Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-160
The Domino Effect: Triple Jeopardy After Angiography
By Chatchai Pitakrattanachai, Wittawat Wattanasiriporn
Presenter
Chatchai Pitakrattanachai
Authors
Chatchai Pitakrattanachai1, Wittawat Wattanasiriporn1
Affiliation
Rajavithi hospital, Thailand1,
View Study Report
TCTAP C-160
Coronary - Complication Management
The Domino Effect: Triple Jeopardy After Angiography
Chatchai Pitakrattanachai1, Wittawat Wattanasiriporn1
Rajavithi hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 66-year-old Thai woman with a history of hypertension (HT) presented for a scheduled elective percutaneous coronary intervention (PCI) to the left main (LM) and left anterior descending (LAD) arteries due to a previous episode of ST-segment elevation myocardial infarction (STEMI), which led to a diagnosis of triple vessel disease (TVD). She had previously undergone coronary angiography (CAG) with PCI to the right coronary artery (RCA) using 3 drug-eluting stents (DES) in October 2023.
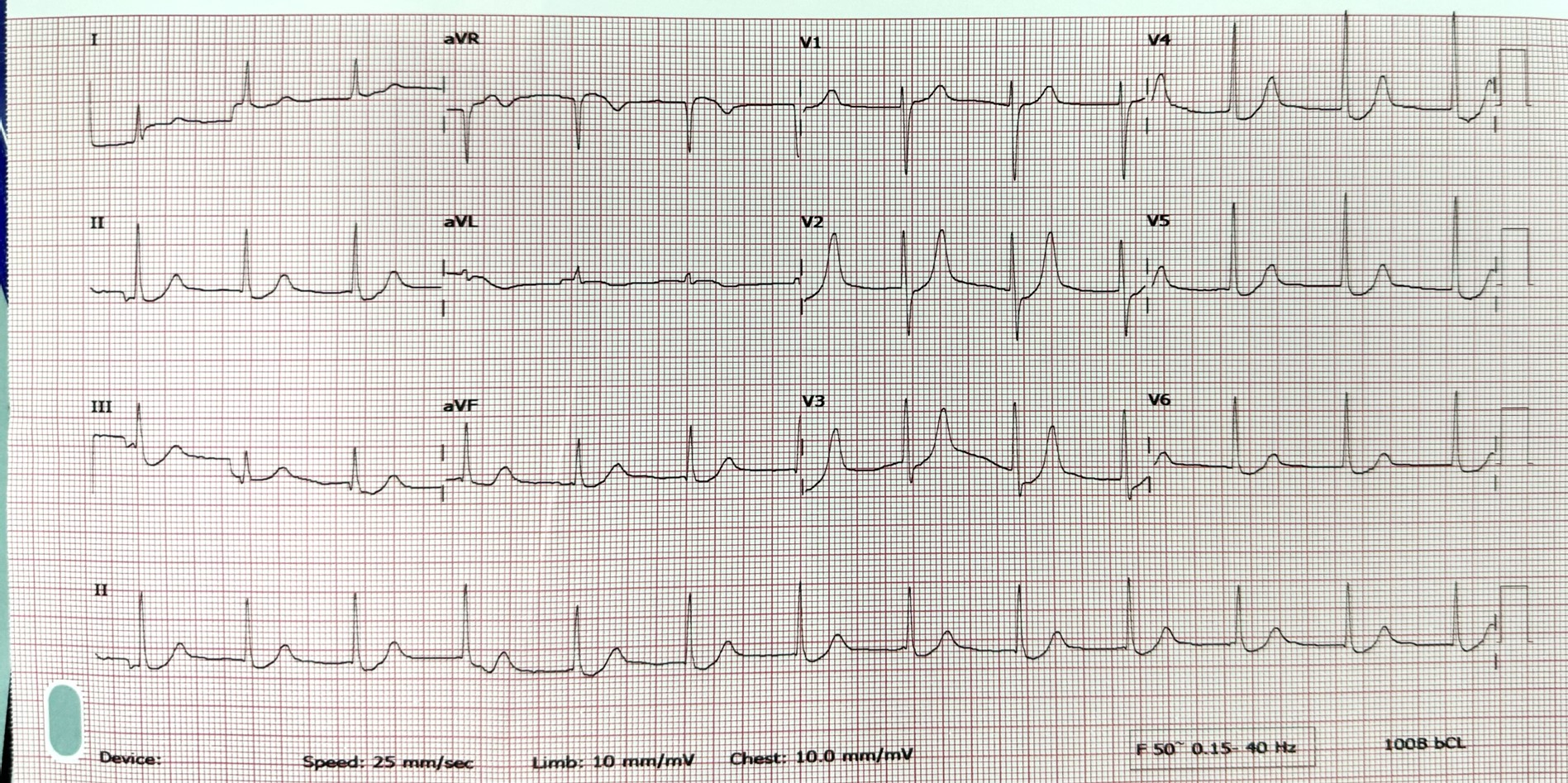
Relevant Test Results Prior to Catheterization
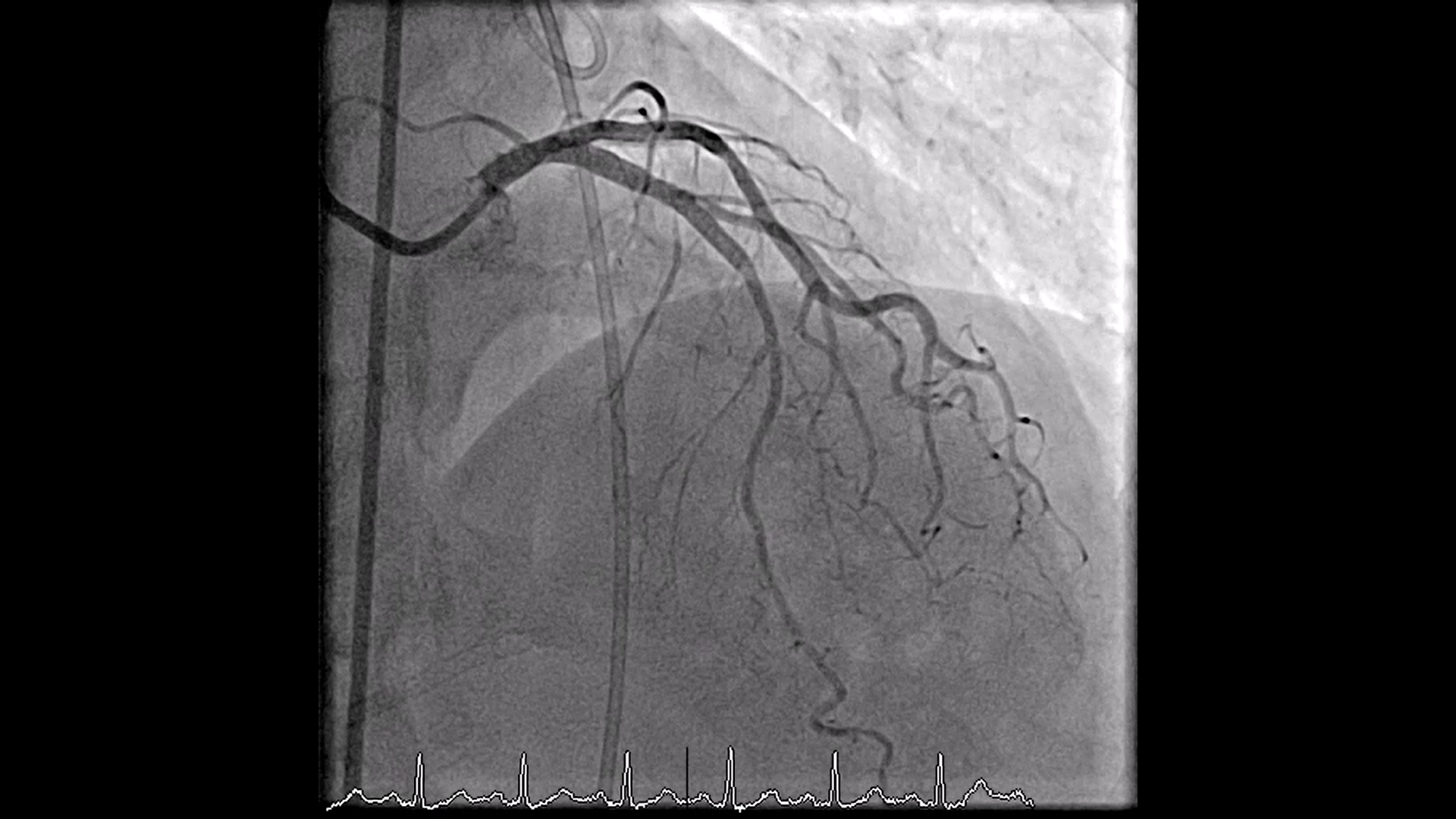
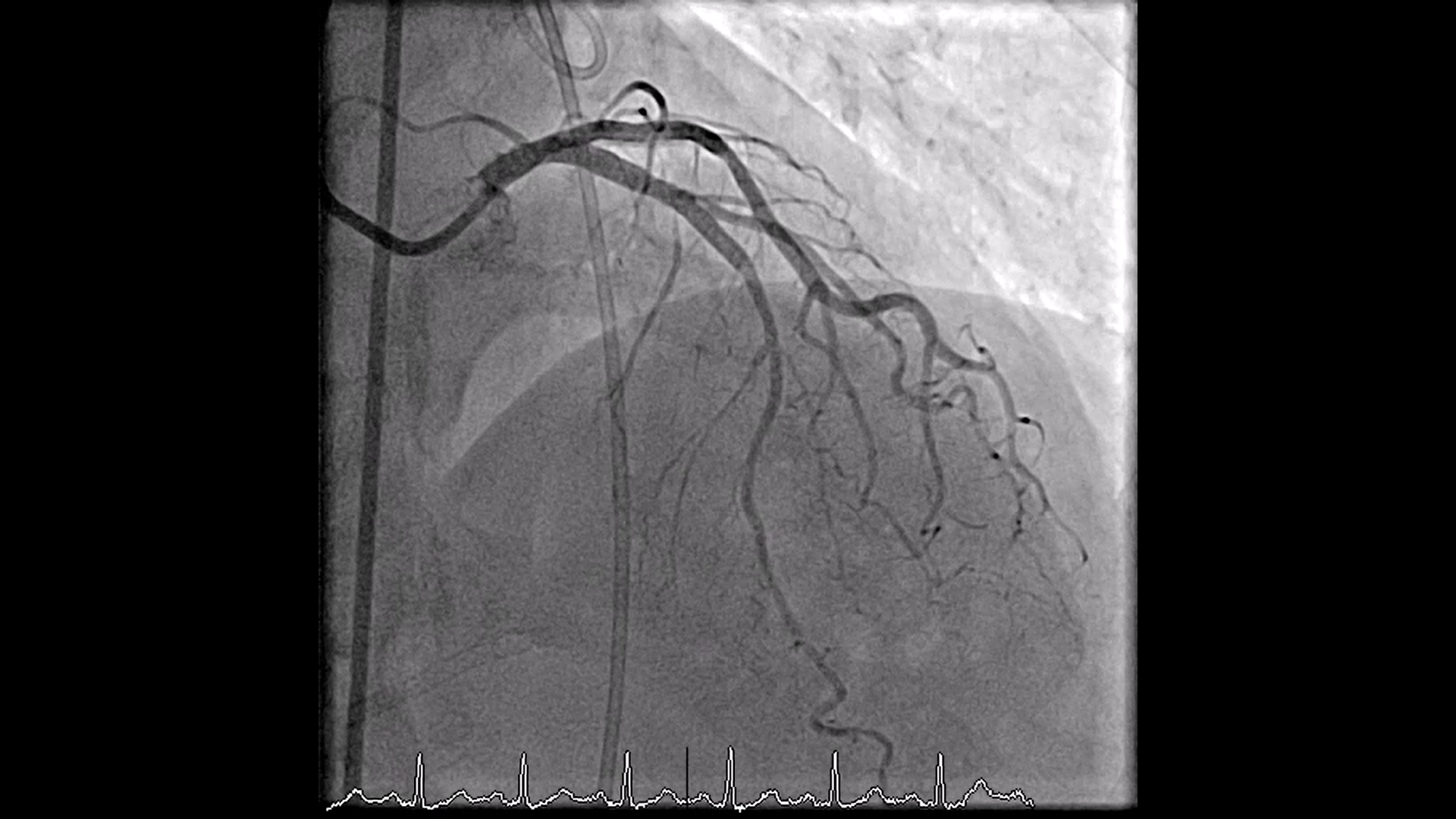
