Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-152
Targeting Complex Coronary Artery Disease in High Lipoprotein(a): Managing Distal Embolization With IVUS and Aspiration Thrombectomy
By Kai-Chun Chang, Hsien-Li Kao
Presenter
Kai-Chun Chang
Authors
Kai-Chun Chang1, Hsien-Li Kao1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-152
Coronary - Complication Management
Targeting Complex Coronary Artery Disease in High Lipoprotein(a): Managing Distal Embolization With IVUS and Aspiration Thrombectomy
Kai-Chun Chang1, Hsien-Li Kao1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
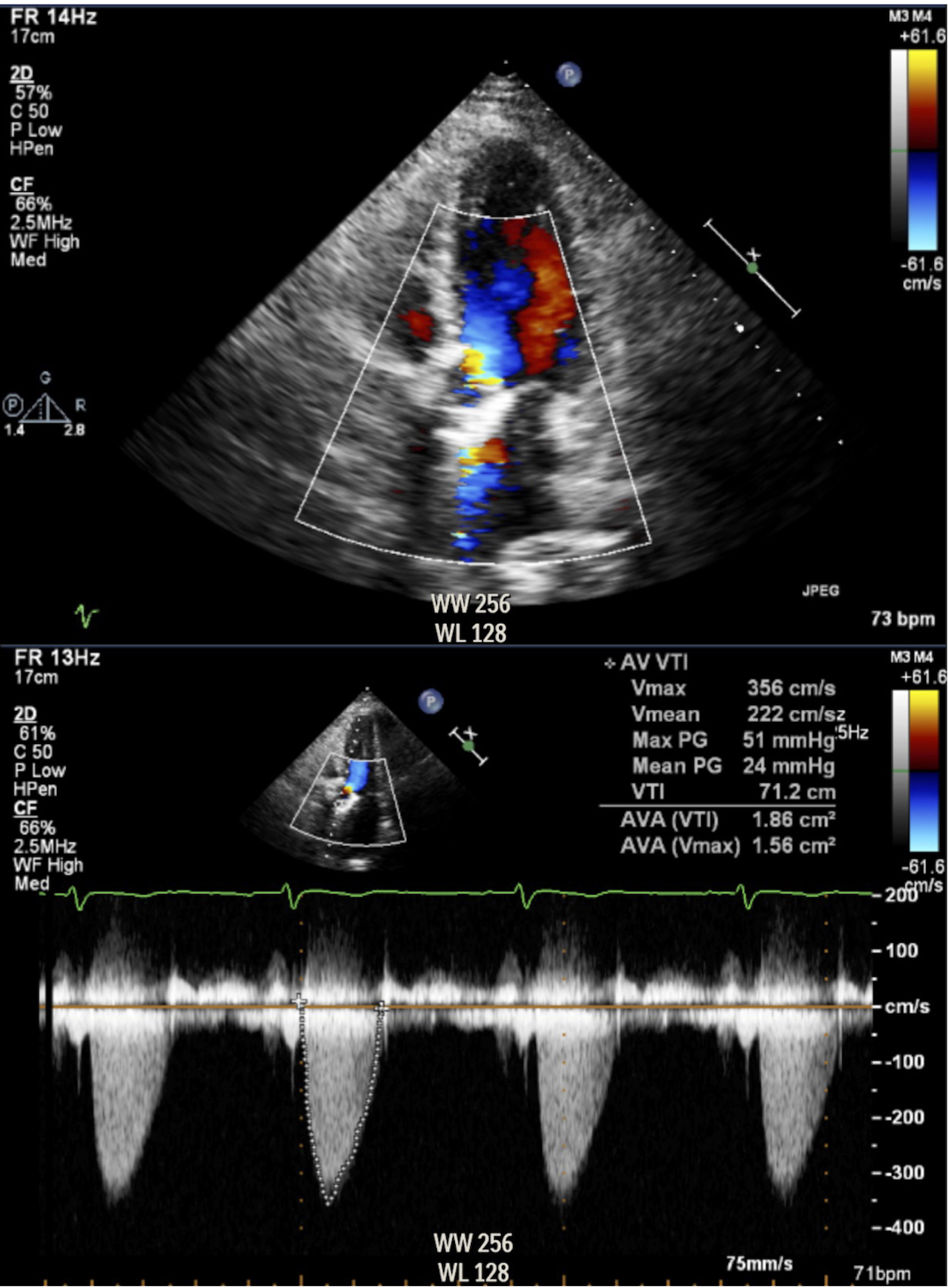
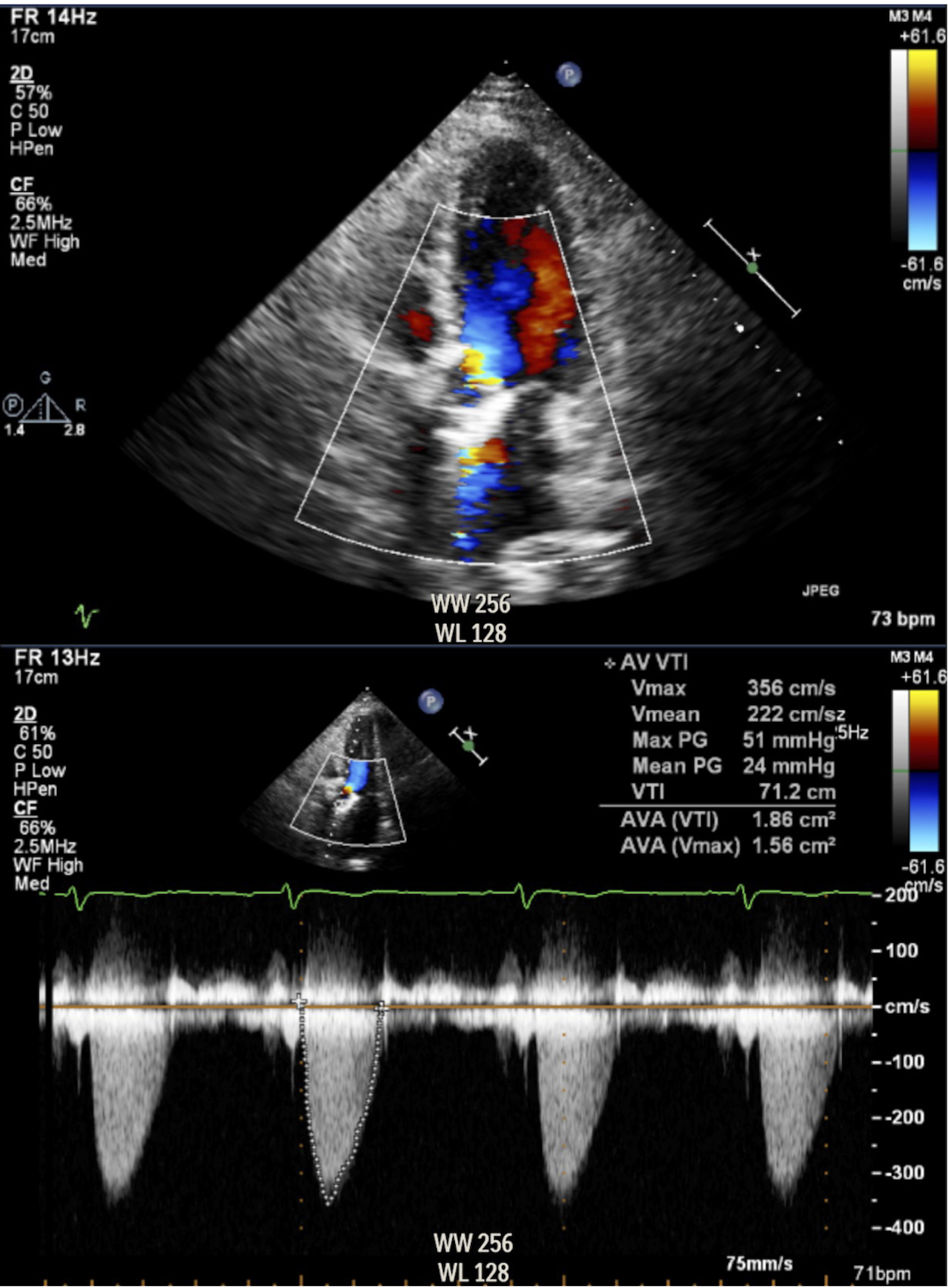
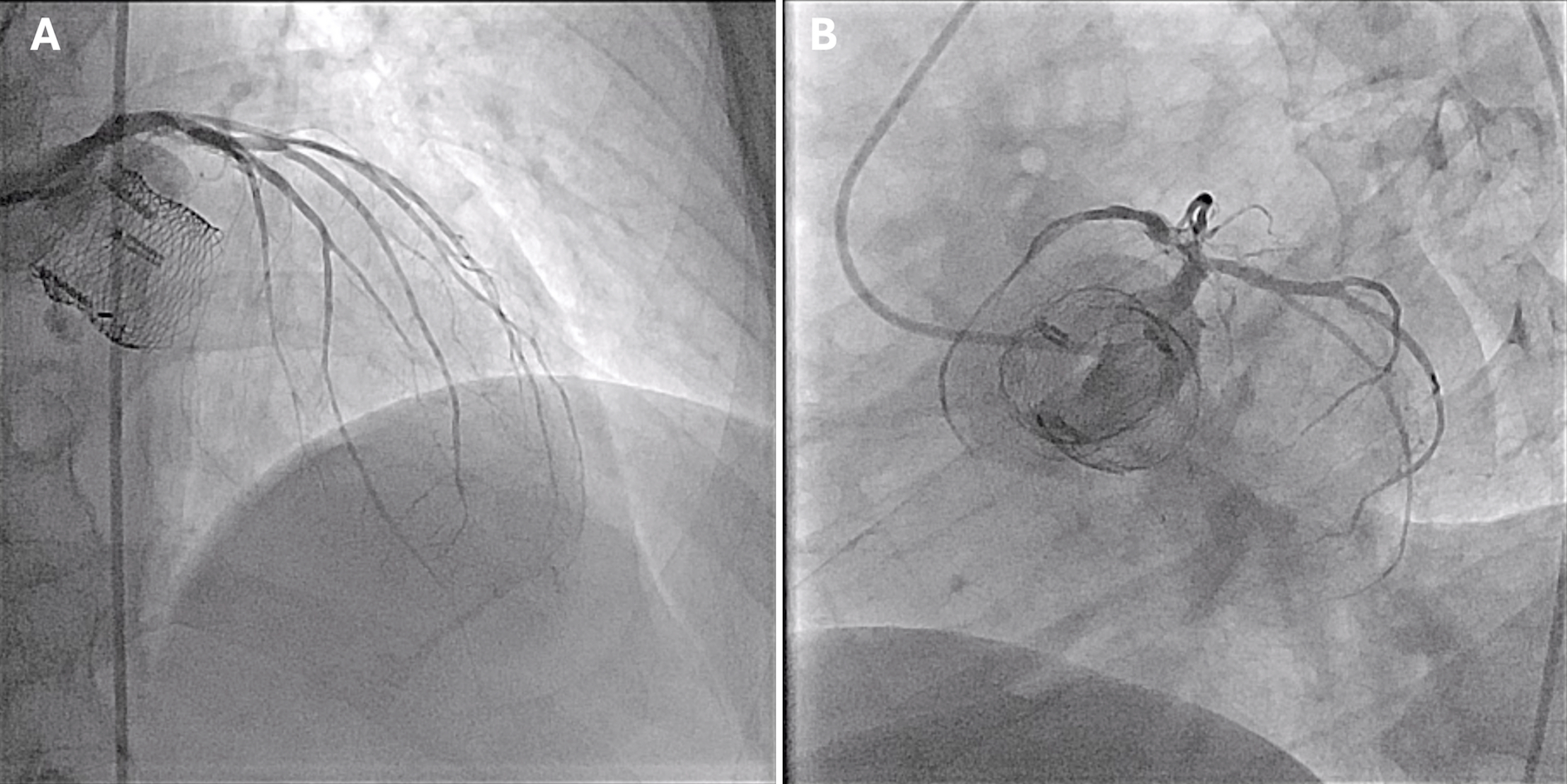
We present a 71-year-old man with diabetes, hypertension, dyslipidemia, and bicuspid aortic stenosis post-TAVR (Boston Scientific Lotus Valve 25 mm) 9 years ago, with known valve degeneration and moderate stenosis (Figure 1). He also has a history of LM-LAD stenting with recurrent in-stent restenosis and presented with 1-month intermittent chest tightness. Physical exam revealed a systolic murmur over the aortic area.
