Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-119
Bioresorbable Vascular Scaffolds in Treating Left Mainstem Coronary Artery Disease: A First Long-Term Imaging Analysis
By Kei Tung Wong, Siu Fung Wong, Hiu Cheong Chow, Tak Shun Chung
Presenter
Kei Tung Wong
Authors
Kei Tung Wong1, Siu Fung Wong1, Hiu Cheong Chow1, Tak Shun Chung1
Affiliation
United Christian Hospital, Hong Kong, China1,
View Study Report
TCTAP C-119
Coronary - Complex PCI - Left Main
Bioresorbable Vascular Scaffolds in Treating Left Mainstem Coronary Artery Disease: A First Long-Term Imaging Analysis
Kei Tung Wong1, Siu Fung Wong1, Hiu Cheong Chow1, Tak Shun Chung1
United Christian Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
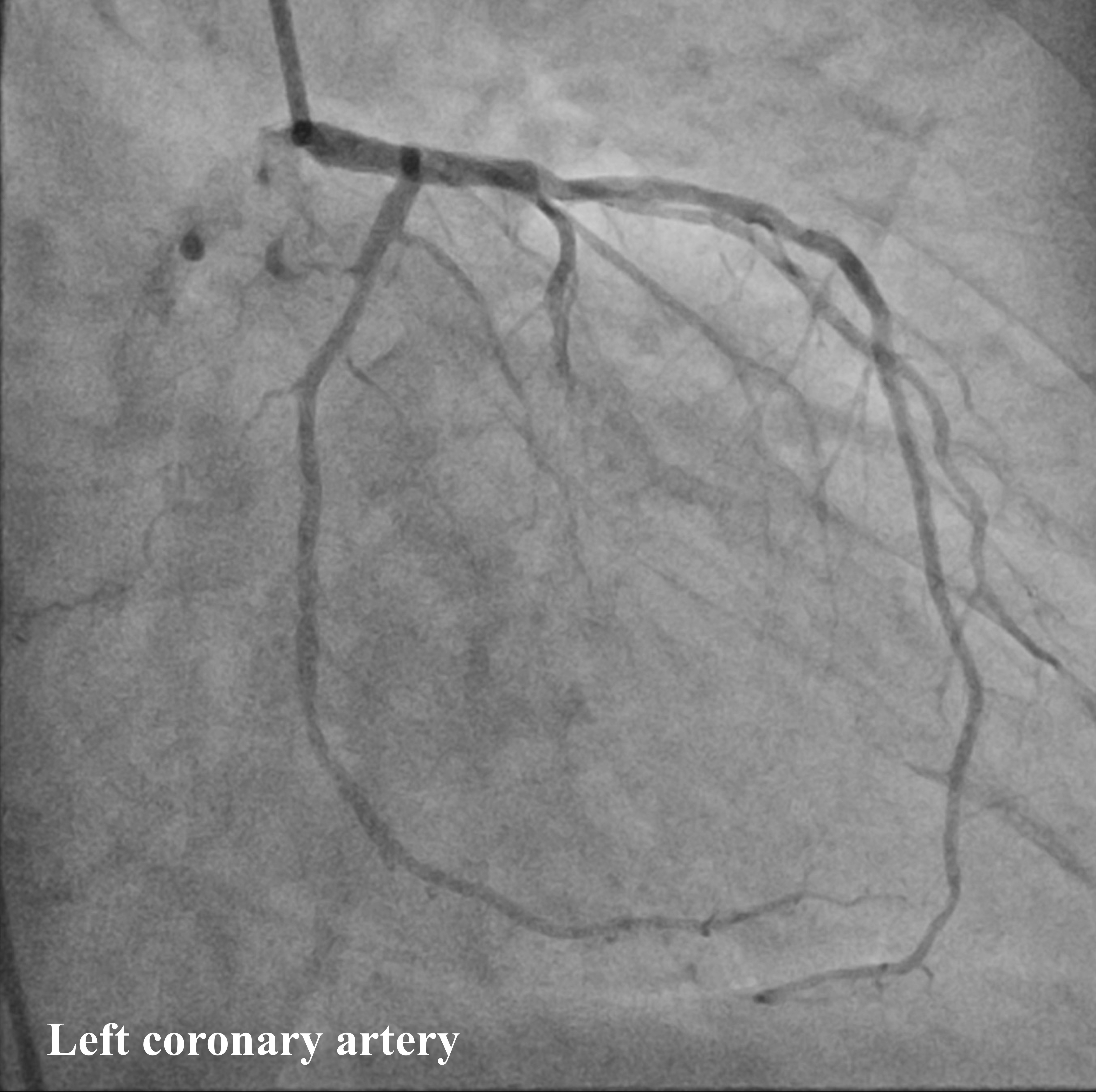
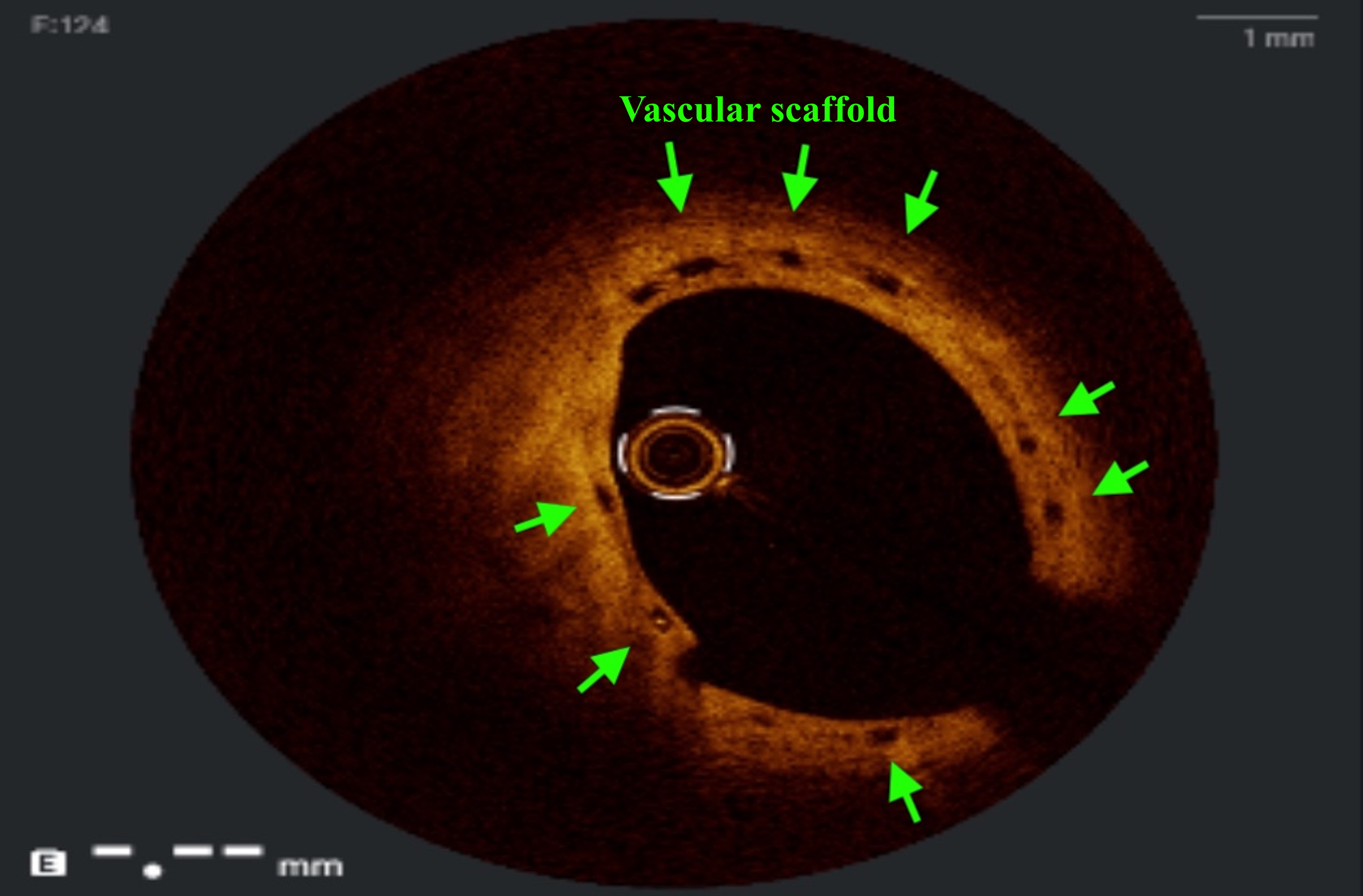
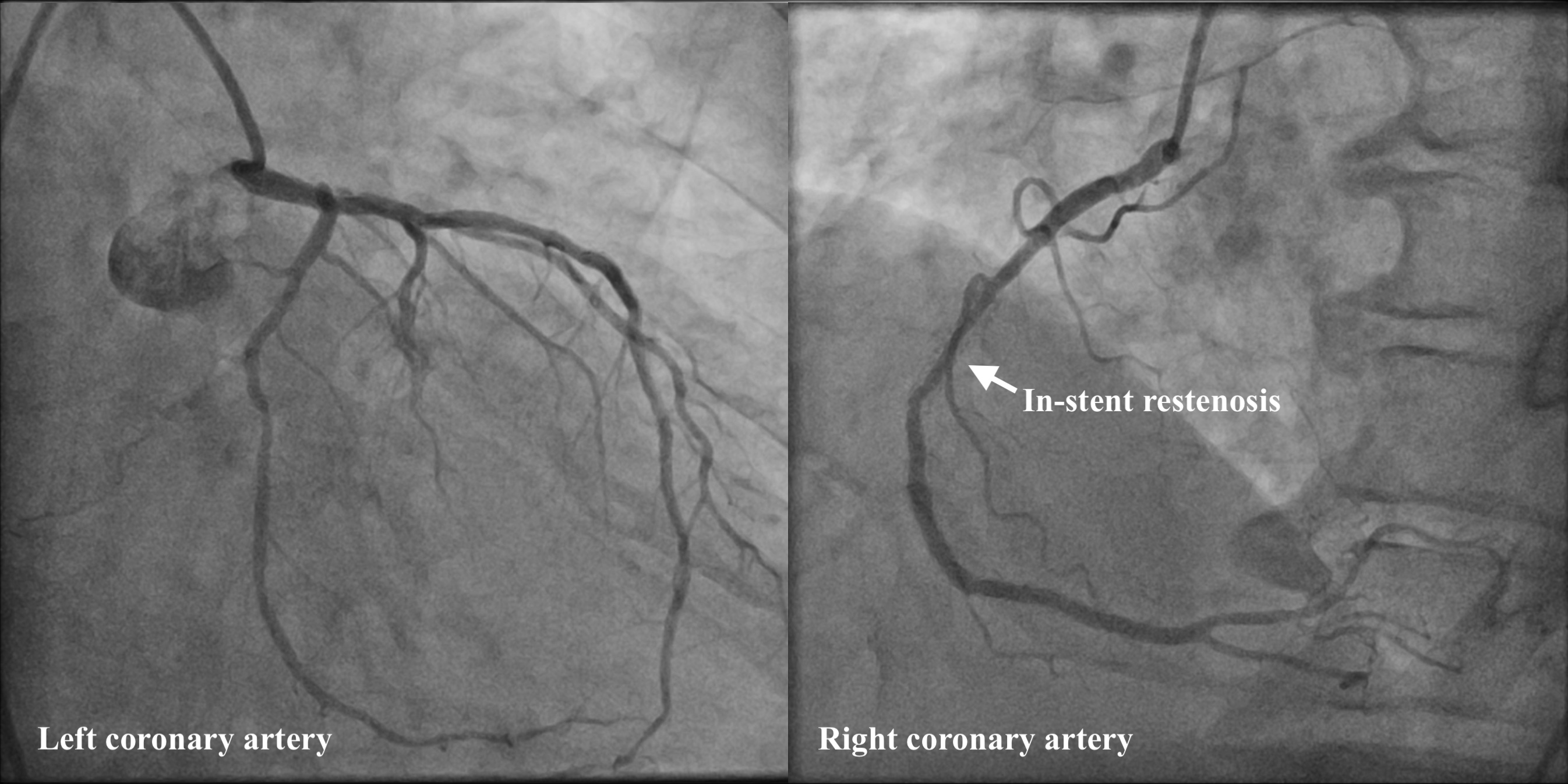
63-year-old male with left main coronary artery (LM) and triple vessel disease had percutaneous coronary intervention in 2016. 3 Absorb biovascular scaffolds (BVS) (Abbott, USA) were implanted from LM to left anterior descending artery (LAD) and 2 BVS in left circumflex artery (LCx). Right coronary artery was treated with drug-eluting stent. Left coronary artery was patent on restudy coronary angiogram and optical coherence tomography in 2018 (Figure 1, 2). His anginal symptoms relapsed in 2024.
