Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-041
Armor Piercing: Approaching an Impenetrable Lesion
By Kay Powpuree, Makha Vipanurat, Viroon Likitlertlum
Presenter
Kay Powpuree
Authors
Kay Powpuree1, Makha Vipanurat1, Viroon Likitlertlum1
Affiliation
Rajavithi Hospital, Thailand1,
View Study Report
TCTAP C-041
Coronary - Adjunctive Procedures (Thrombectomy, Atherectomy, Special Balloons)
Armor Piercing: Approaching an Impenetrable Lesion
Kay Powpuree1, Makha Vipanurat1, Viroon Likitlertlum1
Rajavithi Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
77-year-old femaleunderlying diease : Hypertension, Dyslipidemia, Chronic kidney disease, CHB on PPM (DDDR)
Presenting : Chest discomfort and orthopnea 2 days prior to hospital admission
Physical examination BP 130/80 mmHg. HR 70 bpm, SpO2 90% (Room air)Pulse : regular, normokinetic pulse both extremitiesHeart : Pansystolic murmur at apex with S3 gallopLung : tachypnea with fine crepition both lower lung field
Presenting : Chest discomfort and orthopnea 2 days prior to hospital admission
Physical examination BP 130/80 mmHg. HR 70 bpm, SpO2 90% (Room air)Pulse : regular, normokinetic pulse both extremitiesHeart : Pansystolic murmur at apex with S3 gallopLung : tachypnea with fine crepition both lower lung field
Relevant Test Results Prior to Catheterization
Lab investigationTroponin I 2401 ng/LBun 35 mg/dl, Creatinine 1.7 mg/dl, Hb 11.5 g/dl, Hct 34 %, platelet count 180,000 /µL
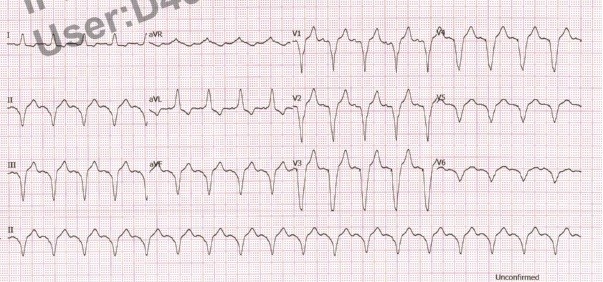
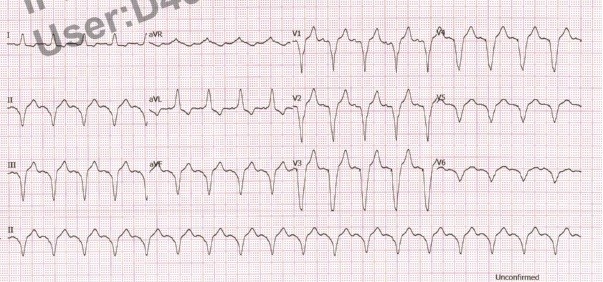
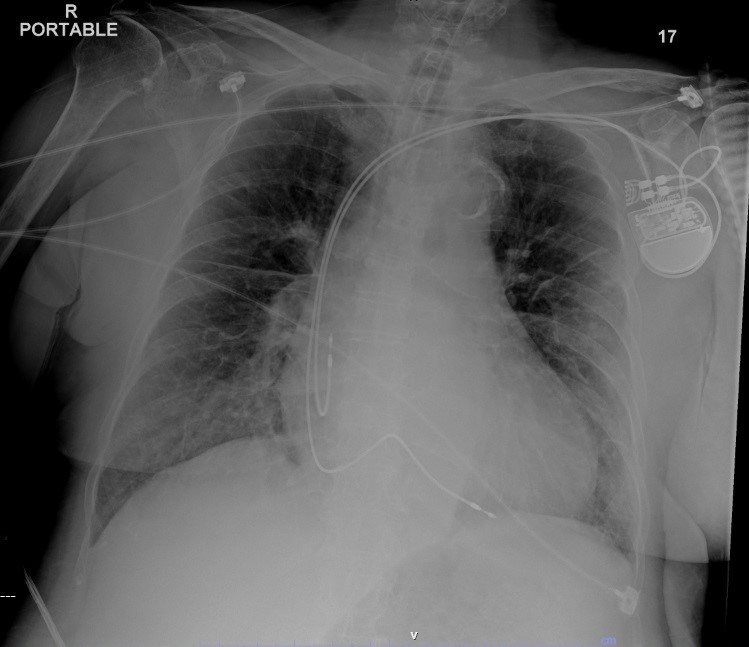