Relevant Test Results Prior to Catheterization
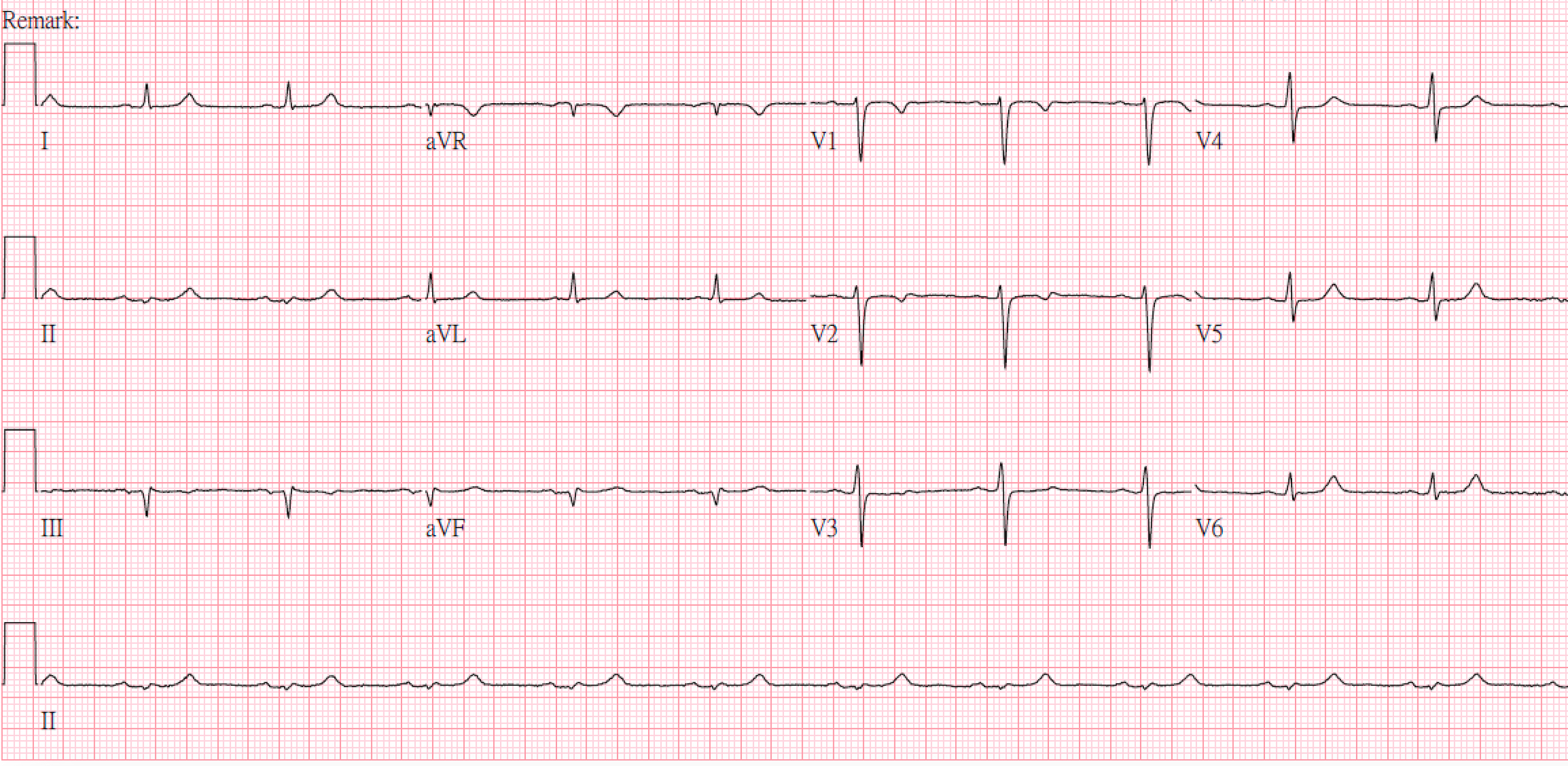
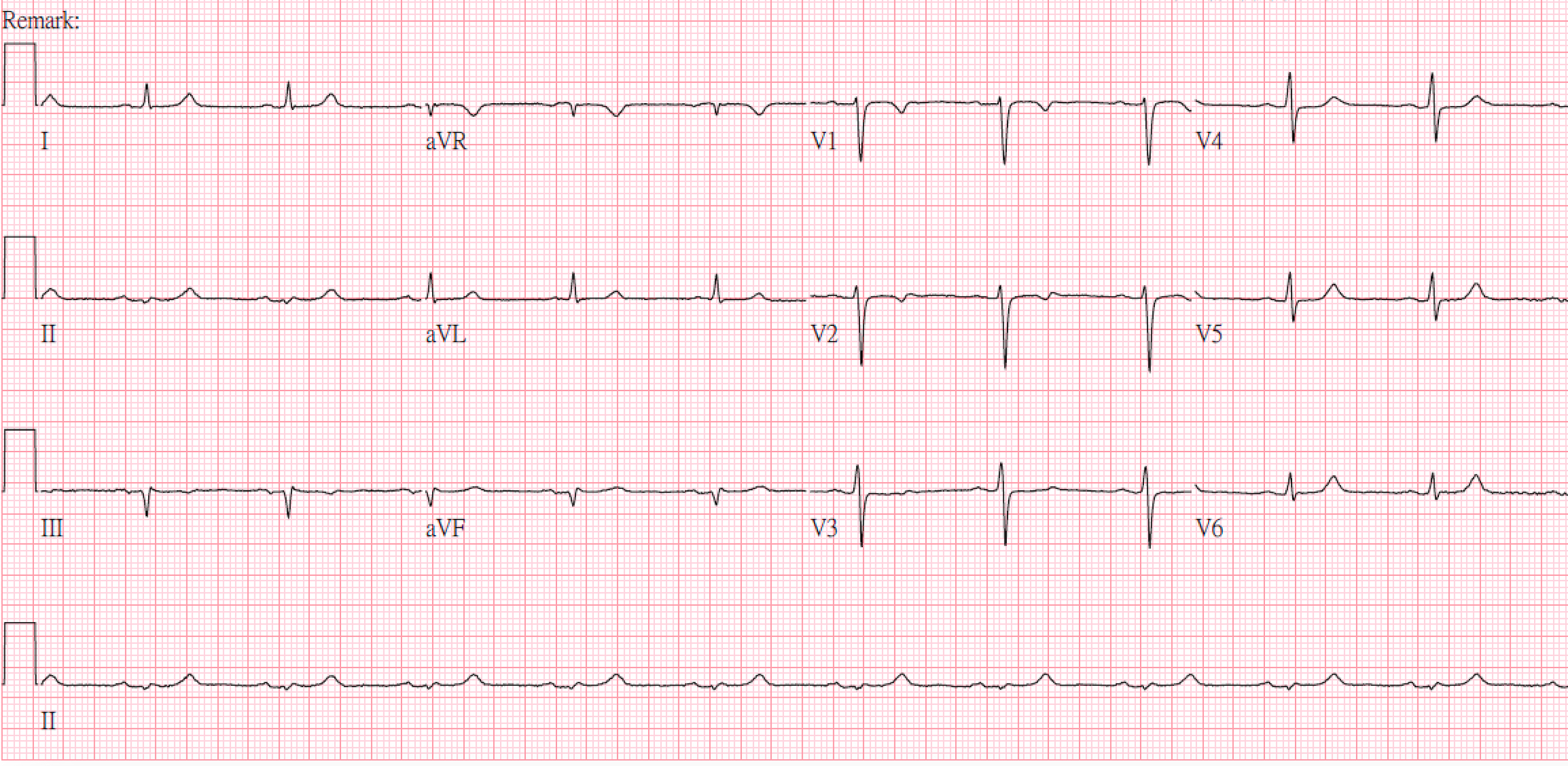
His electrocardiography revealed sinus rhythm without significant ST-segment deviation (Figure 2). Laboratory data revealed fair hemoglobin (14.3 g/dL), creatinine (1.3 mg/dL) and LDL-cholesterol (61 mg/dL) but a significantly elevated lipoprotein(a) (116.8 mg/dL).
Relevant Catheterization Findings
Diagnostic catheterization revealed a stationary trans-aortic valve peak-to-peak pressure gradient of 