Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-143
IVUS Guided Intervention: Diffuse LIMA Dissection During PCI
By Chenan Chao, Hsien-Li Kao
Presenter
Chenan Chao
Authors
Chenan Chao1, Hsien-Li Kao1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-143
Coronary - Complication Management
IVUS Guided Intervention: Diffuse LIMA Dissection During PCI
Chenan Chao1, Hsien-Li Kao1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 69-year-old male has a history of diabetes mellitus, dyslipidemia, and hypertension. He received coronary artery bypass grafting in 2000, followed by multiple percutaneous coronary intervention and stenting procedures for in-stent restenosis and chronic total occlusion. This time, he presents with intermittent chest tightness in the past six months.
Relevant Test Results Prior to Catheterization
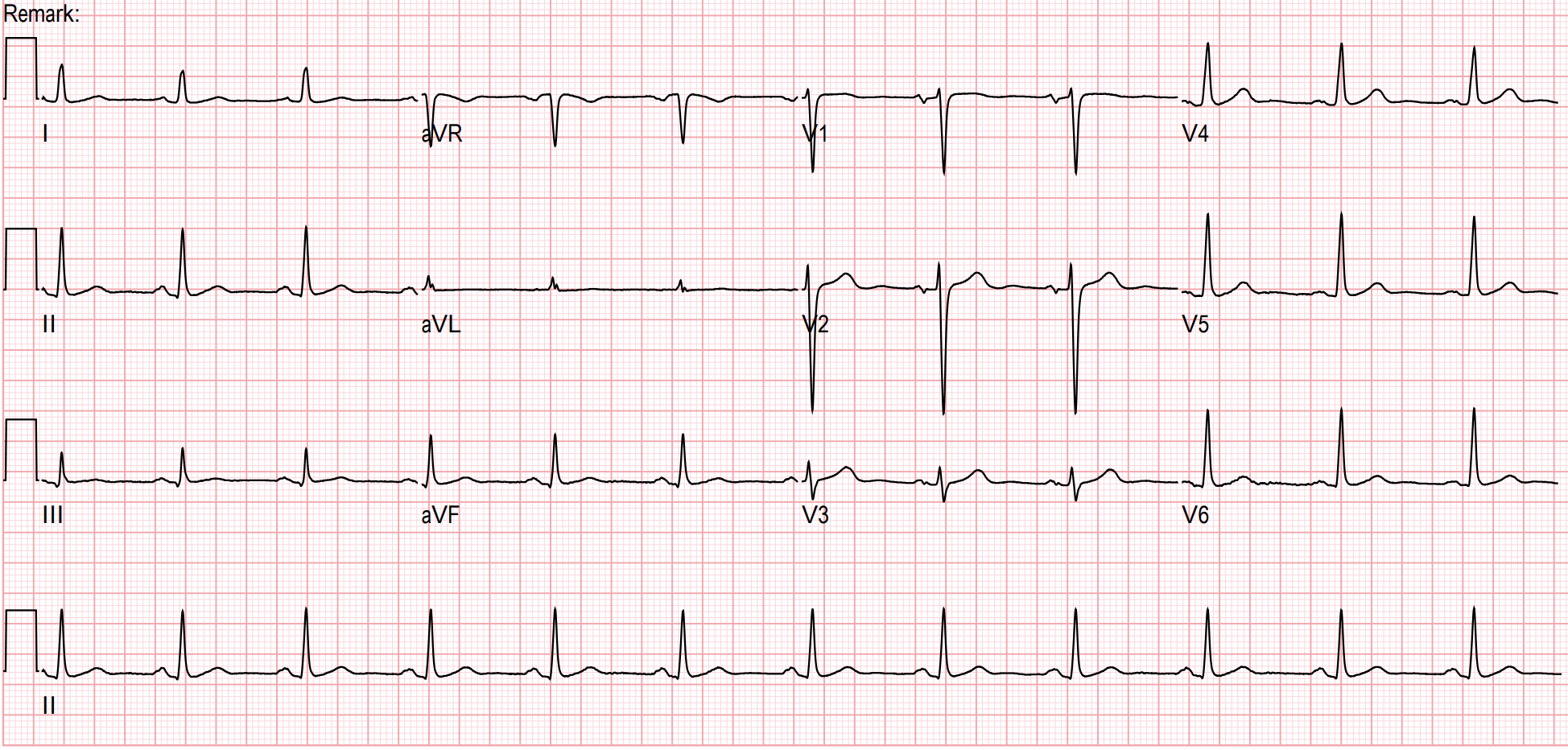
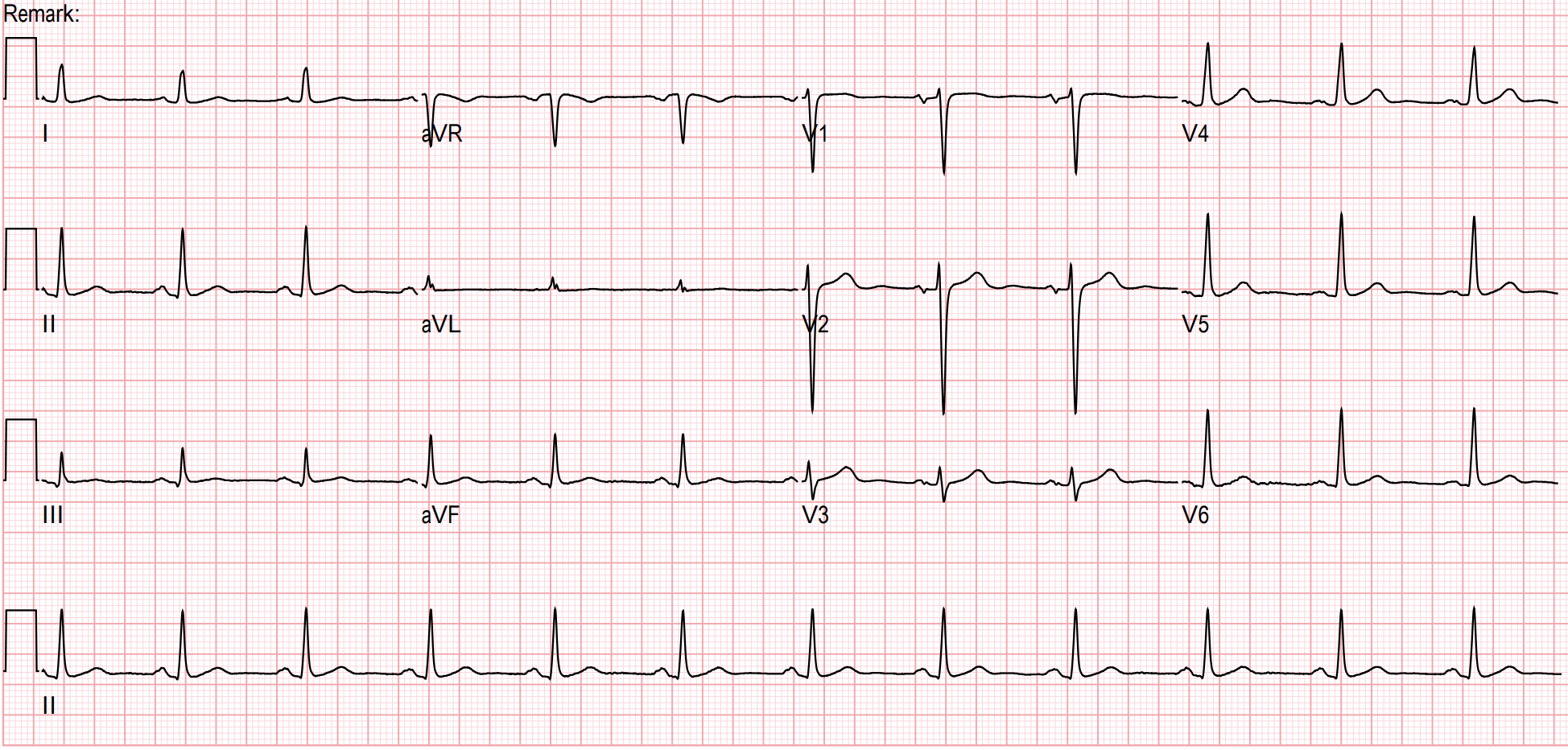
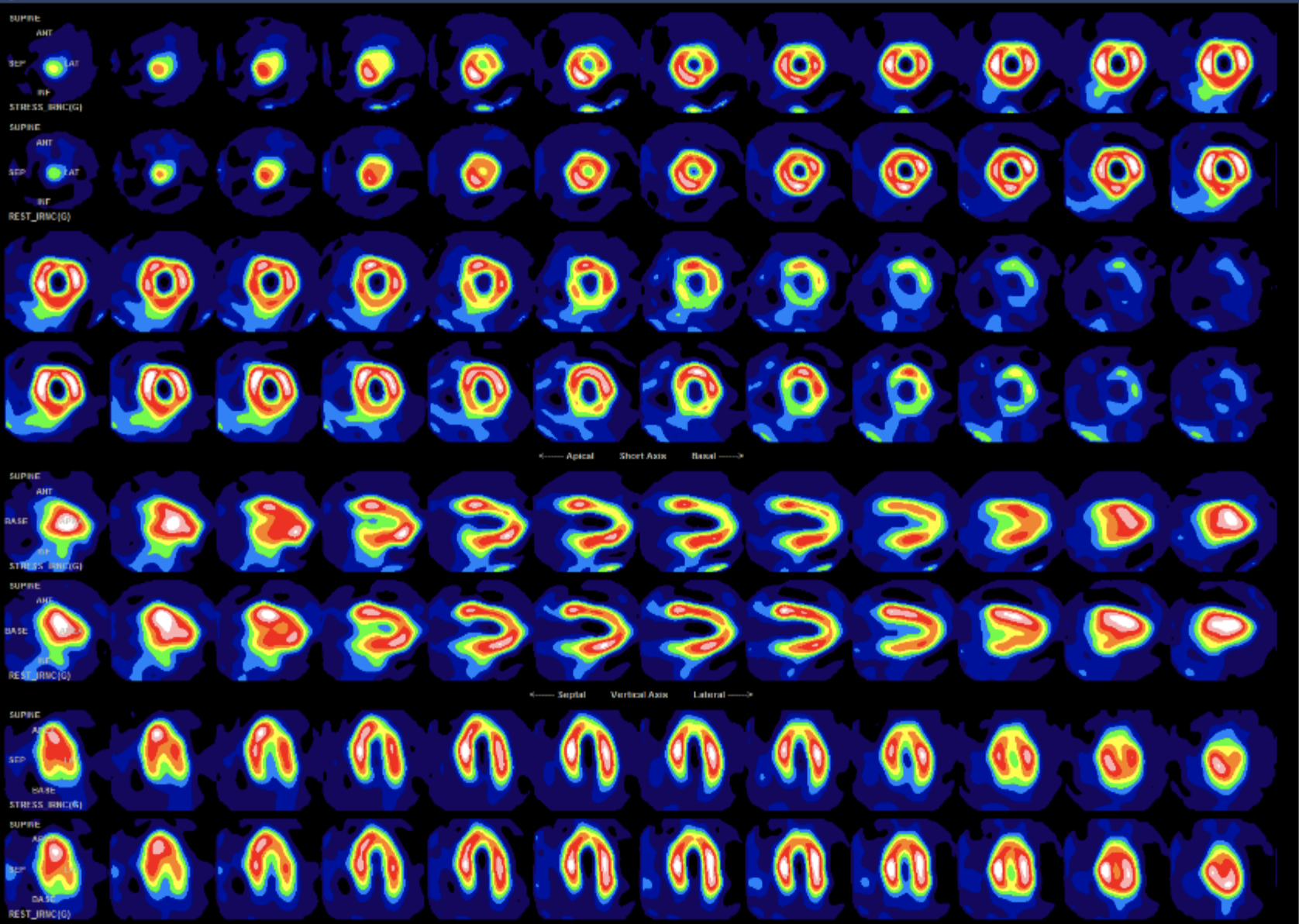
