Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-244
Fulminant Myocarditis Complicated With Recurrent Arrhythmia and Bi-Ventricular Failure Survived Under Micro-Axial Flow Catheter Support
By Kuo Hsuan Hung, Chih-Fan Yeh
Presenter
Kuo Hsuan Hung
Authors
Kuo Hsuan Hung1, Chih-Fan Yeh1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-244
Heart Failure - Mechanical Circulatory Support
Fulminant Myocarditis Complicated With Recurrent Arrhythmia and Bi-Ventricular Failure Survived Under Micro-Axial Flow Catheter Support
Kuo Hsuan Hung1, Chih-Fan Yeh1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
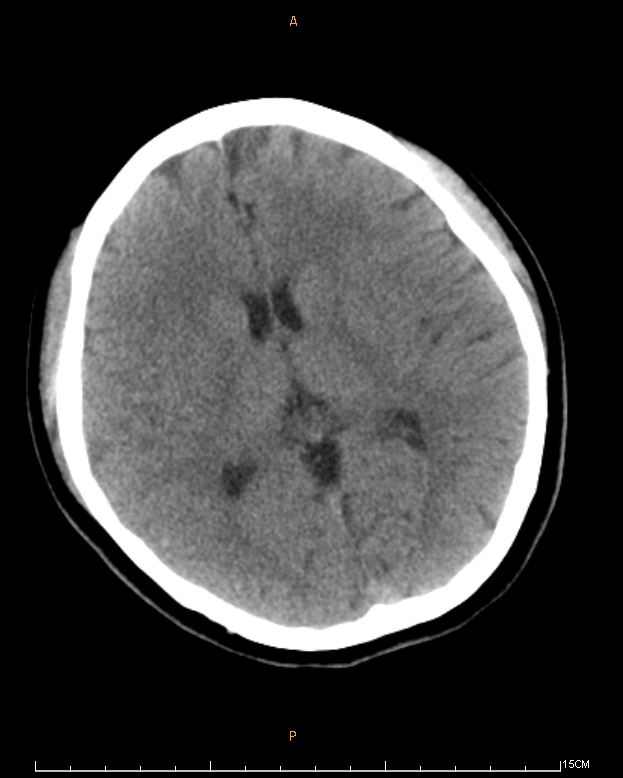
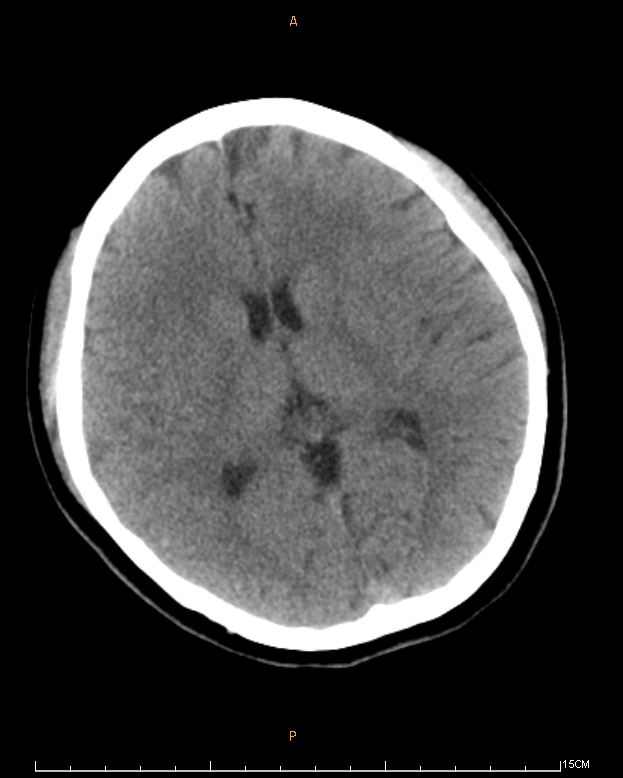
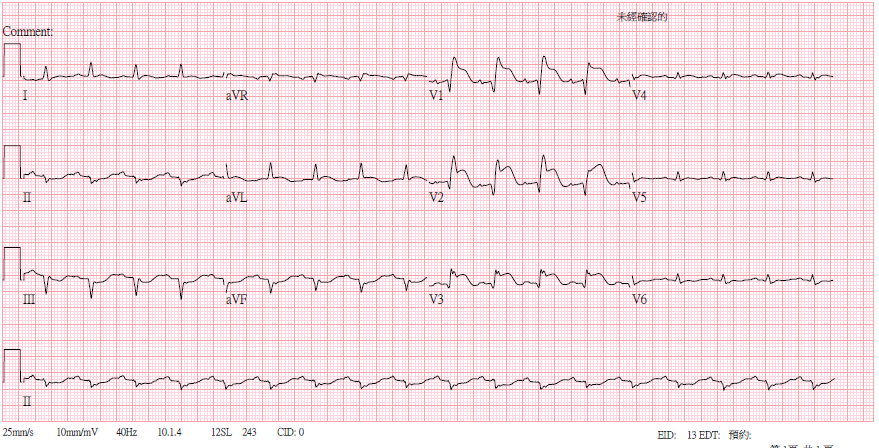
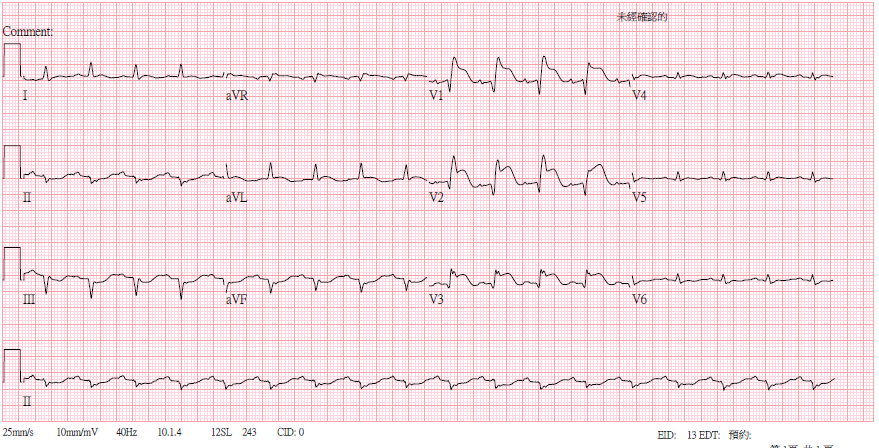
A 24-year-old womanexperienced nausea and abdominal discomfort days before a shortsyncope episode. She was taken to a local hospital. EKG showed sinustachycardia, low QRS voltage, and ST elevation over aVR, V1-3. CT scan of the brain revealed no signs of