EKG : A sens, V pace rate 70 bpmCXR : cardiomegaly, peri-hilar congesion
Echocardiogram show : Moderately impaired LV systolic function, LV diastolic dysfunction, Global wall hypokinesia with marked hypokinesia at anterior, from mid to apical regions
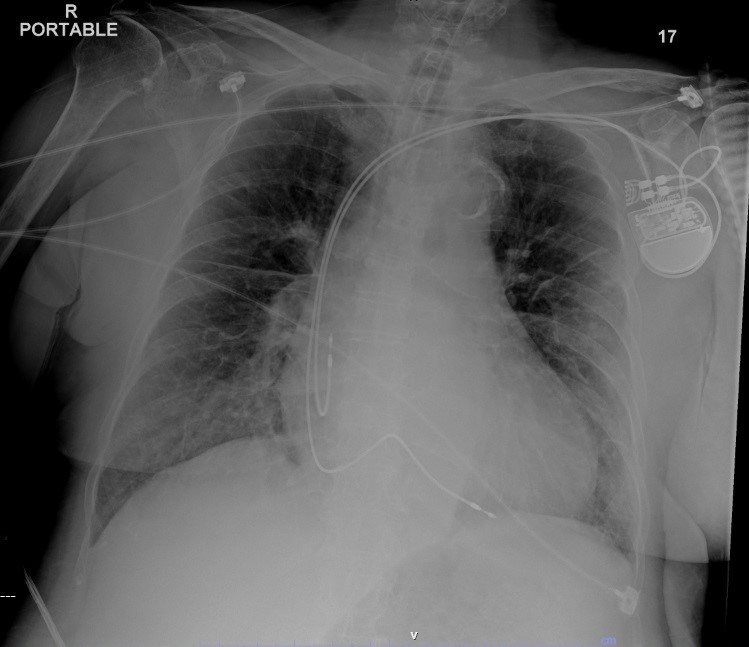
EKG : A sens, V pace rate 70 bpmCXR : cardiomegaly, peri-hilar congesion
Echocardiogram show : Moderately impaired LV systolic function, LV diastolic dysfunction, Global wall hypokinesia with marked hypokinesia at anterior, from mid to apical regions
