Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-136
A Nightmare Before My Birthday, Losing It Before Celebrating - Our Approach of Stent Retrieval
By Navindran Selavraju, Surenthiran Ramanathan, Asri Ranga Abdullah Ramaiah, Kamaraj Selvaraj, Glendon Lau Seng Kiong, Abdul Kahar Abdul Ghapar
Presenter
Navindran Selavraju
Authors
Navindran Selavraju1, Surenthiran Ramanathan1, Asri Ranga Abdullah Ramaiah1, Kamaraj Selvaraj1, Glendon Lau Seng Kiong1, Abdul Kahar Abdul Ghapar1
Affiliation
Hospital Sultan Idris Shah Serdang, Malaysia1,
View Study Report
TCTAP C-136
Coronary - Complication Management
A Nightmare Before My Birthday, Losing It Before Celebrating - Our Approach of Stent Retrieval
Navindran Selavraju1, Surenthiran Ramanathan1, Asri Ranga Abdullah Ramaiah1, Kamaraj Selvaraj1, Glendon Lau Seng Kiong1, Abdul Kahar Abdul Ghapar1
Hospital Sultan Idris Shah Serdang, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
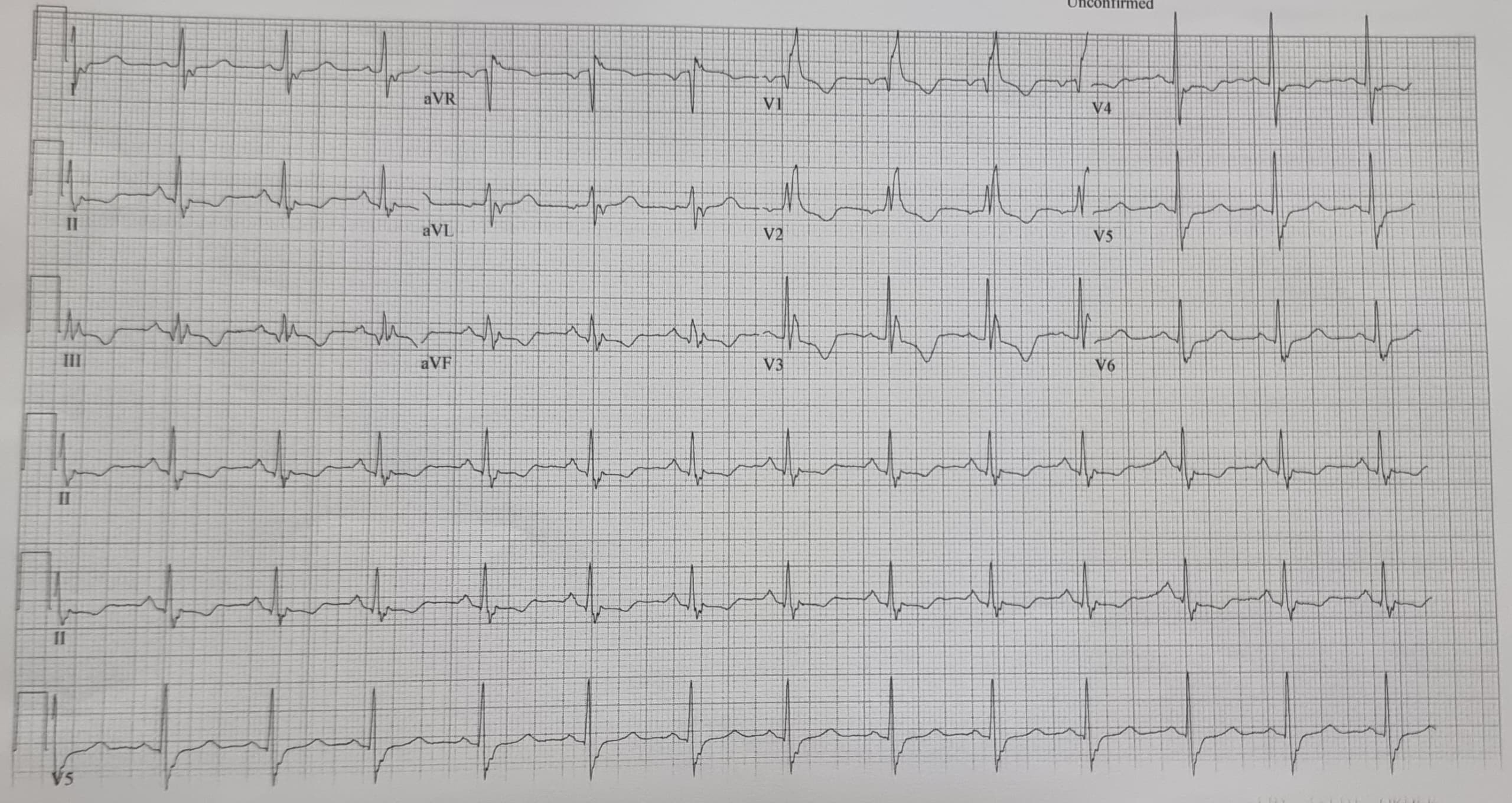
A 74 Chinese Female with Dyslipidemia and Hypertension with chest discomfort for 2 days presented to our emergency department. On arrival her pressure was 122/72, pulse was 68. Clinical examination showed no pedal edema and heart sounds were unremarkable.ECG showed RBBB, T inversion V1- V5, ST depression II, III, avF. Bedside ECHO was 56 %. Her HAS-BLED score was 2. She previously underwent a CT angiogram at a private centre which showed severe stenosis of 80% over the LAD.
