Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-184
Strategic Cardiac Rescue: Staged Coronary Intervention in a High-Risk Post Cardiac Arrest Patient With Multivessel Disease and End-Stage Renal Disease
By Saurabh Goel, Baburaj Hegde, Ashish Goel
Presenter
Saurabh Goel
Authors
Saurabh Goel1, Baburaj Hegde1, Ashish Goel2
Affiliation
Wockhardt Hospital, India1, Fayth Clinic, India2,
View Study Report
TCTAP C-184
Coronary - High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
Strategic Cardiac Rescue: Staged Coronary Intervention in a High-Risk Post Cardiac Arrest Patient With Multivessel Disease and End-Stage Renal Disease
Saurabh Goel1, Baburaj Hegde1, Ashish Goel2
Wockhardt Hospital, India1, Fayth Clinic, India2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 51-year-old patient presented with acute chest discomfort and breathlessness of 45-minute duration. He had hypertension and nephropathy (last creatinine 2.5 mg/dL four months prior), and no history of DM or IHD. On arrival to emergency, he experienced a cardiac arrest. After successful resuscitation, the patient was intubated and maintained on a ventilator, with a post-resuscitation blood pressure of 180/100 mmHg.
Relevant Test Results Prior to Catheterization
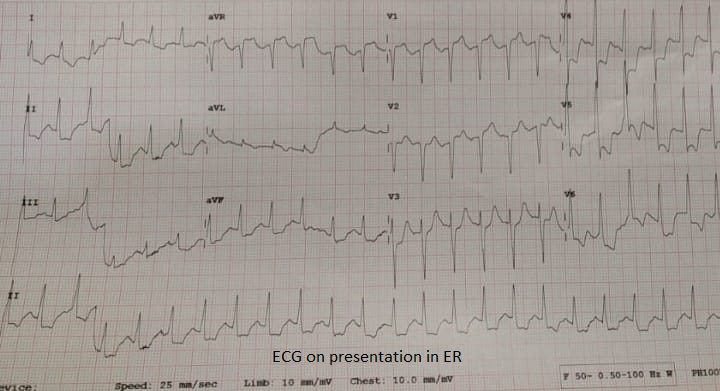
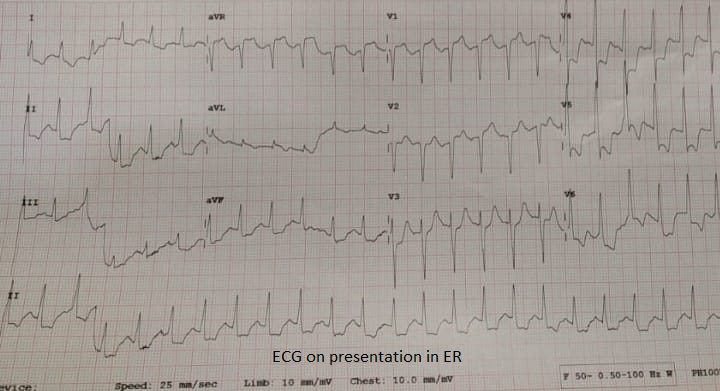
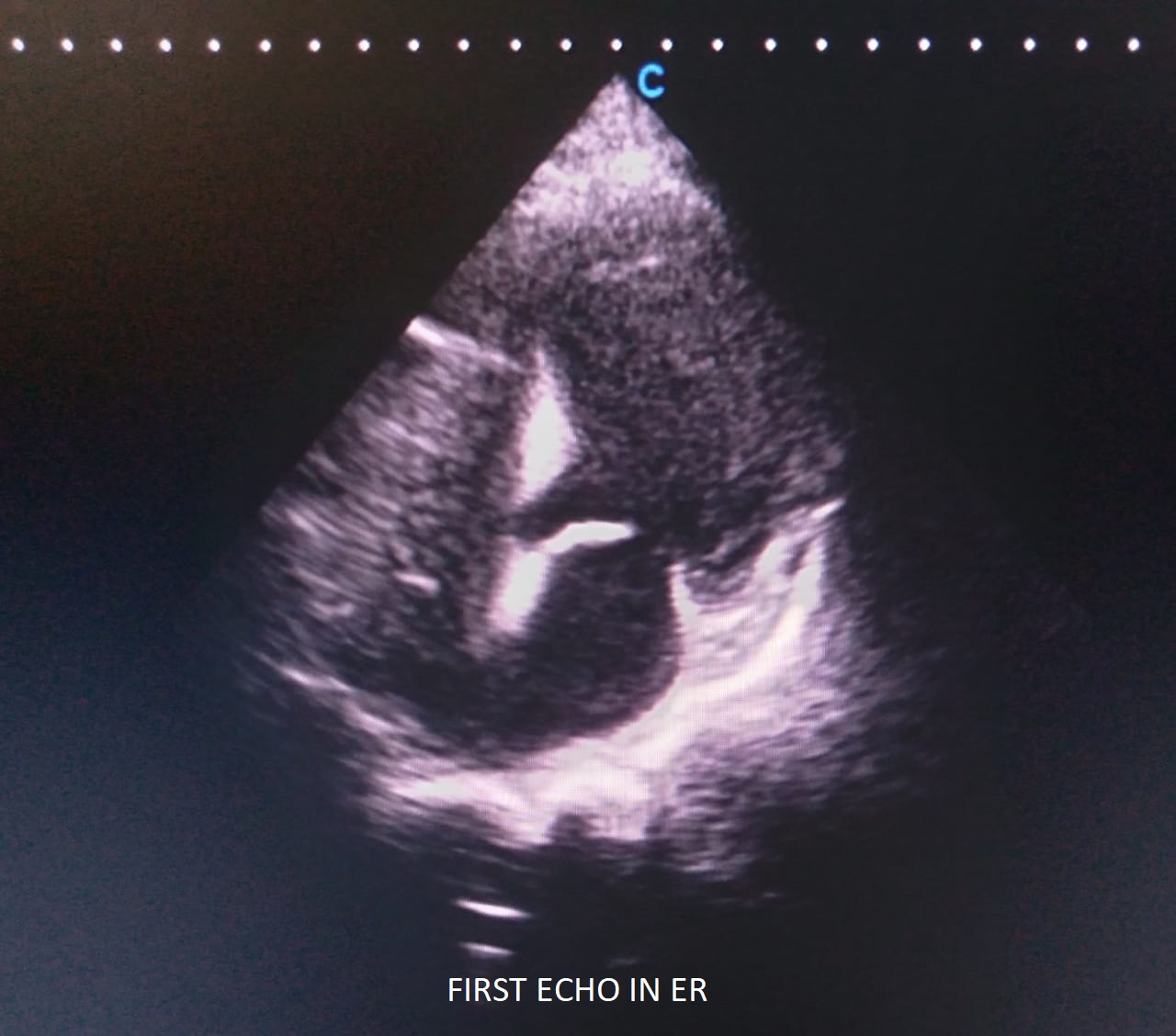
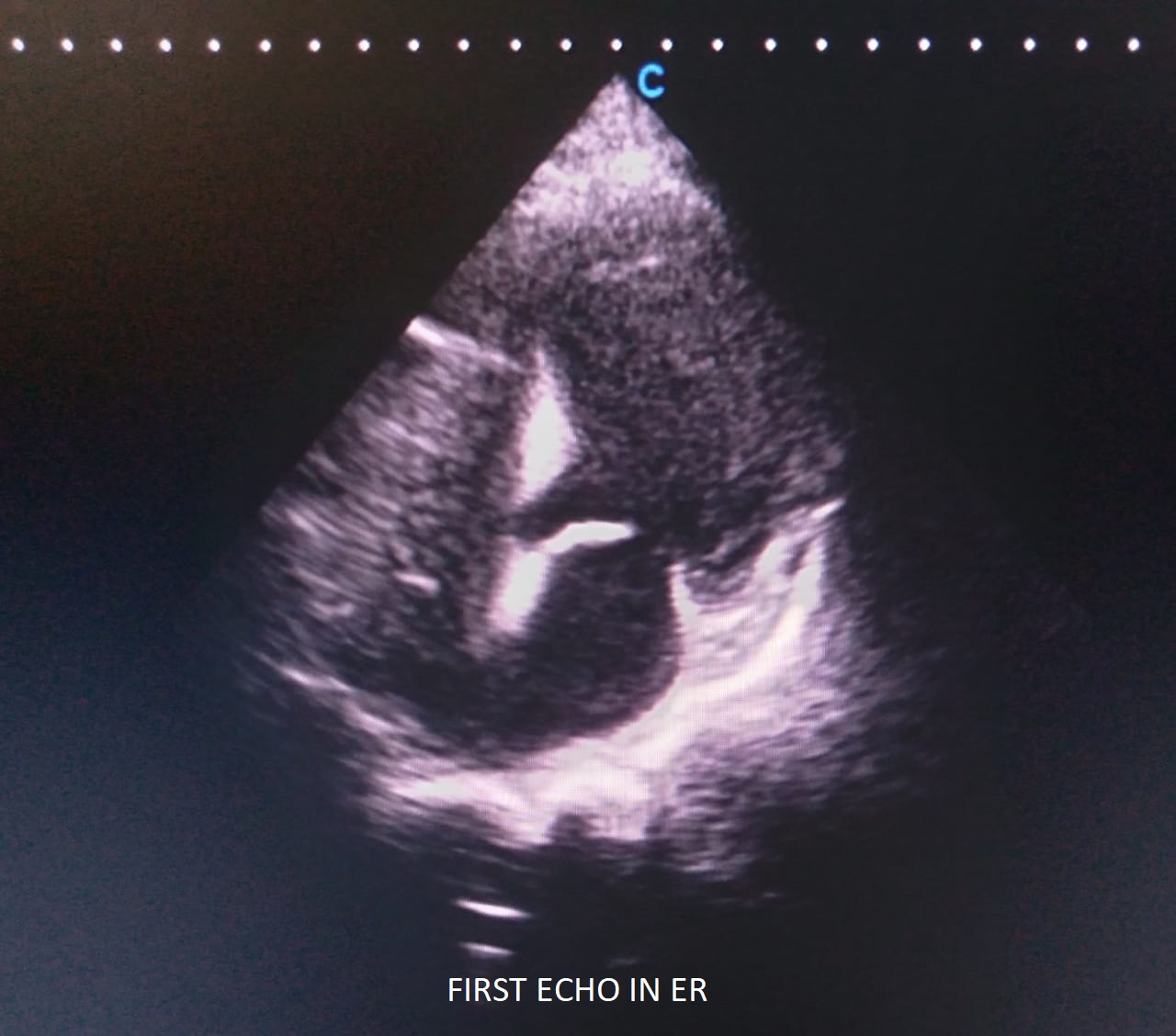
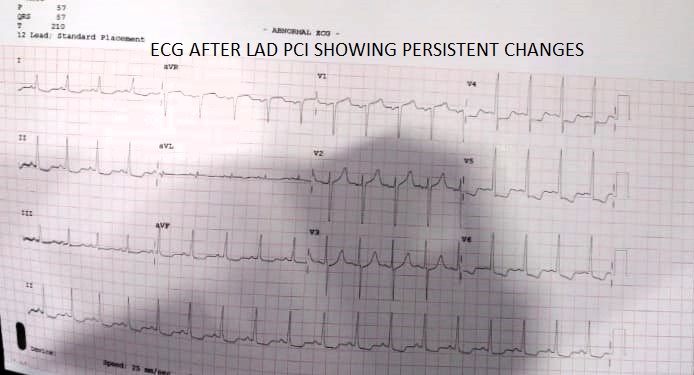
ECG showed tachycardia, ST elevation in AVR and V1, and ST depression in II, III, AVF, V4-V6. Bedside