Relevant Test Results Prior to Catheterization
Echocardiography showed mildly impaired left ventricular ejection fraction.
Relevant Catheterization Findings
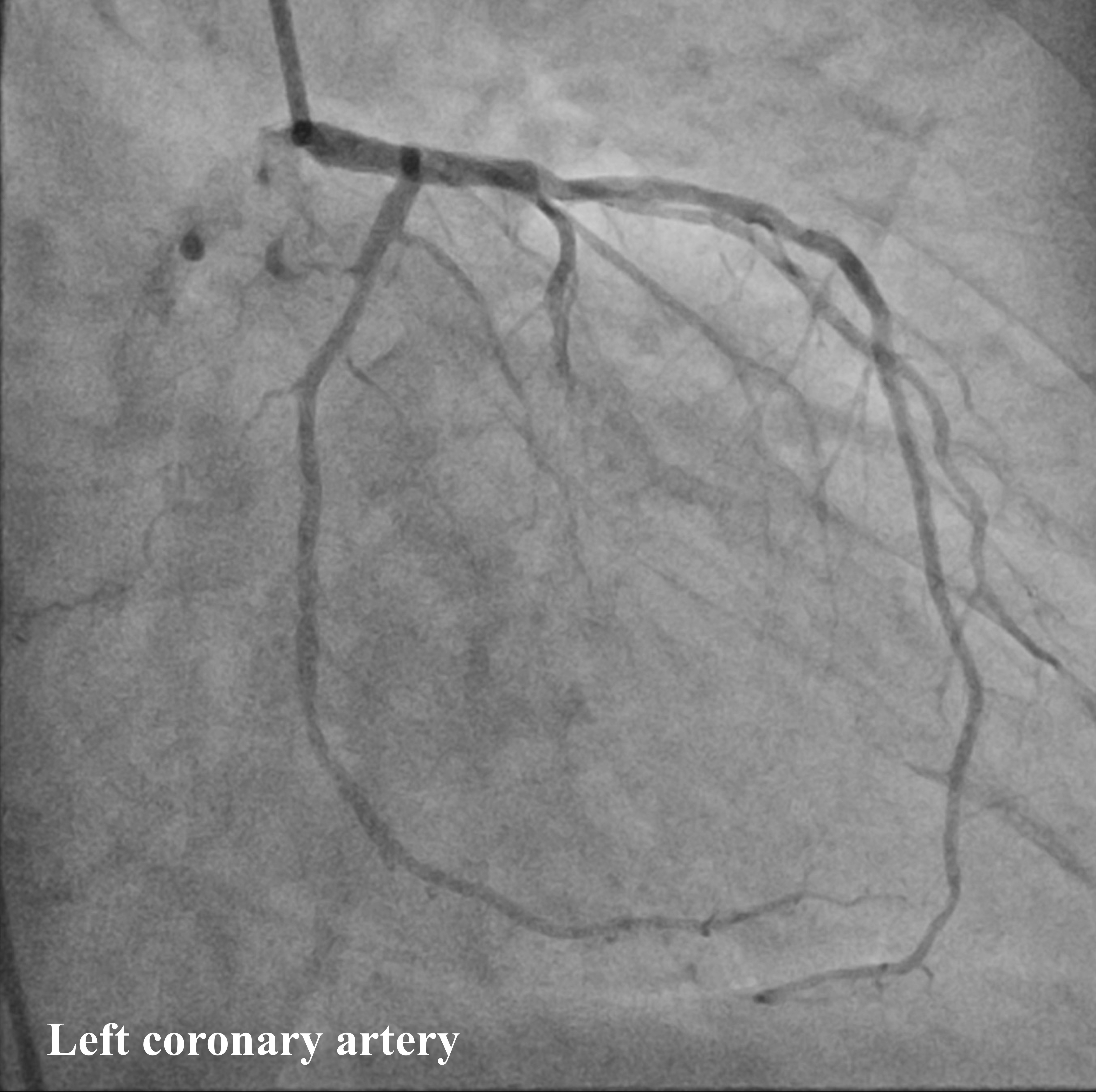
Coronary angiography showed normal LM, mild disease in LAD and LCx, and severe in-stent restenosis in right coronary artery (Figure 3).