Relevant Test Results Prior to Catheterization
Her Blood workup revealed Hemoglobin of 12.2g/dl, white cell count of 4.4, and platelet count of 210. Her Liver function test was unremarkable. Her Urea was 6.1, and creatinine was 78. Her lipid profile revealed total cholesterol of 4.5, with LDL of 2.6, HDL of 1.58, and TG of 0.65. Her HBA1c was 6.5%. Troponin I was 13. ProBNP was less than 60.
Relevant Catheterization Findings
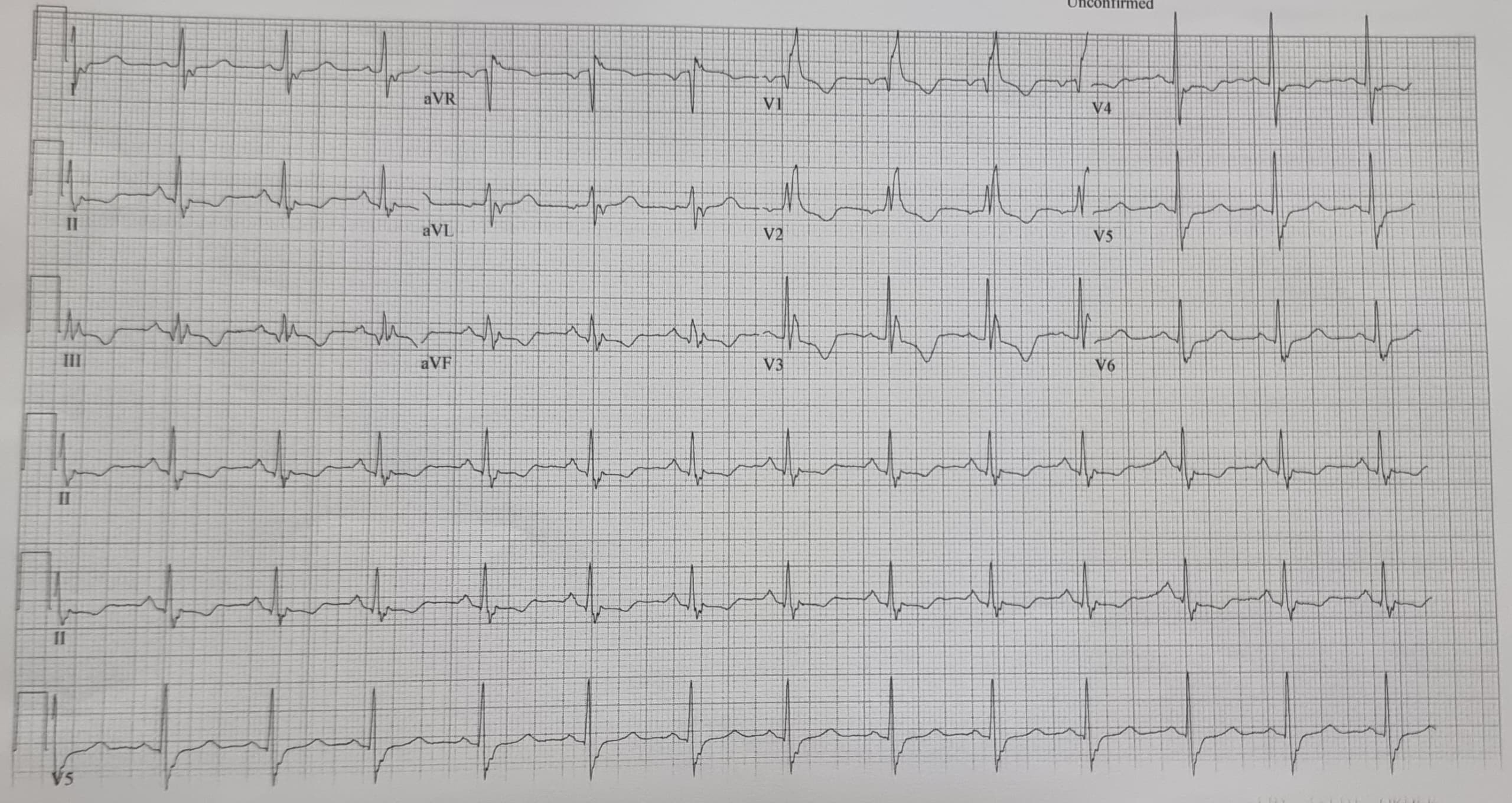
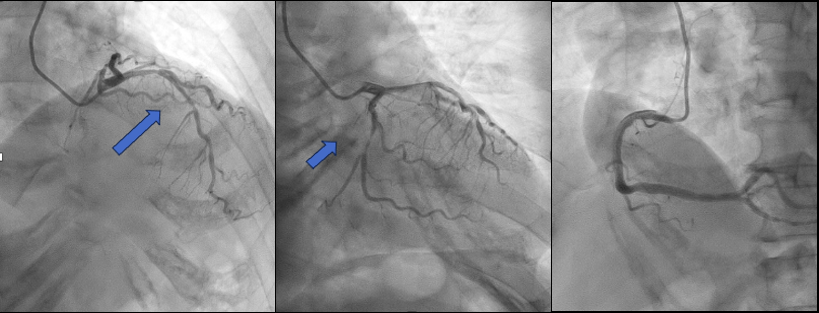
An angiogram revealed that the Left main was smoothLAD --proximal to mid-60 %, LCX showing mid-diffuse disease - 80-90%. RCA was smooth. Our strategy was PCI to LCx and RFR to LAD, and if physiologically significant, PCI to LAD as well.
Interventional Management
Procedural Step
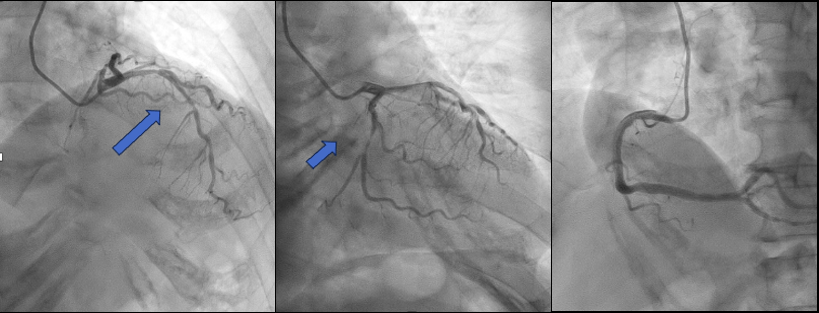
