Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-188
Drug Coated Balloon Only iFR, uFR and IVUS Guided Complete Coronary Revascularization in High Bleeding and Contrast Induced Nephropathy Risk Patient With NSTEMI
By Farhat Fouladvand, Guido Belli, Mauro Musmeci
Presenter
Farhat Fouladvand
Authors
Farhat Fouladvand1, Guido Belli1, Mauro Musmeci1
Affiliation
Clinica Polispecialistica San Carlo, Italy1,
View Study Report
TCTAP C-188
Coronary - Imaging & Physiology - FFR
Drug Coated Balloon Only iFR, uFR and IVUS Guided Complete Coronary Revascularization in High Bleeding and Contrast Induced Nephropathy Risk Patient With NSTEMI
Farhat Fouladvand1, Guido Belli1, Mauro Musmeci1
Clinica Polispecialistica San Carlo, Italy1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 58 years male with following risk factors: diabetes, hypertension, dyslipidaemia (intolerance to any statin), heavy smoker (20 p/y), known for important anaemia due to thalassemia with several blood transfusions, severe renal insufficiency due to multifactorial causes and previous stroke was admitted in emergency room for rest chest pain for less than 4 hours. His physical exam findings at admittance were normal.
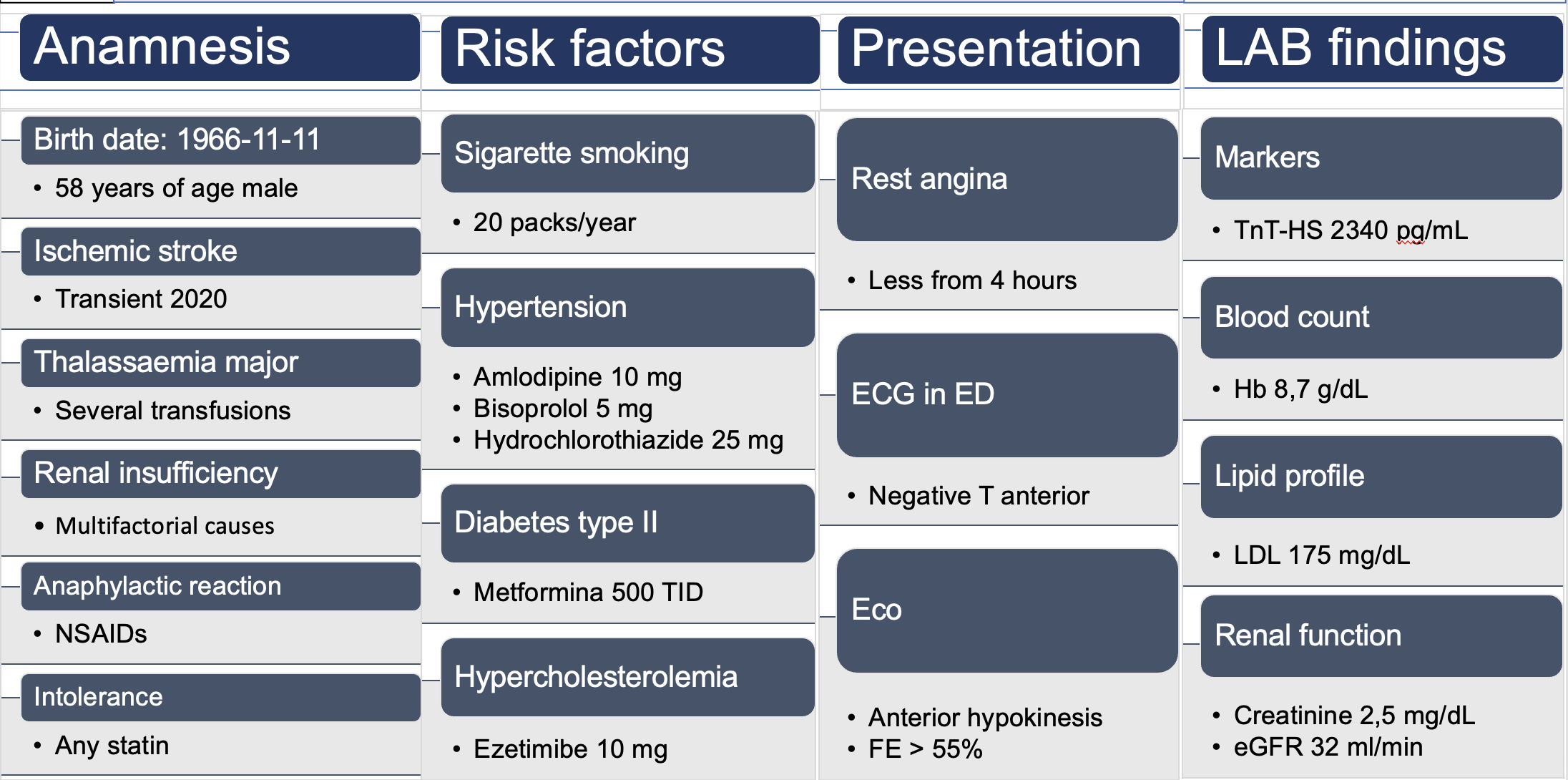
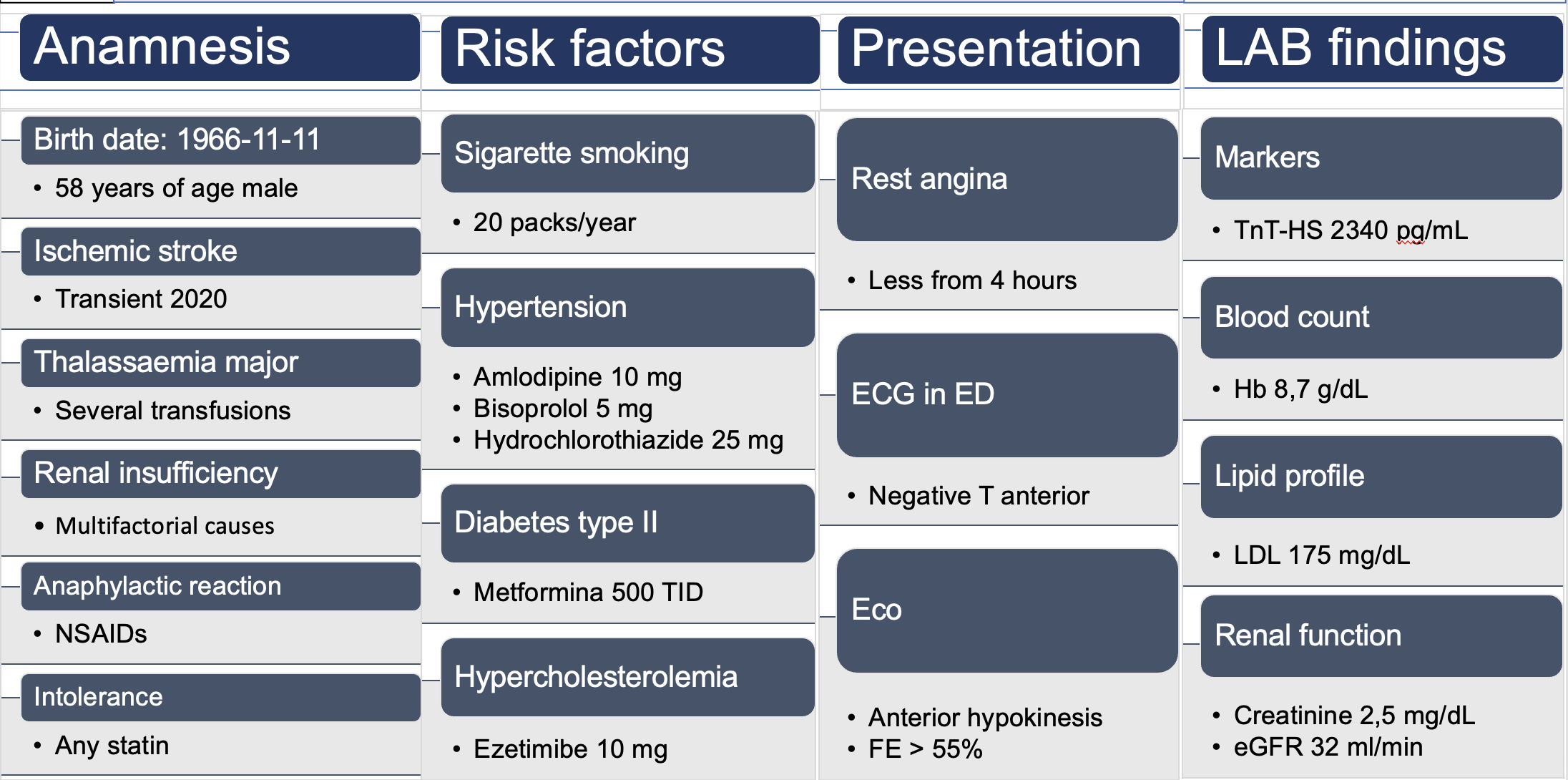
Relevant Test Results Prior to Catheterization
The ECG shows anterior negative T-waves, the echocardiogram indicates moderate hypokinesis of the anterior septum and lateral wall with FE> 55%. Lab tests reveal a 100-fold increase in TnI-HS (23400 pg/mL), anemia (Hb 8.7 g/L), stage 3b renal failure (eGFR 32 ml/min), and high LDL-cholesterol (175 mg/dL). Initial risk stratification categorizes the patient as high bleeding