intracranial hemorrhage. Shewas transferred to our hospital under norepinephrine infusion.
Relevant Test Results Prior to Catheterization
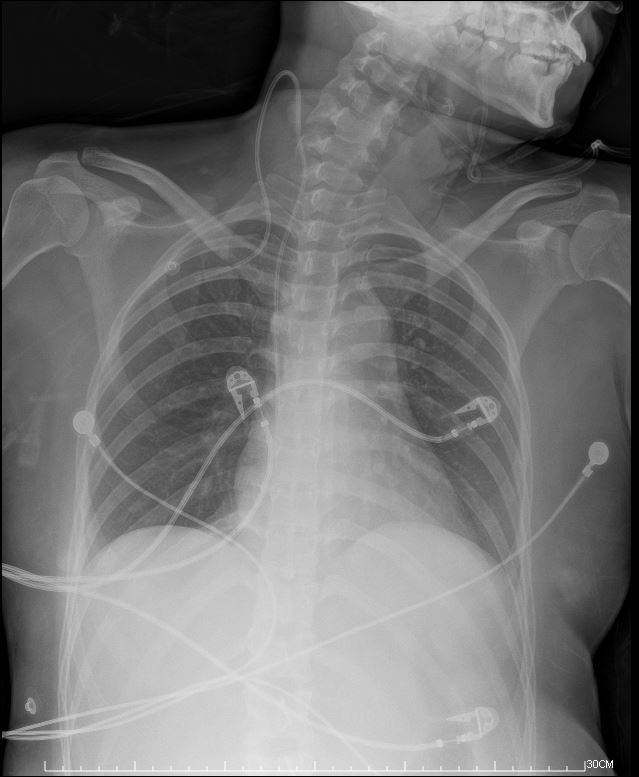
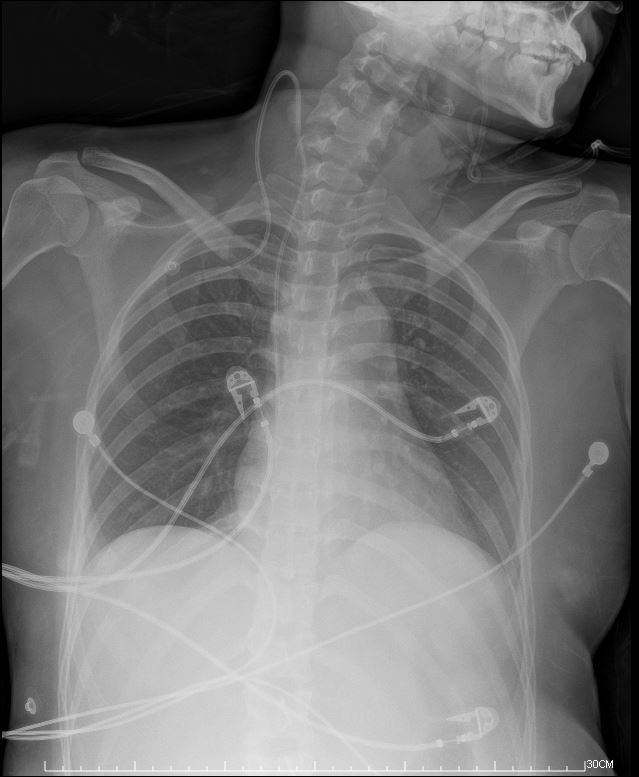
At triage, she wasalert but hypotensive. Labs showed elevated troponin-T and NT-pro BNPlevels and leukocytosis. CXR showed perihilarinfiltrates, and TTE indicated mild LVEF reduction and globalhypokinesia of LV. Given the suspicion of fulminant myocarditis, shebegan IVIG therapy.
Relevant Catheterization Findings