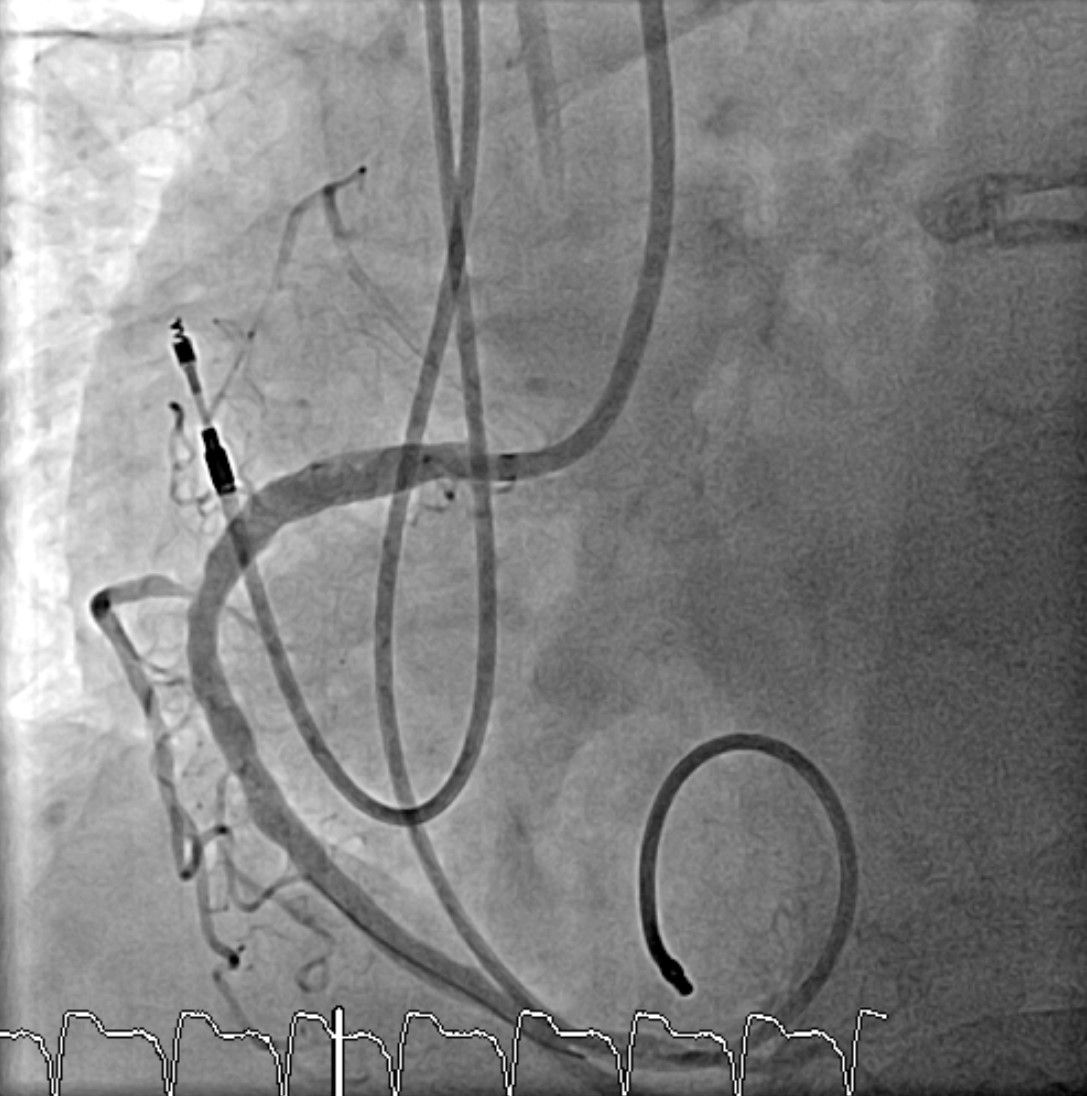
Relevant Catheterization Findings
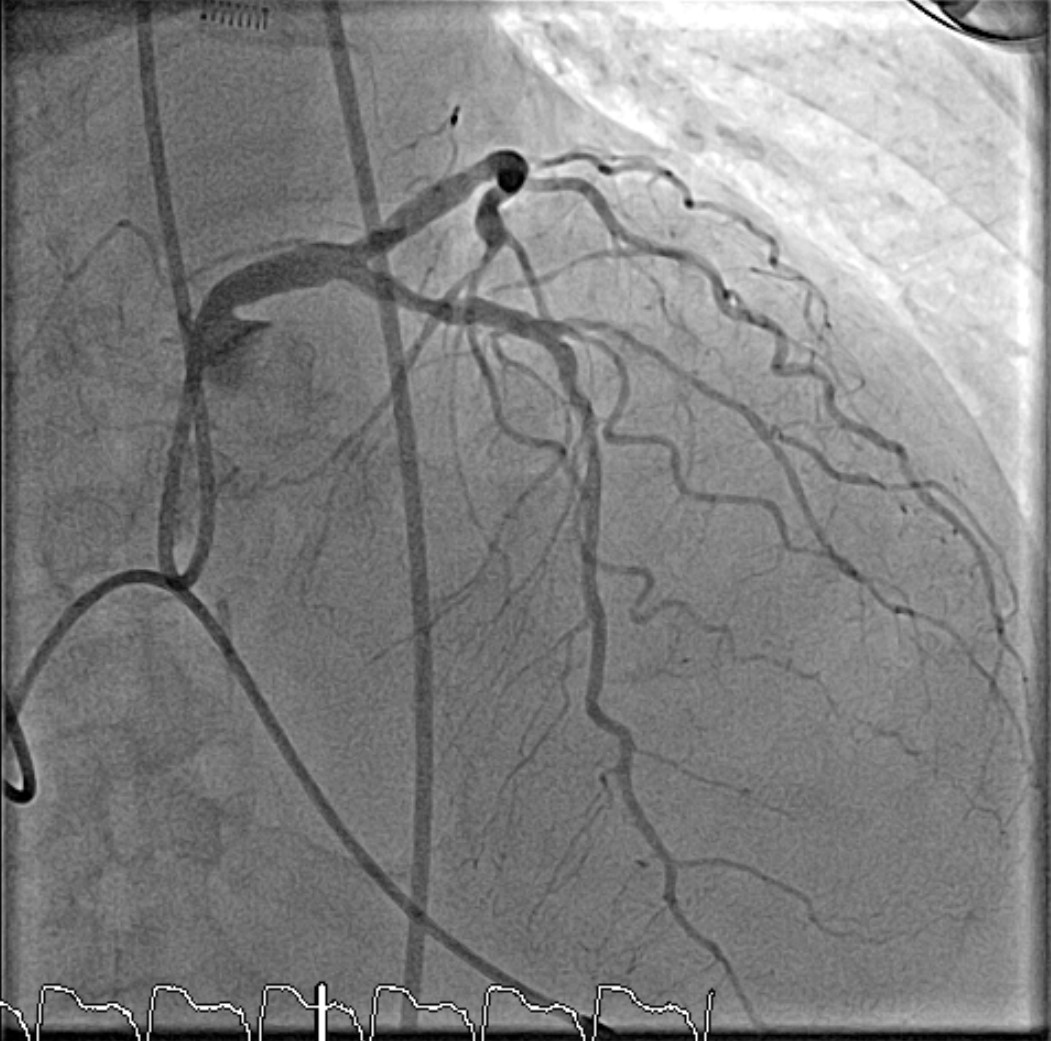
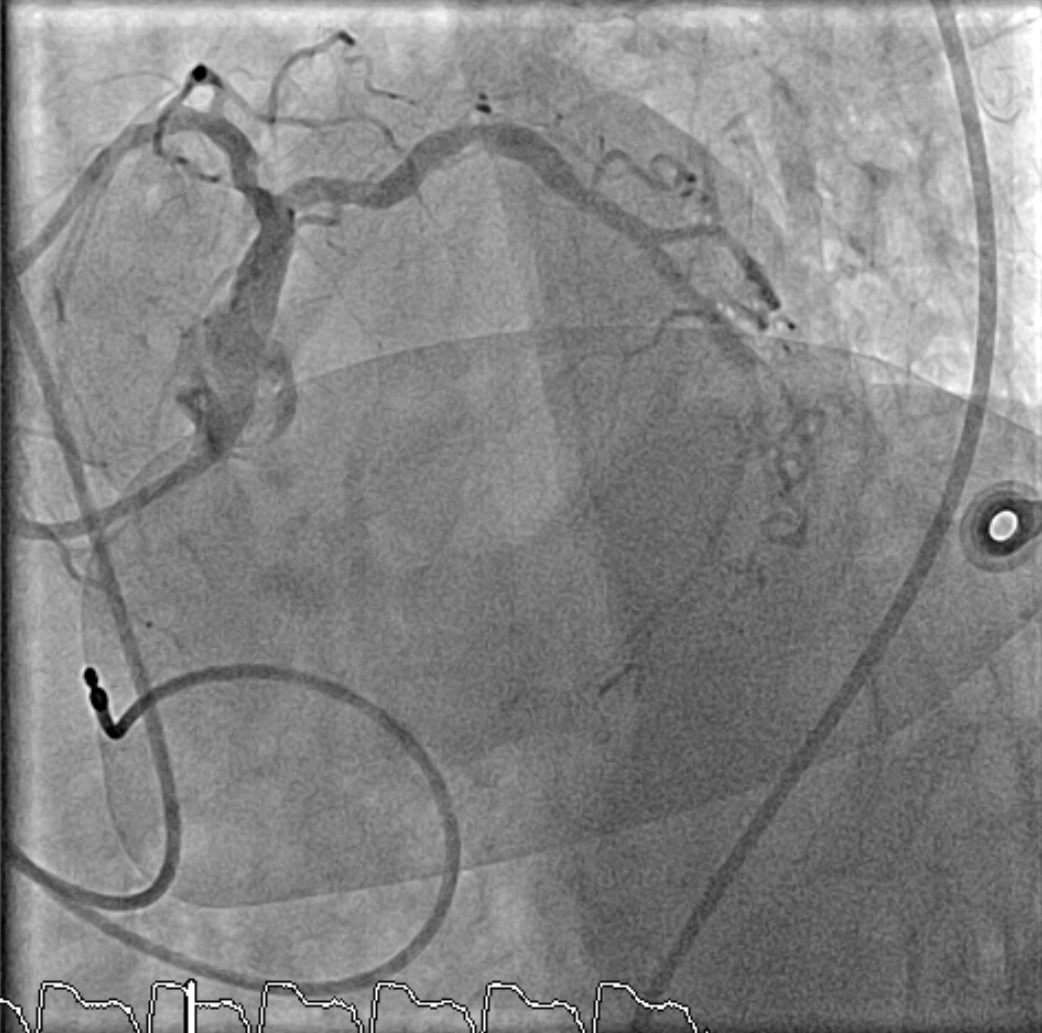
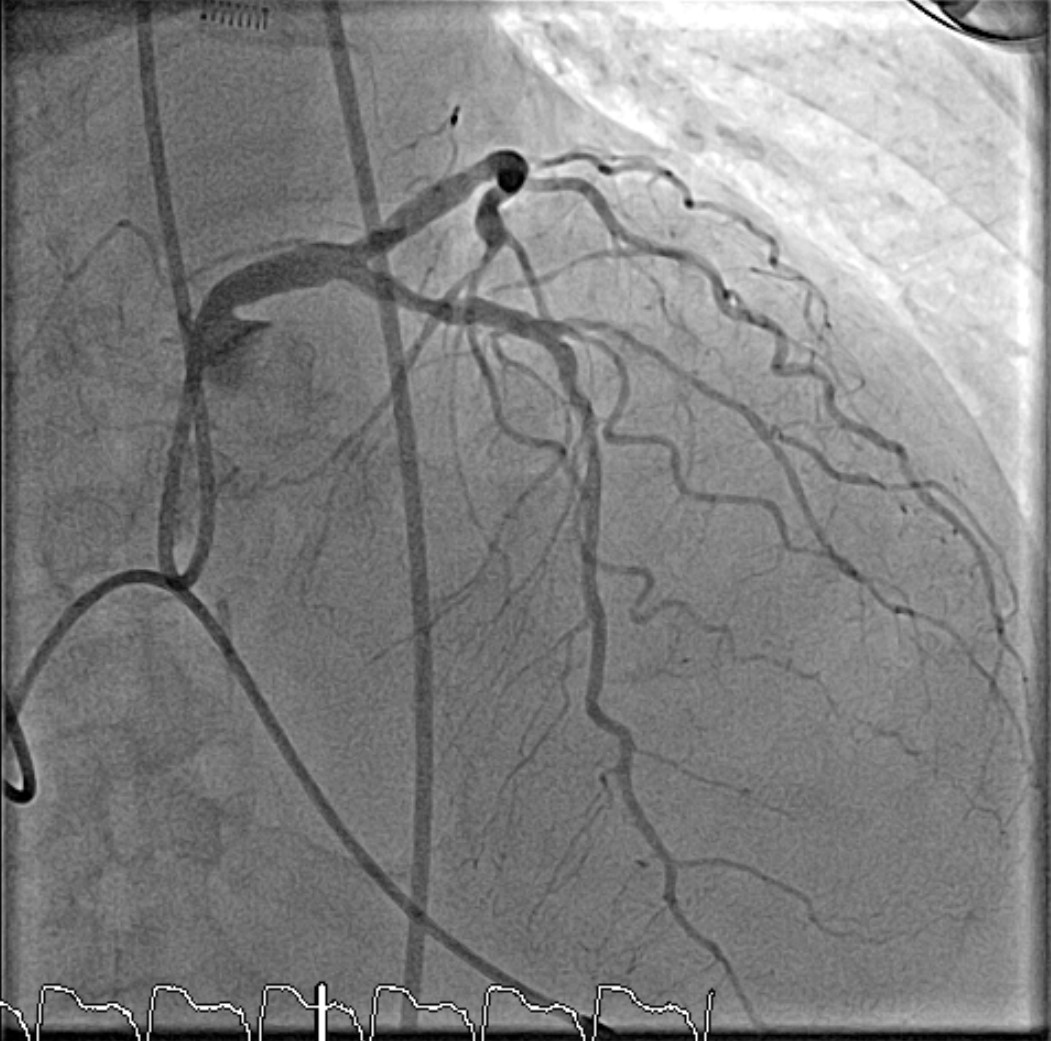
Right dominantLM : Heavy calcified LAD : Heavy calcified, 50% stenosis at proximal LAD, 80% stenosis mid LAD (TIMI flow III)Lcx: Heavy calcified, 70% stenosis proximal Lcx with large calcium noduleRCA : Heavy calcified, 85 % stenosis at proximal RCA with eccentric calcified nodule at proximal RCA


Interventional Management