risk (CRUSADE and PRECISE-DAPT), and very high risk for contrast-induced nephropathy (Mehran and Chen).
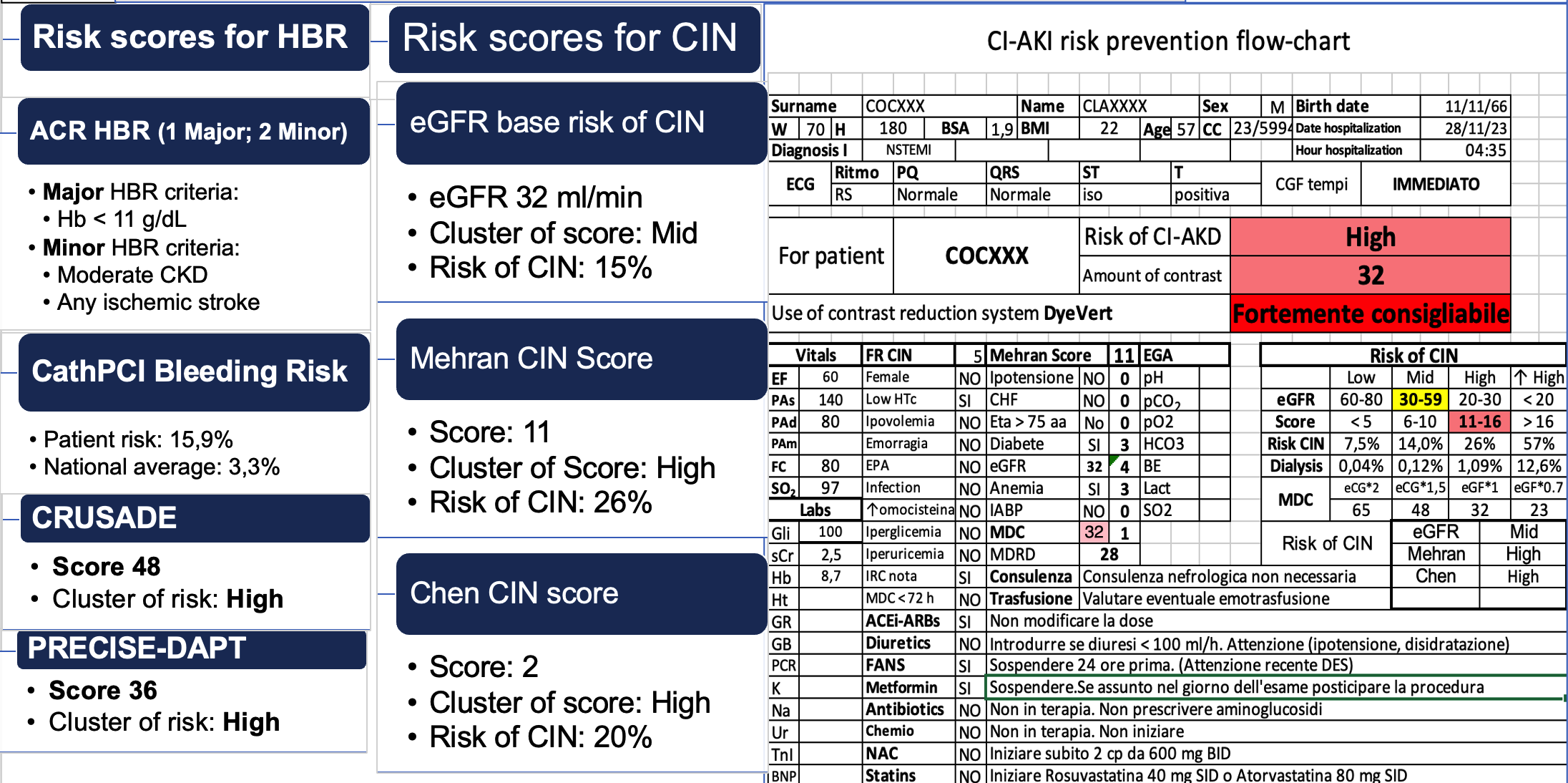
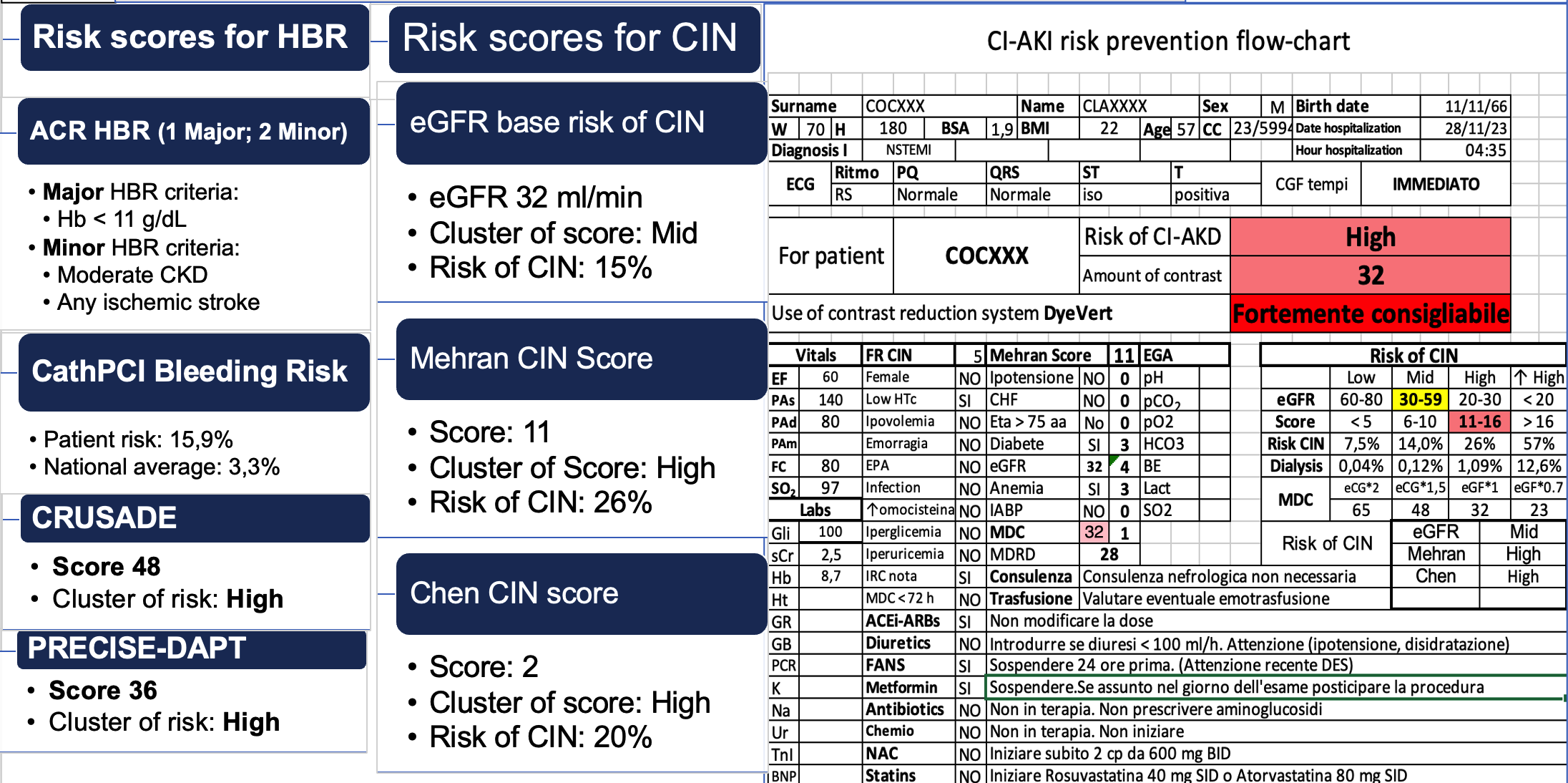
Relevant Catheterization Findings
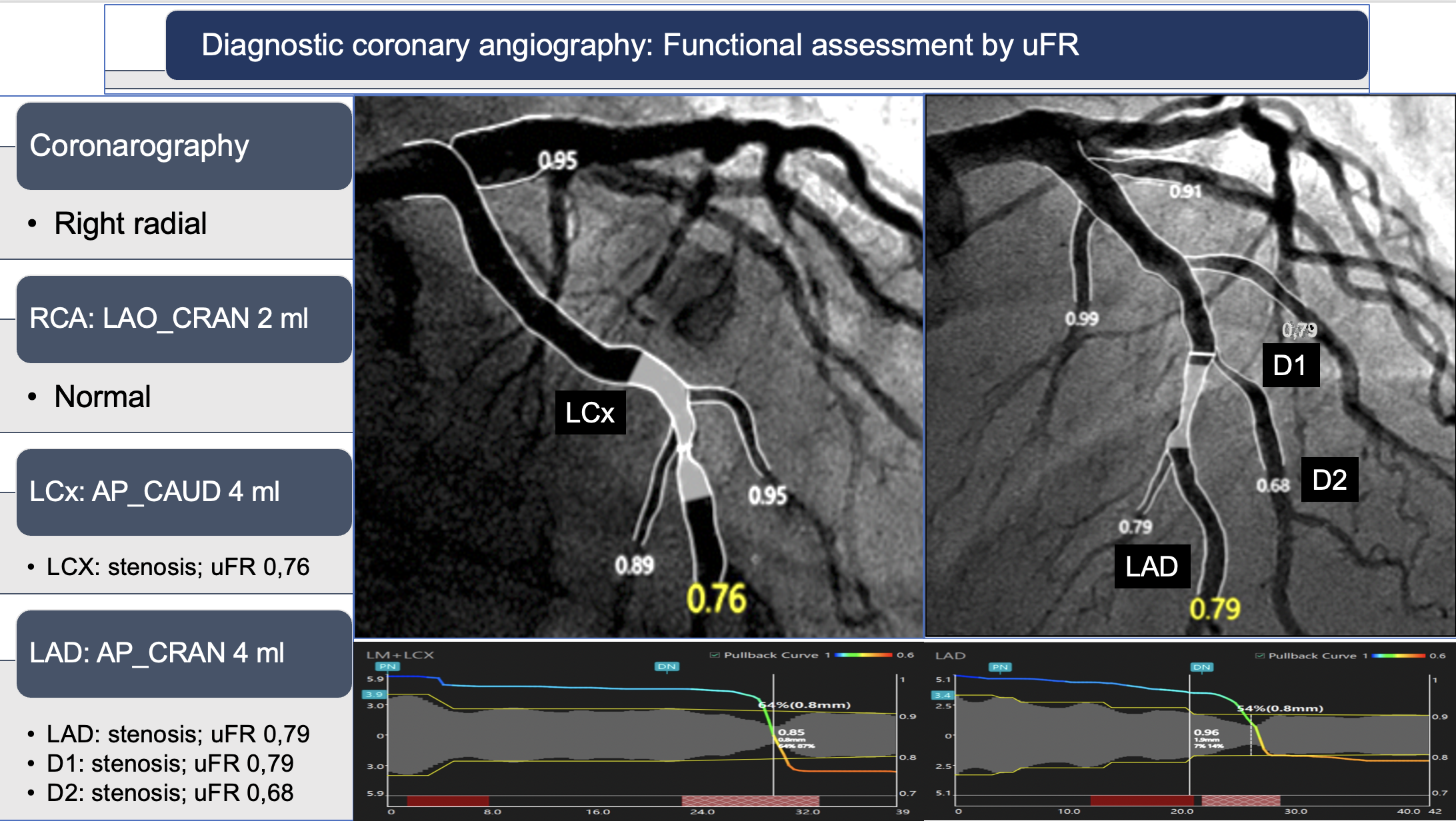
Due to the high risk of CIN, the pre-stabilized CD to be used was 32 ml. From the right radial artery, the right coronary artery was opacified with 2 ml of contrast and appeared normal. The left coronary artery was visualized in two projections, each with 4 ml of contrast (total 8 ml), revealing critical stenosis