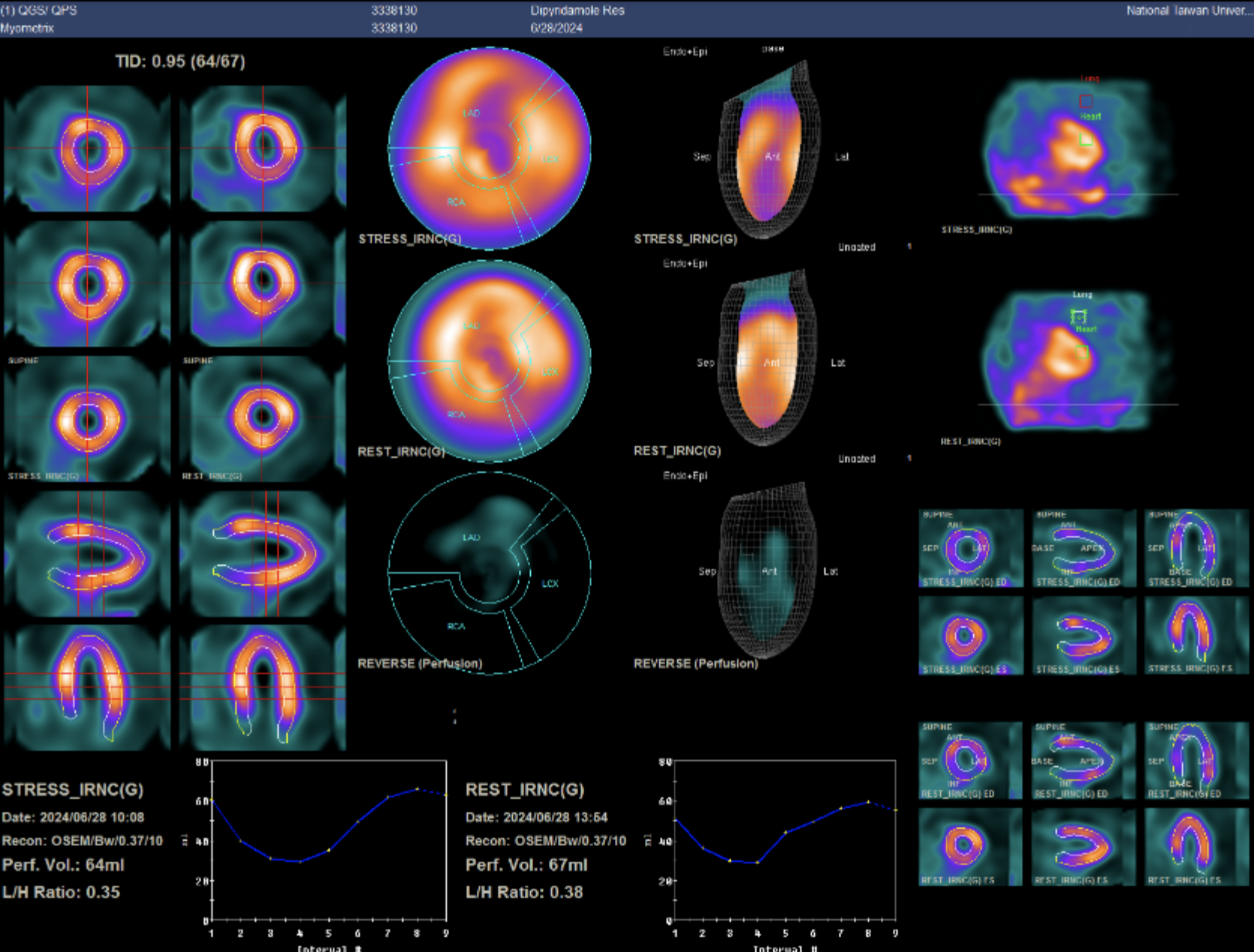
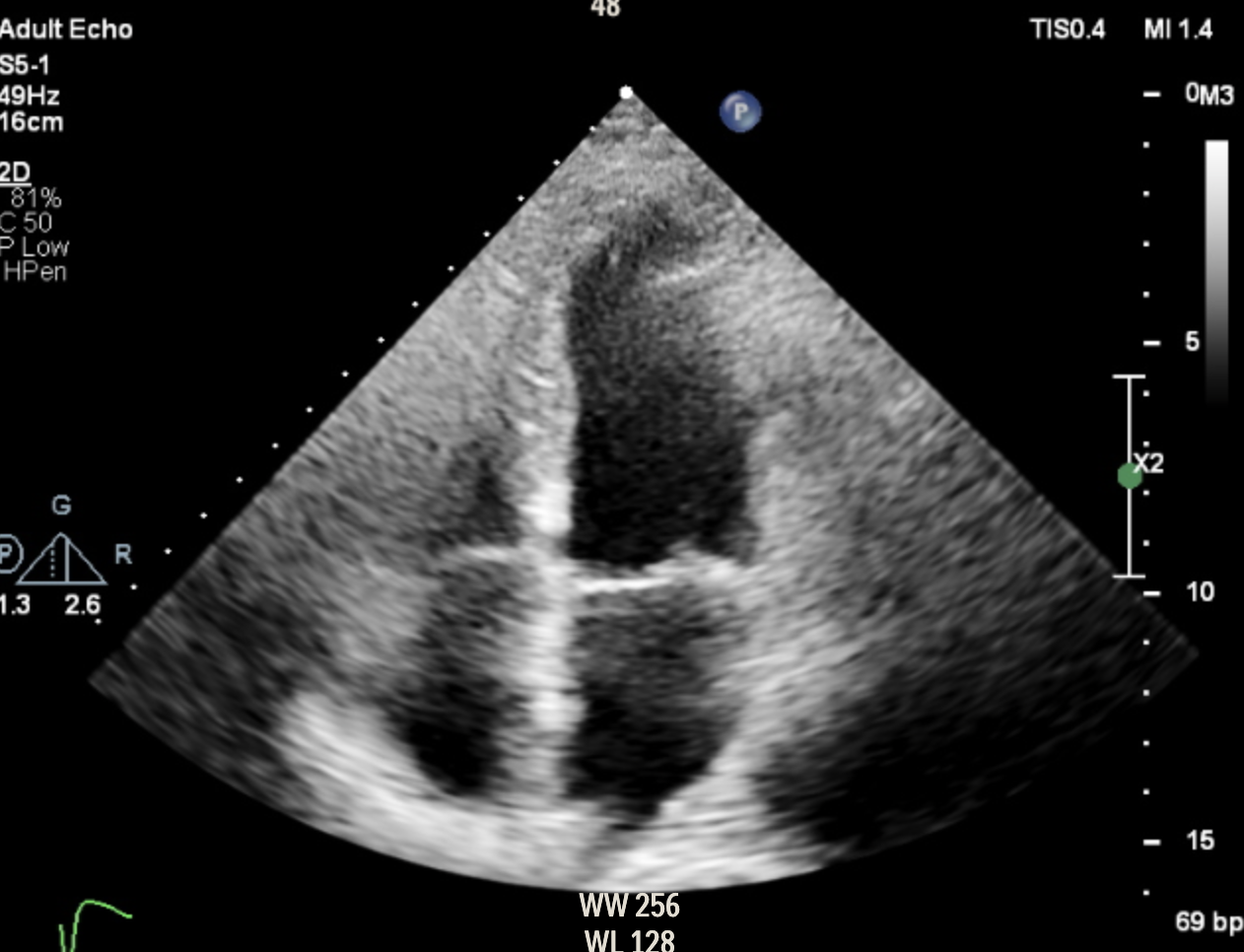
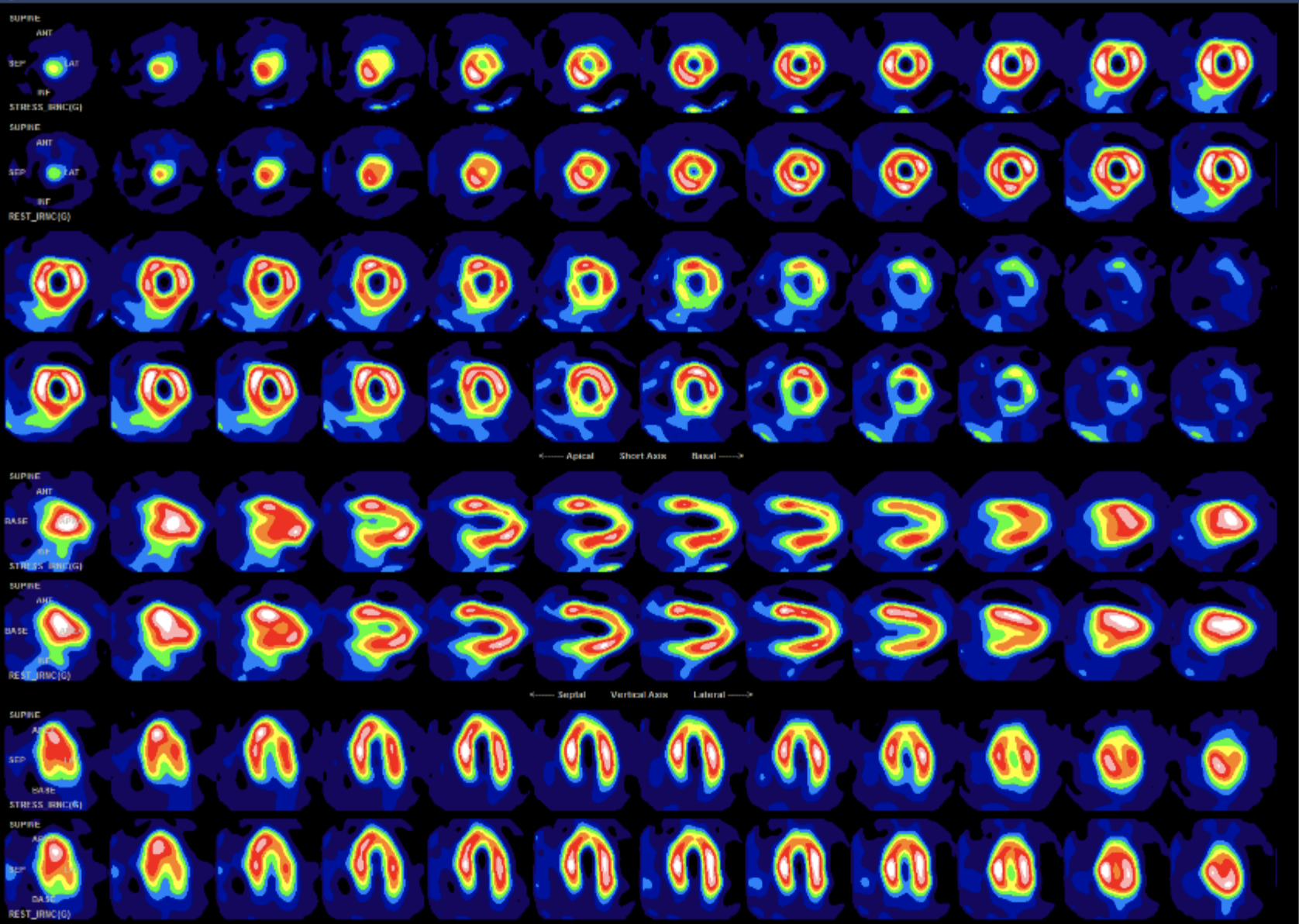
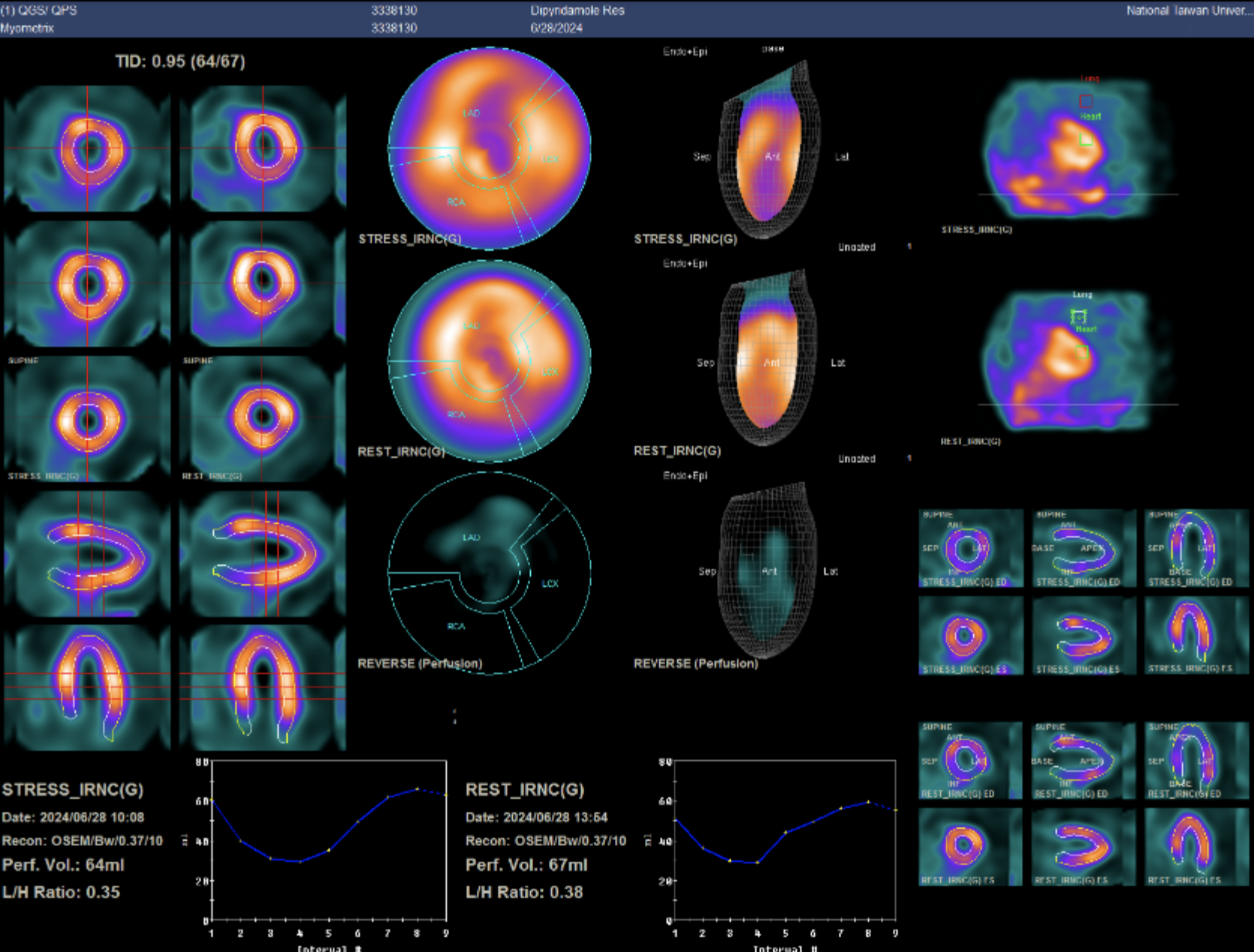
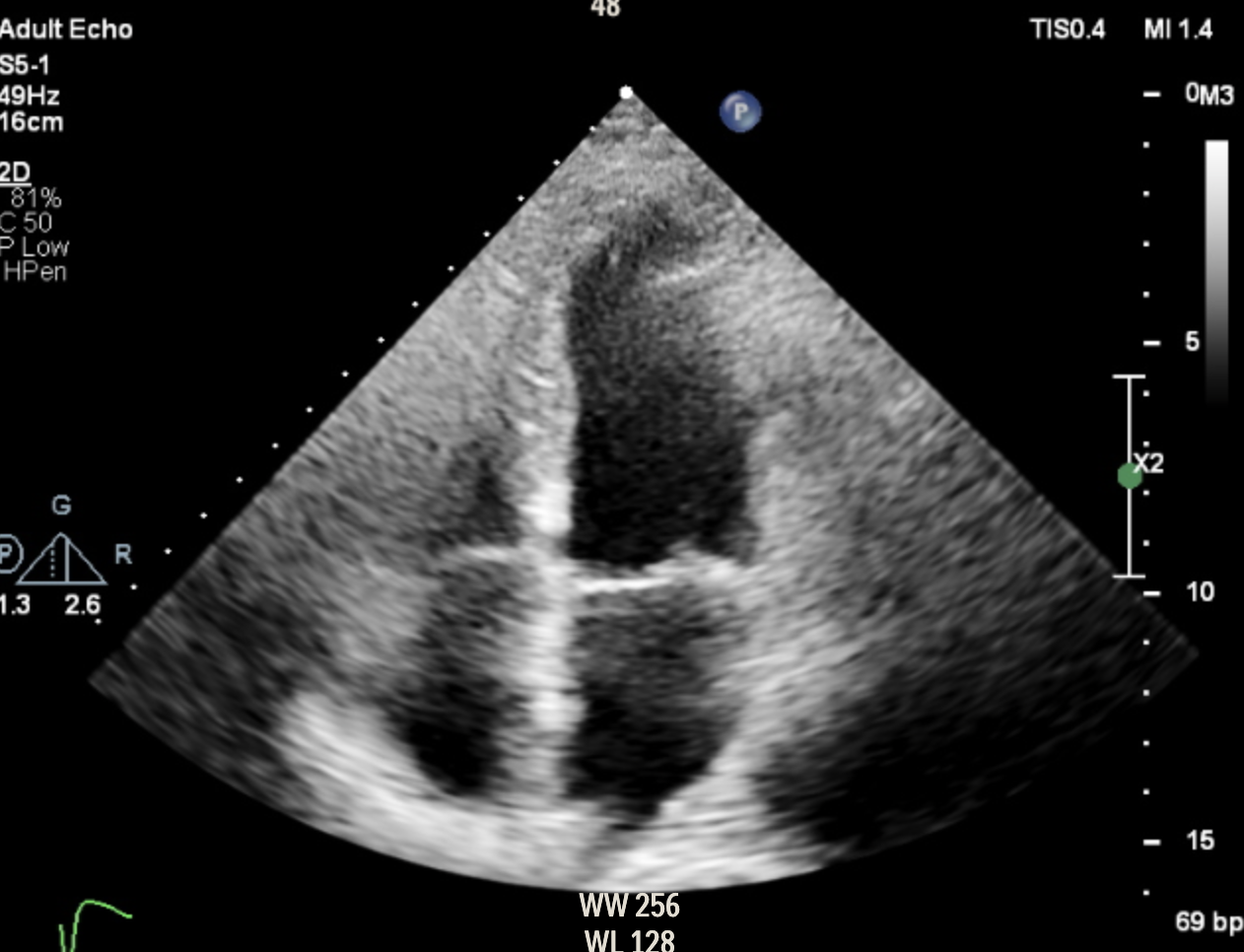
Thallium scan demonstrated reduced flow reserve at the apex, basal anteroseptum, and mid anterior wall, with a summed stress score of 