Interventional Management
Procedural Step
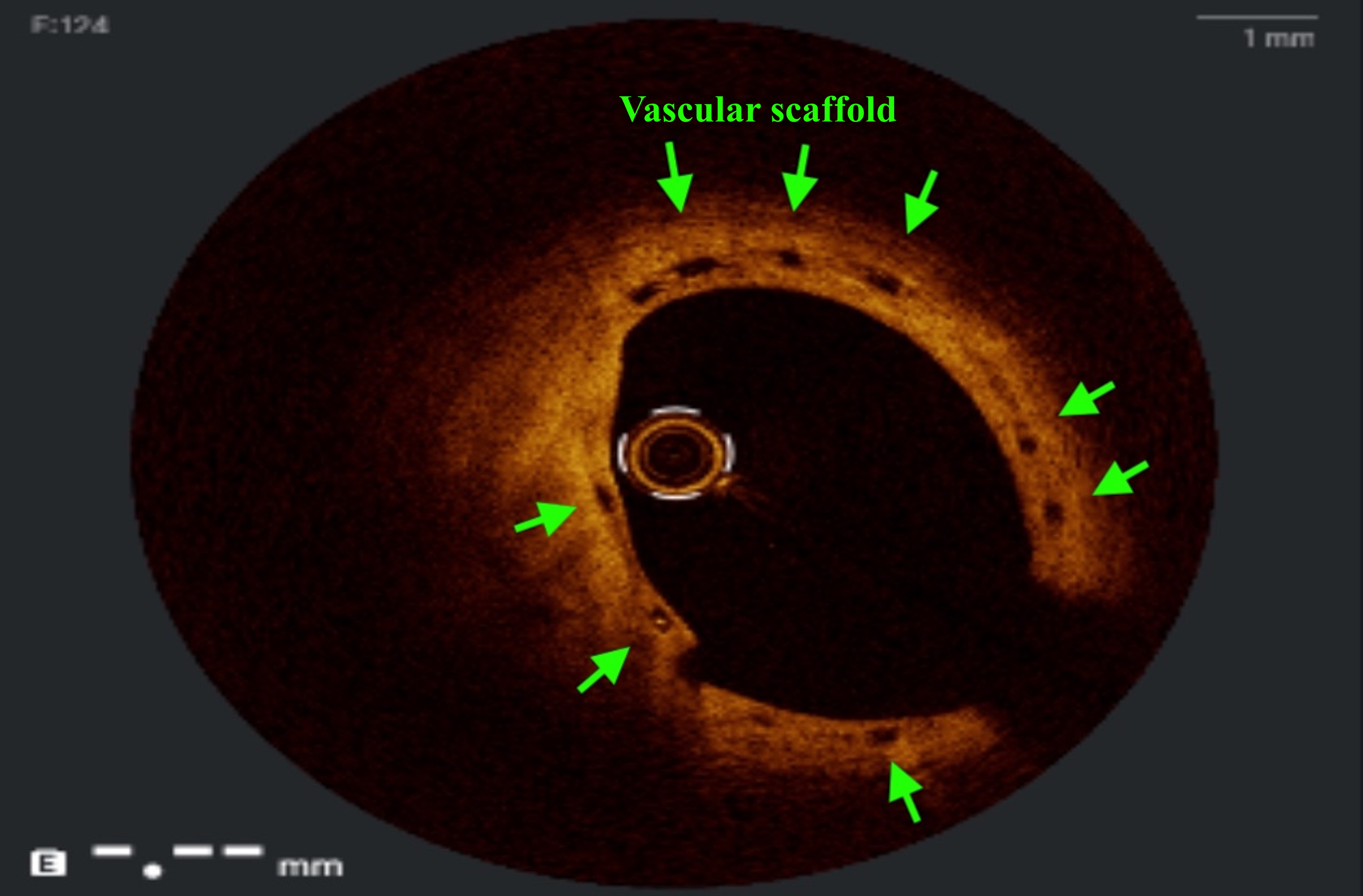
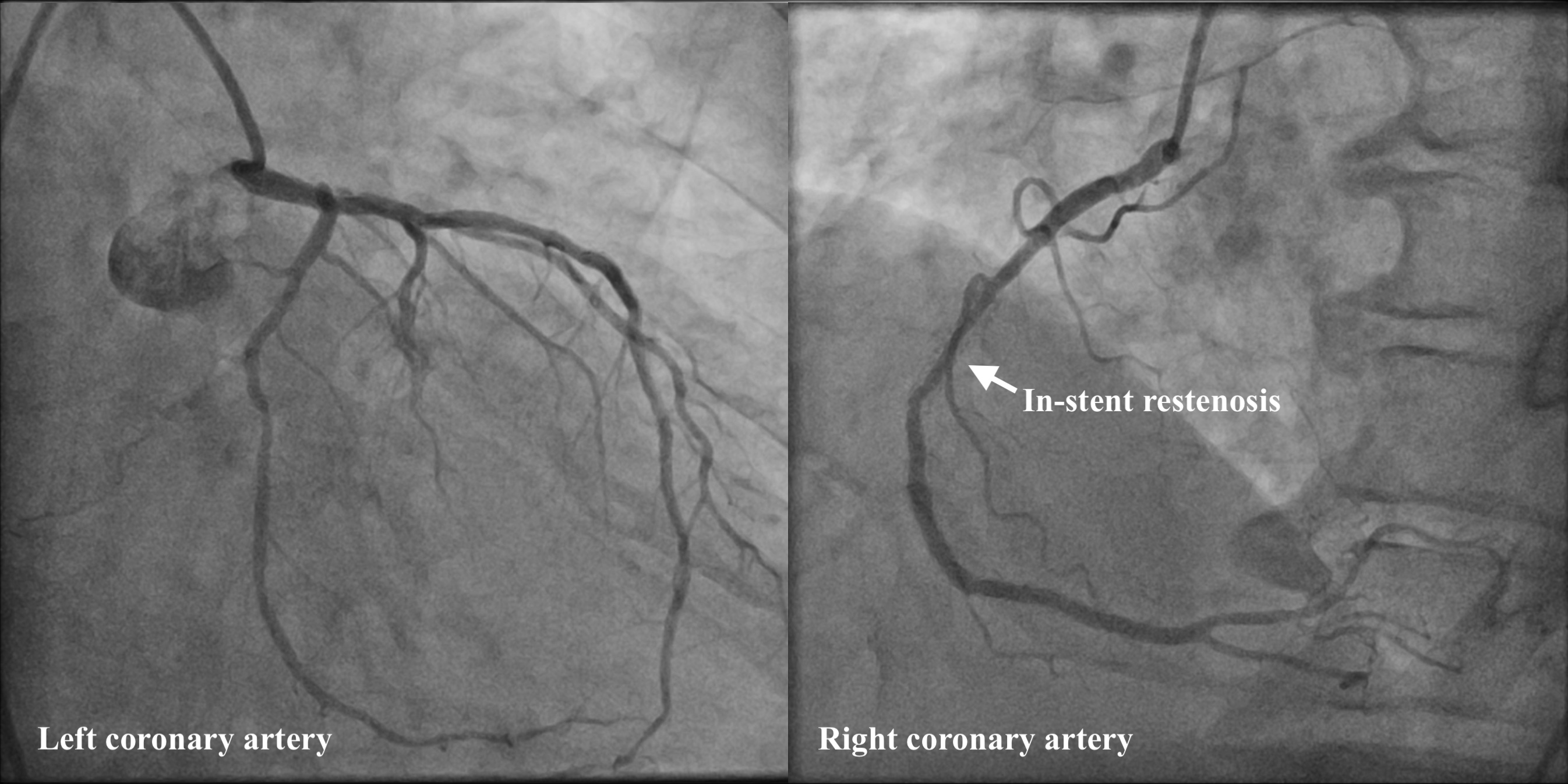
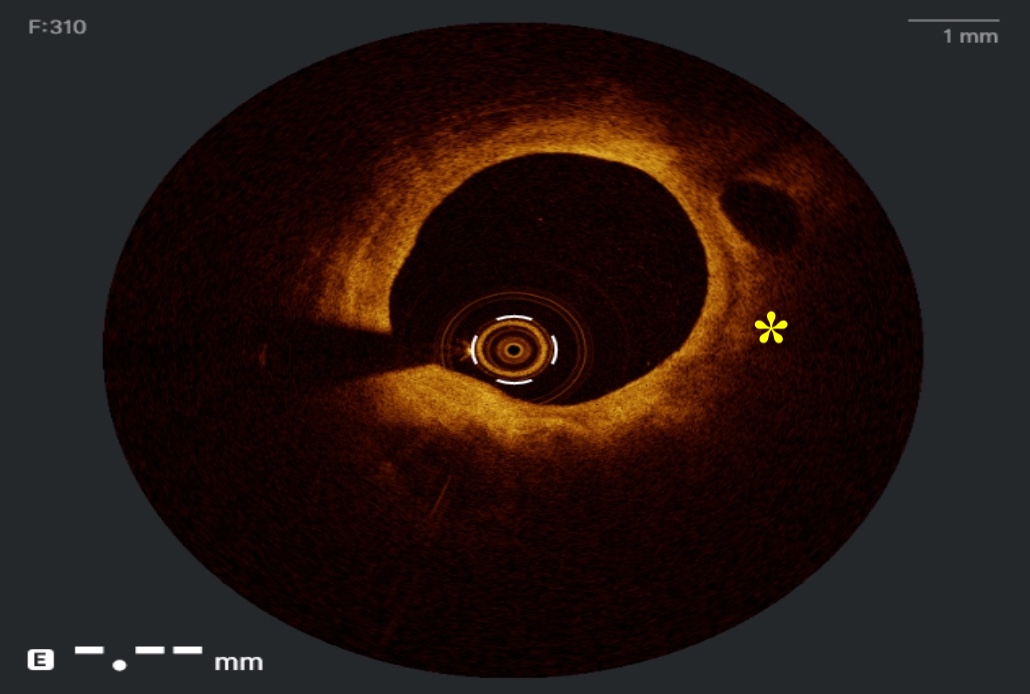
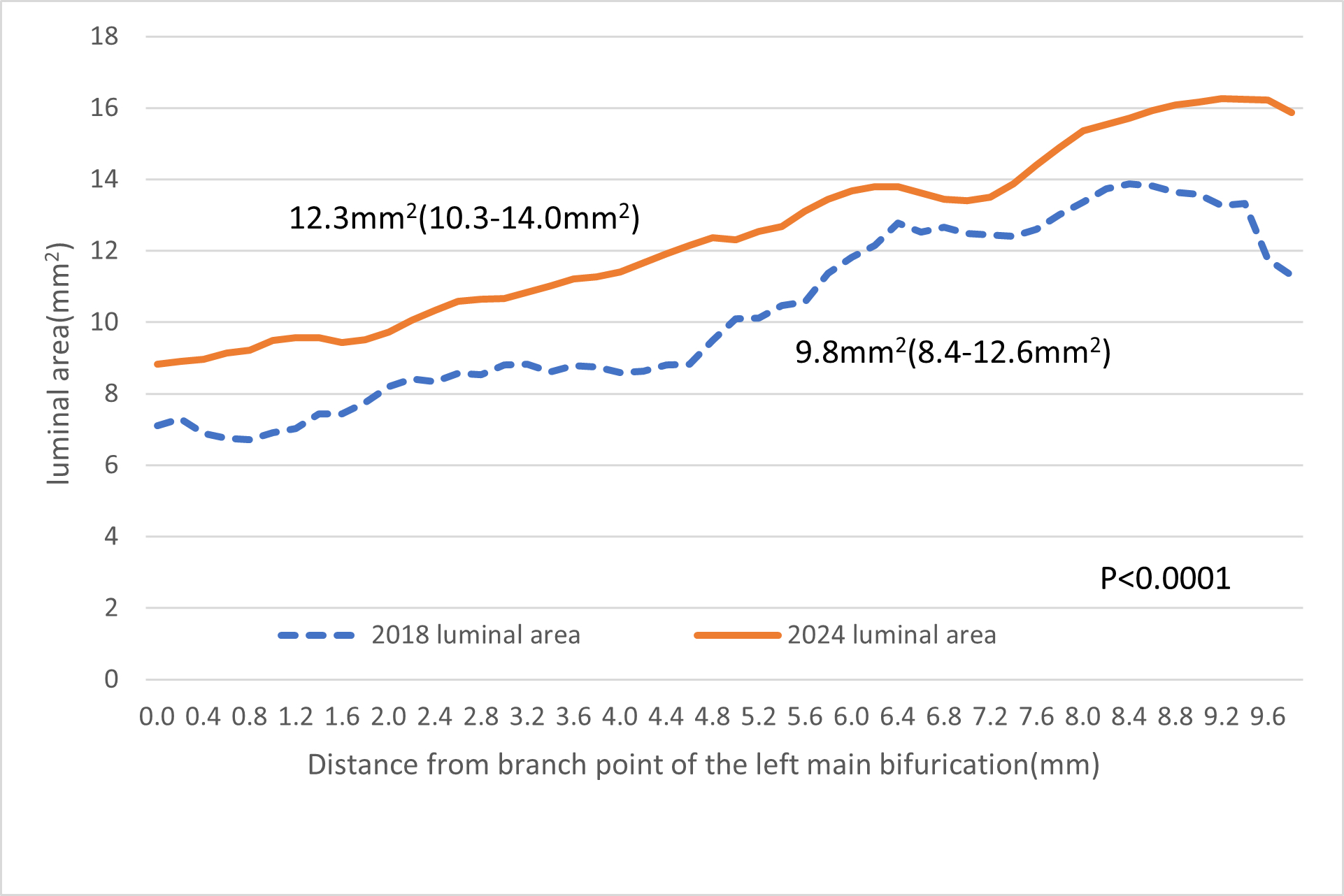
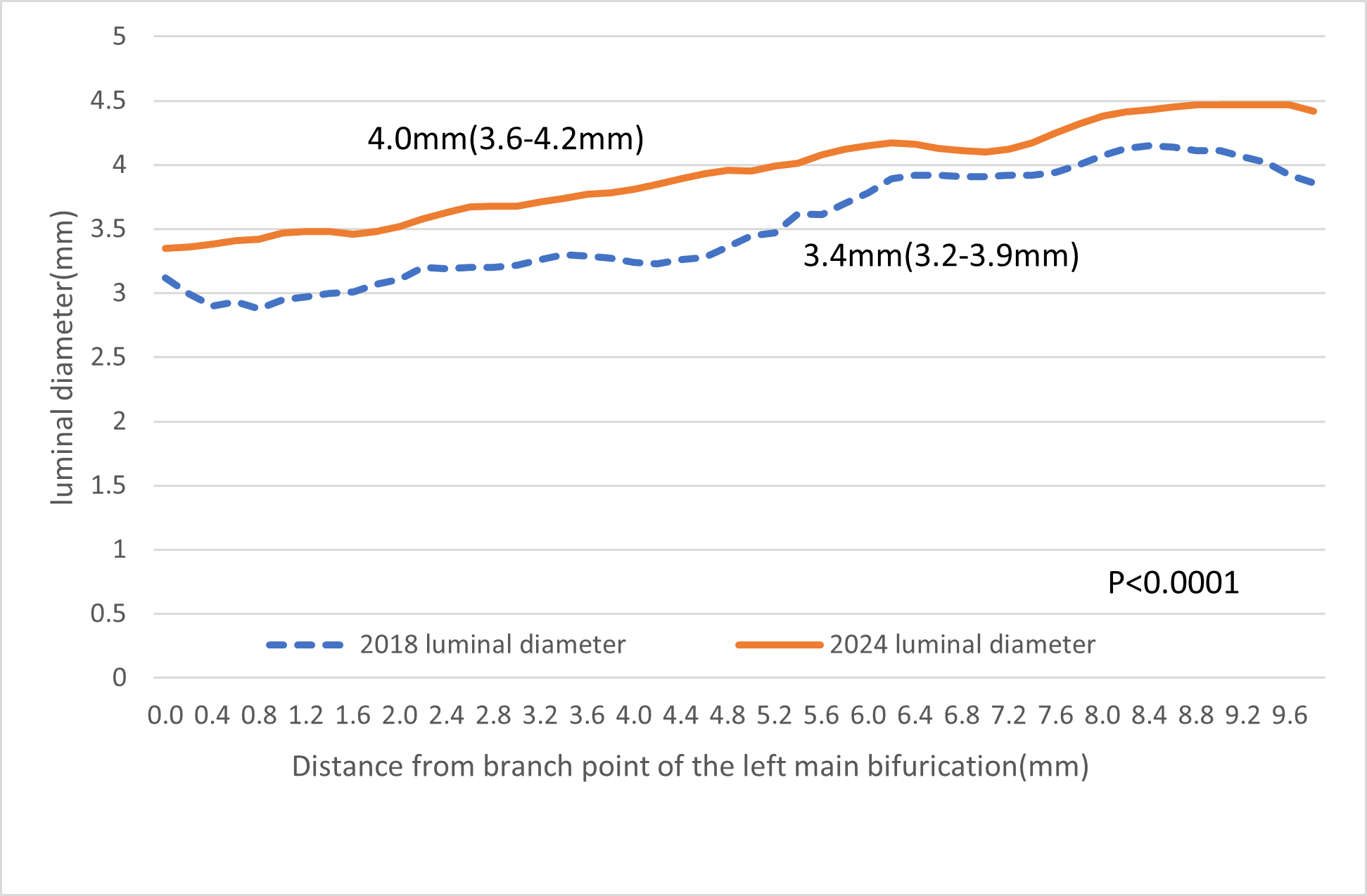
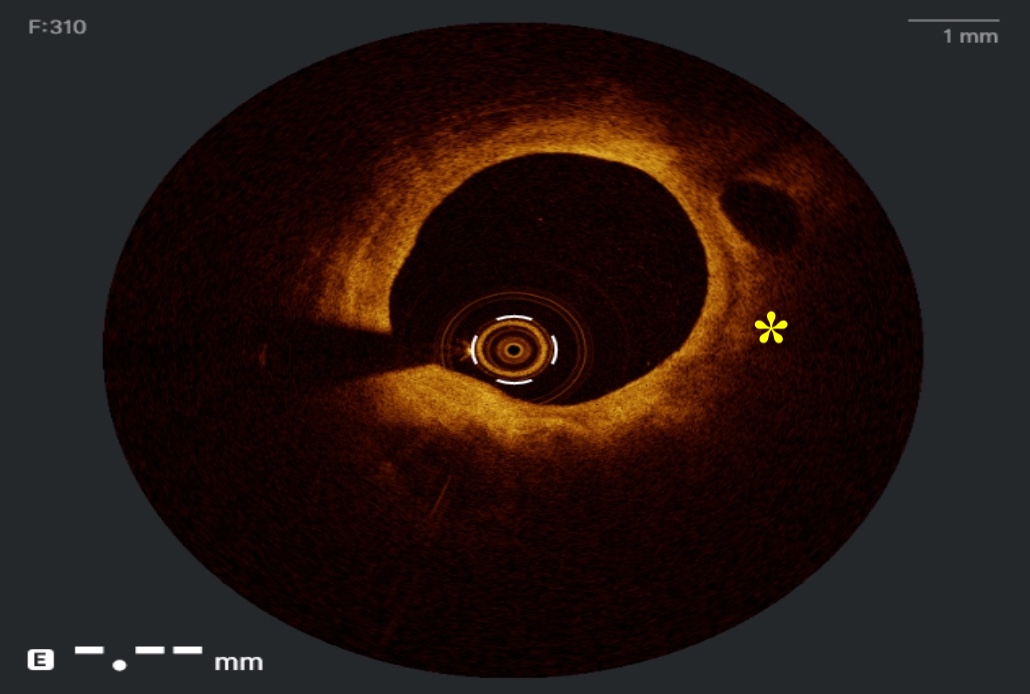
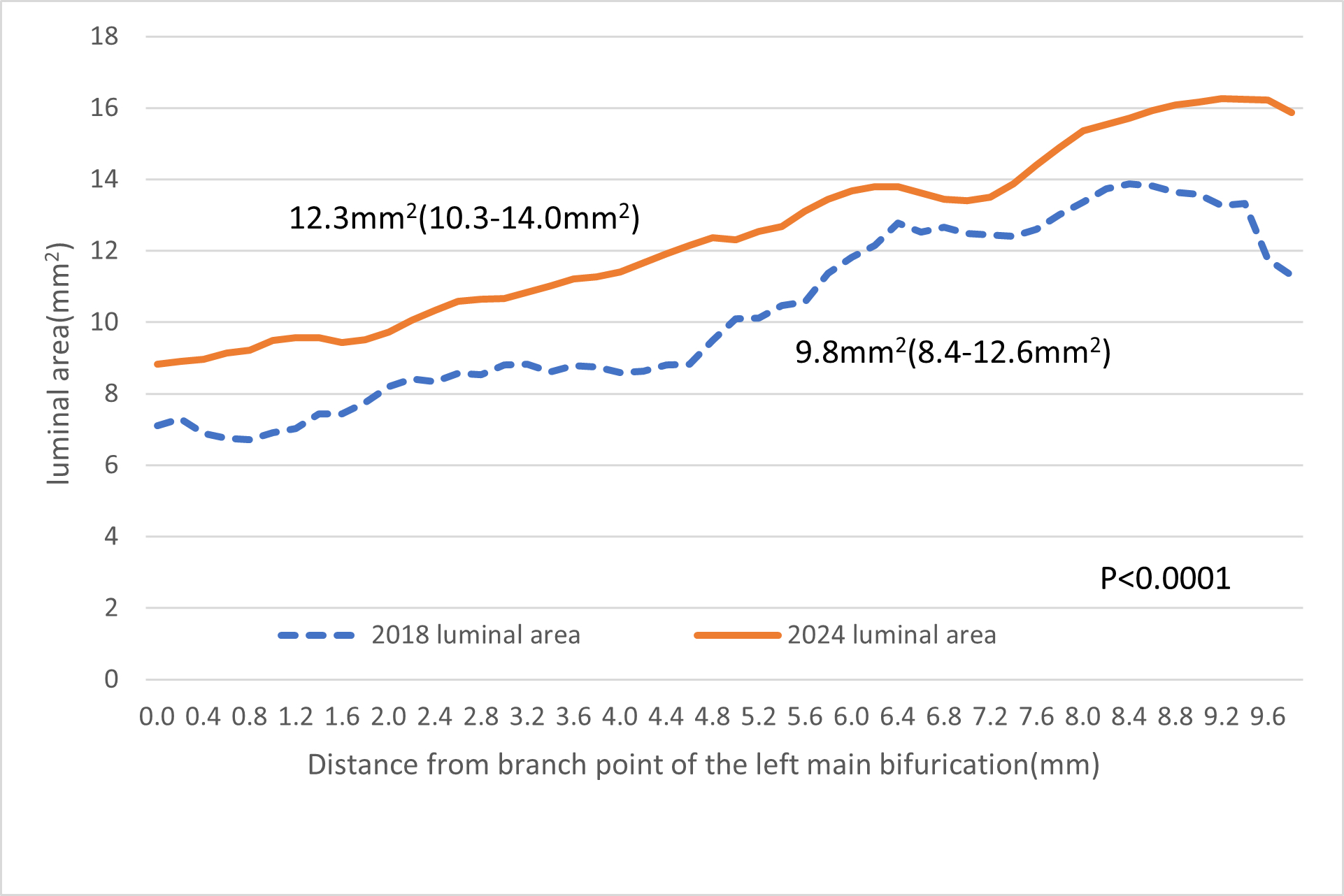