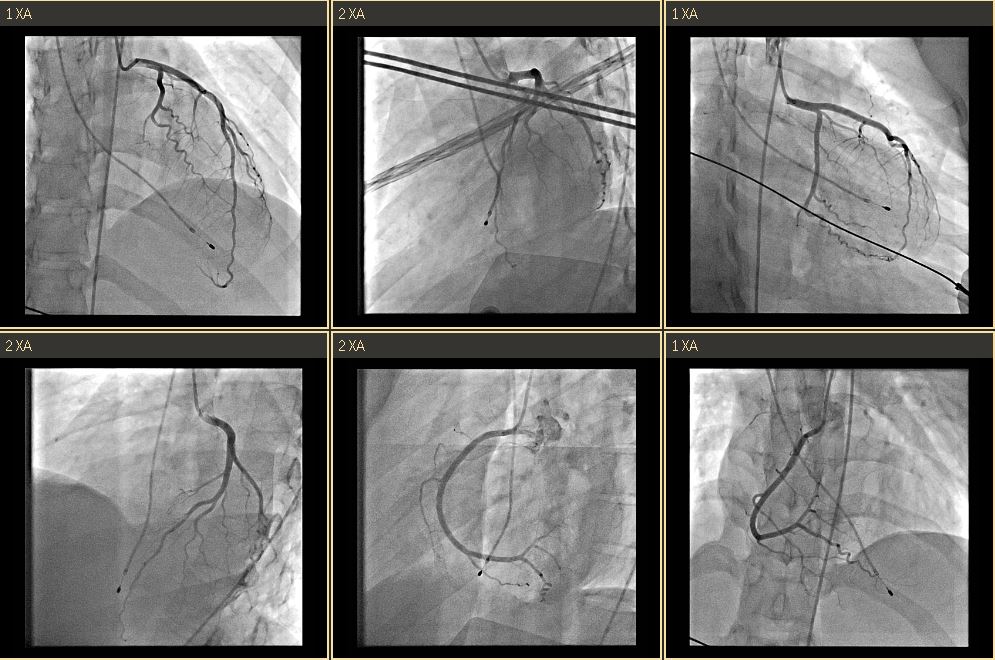
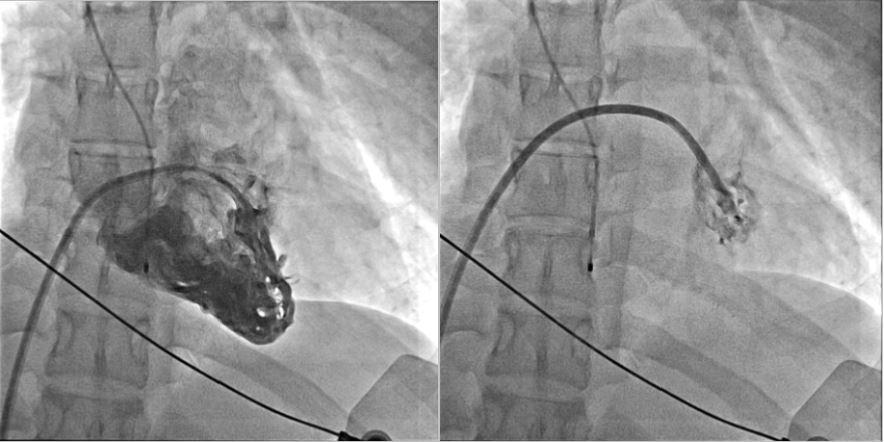
Coronary Angiography:
LM: Patent
LAD: Patent
LCX: Patent
RCA: Patent
Hemodynamics:
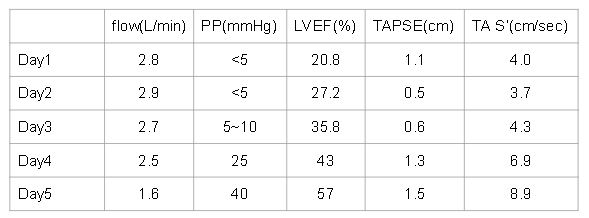
Cardiac output : Average 2.13 ( L/min ) by thermodilution
RPAW: 19 mmHg
MPA: 28/22 mmHg
RA 26/22 mmHg
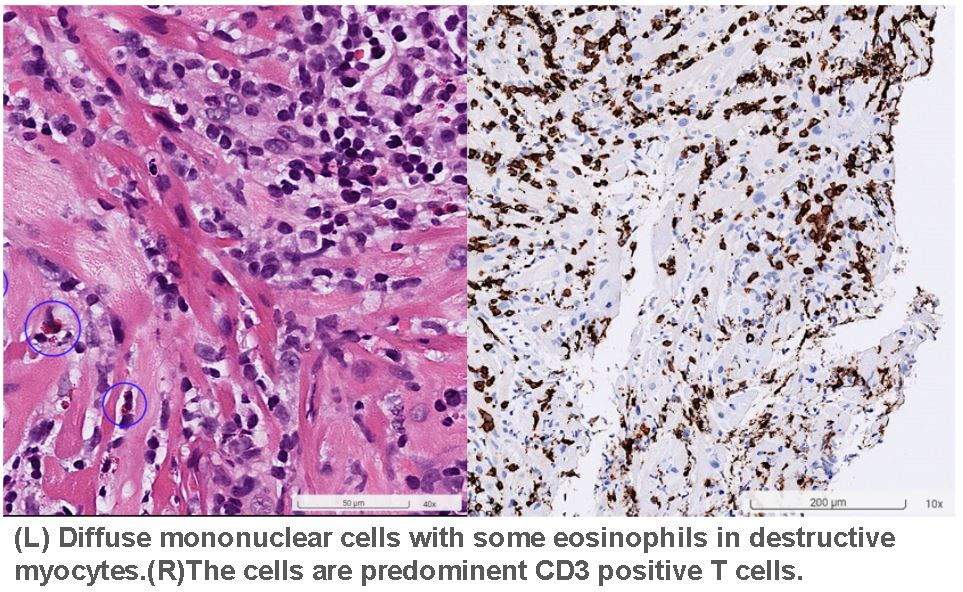
Pathology:
Diffuse mononuclear cells with some eosinophils in destructive myocytes.The cells are predominent CD3 positive T cells. Viral myocarditis isfavored.