in the circumflex (CX uFR 0.76), left descending artery (LAD uFR 0.79), and first (D1 uFR 0.79) and second (D2 uFR 0.68) branches. Total contrast used was 10 ml.
Interventional Management
Procedural Step
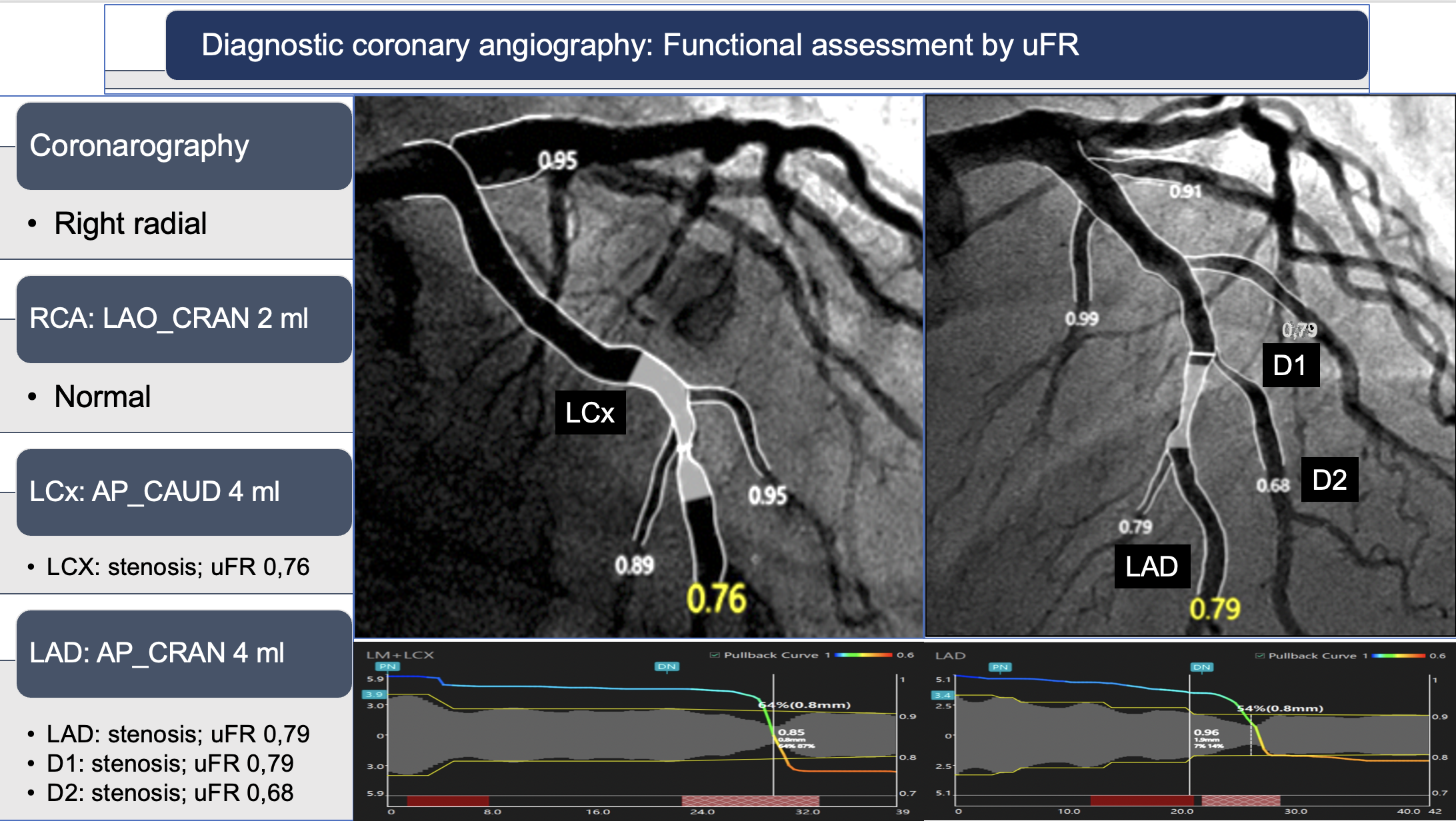
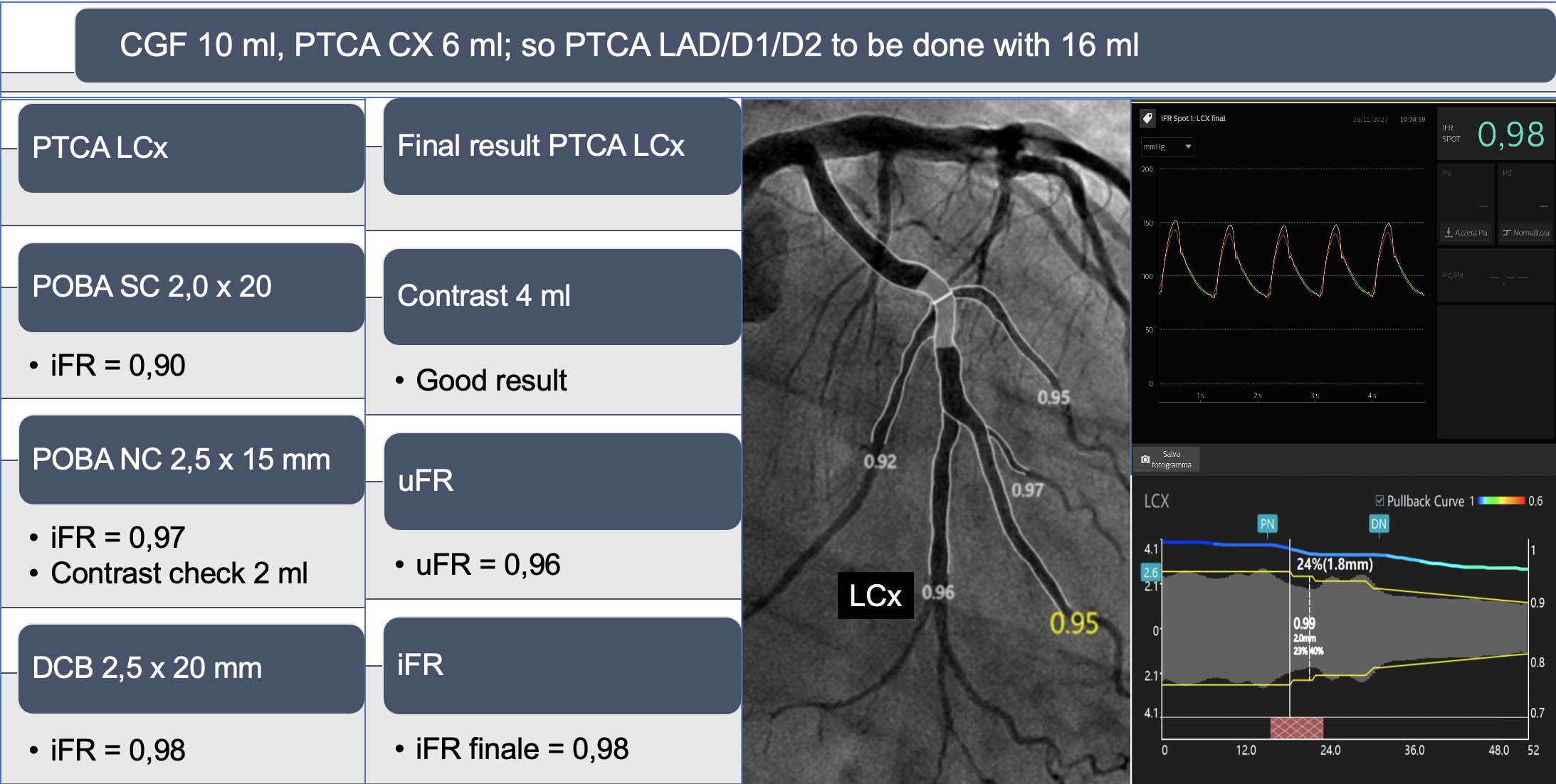
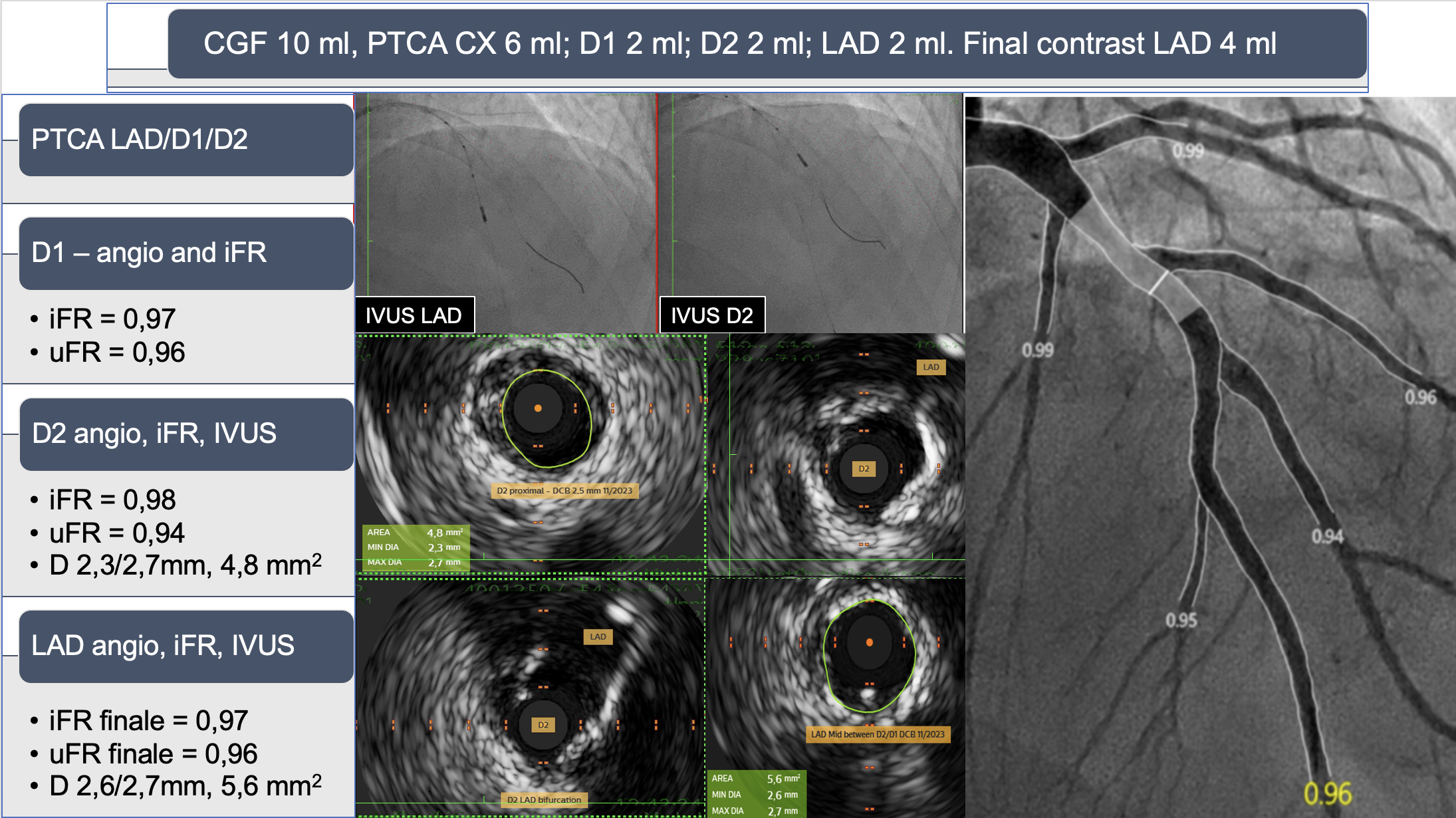
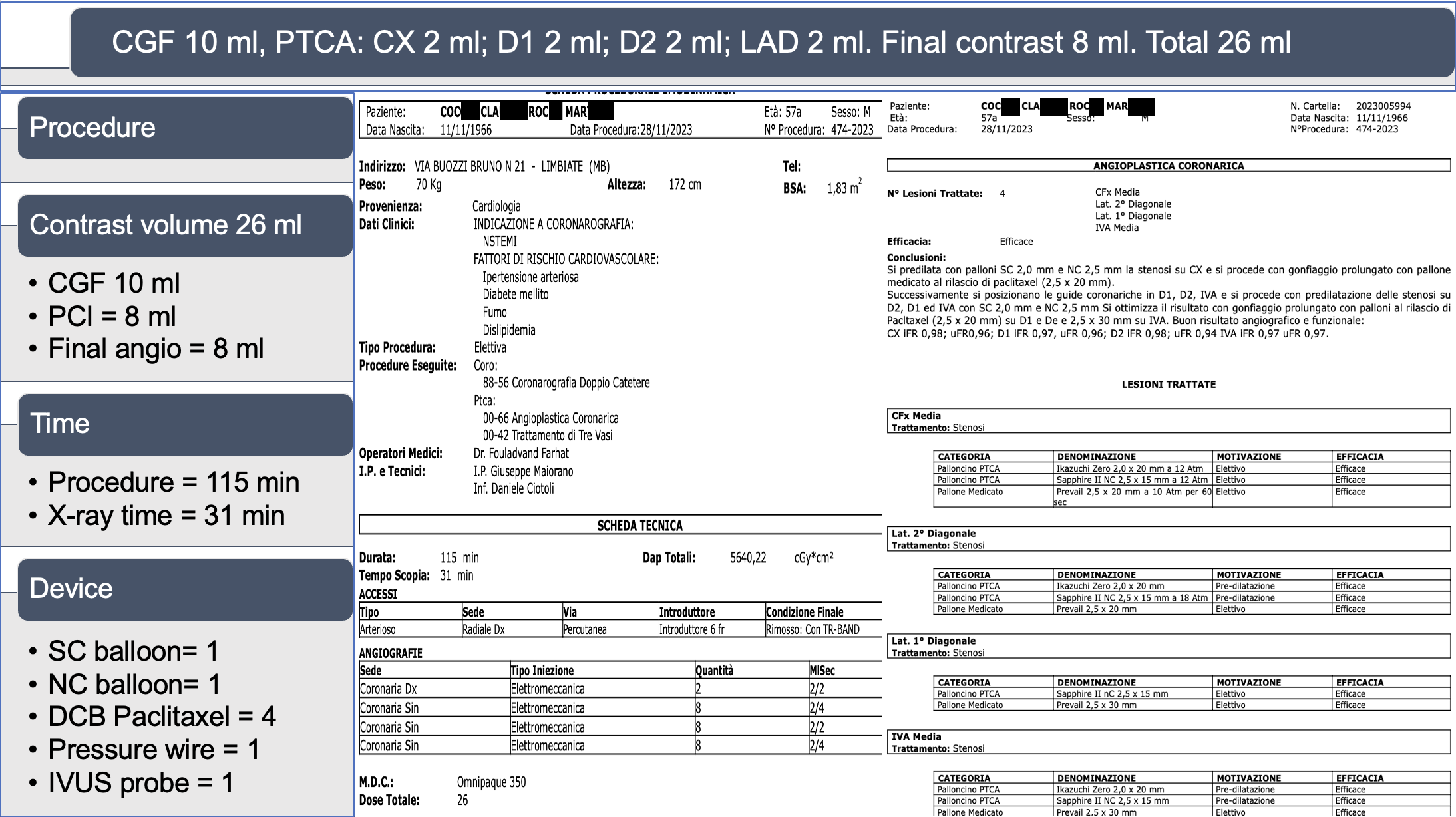
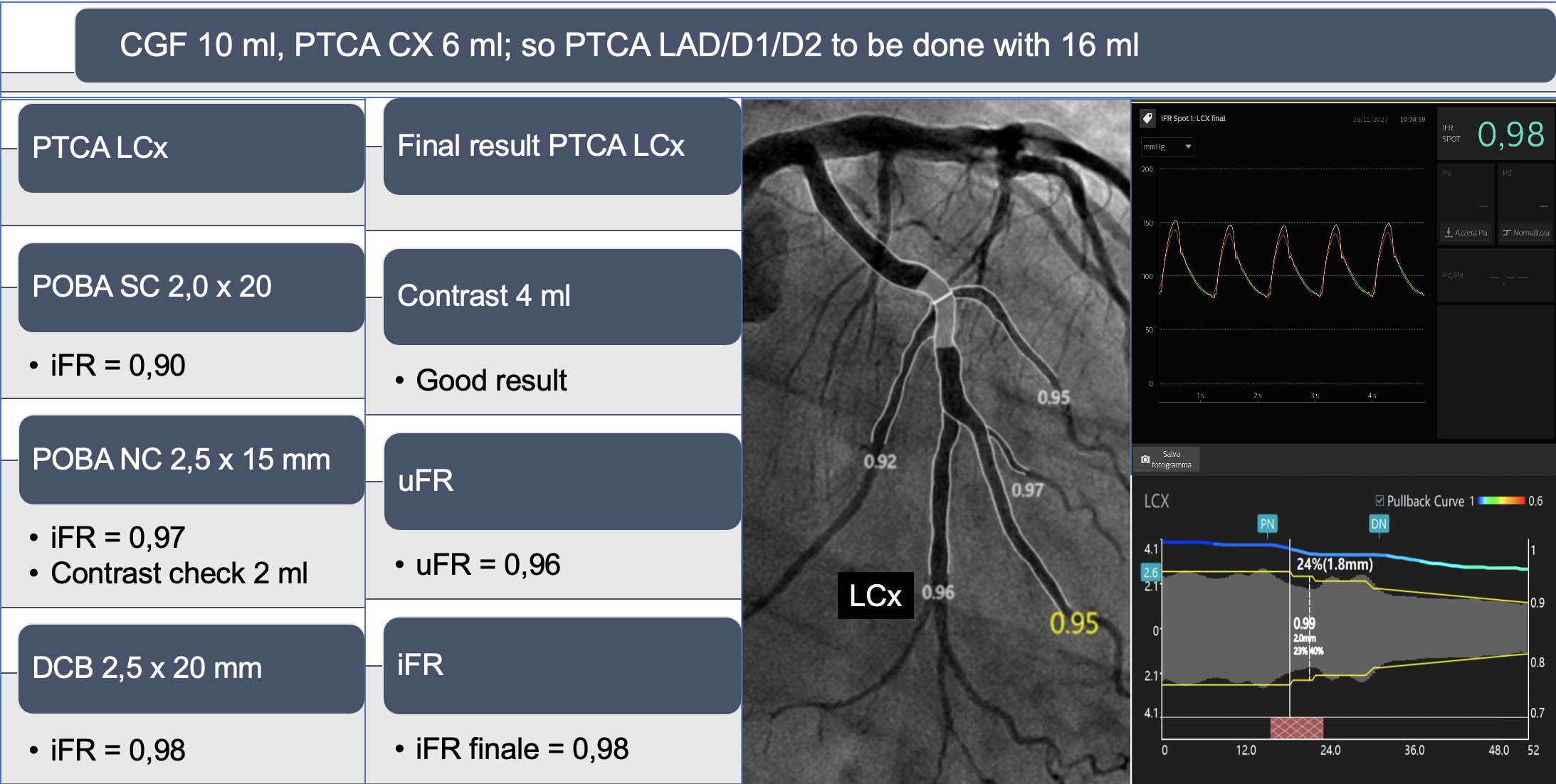
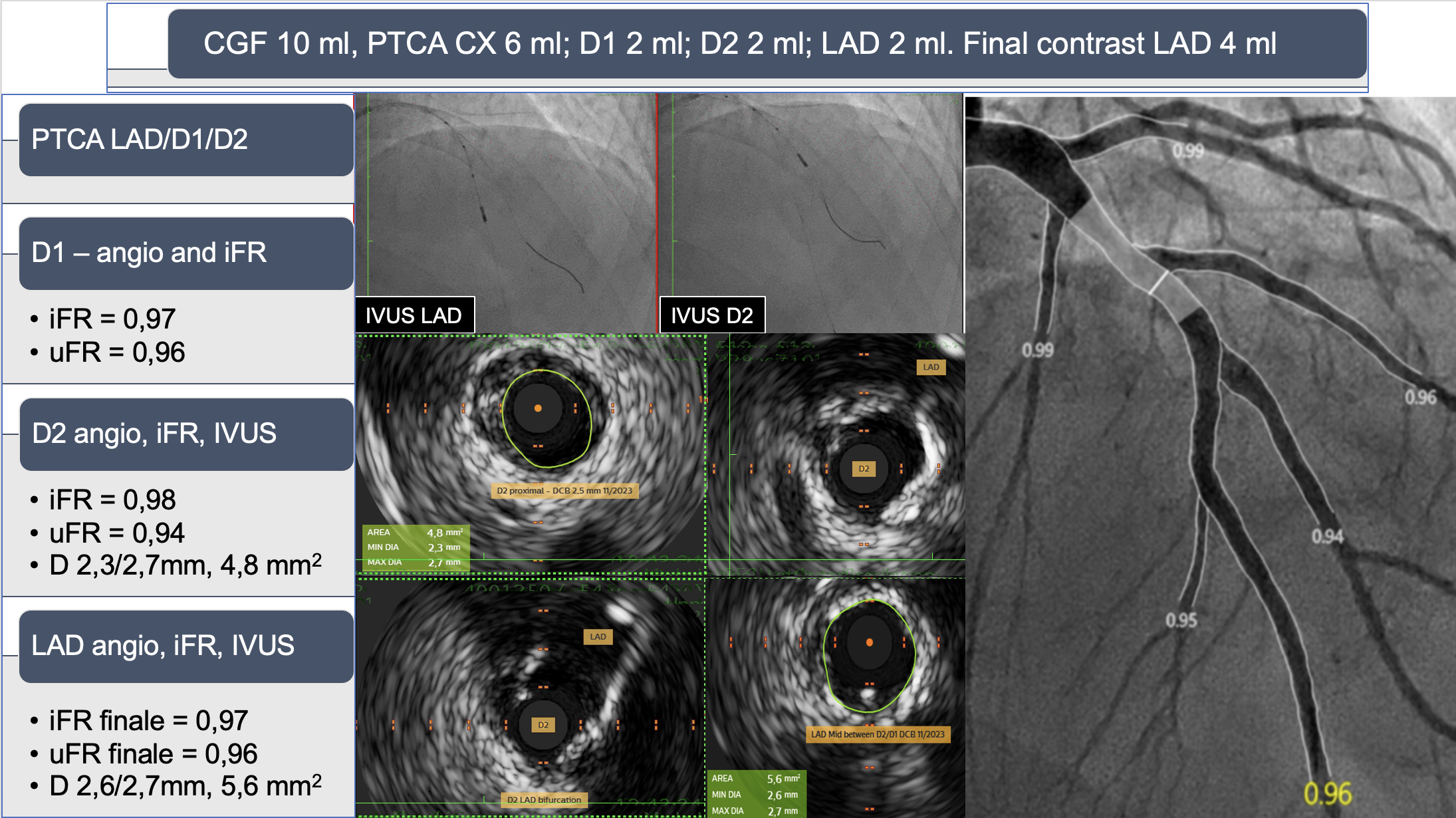
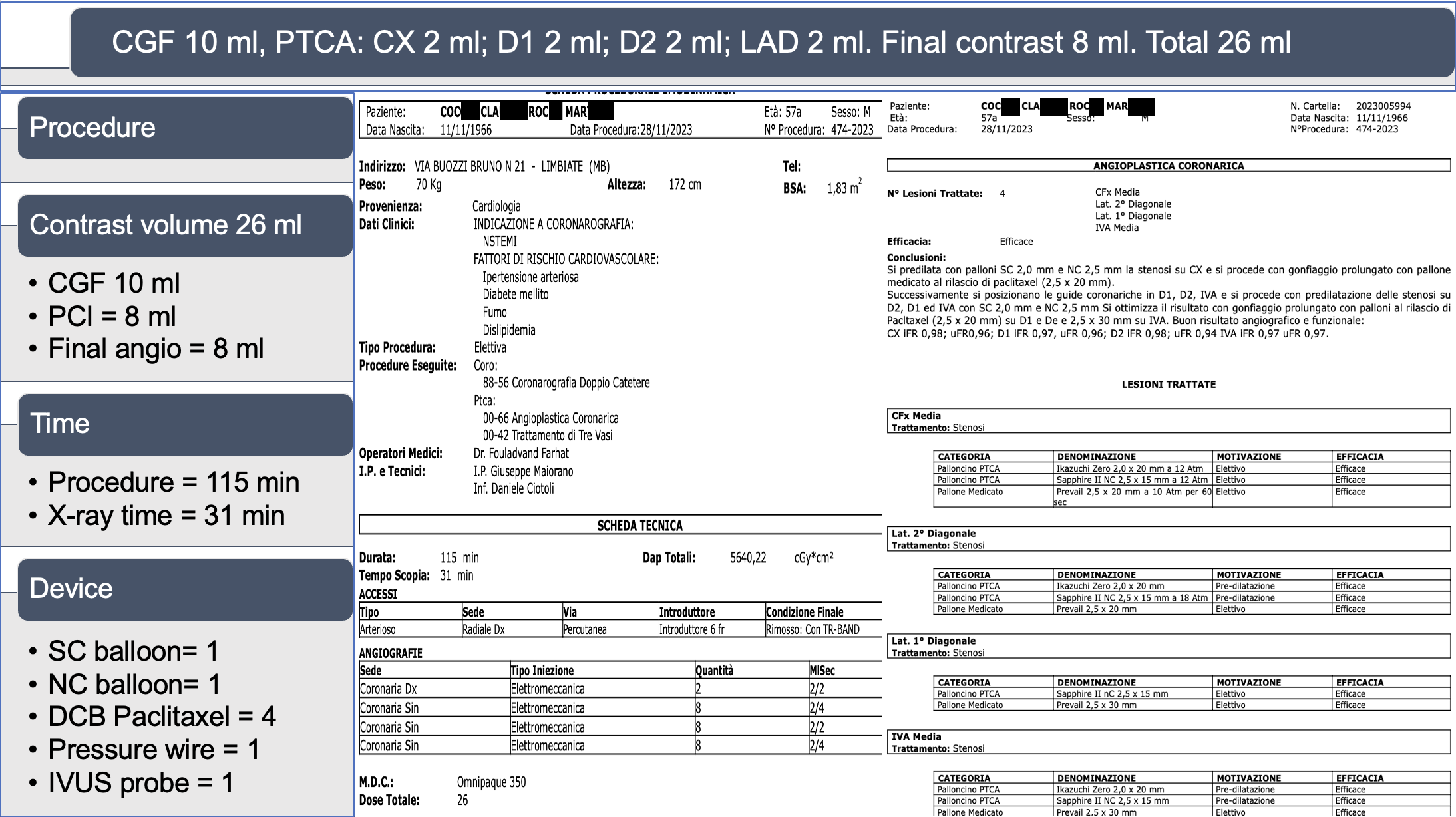