Echo revealed distal septal and apical akinesia, global hypokinesia of other segments with no significant MR, and marked diastolic dysfunction. LVEF was 25-30%. Patient was taken for emergency intervention and pathology results received later showed creatinine of 10.3 mg/dL, BUN of 98 mg/dL, Hb of 9.8 g/dL, positive troponin I assay and electrolyte panel showing hyperkalemia at 5.8 mEq/L.
Relevant Catheterization Findings
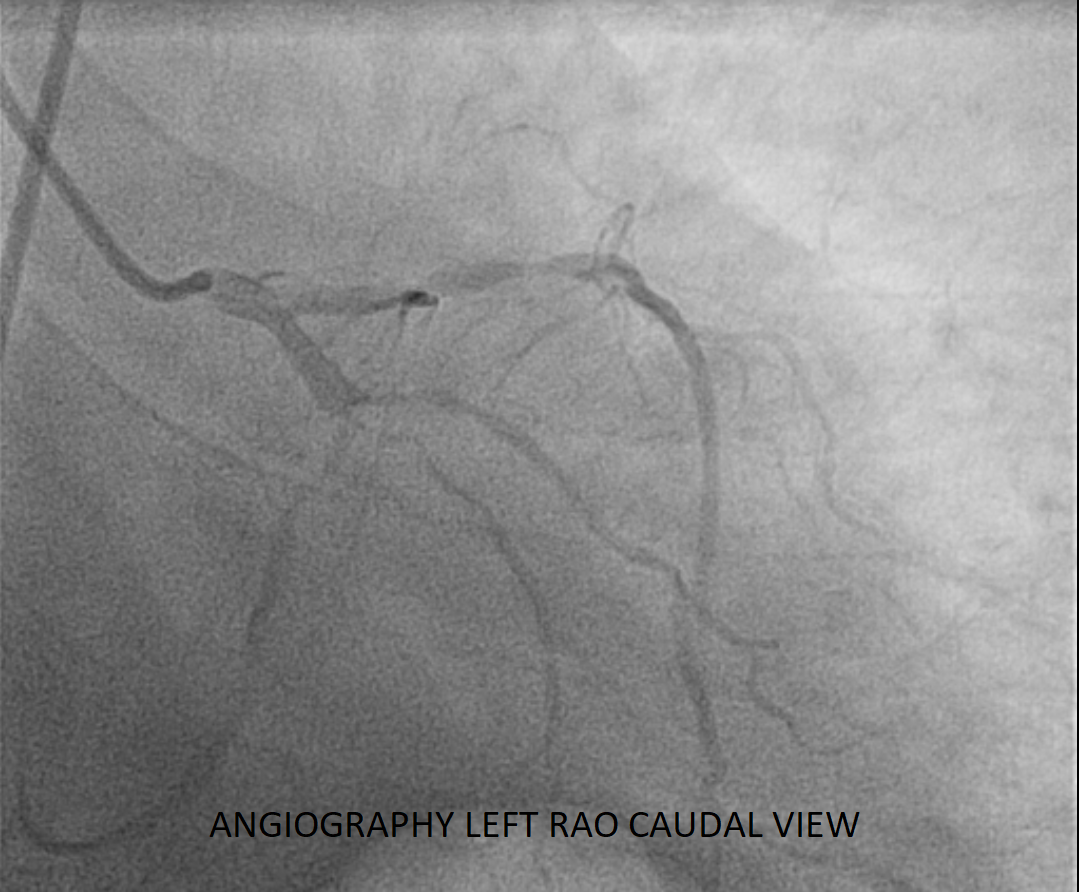
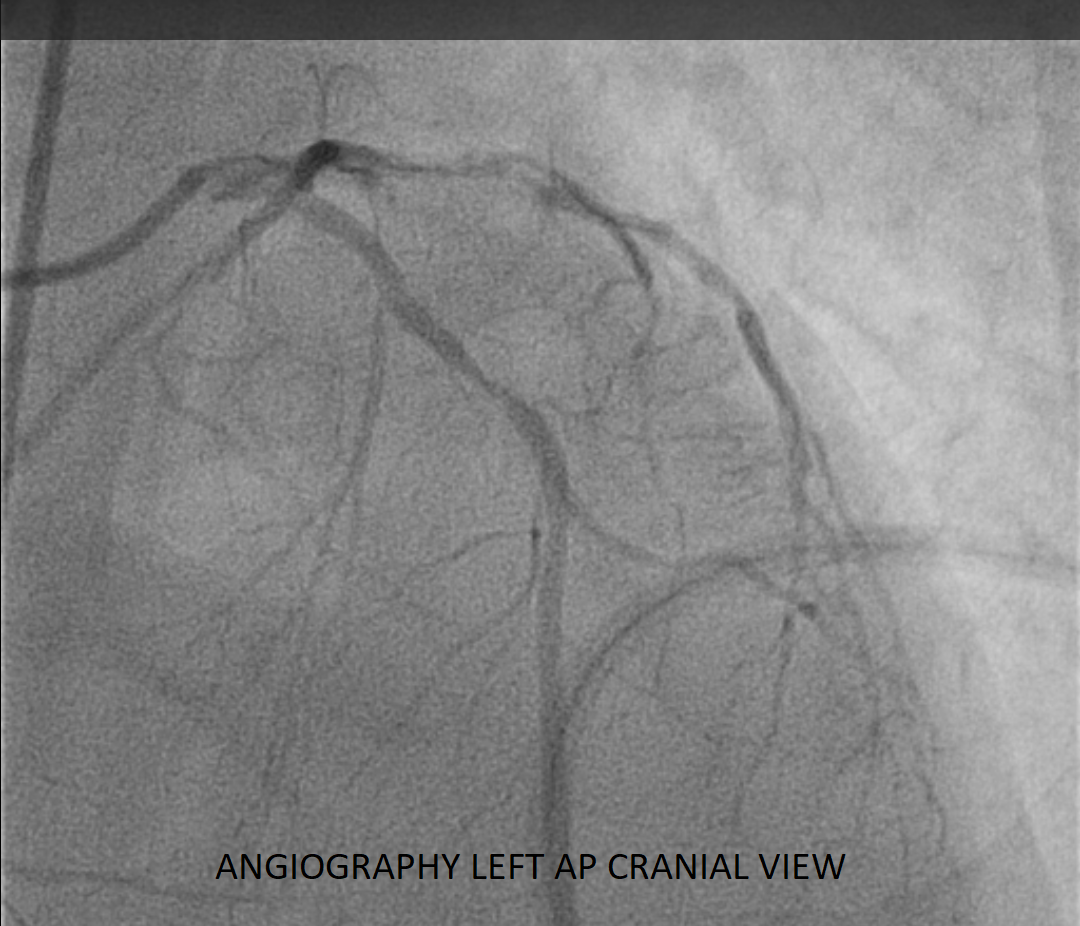
