Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-211
Navigating the Crossroads: Successfully Managing a Cruciform Fistula After Transcaval TAVI
By Yu-Chuan Chuang
Presenter
Yu-Chuan Chuang
Authors
Yu-Chuan Chuang1
Affiliation
Taichung Veterans General Hospital, Taiwan1,
View Study Report
TCTAP C-211
Structural - Aortic Valve Intervention - Non-femoral TAVR
Navigating the Crossroads: Successfully Managing a Cruciform Fistula After Transcaval TAVI
Yu-Chuan Chuang1
Taichung Veterans General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Relevant Test Results Prior to Catheterization
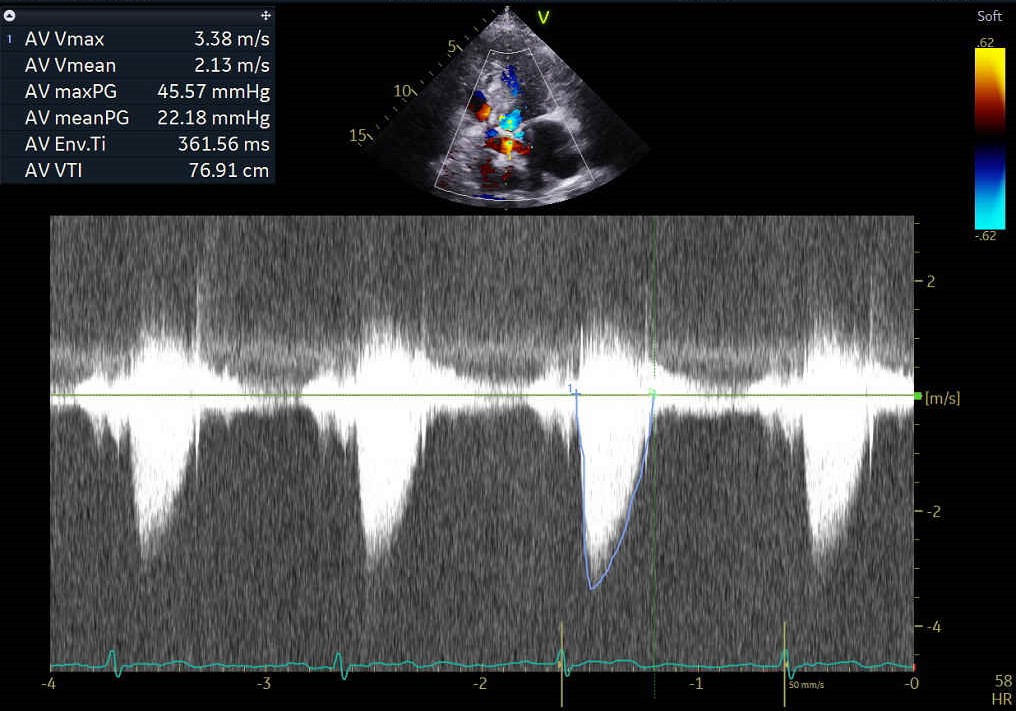
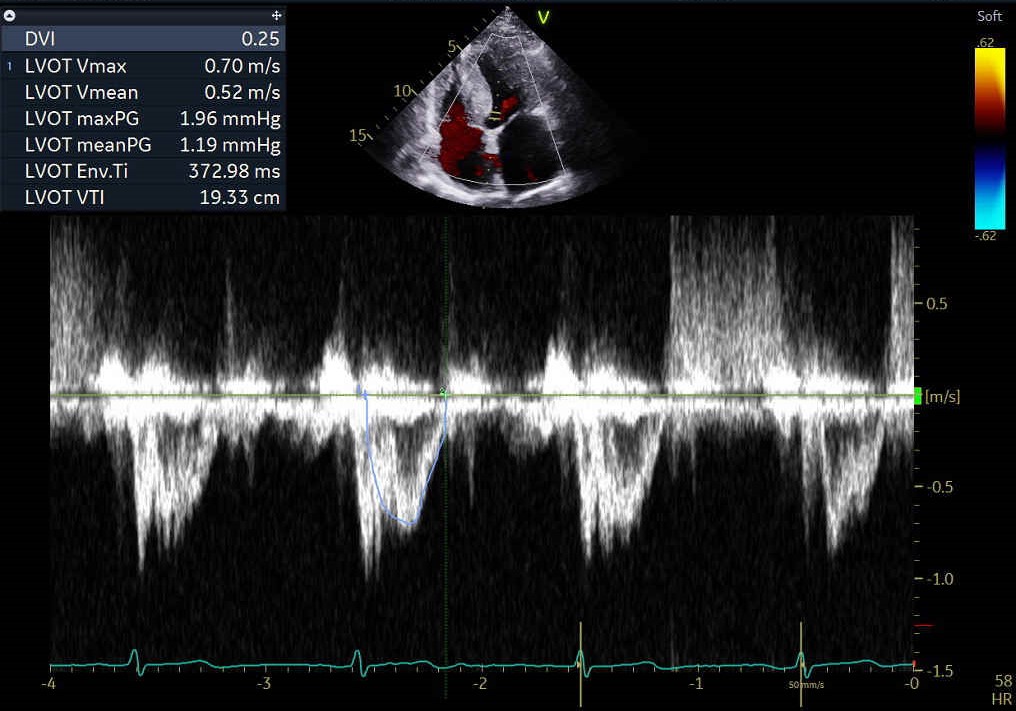
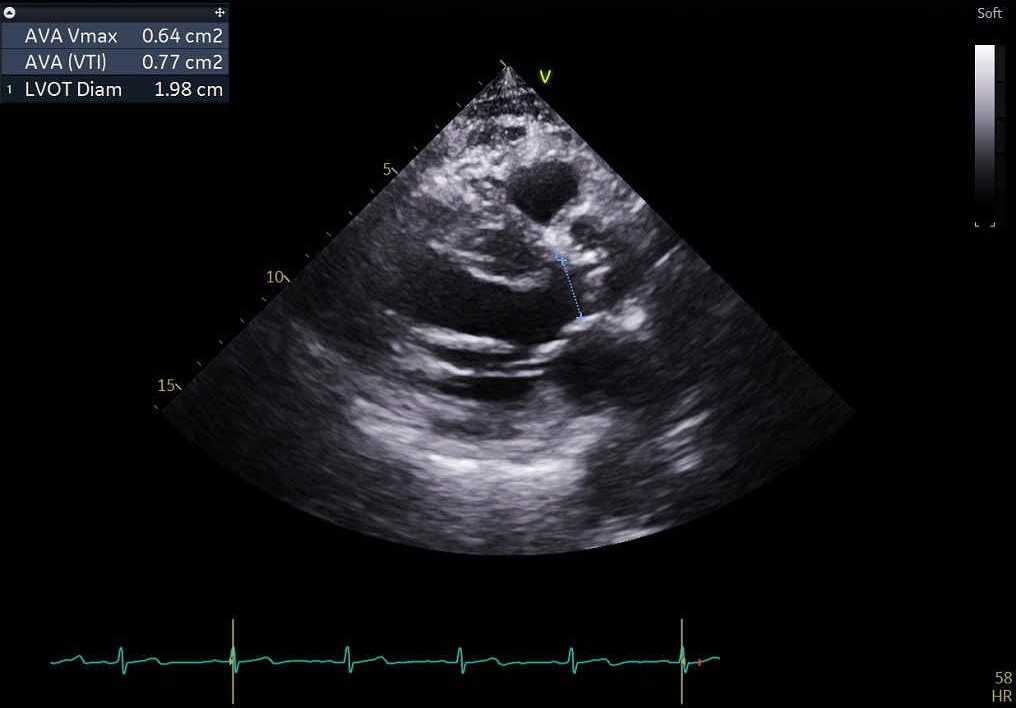
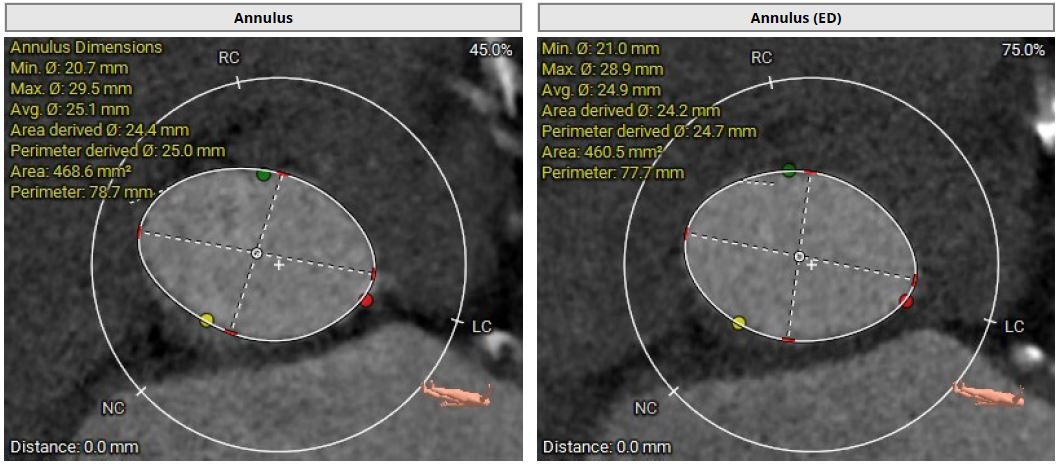