For the PTCA of all vessels (CX, LAD, D1, and D2), the permitted contrast was 22 ml (after 10 ml for coronarography). Due to high bleeding risk, we aimed to treat all vessels only with drug-coated balloons (DCB). To minimize contrast, we pre-dilated with balloons increasing in diameter up to a 1:1 ratio of artery diameter. Instead of using contrast for control, we measured iFR after any pre-dilatation. At achievement of a satisfactory iFR, we performed final dilatation with Paclitaxel DCB and repeat iFR measurement. If satisfactory, we moved to the next vessel without control angio, repeating the steps. Final angiography was performed in 2 projections using 4 ml of contrast for each projection; uFR was calculated for each vessel. The final functional assessment showed: CX uFR 0.96, iFR 0.98; D1 uFR 0.96, iFR 0.97; D2 uFR 0.92, iFR 0.98; LAD uFR 0.96, iFR 0.97. For the presence of a dissection at the ostial level of D2 we performed IVUS evaluation of D2 and LAD that revealed a good opening with diameters of 2.3/2.7 mm and area of 4.8 mm² for D2, and diameters of 2.6/2.7 mm and area of 4.8 mm² for LAD. The procedure utilized 3 coronary wires, 1 pressure wire, 1 semi-compliant balloon (2.0 x 20 mm), 1 non-compliant balloon (2.5 x 15 mm), 1 IVUS catheter, and 4 Paclitaxel DCBs. Amount of all used contrast for diagnostic angiography (10 ml) and (PCI 16 ml) was 26 ml. Discharge eGFR was 40 ml/min and medicine where Clopidogrel, beta-blocker, ace-inhibitor, antidiabetics and PCSK9.
Case Summary
Prior risk stratification for risks of bleeding and contrast induced nephropathy and establishing the strategies to reduce the amount of contrast used and the need of double antiaggregation therapy is of a crucial importance for every patient entering in the cath lab.