Her preoperative cardiovascular examination and laboratory results were unremarkable.CAG results:
Right Dominant coronary artery
LM: 60-70% stenosis from ostial to distal LM
LAD: 85% stenosis from ostial to proximal LAD, 70% stenosis mid LAD
LCx: 60-70% stenosis proximal LCx, 70% stenosis mid LCx
RCA: Patent stent, non-significant stenosis
Right Dominant coronary artery
LM: 60-70% stenosis from ostial to distal LM
LAD: 85% stenosis from ostial to proximal LAD, 70% stenosis mid LAD
LCx: 60-70% stenosis proximal LCx, 70% stenosis mid LCx
RCA: Patent stent, non-significant stenosis
Relevant Catheterization Findings
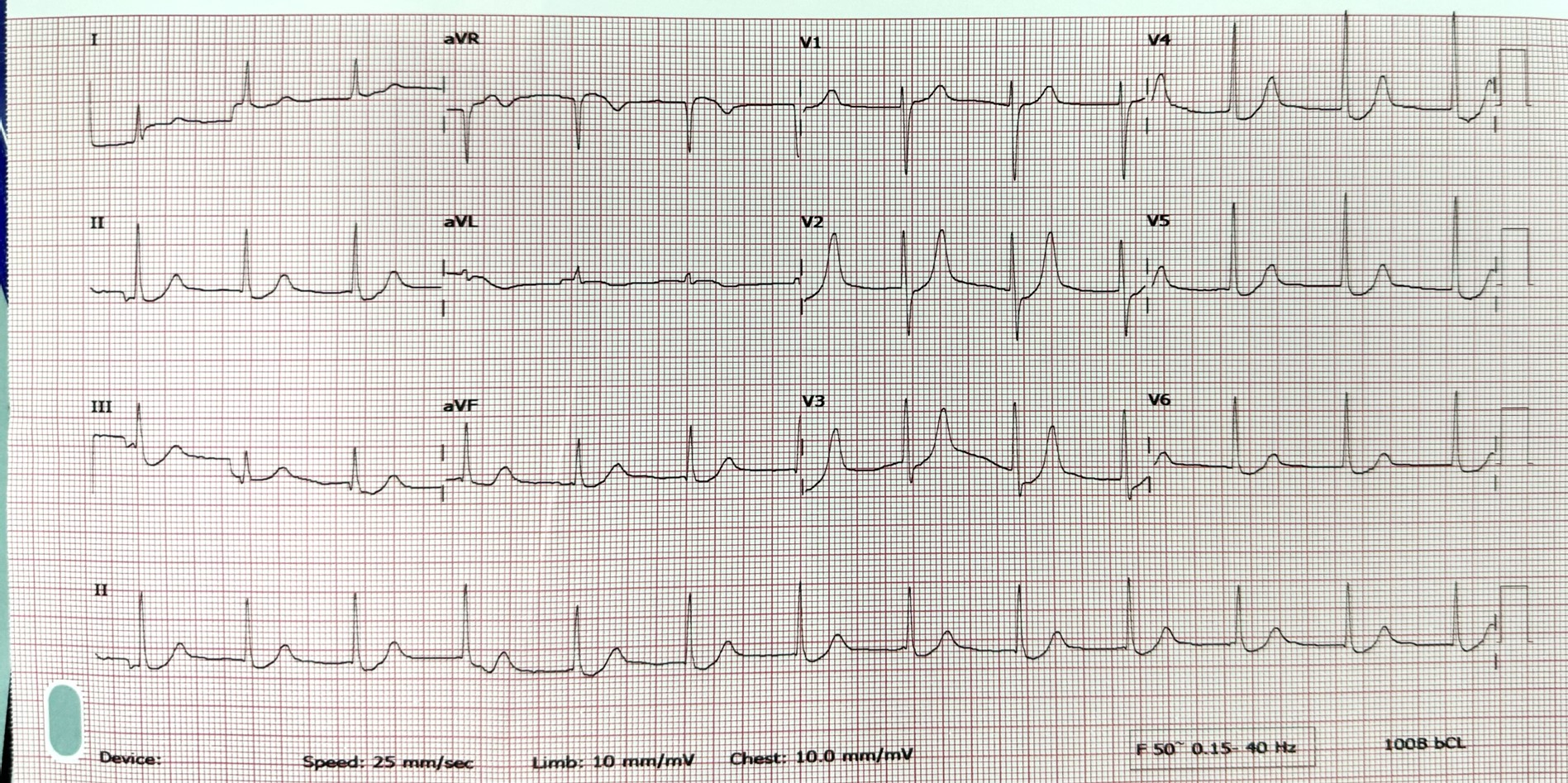
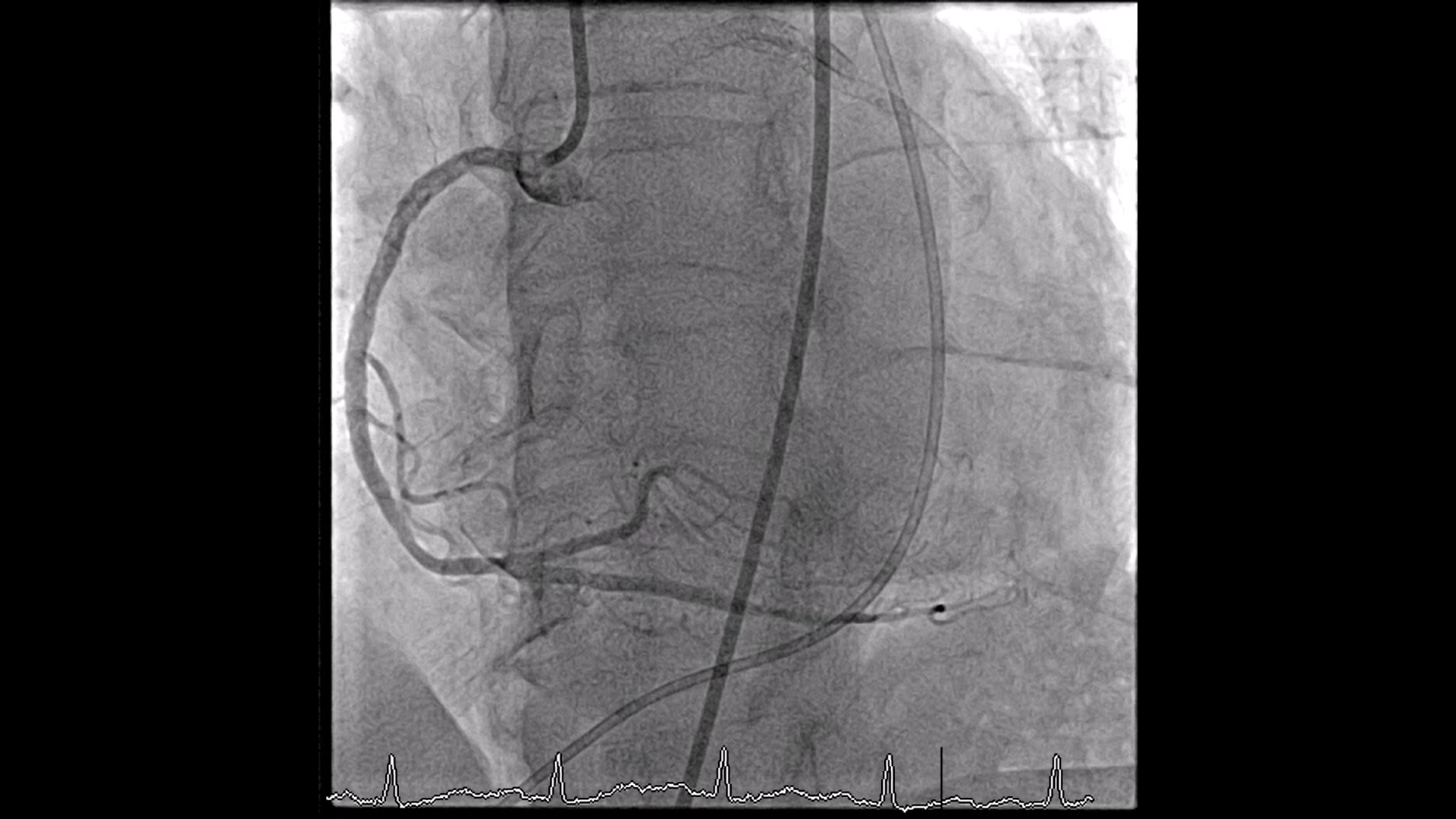
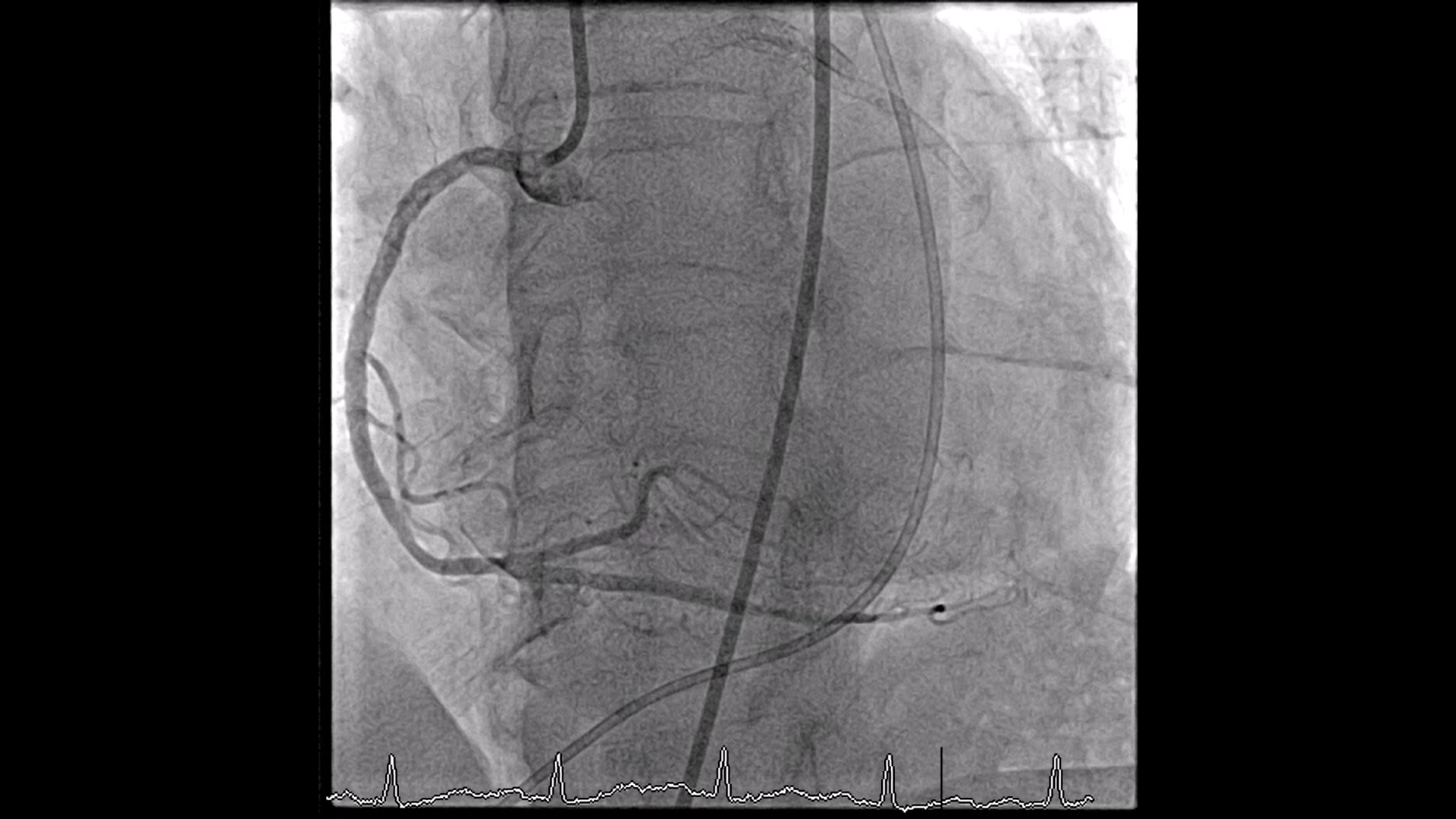
Soon after arriving CCU. The patient developed VF cardiac arrest. ROSC was achieved through defibrillation 200 joules, along with endotracheal intubation. An urgent repeat coronary angiography (Re-CAG) was performed, and temporary transvenous pacing attempted multiple times to capture RV free wall via right femoral vein due to unstable bradycardia (Sinus arrest). The Re-CAG revealed acute in-stent thrombosis at both ostial LCx and mLAD, suspected from stent under expansion.