The echocardiographic findings indicate an LVEF of 55%, an aortic valve area of 0.77 cm², a maximum velocity of 3.28 m/s, a mean pressure gradient of 22 mmHg. Intermittent shortness of breath and heart failure symptoms have been reported for more than six months and are deemed to be related to low flow, low gradient severe aortic stenosis. His surgical risk, represented by an STS score of 12.4%, reinforces the decision to proceed with the TAVI intervention.
Relevant Catheterization Findings
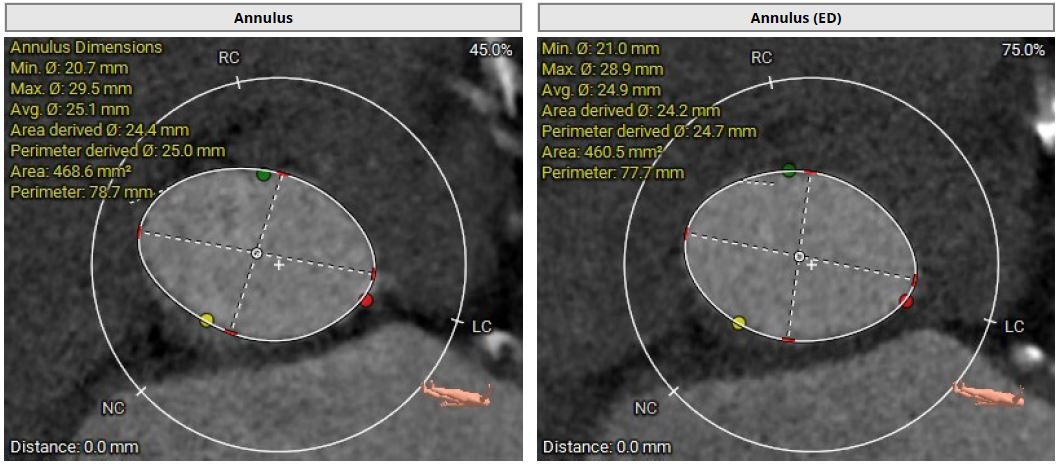
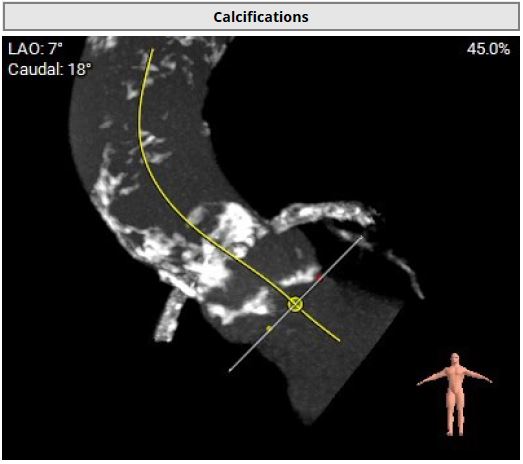
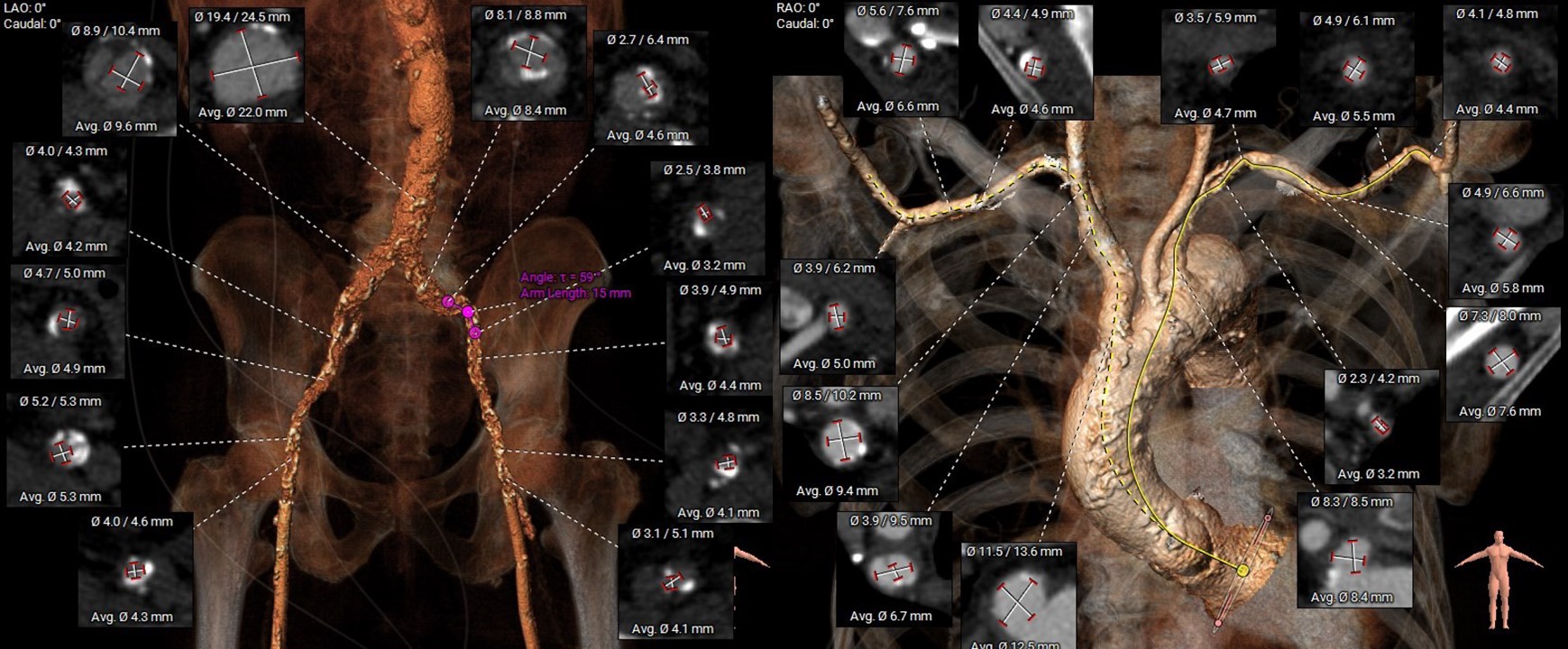
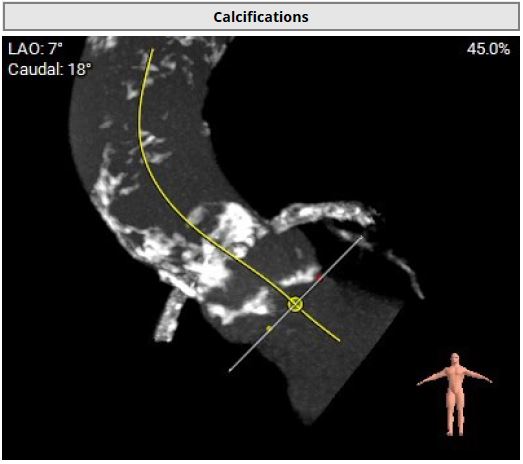
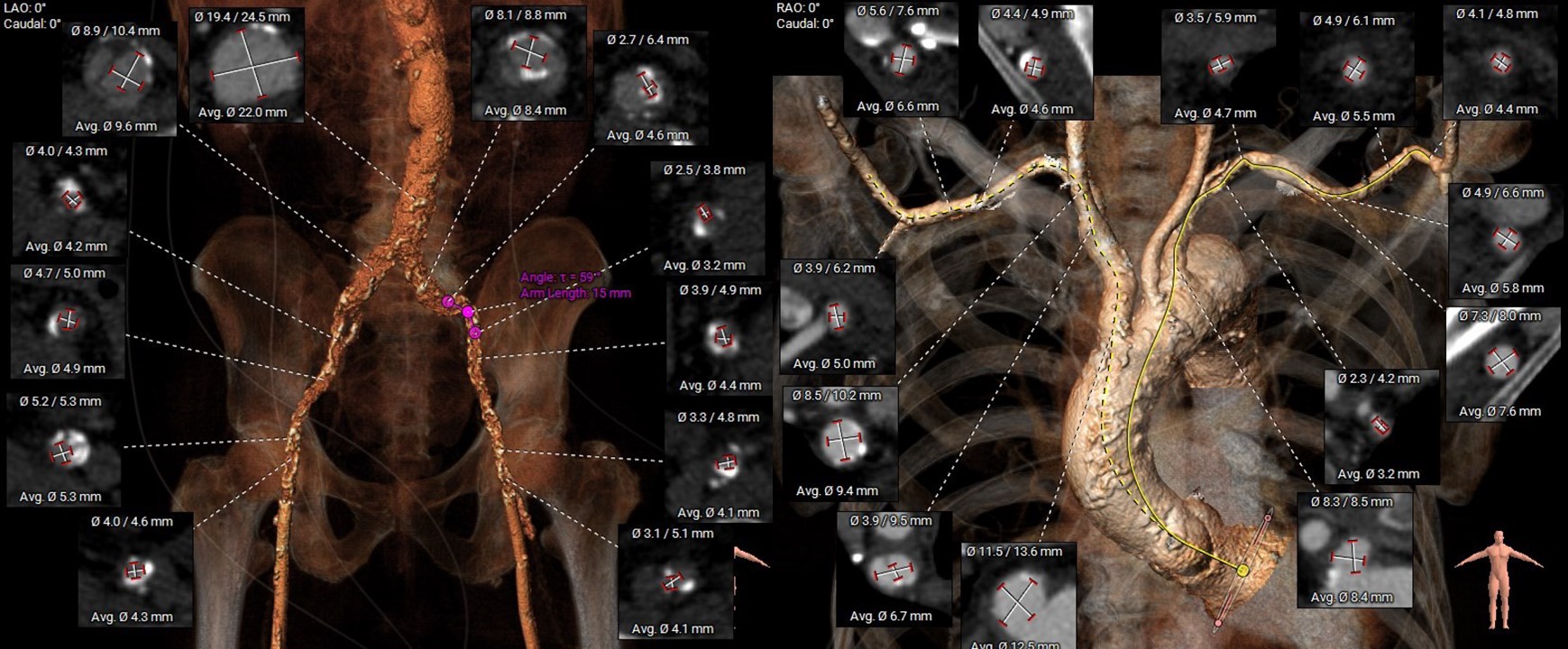
However, multislice CT scan revealed severe stenosis and calcific change in bilateral femoral arteries, making the transfemoral arterial approach unfeasible. Alternative access sites, including bilateral carotid and axillary arteries, were also not feasible. Although there was severe calcification in the abdominal aorta, the transcaval approach targeting a calcium-free segment of the aorta at the L3 level represented barely the last resort for carrying out TAVI procedures.