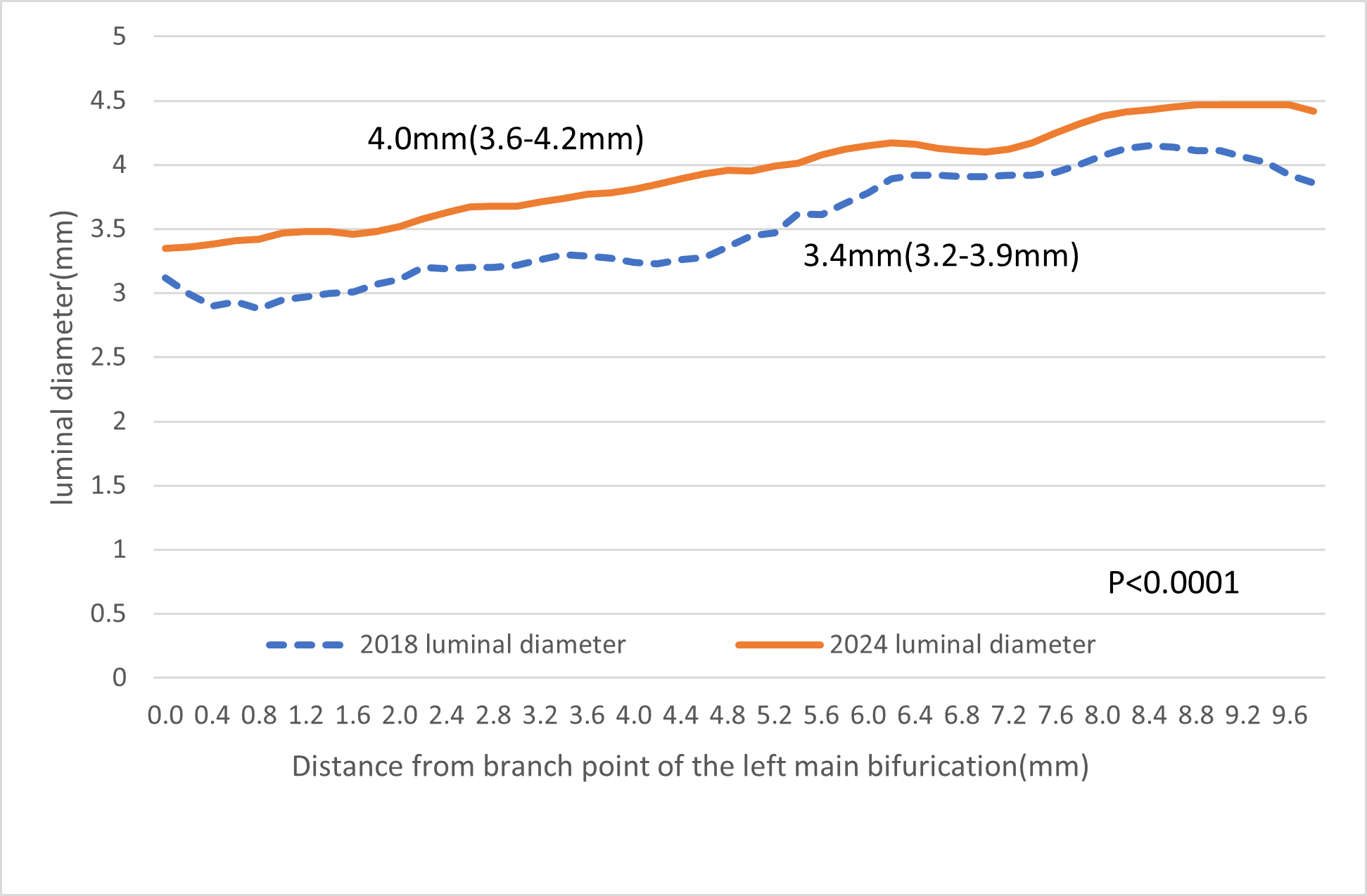
Optical coherence tomography (OCT) assessment of the LM showed all scaffolds were completely resorbed. A thick and stable fibrous intimal cap (yellow asterisk, Figure 4) was seen overlying atherosclerotic plaque. There was significant luminal gain of LM when compared to the study in 2018. In OCT assessment, there was an increase in LM minimum luminal area (MLA) from 6.71 mm2 to 8.82 mm2, and an increase in LM minimum luminal diameter from 2.88mm to 3.35 mm2, with a percentage increase of 31.45% and 16.32% respectively. The median luminal area increased from 9.8mm2 to 12.3mm2 (p <0.0001) (Figure 5). The median luminal diameter increased from 3.41mm to 3.96mm (p<0.0001) (Figure 6). The RCA ISR was treated with drug-coated balloon.
Case Summary
BVS were uncommonly used in LM disease, owing to the size and limited over-expansion capacity of BVS. To our best knowledge, this is the first reported case of long-term follow-up of BVS in LM up to 8 years with serial analysis by intracoronary imaging. Our case demonstrated continuous positive remodeling with late luminal enlargement from 2 to 8 years after implantation. Use of BVS in LM is feasible with favorable long-term clinical and imaging results.