9%. Treadmill test was positive for ischemia, and TTE showed preserved LVEF (61%) with mild-moderate TR.
Relevant Catheterization Findings
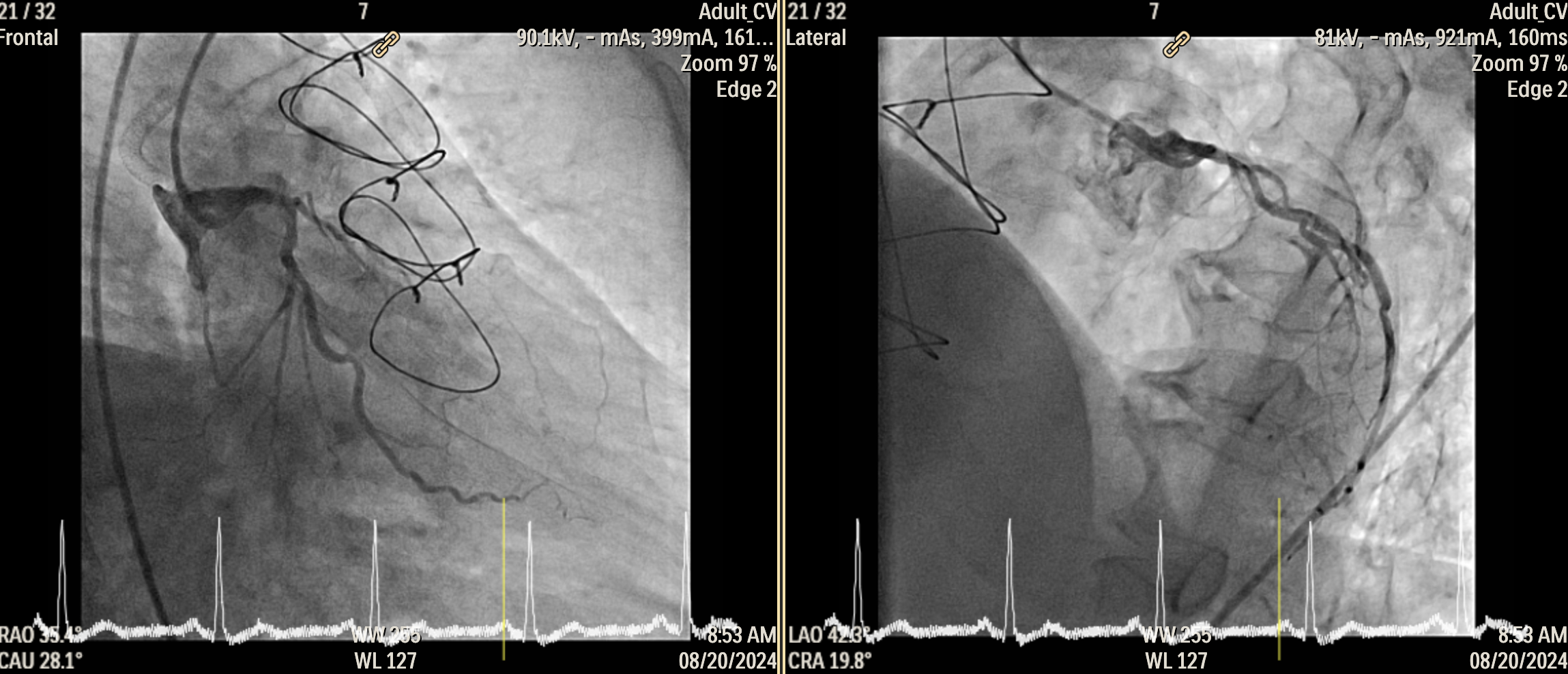
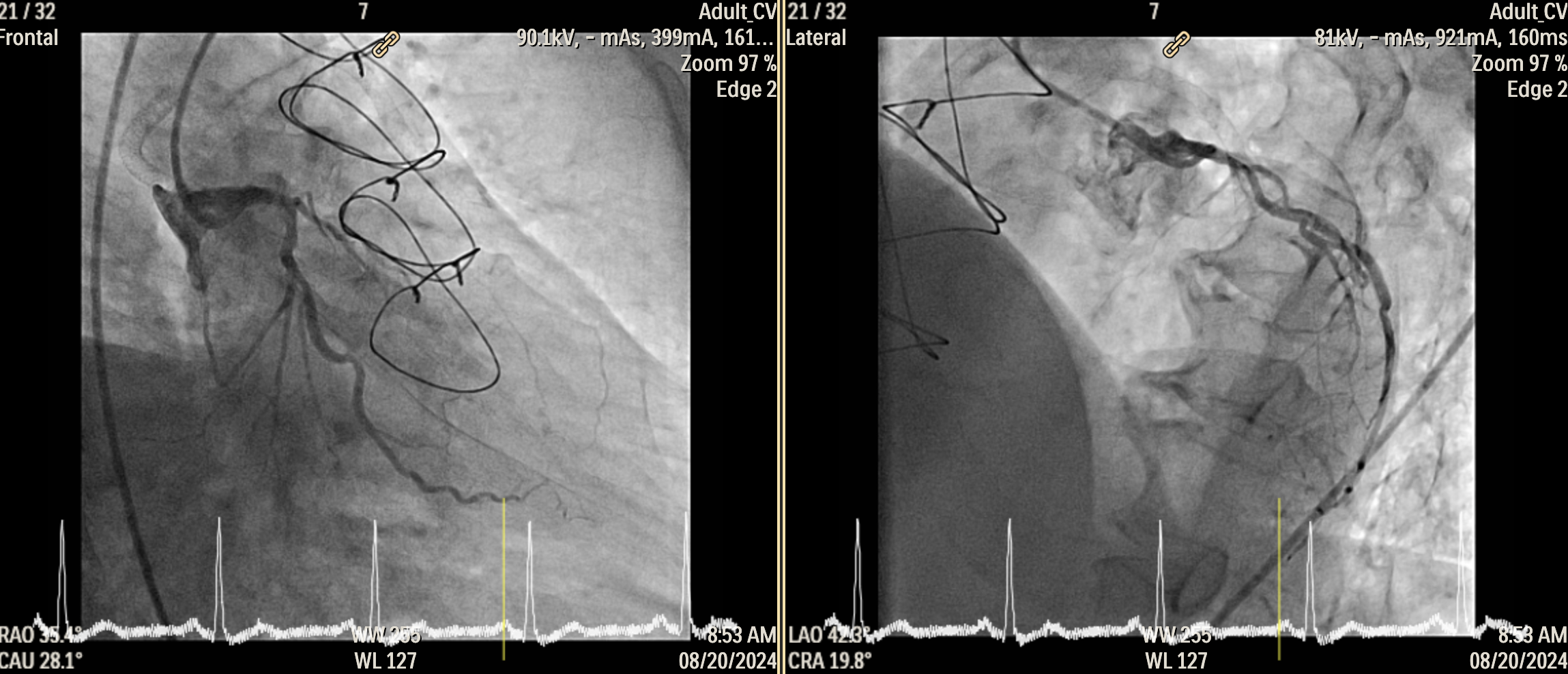
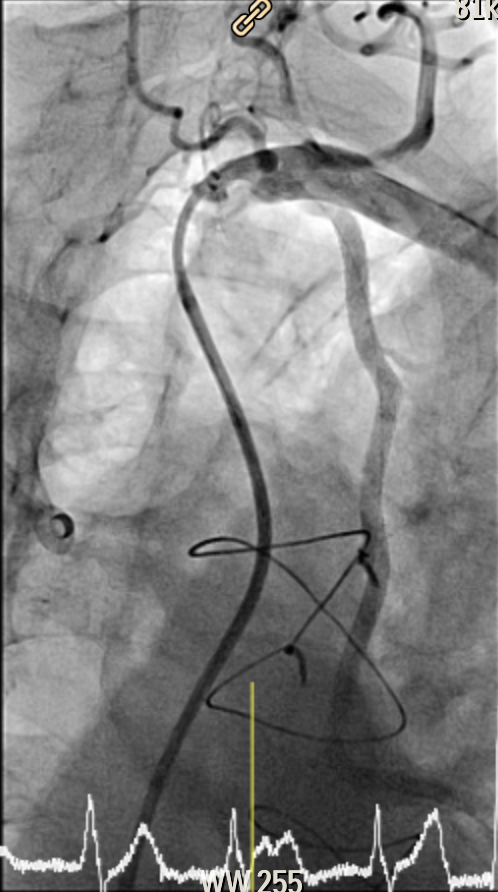
Angiography revealed proximal stenosis of the left internal mammary artery (LIMA) graft, which supplies both the diagonal branch and distal left anterior descending (LAD) artery, with no in-stent restenosis (ISR) in right coronary artery (RCA) and left circumflex (LCX) vessels. Two saphenous vein grafts supporting RCA and LCX were totally occluded according to angiography two years ago.