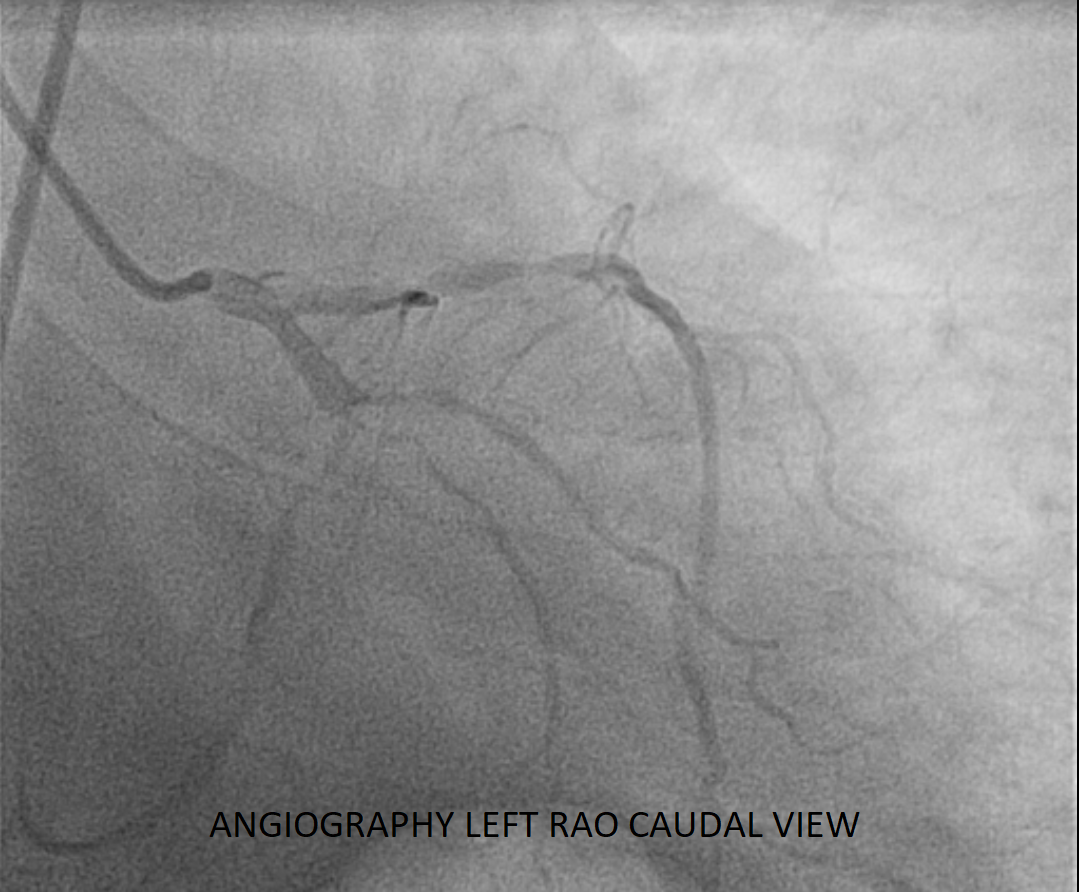
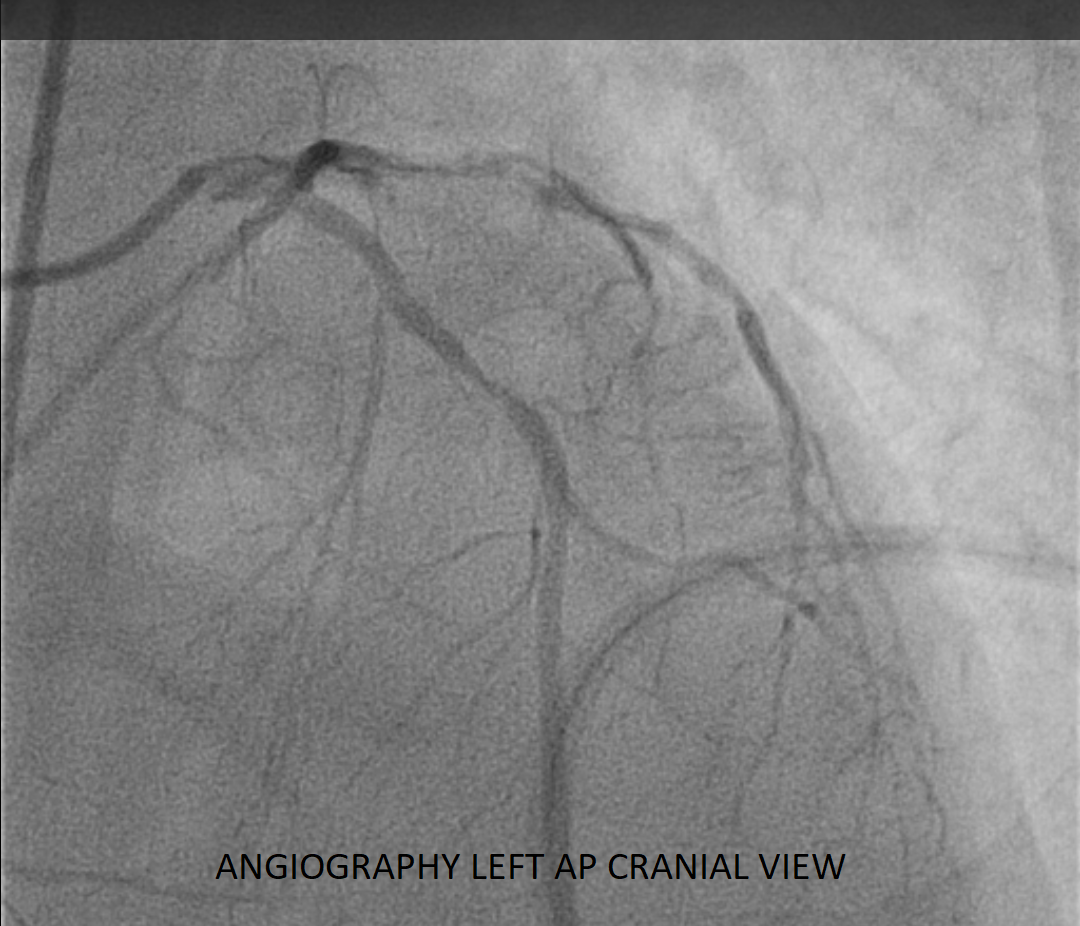
Angiography was done from right femoral route and a right venous sheath was also placed. Findings: Left Main was normal. LAD showed 90% long stenosis in proximal LAD, plaque in mid LAD, diagonal was normal. LCX was large and dominant with proximal to mid segment long 90% stenosis, large OM1 at 90% in proximal segment, PDA and PLV were under filled. RCA was a non-dominant small caliber vessel, showing 70% stenosis at ostium.