Interventional Management
Procedural Step
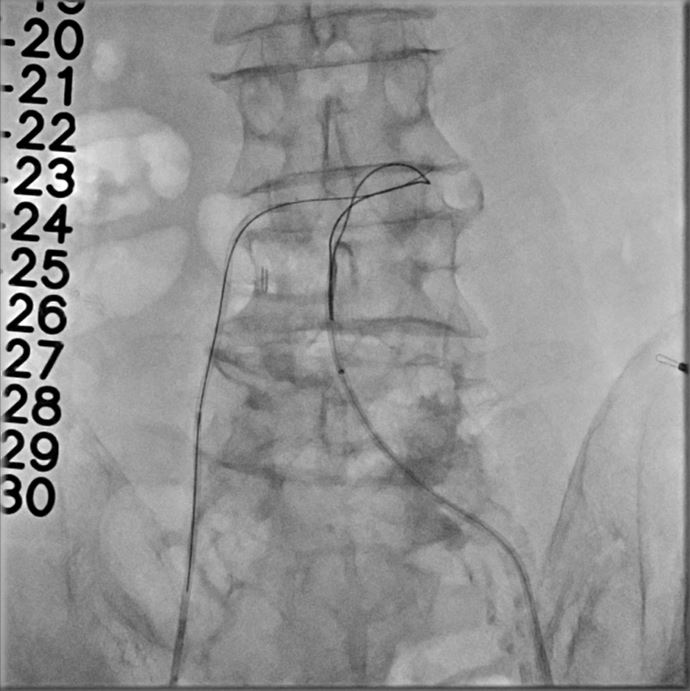
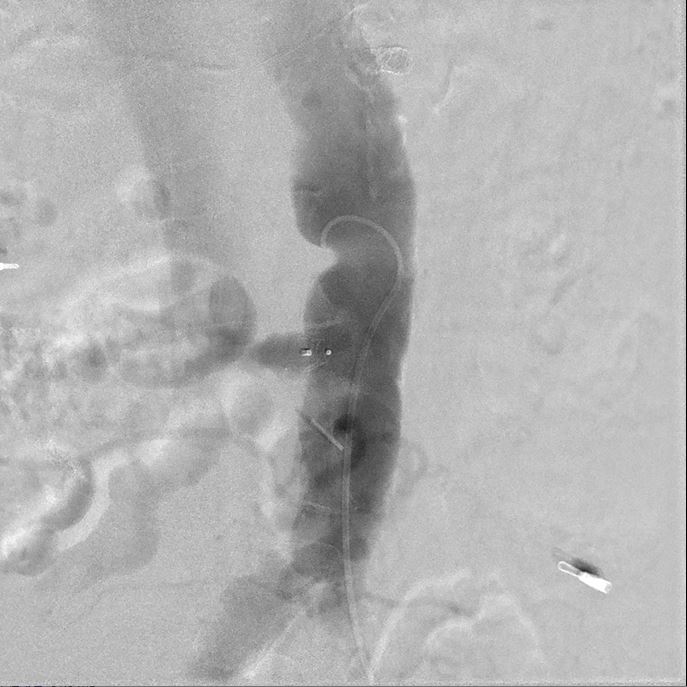
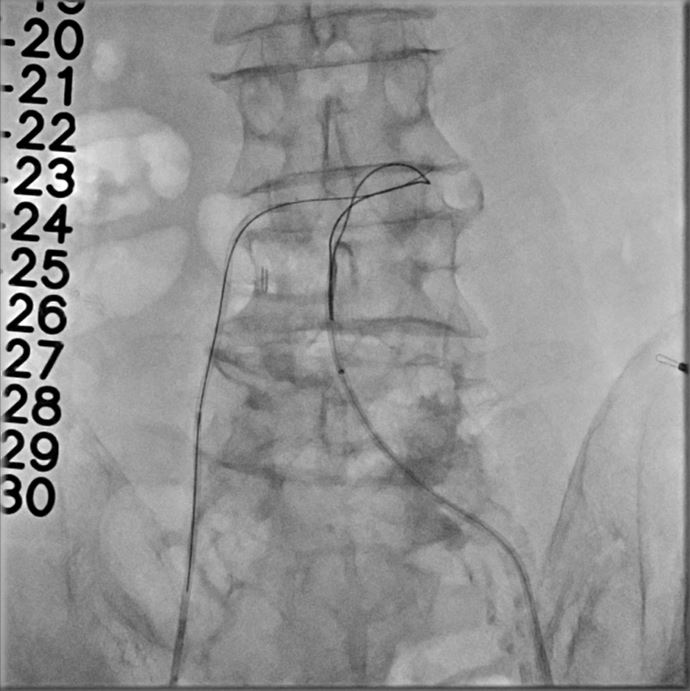
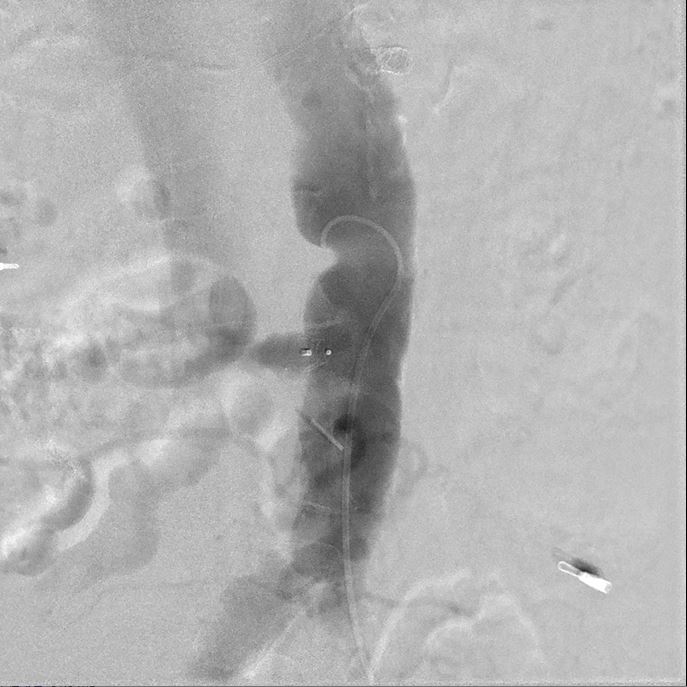
The transcaval approach starts with descending abdominal aortography. A 7-F renal double curve guide catheter which was advanced through the right femoral vein. An Astato wire along with a CXI microcatheter were advanced through the catheter to the indexed L3 level for transcaval puncture with the distal end of the Astato guidewire connecting with an electrosurgery pencil. After the Astato guidewire cross the vena cava and the adjacent aortic wall, the Asatato-CXI system was then captured by a 25 mm Gooseneck snare placed at the corresponding aortic level through left femoral atery, and sent upward to the thoracic aortic level. The Asatato wire was exchanged for a Lunderquist guidewire, through which an 20 French long sheath was advanced through RFV to the abdominal aorta. Standard TAVI procedures employing a Navitor 27 mm transcatheter heart valve were then performed through this vena-aortic connection facilitated by LV on-wire pacing. At the end of the procedure, an Amplatzer Duct Occluder was deployed to close the aorto-caval tract, with post-procedural angiography confirming a patent fistula with cruciform contrast flow around the neck of the occluder but with contrast returning to the cava. After careful examination, there was no extravasation on the digital subtraction angiogram. The next day, a follow-up angiogram of the aorto-caval fistula was performed, which revealed a patent fistula but without extravasation. The patient is doing well during one year of follow-up.