25 mmHg and a critical in-stent restenosis over proximal LAD (Figure 3). Other coronary arteries were patent. After a shared decision making, intravascular image (IVI)-guided percutaneous coronary intervention (PCI) was initiated.
Interventional Management
Procedural Step
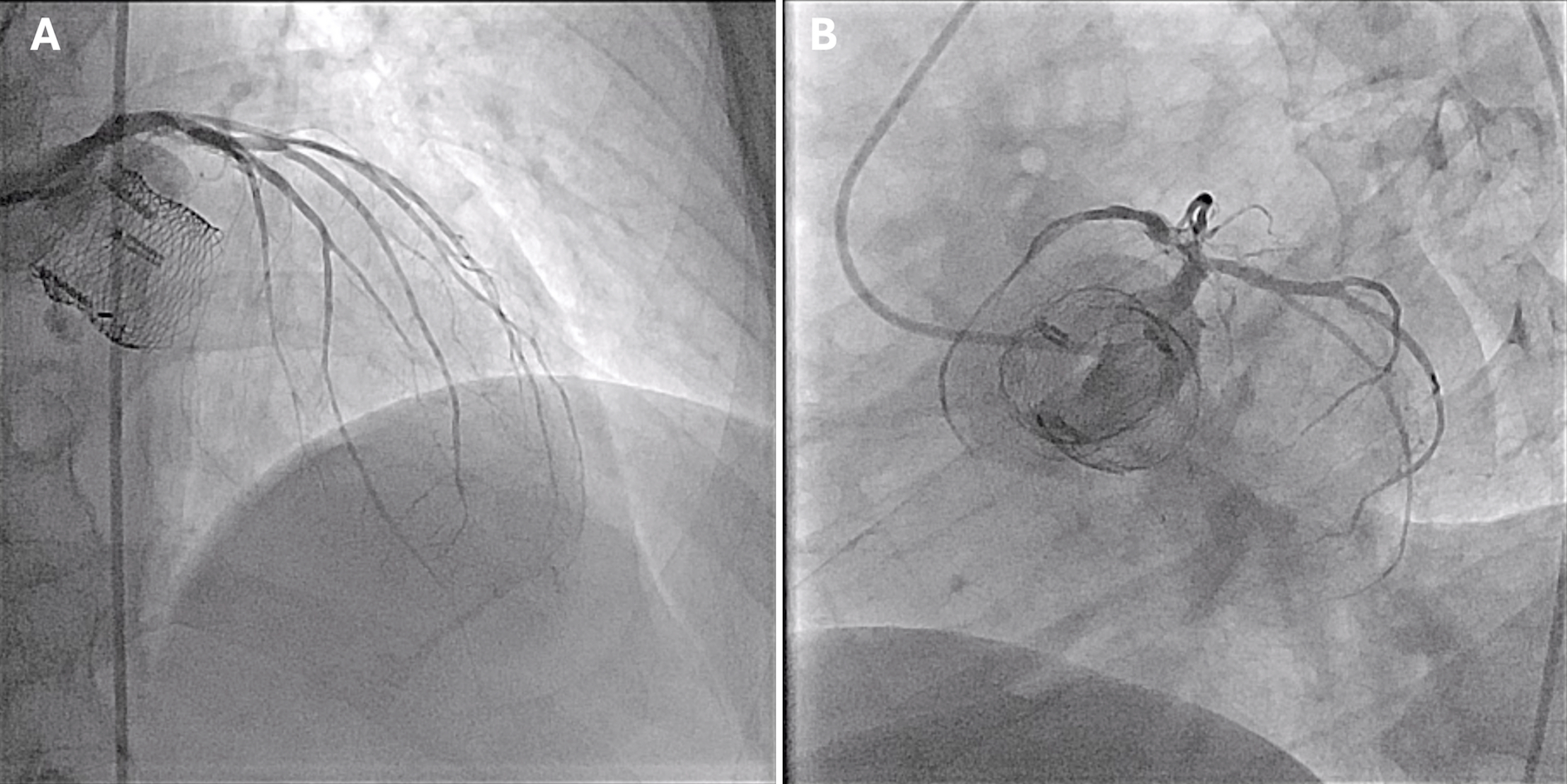
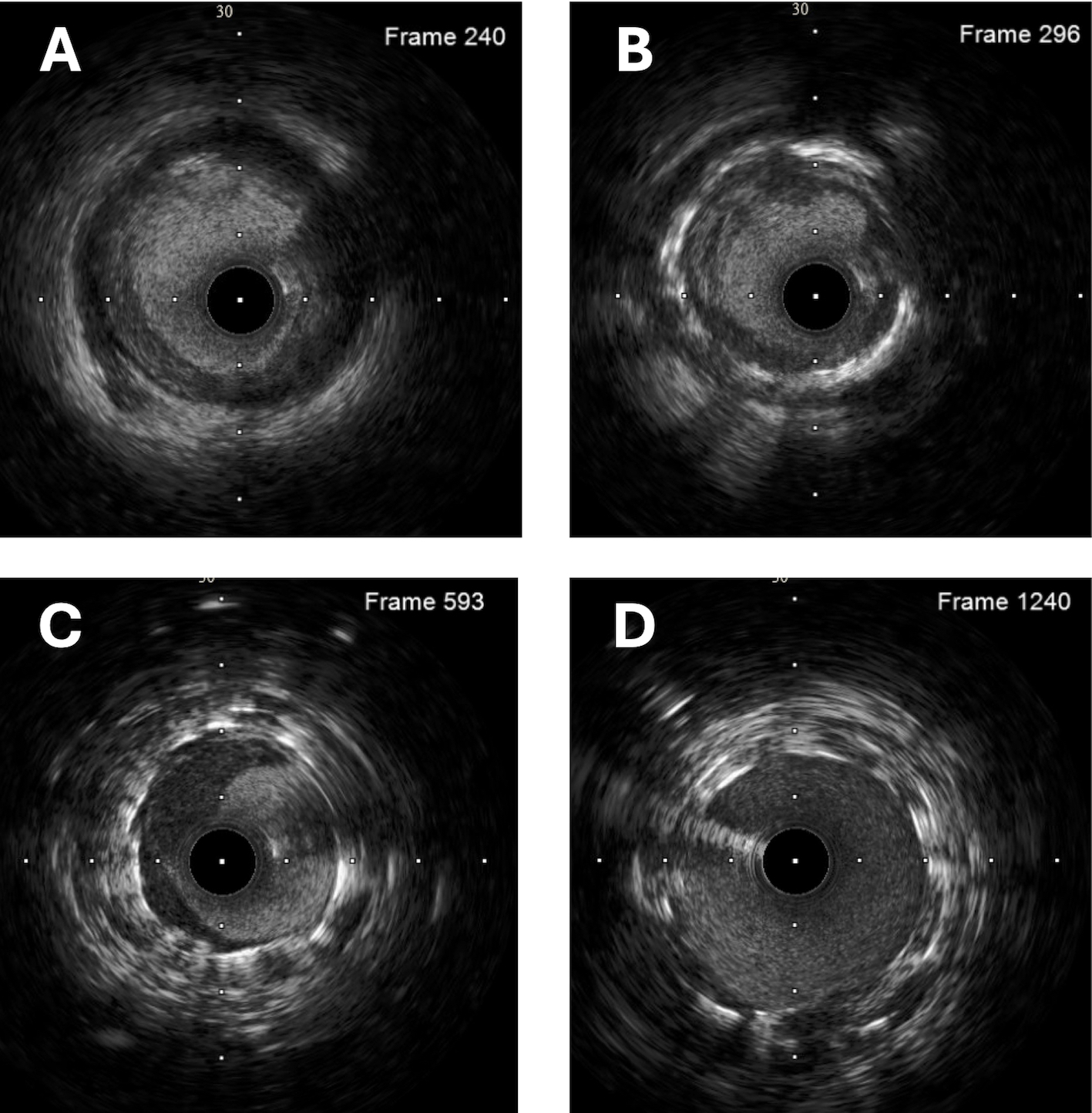
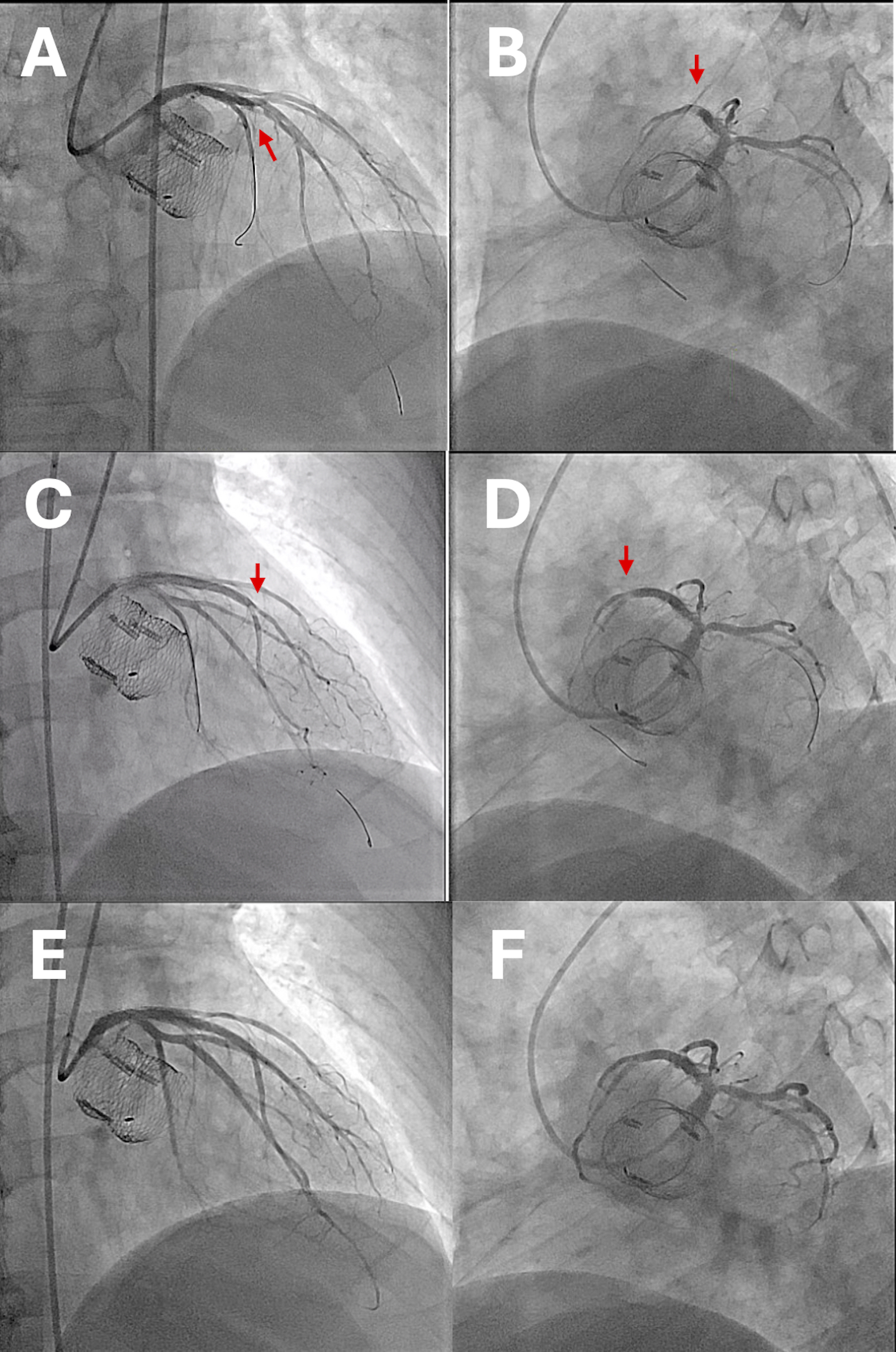
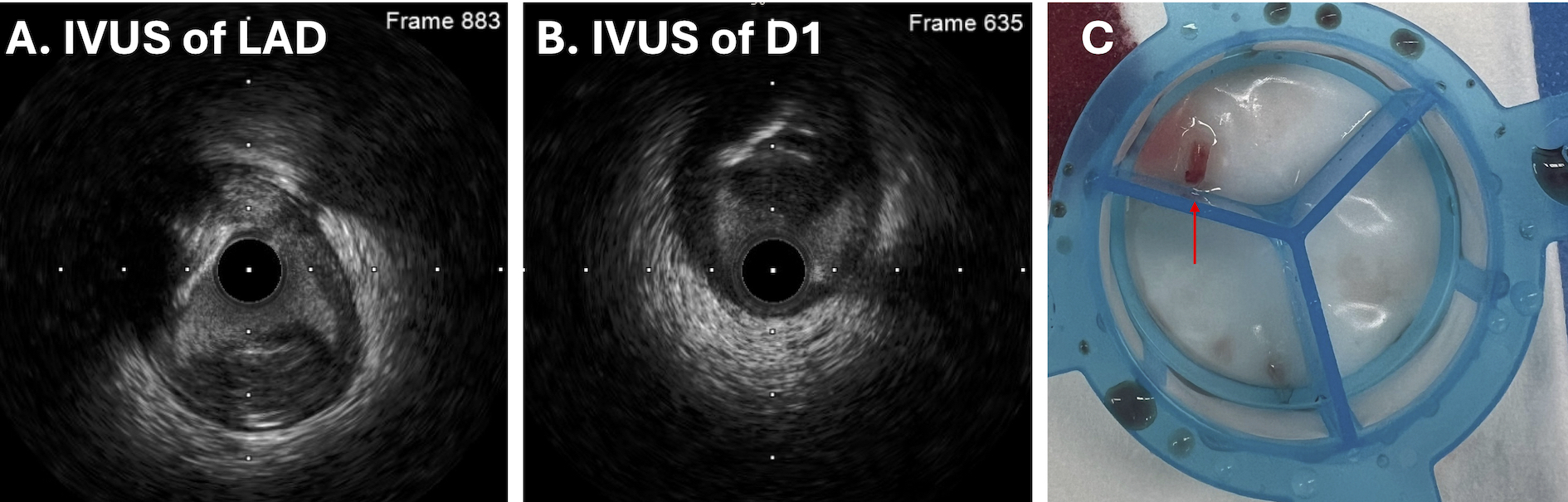
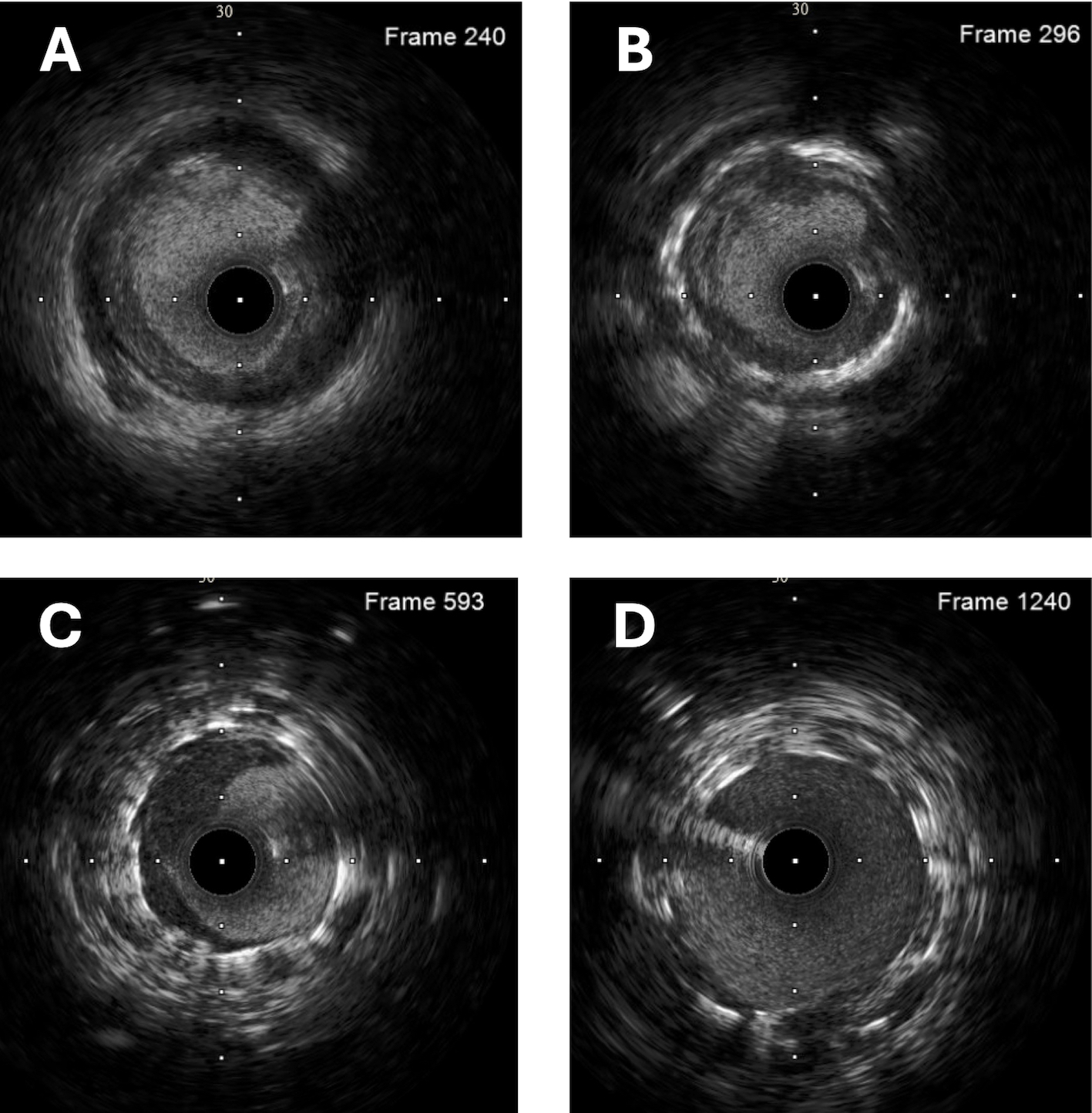
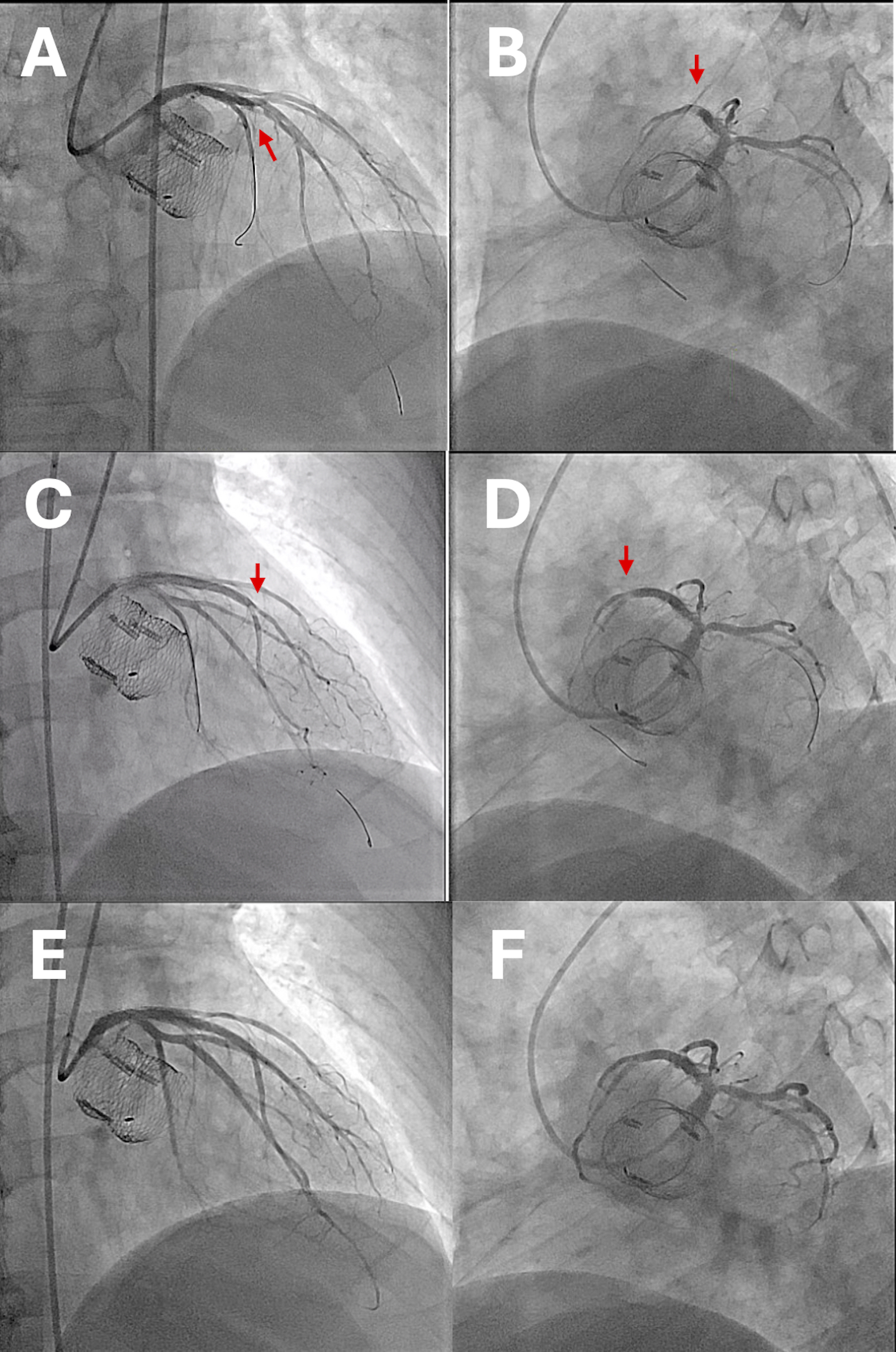