Interventional Management
Procedural Step
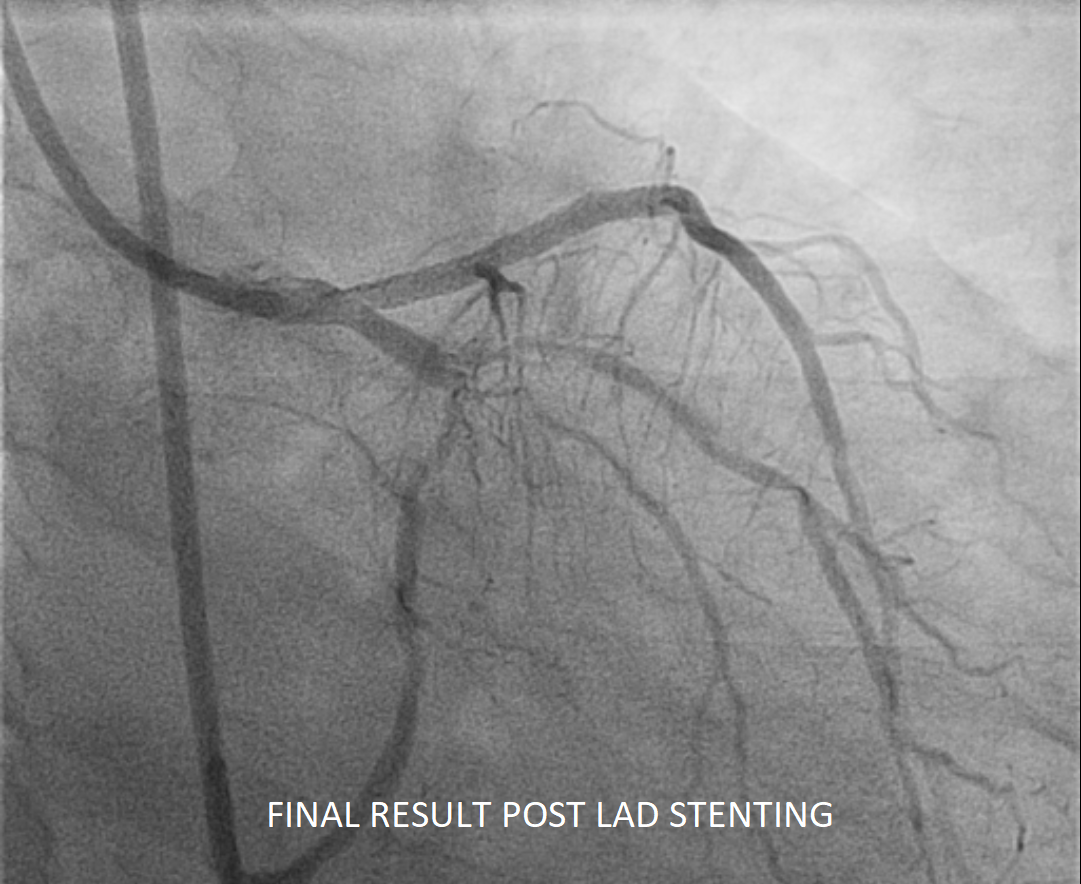
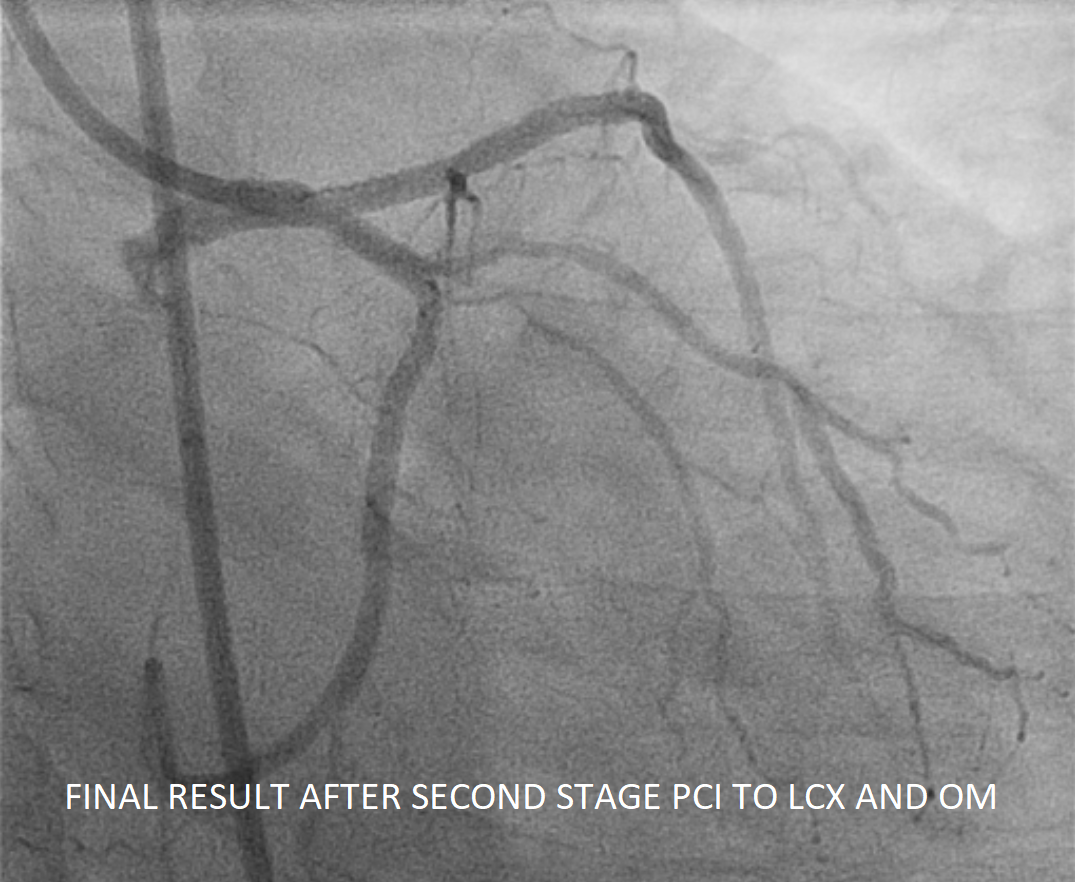
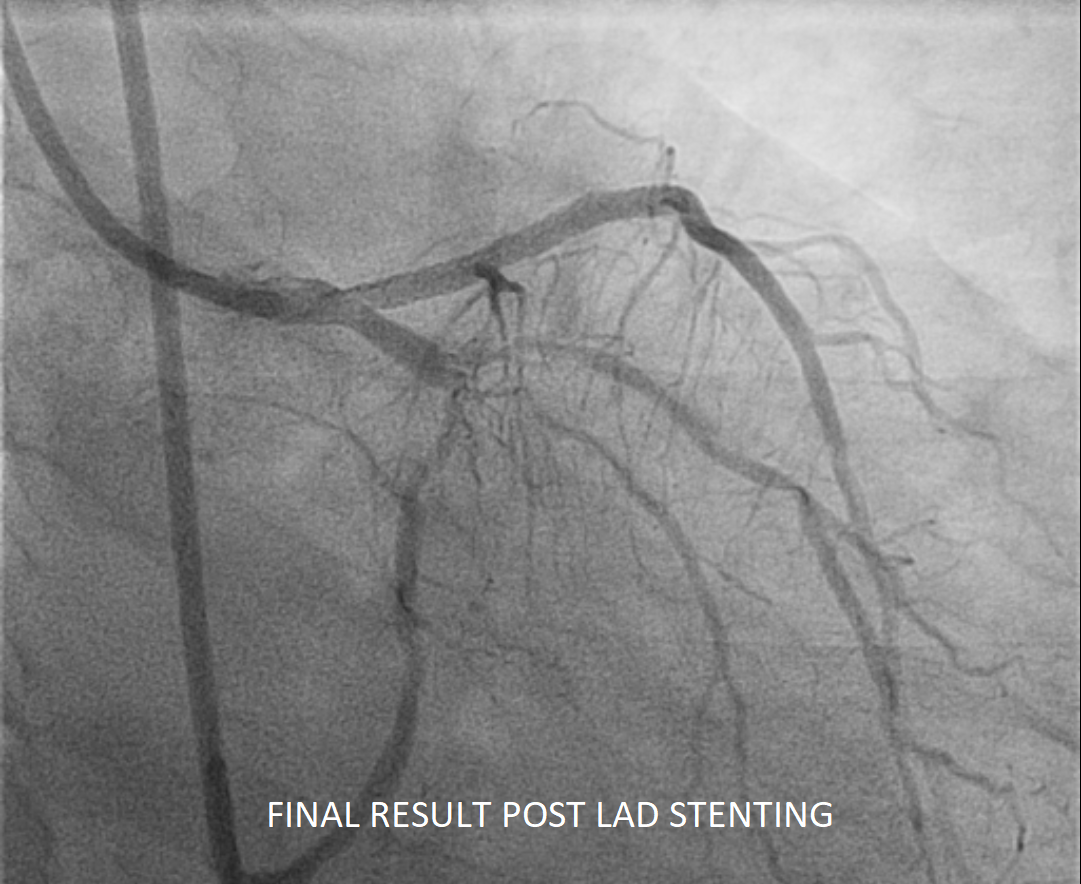
Immediate PTCA was performed. The LAD lesion was crossed with a Turn Trac wire, and pre-dilation was done using a 2.5x15mm NC TREK balloon. A 3.0x48mm XIENCE XPEDITION Stent (Abbott Vascular) was then deployed from the proximal to mid LAD covering the entire lesion. Post-dilation was done with a 3.25x15mm balloon, achieving TIMI III flow. Following procedure, the patient was placed on dialysis for ESRD, receiving three sessions over five days, but continued to remain ventilator-dependent. Patient was taken off sedation and found to be neurologically normal. ECG however, showed persistent ST-T changes, with regional wall motion abnormalities in LCX territory. Due to continued hemodynamic instability, a second-stage PTCA was performed with patient on ventilator. The LCX lesion was crossed with a Turn Trac wire and pre-dilated using a 2.5x15mm NC TREK balloon. Then, a 2.75 X 38 mm XIENCE Alpine Stent (Abott Vascular) was deployed in LCX covering entire lesion. Thereafter, another Turn Trac wire was passed in OM 1 through the stent and pre-dilatation of OM1 was performed with a 2.5x15mm NC TREK balloon. The lesion was then dilated using a 2.5x20mm MagicTouch Sirolimus Eluting Balloon, followed by final kissing dilatation achieving TIMI III flow. Following staged PCI and stabilization, the patient’s LVEF improved to 40-45%. The patient was weaned from the ventilator, and continued on outpatient dialysis. He was discharged in stable condition.