Interventional Management
Procedural Step
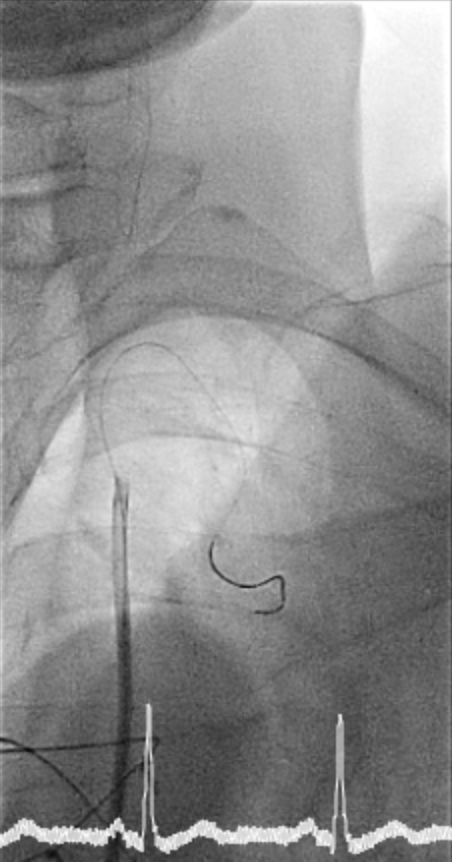
1. We engaged 6Fr JR4 guiding catheter proximal to, but near the LIMA ostium and positioned a Terumo Runthrough Extra floppy guidewire into the distal LIMA. Intravascular ultrasound (Boston Scientific IVUS OptiCross HD) imaging identified a focal plaque in the proximal LIMA. However, the patient suddenly developed chest pain, and LIMA flow was impaired. Vascular spasm was highly suspected, so nitroglycerin was administered, followed by balloon angioplasty (2.5 x 15 mm) up to 6 atm. However, there was no improvement in LIMA flow.
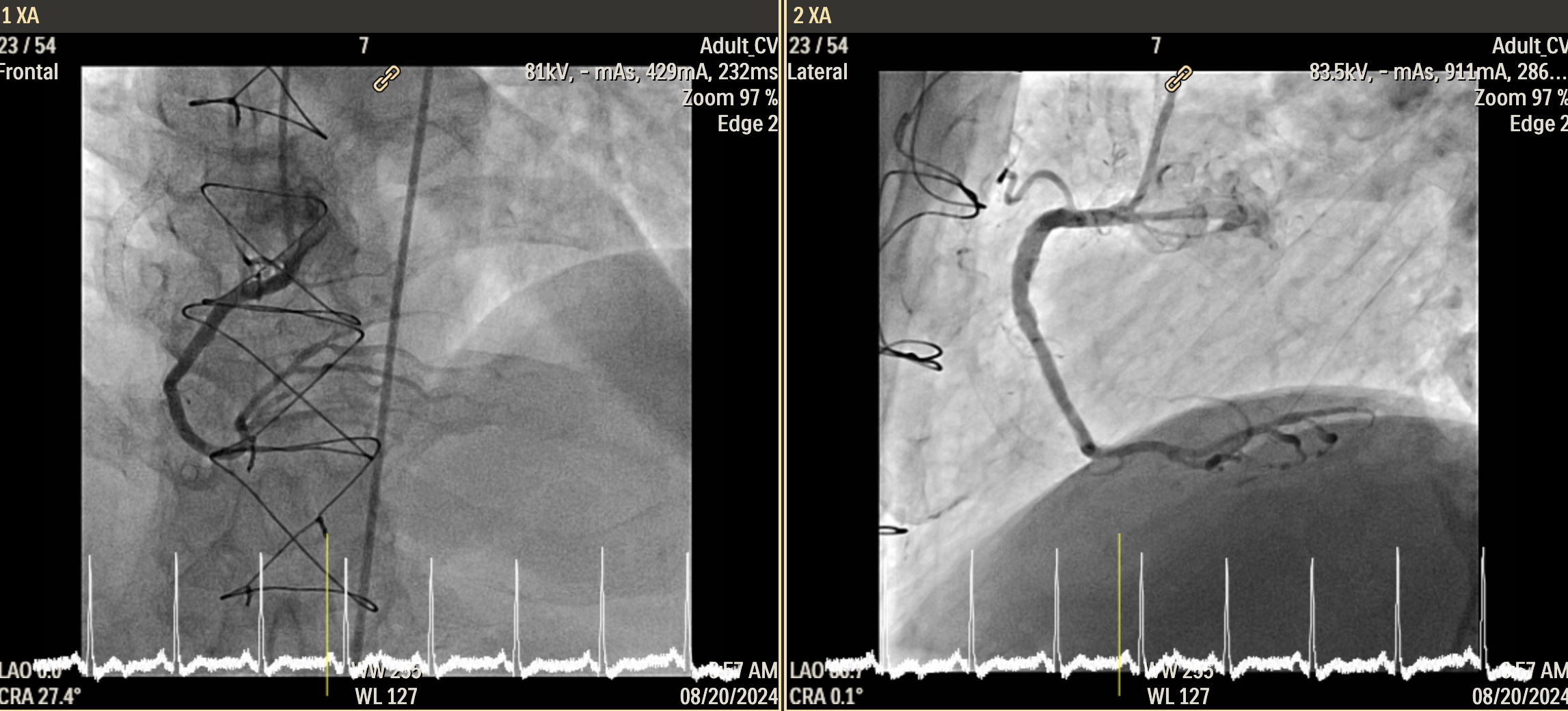
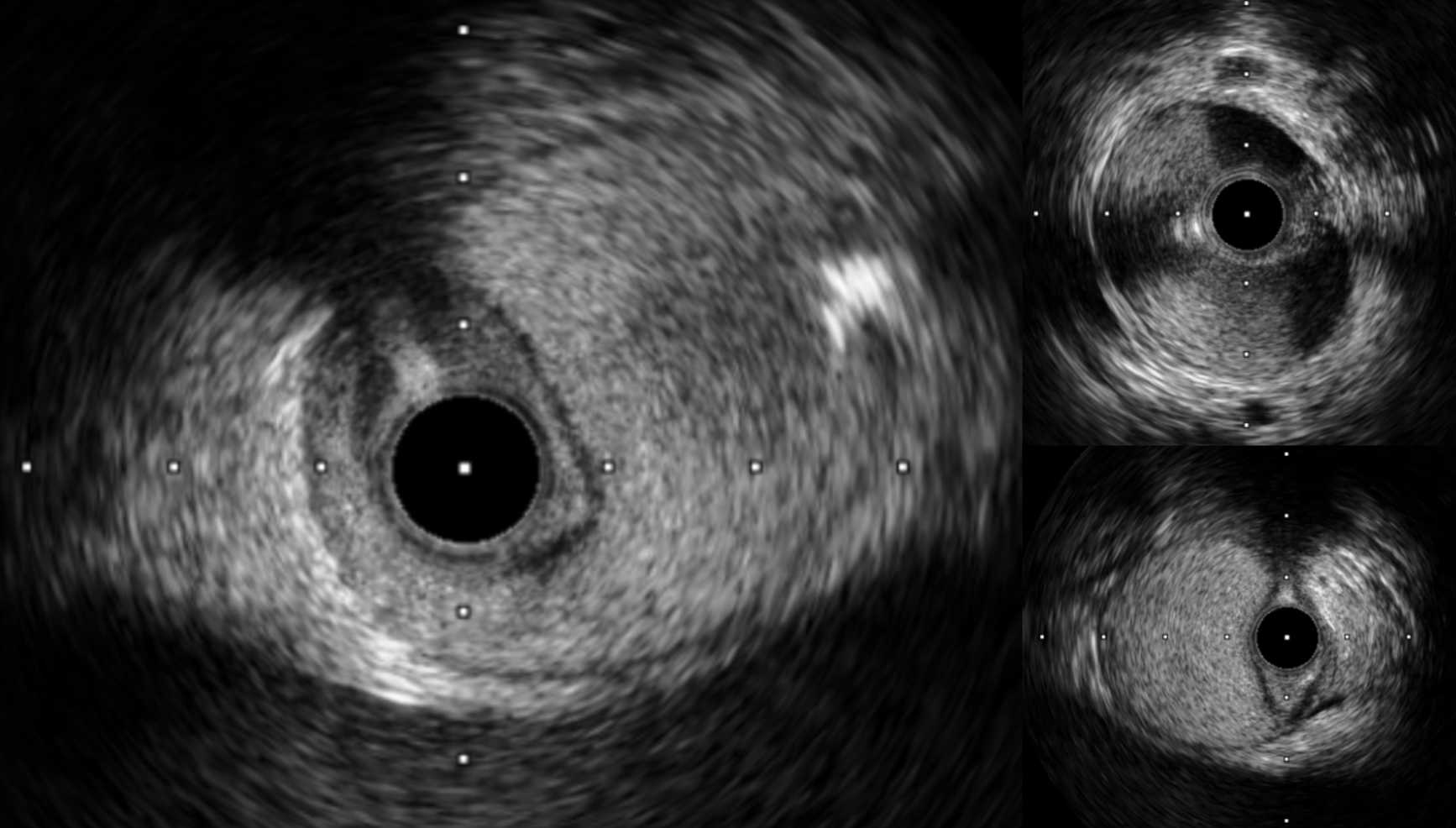
2. To confirm wire position, a double-lumen catheter (ASAHI SASUKA Catheter) was advanced to the distal LIMA, showing the wire is in the true lumen. We also exchanged the wire for a flexible wire (ASAHI SUOH 03) to reduce the risk of further vascular spasm. A repeat IVUS scan revealed diffuse dissection with hematoma in the LIMA, compromising the true lumen.
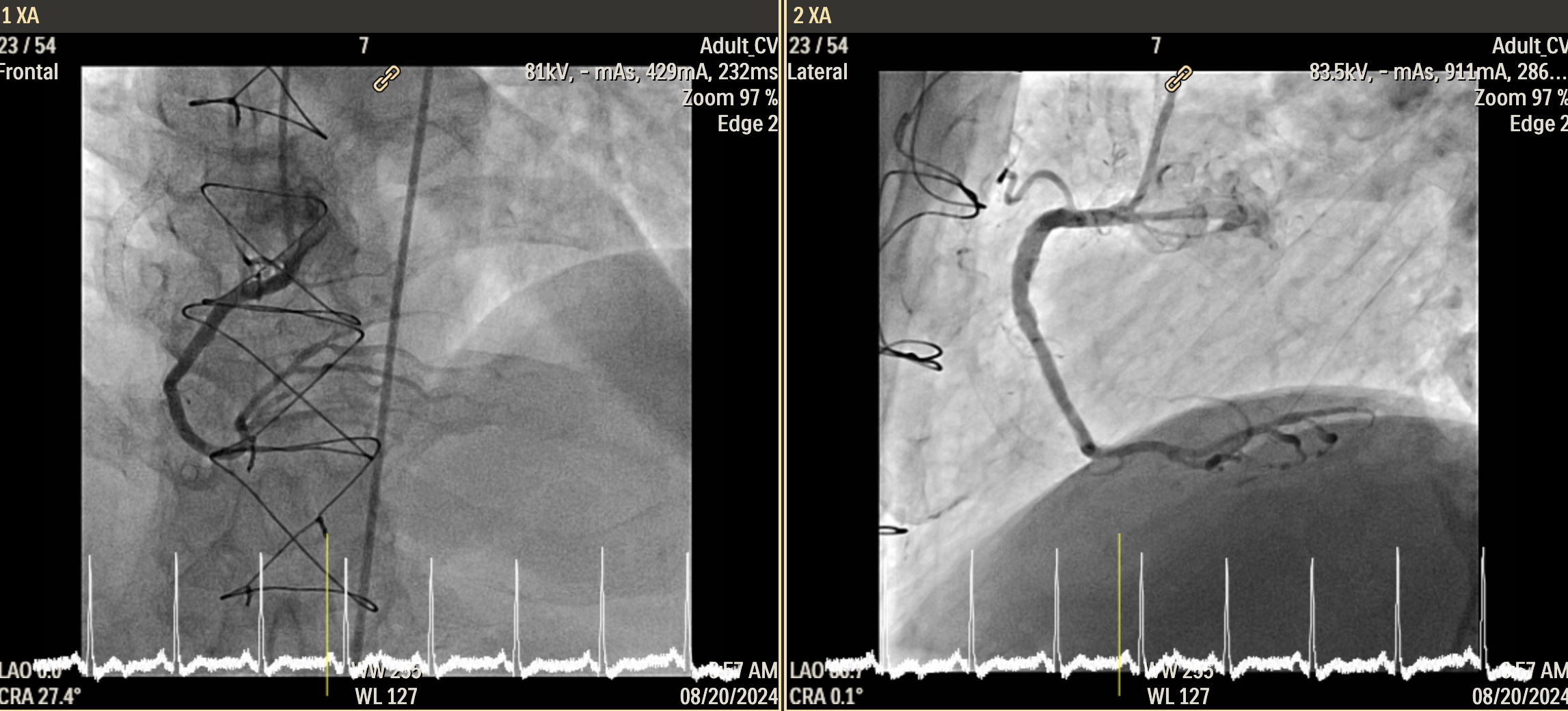
3. A 3.5 x 48 mm drug-eluting stent (DES, Boston Scientific Stent SYNERGY) was deployed in the distal LIMA, followed by another 3.5 x 48 mm DES in the proximal LIMA. Post-dilation was performed with the stent balloon to ensure full apposition.
4. Final IVUS imaging showed persistent minor dissection at the LIMA ostium and proximal axillary artery, while angiography noted subclavian artery dissection with adequate flow. The patient’s chest pain was resolved, and satisfactory final flow (TIMI 3) of the LIMA was achieved.
Case Summary
Guidewire manipulation within the arteries can sometimes cause trauma to the vessel wall and lead to intimal tearing and dissection. In this case, the engaged contrast injection by an autoinjector further exacerbated the dissection, creating a hematoma that compromised the true lumen and impaired blood flow. IVUS guidance was essential in identifying and treating these complications. The patient remained stable after one night of close monitoring in the CCU. This case highlights the complexities of managing graft complications and underscores the critical role of IVUS in diagnosis, restoring vessel integrity and effective flow restoration.


