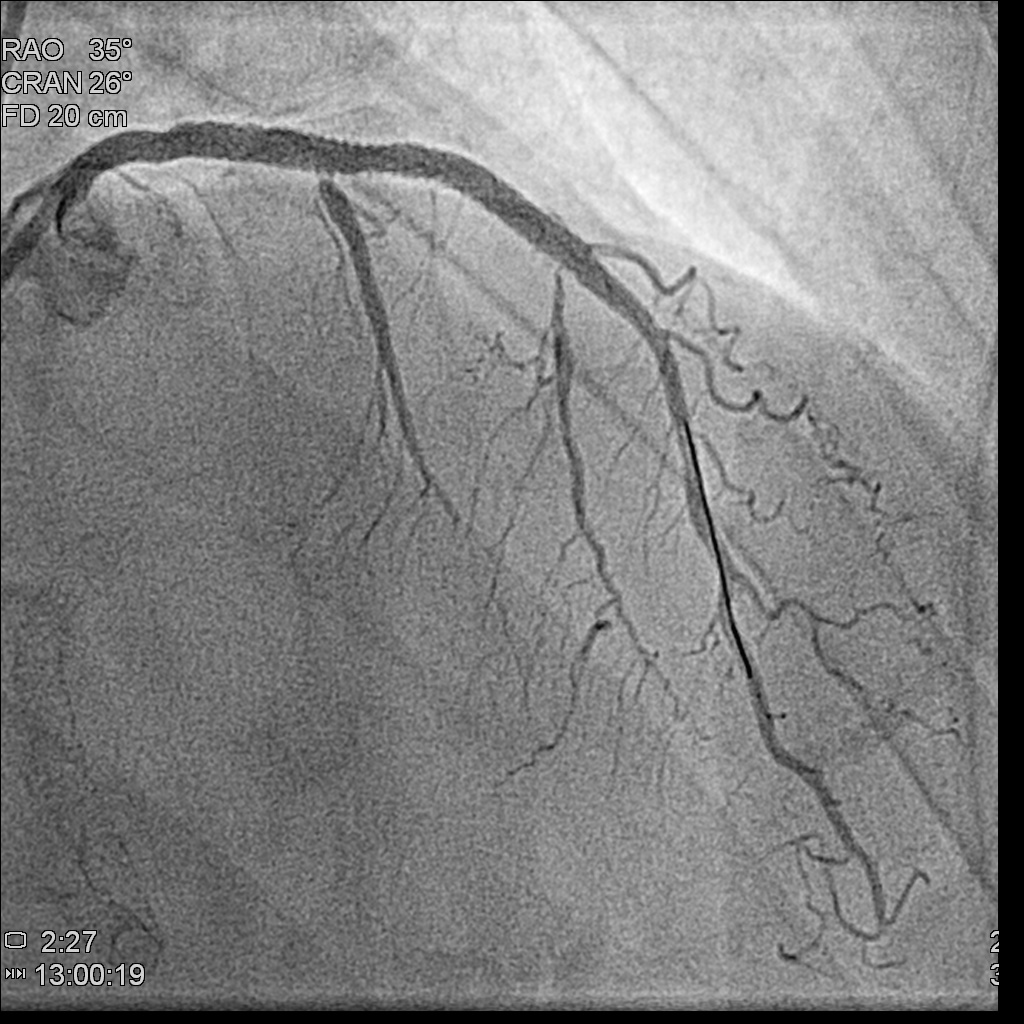
Few months later, we saw the collateral vessels providing RCA previously were all disminished and the RCA flow was fine .We attempted his LM-LAD lesion with Miracle 6 and Gaia II guidewires.The microcatheter successfully entered the LAD stenotic segment. The Gaia II guidewire was negotiated through the point successfully. Dilatation was performed with 2.5x15mm,3.0x30mm Trek balloons sequentially. A Synergy 3.5x48mm DES was deployed from the middle left main (LM) to the middle LAD, followed by post-dilatation with 4.5x15mm NC Euphora balloon. The final result showed acceptable results