Interventional Management
Procedural Step
**STEP 1: DiagnosticCAG**Puncturedright EIA; placed 6Fr sheath.EngagedLCA with 5Fr JL4 catheter, showing patent LCA, and with 5Fr JR4 for RCA,showing patent RCA.
**STEP2: Endomyocardial Biopsy**Puncturedright EIV; placed 7Fr sheath.Advancedlong sheath with 6Fr pigtail for RV angiography, localized atmid-septum. Collected 4 biopsy specimens (1 mm³ each) forhistopathology.
**STEP3: PAC for Hemodynamic Study**InsertedSwan-Ganz catheter to distal RPA.
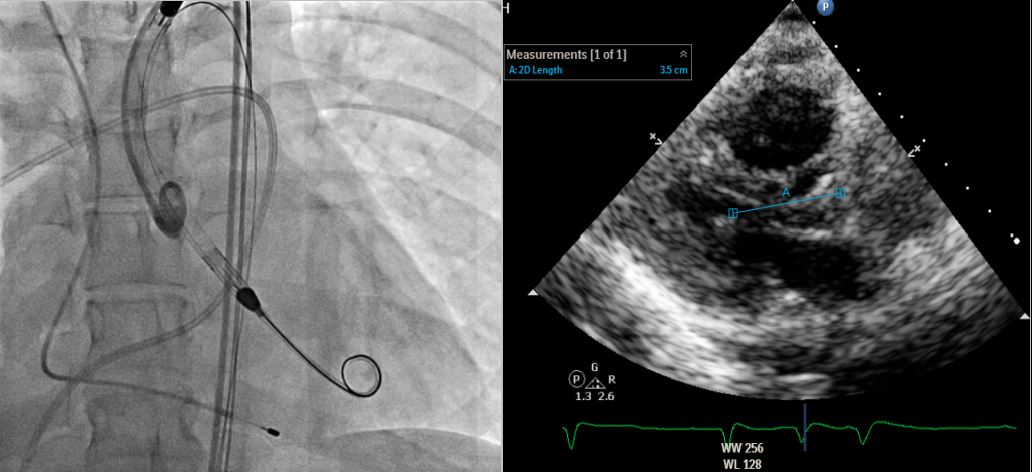
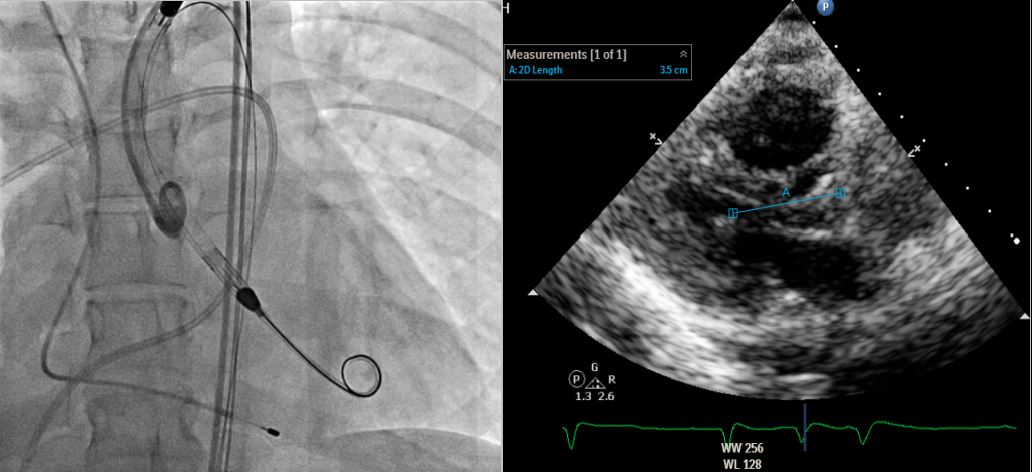
**STEP 4: Insert ABIOMED Impella CP® Microaxial Flow Catheter for Cardiogenic Shock** Pre-embedded 2 Abbott Perclose ProGlide™ SMC System sutures at right EIA sheath. Inserted Impella sheath; Advanced 0.18 wire to LV with pigtail, and checked Impella CP device for function and primed with saline. Positioned Impella tip in LV using fluoroscopy; removed guidewire and connected to console. Confirmed Impella function; secured access site.