LMS engaged with EBU 3.0 6FR- LCX with Sion Blue and Runthrough Floppy to LAD. After successful DCB SeQuent Please 2.75mm x 30 to MLCx, RFR to LAD showed 0.81-significant lesion. Predilated LAD with 2.75x20mm Scoreflex up to 18atm. However, there was a Type B dissection, so decided to stent mLAD with
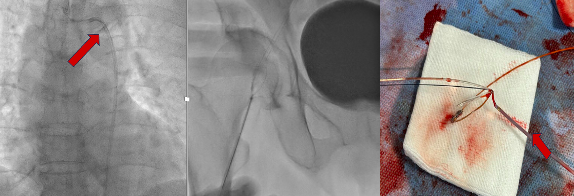
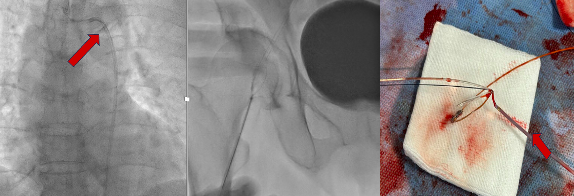
Case Summary
Stent dislodgement is a rare but serious complication. Transradial is preferred but limitations include the small size of the radial artery and the risk of spasm restricting the ability to upsize in sheath size. The transradial approach may be suitable for non-critical coronary segments where the stent is crushed against the coronary vessel wall. For LMS or bifurcation lesions, transfemoral may be more suited. Failure to retrieve the dislodged stent can result in several complications,including stent thrombosis, myocardial infarction, embolic stroke, and death. Although there are a few techniques available, operators should customise the best-suited method to minimise the risk of complications