Interventional Management
Procedural Step
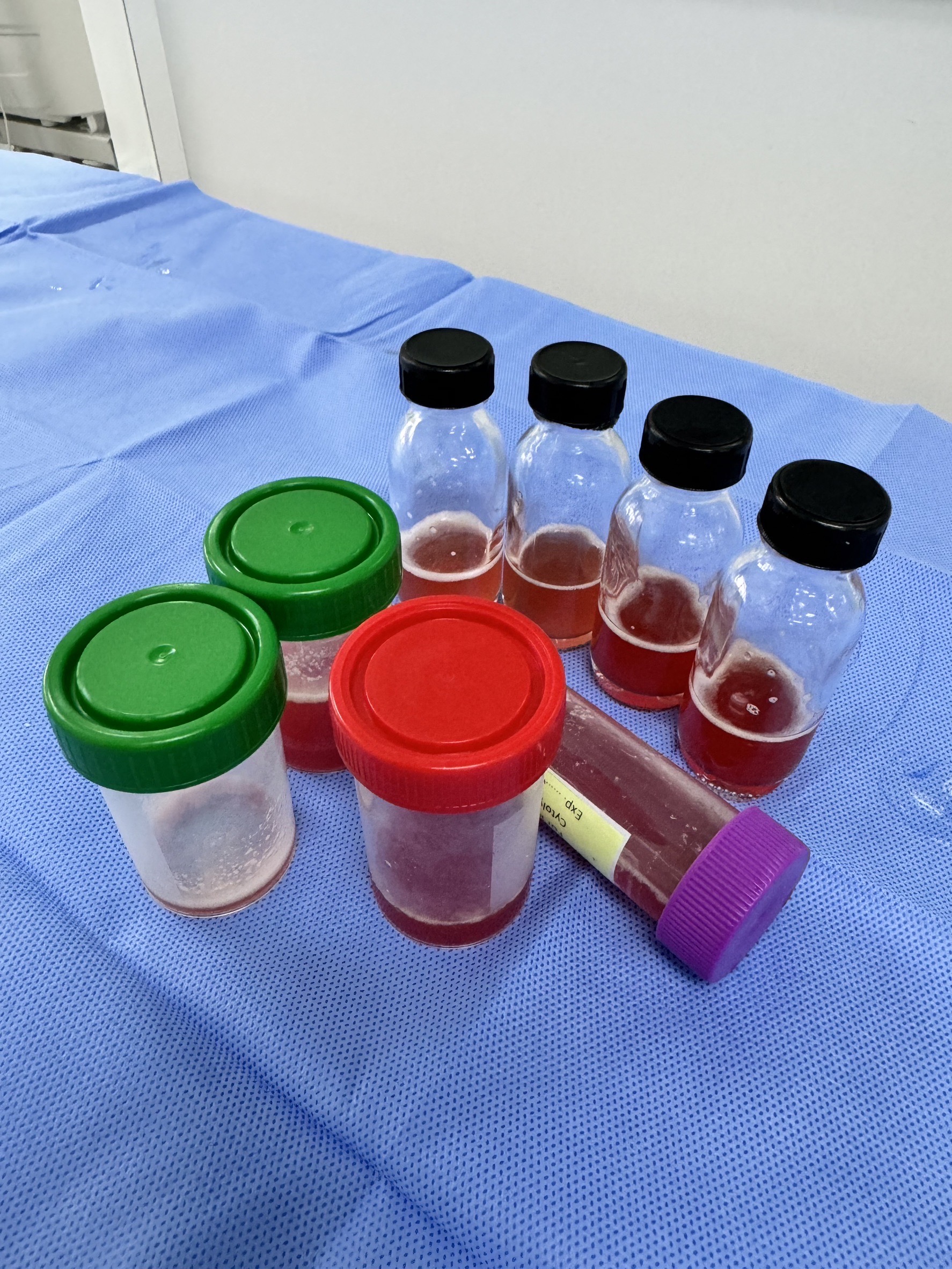
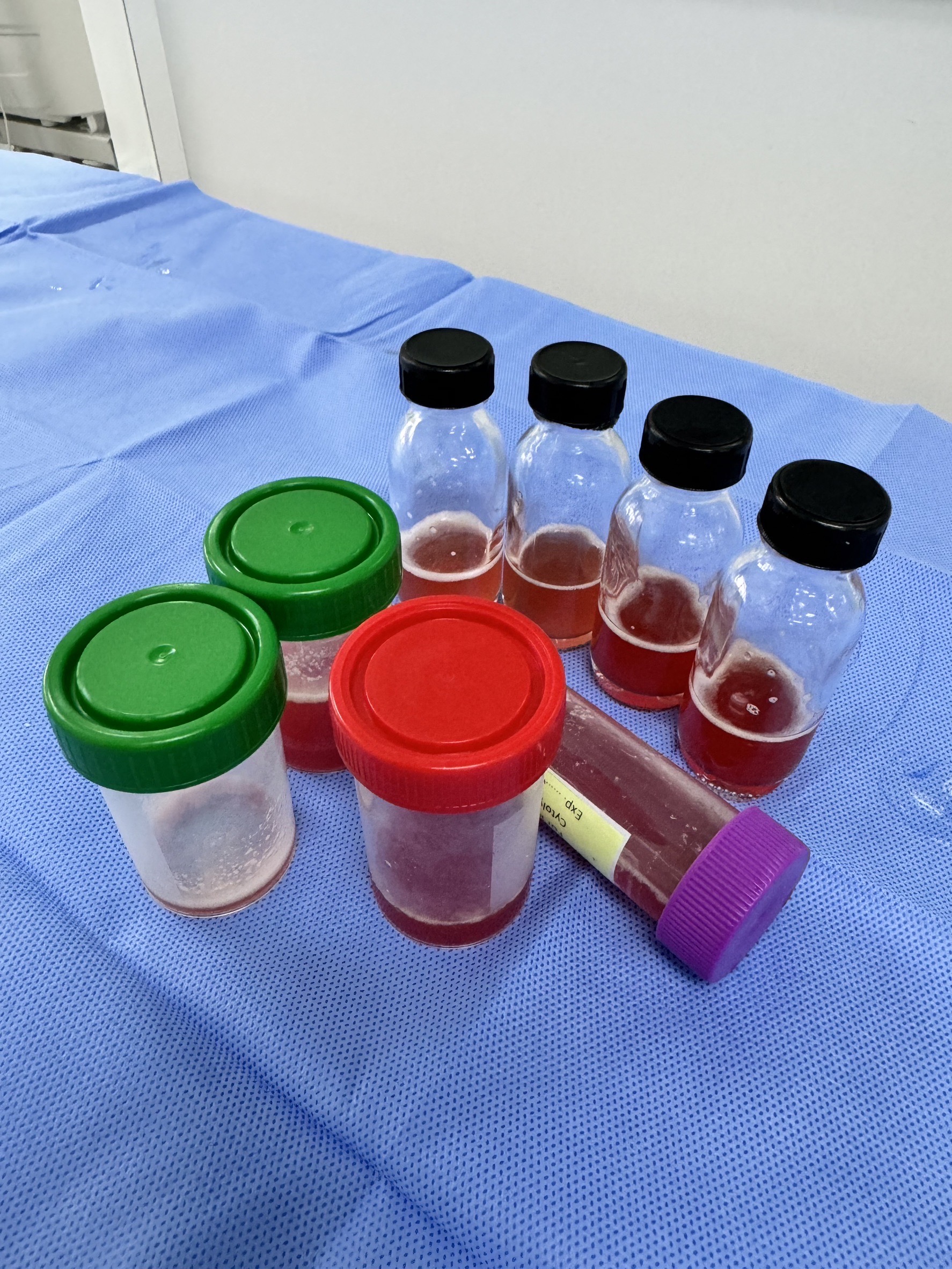
Re-PCI to LCx, LAD - GD: JL SH 6 Fr 3.5 and Turntrac to LAD, LCx.- PCI to LCx: SC balloon 2.0 x 15 mm was inflated 10 atm LCx. - NC balloon 3.0 x 15 mm was inserted to proximal LCx inflated to 25 atm. - Everolimus eluting stent 2.25 x 28 mm was deployed at mLCx to OM1 inflated up to 14 atm.- NC balloon 3.0 x 15 mm post dilated up to 16 atm at pLCx.- SC balloon 2.0 x 15 mm post dilated at mLCx up to 8 atm. - PCI to LAD : NC balloon 3.0 x 15 mm deployed p-mLAD up to 16 atm.- IABP was inserted due to unstable hemodynamic during procedure. On post-procedural day 4, shortly after removal of the transvenous pacing catheter from the right femoral vein, the patient became unresponsive, presenting with cold and clammy skin. ECG showed a junctional rhythm at 60 bpm, and BP 80/40 mmHg. A bedside echocardiogram revealed a new large, loculated pericardial effusion (measuring 3.2 cm) with blood clot along the inferior aspect adjacent to RV free wall, with total collapse of the RV chamber. Acute cardiac tamponade was suspected as the primary cause of the patient’s instability. The patient was subsequently prepared for urgent pericardiocentesis. Subxiphoid pericardial tapping was performed, revealed 150 ml of bloody pericardial fluid. Re-CAG with RV gram in order to rule out RV perforation from pacemaker insertion, showed patency of all coronary stents with no evidence of coronary artery or RV chamber leakage. Given the patient’s stable condition at the time, conservative management was chosen.
Case Summary
- Post-procedural complication of cardiac tamponade in this case, providing a differential diagnosis that includes coronary perforation, free wall rupture, and injuries from intra-cardiac devices.- The conservative approach of pacemaker lead induced RV perforation by lead removal and observation, less invasive but can lead to fatal complications such as cardiac tamponade or hemorrhagic shock. - Calcific plaque may cause coronary stent under expansion leading to acute stent thrombosis and increase the risk of future adverse cardiac events.