Procedural Step
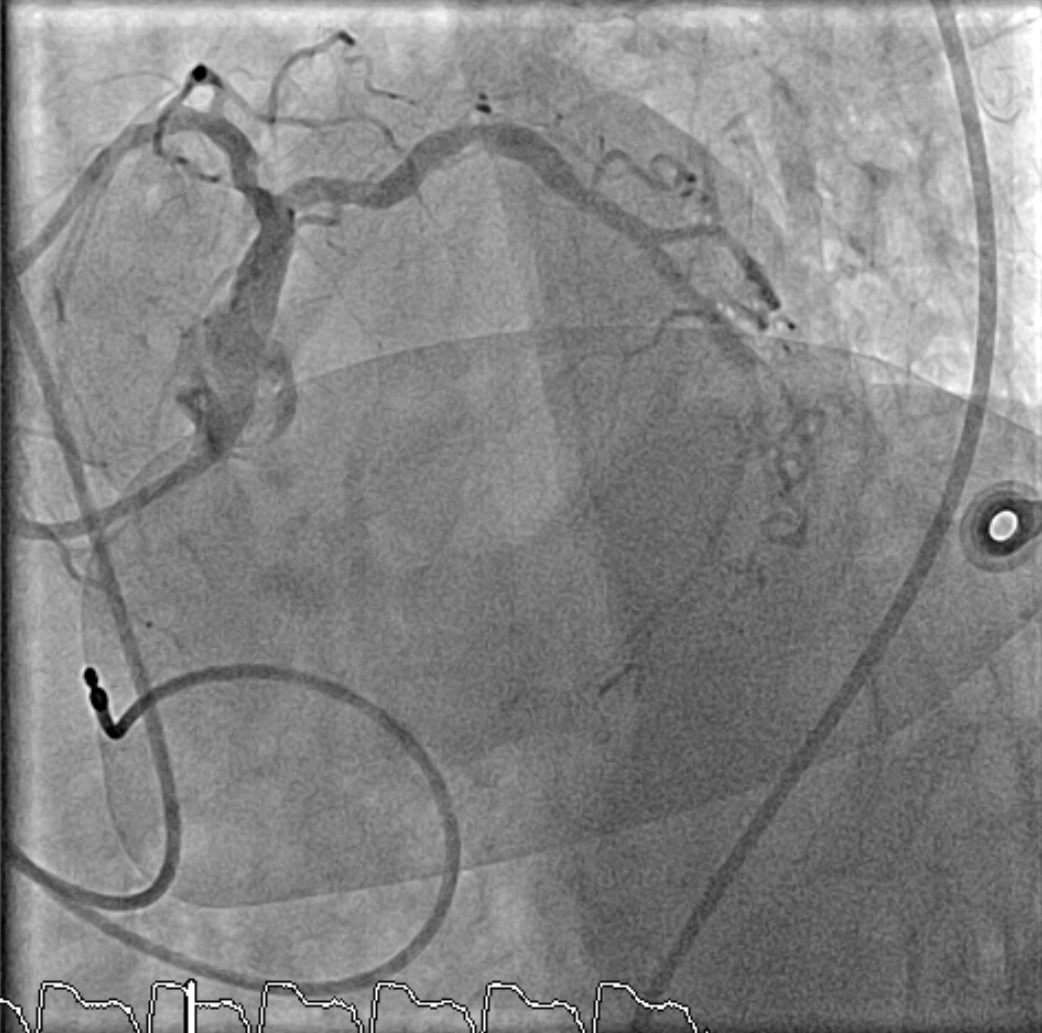
The RCA showed significant stenosis with a calcium nodule. The operator attempted to pre-dilate with a balloon and deployed a stent at the proximal RCA over the calcium nodule, but the stent could not fully expand. After multiple attempts to expand it with a non-compliant balloon, the NC balloon ruptured under high pressure and became trapped in the lesion. The operator safely removed it by manual traction. The procedure was halted, and a re-CAG was planned for 4 days later.