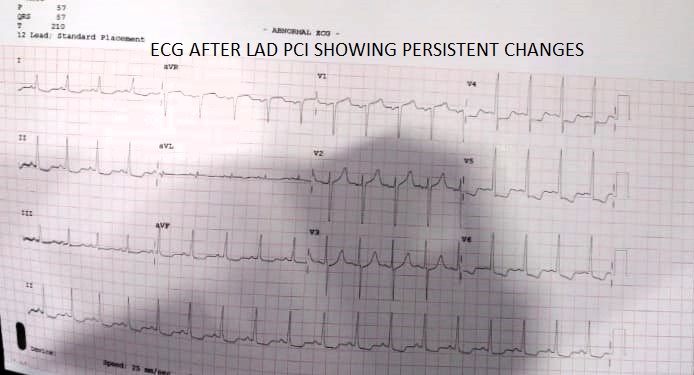
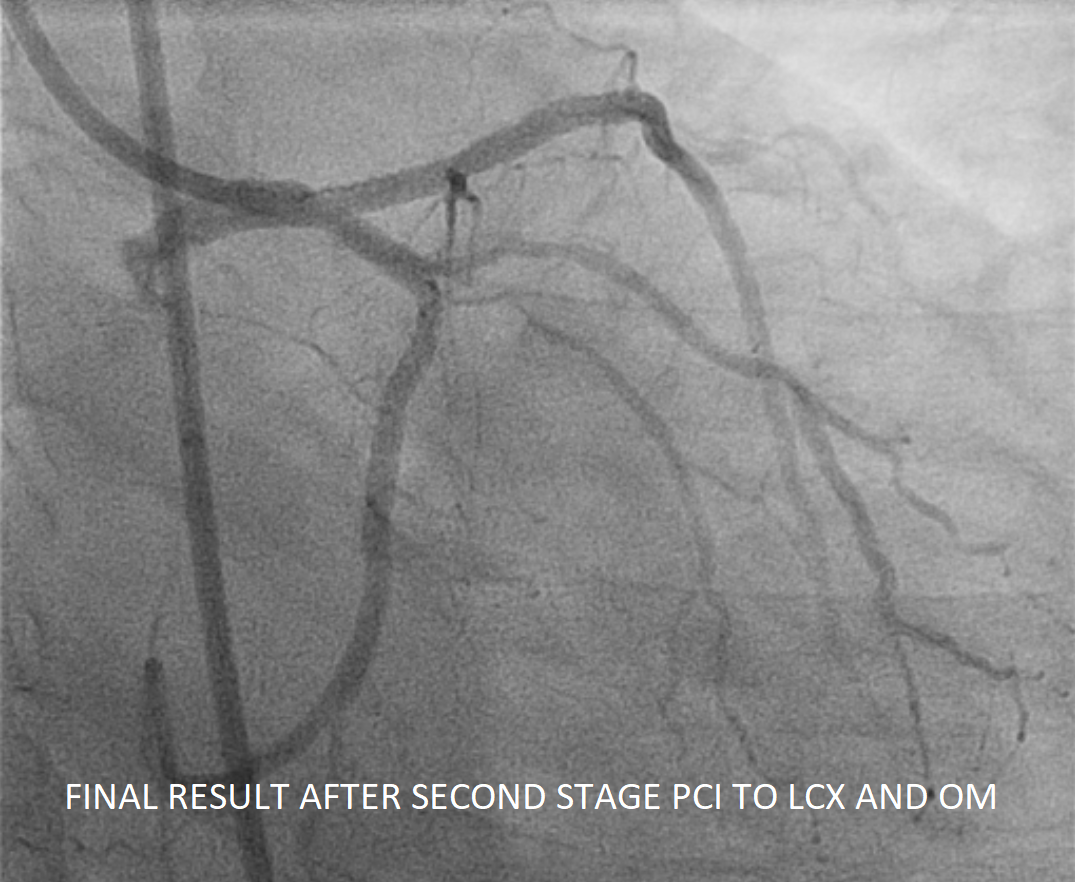
Case Summary
Despite the life-threatening presentation, a strategic PCI approach was effective. Initial ECG showed marked ST elevation in AVR and V1, and ST depression in multiple leads, suggesting possible severe disease in the proximal LAD/multivessel disease. Given CKD history, minimal dye was used, addressing only the LAD swiftly to promote recovery. He, however, remained ventilator-dependent despite dialysis. Further intervention of the dominant LCX and OM1 completed revascularization, improving ECG, LV function, and enabling ventilator weaning. This case highlights the utility of swift, individualized, staged intervention in managing critically ill patients with complex multivessel CAD and ESRD.