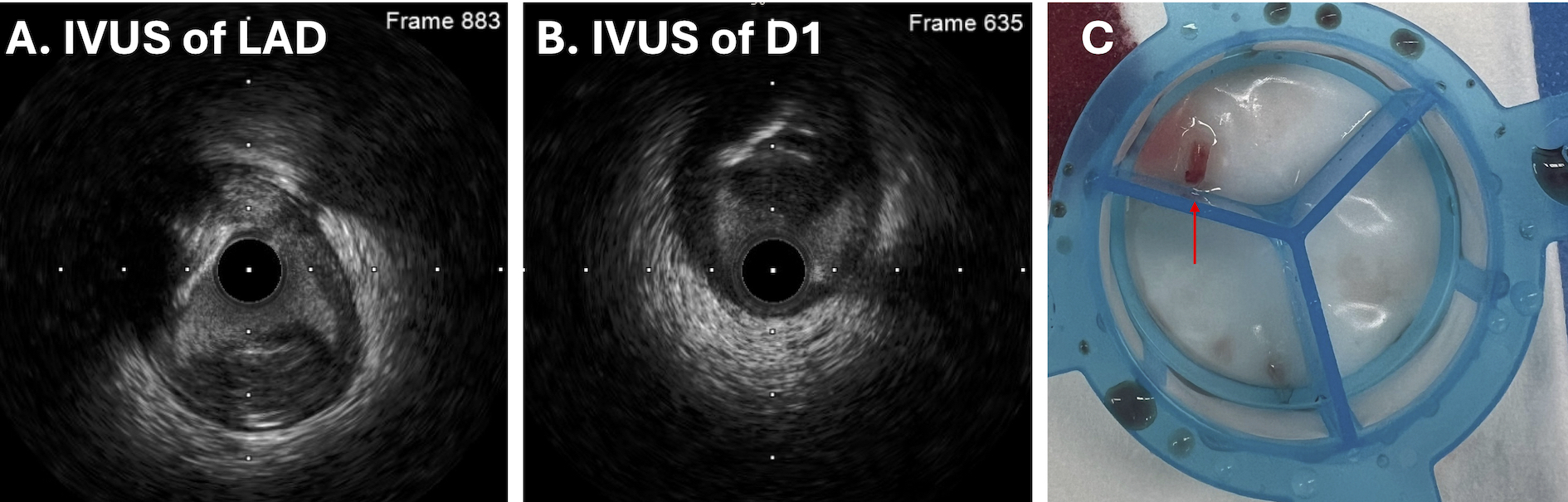
The procedure began with left coronary artery engagement using a 6 Fr Terumo BL3.5 guiding catheter. A Runthrough floppy wire was advanced into the distal LAD, with a Sion wire placed in the left circumflex artery (LCX). Intravascular ultrasound (IVUS) of the LAD revealed fibrous plaque distal to the stent edge in the proximal LAD (Figure 4A), in-stent restenosis with neointimal proliferation and lipid-rich plaque (Figures 4B, 4C), and satisfactory LM stent status (Figure 4D). Angioplasty was