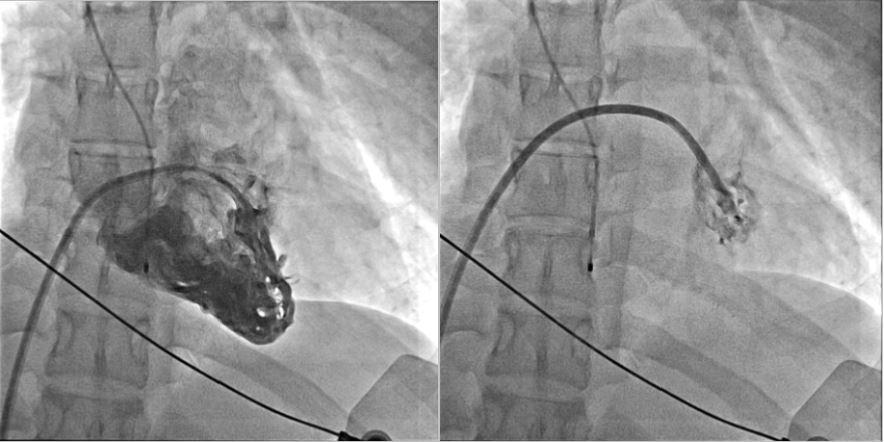
**STEP 5: Removal of Impella on Day 5** Removed Impella after inserting 0.35 J-tip wire to aorta; Achieved hemostasis using ProGlide™ sutures.
**STEP2: Endomyocardial Biopsy**Puncturedright EIV; placed 7Fr sheath.Advancedlong sheath with 6Fr pigtail for RV angiography, localized atmid-septum. Collected 4 biopsy specimens (1 mm³ each) forhistopathology.
**STEP3: PAC for Hemodynamic Study**InsertedSwan-Ganz catheter to distal RPA.
**STEP 4: Insert ABIOMED Impella CP® Microaxial Flow Catheter for Cardiogenic Shock** Pre-embedded 2 Abbott Perclose ProGlide™ SMC System sutures at right EIA sheath. Inserted Impella sheath; Advanced 0.18 wire to LV with pigtail, and checked Impella CP device for function and primed with saline. Positioned Impella tip in LV using fluoroscopy; removed guidewire and connected to console. Confirmed Impella function; secured access site.
**STEP 5: Removal of Impella on Day 5** Removed Impella after inserting 0.35 J-tip wire to aorta; Achieved hemostasis using ProGlide™ sutures.
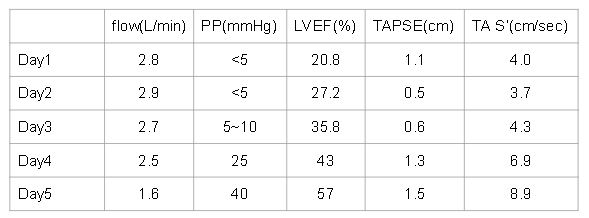
Case Summary
We report a youngwoman with fulminant myocarditis, who survived with temporary Impella CP® support. An initial ECG showed ST elevation in V1 and aVR, indicatingpossible right ventricular involvement. For circulatory support, wechosed Impella CP® because VA-ECMO would increase afterload, leadingto pulmonary edema and poor LV recovery. Even RV was involved withimpaired RV function, her clinical condition remained stable underthe treatment guided by PAC. By day 3, her cardiac function hadimproved much, and the Impella CP® was removed on day 5. The patient wasdischarged on day 11. One-month follow-up showed full RV and LVrecovery.