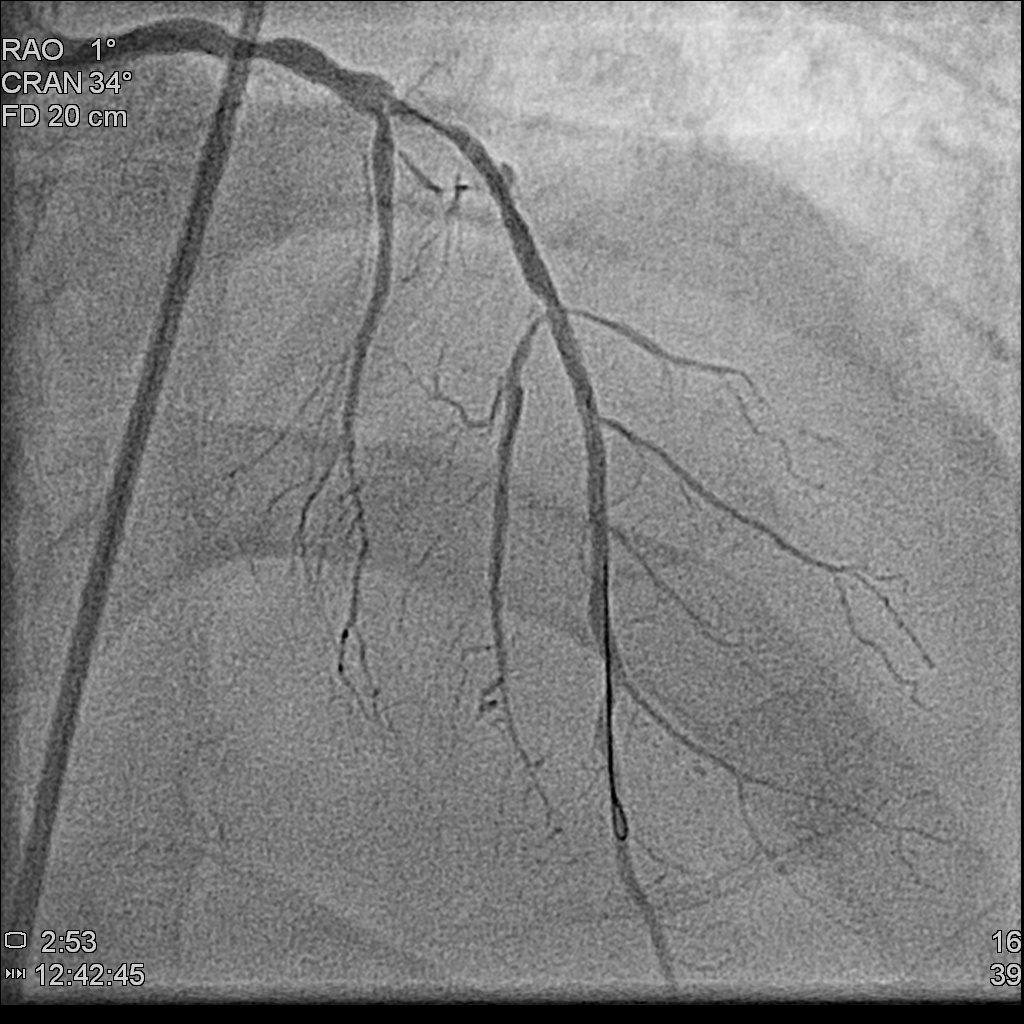
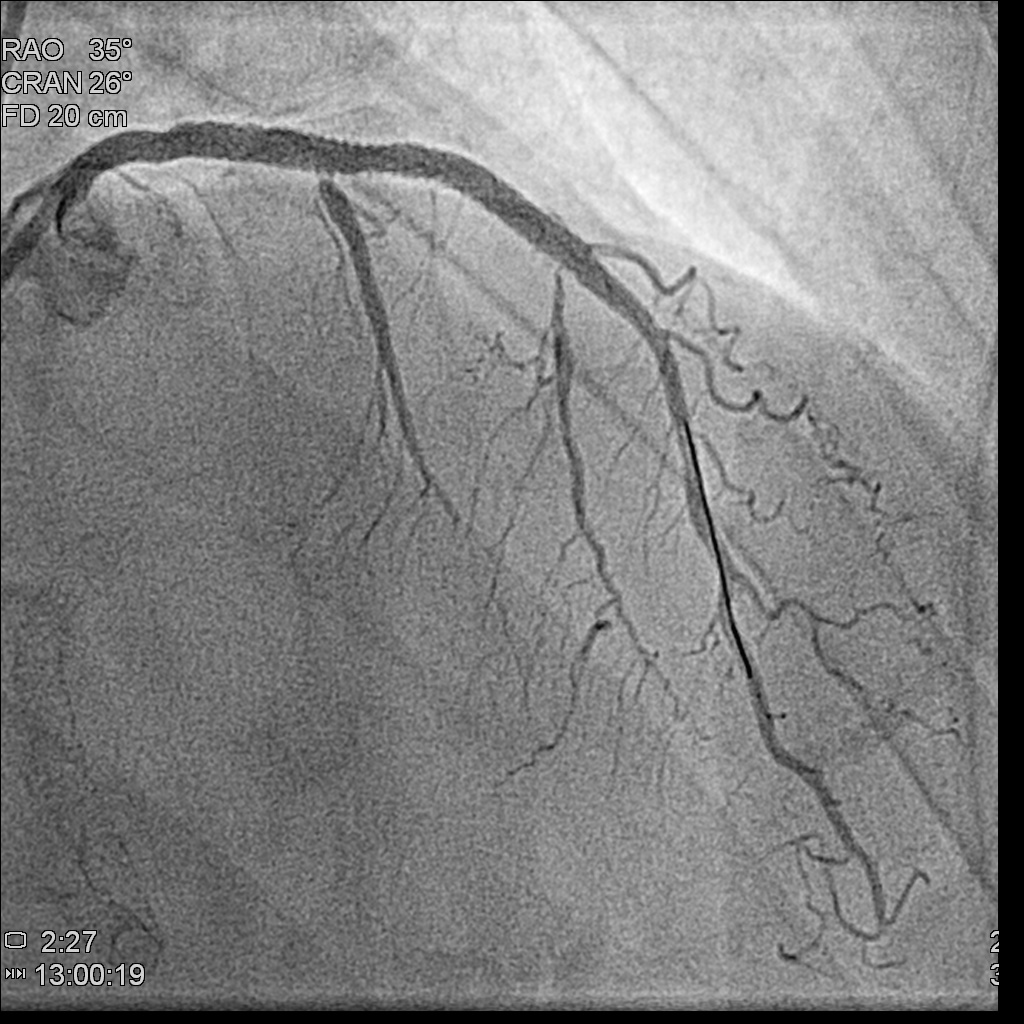
Few months later, we saw the collateral vessels providing RCA previously were all disminished and the RCA flow was fine .We attempted his LM-LAD lesion with Miracle 6 and Gaia II guidewires.The microcatheter successfully entered the LAD stenotic segment. The Gaia II guidewire was negotiated through the point successfully. Dilatation was performed with 2.5x15mm,3.0x30mm Trek balloons sequentially. A Synergy 3.5x48mm DES was deployed from the middle left main (LM) to the middle LAD, followed by post-dilatation with 4.5x15mm NC Euphora balloon. The final result showed acceptable results

Case Summary
The congenital absence of LCx with a super-dominant RCA is quite rare and presents a significant challenge for PCI, especially when multiple vessels are involved. The optimal strategy in such cases would be to first manage the dominant RCA, taking advantage of the collateral supply from the opposite side, and initially attempt the antegrade approach. If the antegrade approach to the RCA fails, the patient can still rely on the collateral circulation, allowing for a change of strategy right afterwards.