performed on the proximal LAD using a Wolverine Coronary Cutting Balloon (3.5mm x 15mm) and NC balloon (3.5mm x 15mm). A distal edge dissection was noticed (Figure 5A, 5B), leading to the deployment of a drug-eluting stent (DES) (Elixir DESyne 2.5mm x 18mm). However, angiography showed decreased distal flow and a new lesion at the LAD-first diagonal artery (D1) bifurcation (Figure 5C, 5D). IVUS identified a hypoechoic lesion at the bifurcation (Figure 6A, 6B), likely distal embolization. Aspiration thrombectomy using the ELIMINATE Aspiration Catheter did not retrieve a thrombus. Kissing balloon technique was applied, showing improvement over bifurcation, with D1 flow remained reduced. A second thrombectomy yielded atheroma-like material (Figure 6C), with improved flow. Angioplasty of the in-stent restenosis was performed using a B.Braun DEB SeQuent Please (3.5mm x 30mm). Final angiography showed TIMI 3 flow without dissection (Figure 5E, 5F); the patient tolerated the procedure well.
Case Summary
We present a case of a gentleman with elevated lipoprotein(a) experiencing recurrent in-stent restenosis. During PCI, distal embolization was observed and managed with IVI and aspiration thrombectomy. Elevated lipoprotein(a) is a key risk factor for residual atherosclerotic cardiovascular disease (ASCVD) and aortic stenosis. Distal embolization during PCI can impair myocardial perfusion, causing no-reflow, and poor outcomes. This case underscores the importance of IVI in managing complex PCI, improving lesion identification, and providing ASCVD pathophysiology insights.