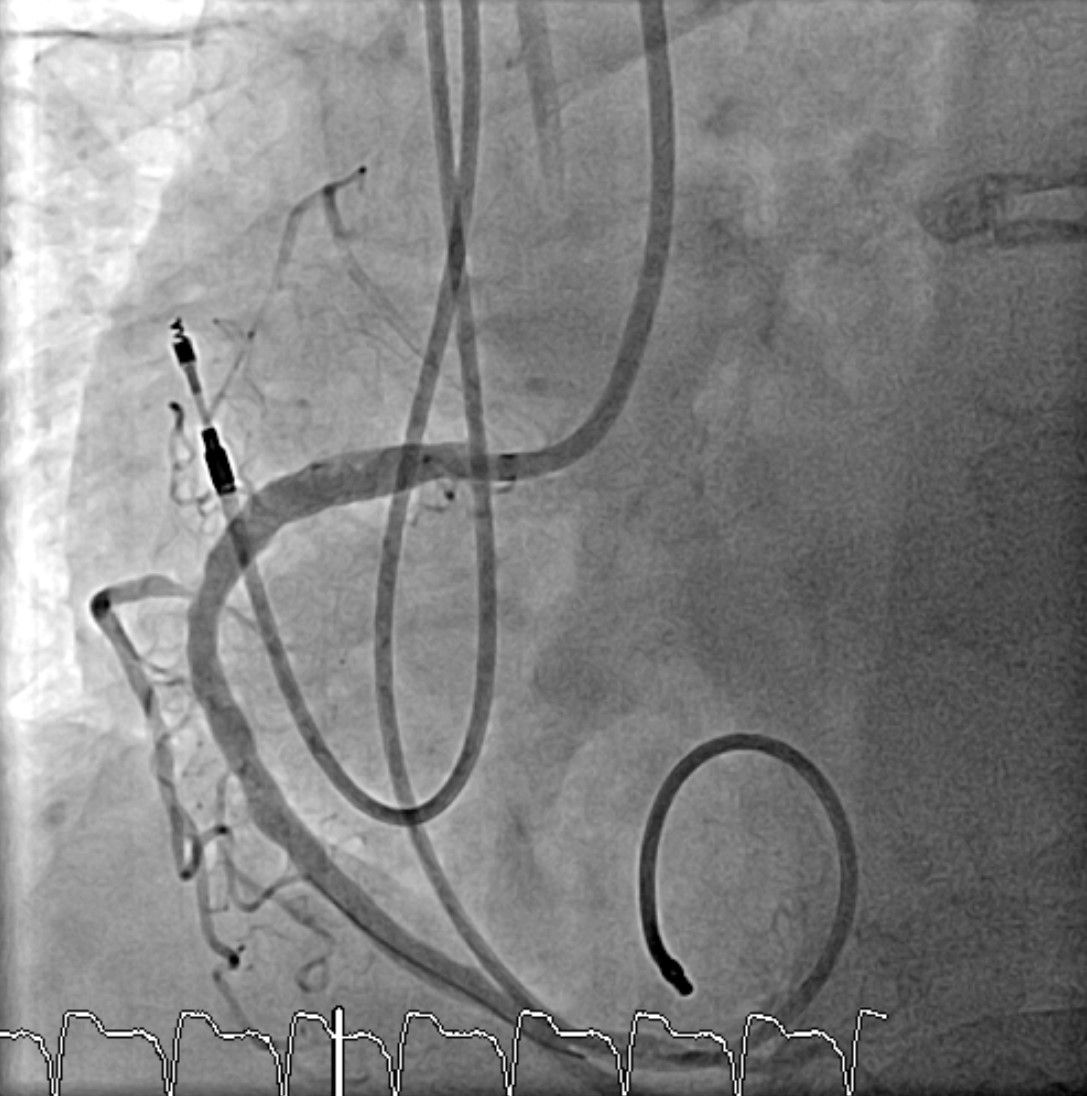
During the second attempt, the operator perform rotational atherectomy with stent placement at the proximal RCA. The operator used a Rota 1.75 burr at 180,000-200,000 RPM for 8 runs and then upsized to a 2.0 burr at 180,000-190,000 RPM for another 8 runs, but the rota burr could not pass the calcium nodule. Attempts to pass a microcatheter were unsuccessful asit got stuck at the lesion. The operator then used a second wire as a buddywire, but even microcatheters such as Finecross and Corsair Pro could not pass. The operator used a 1.25 Rota burr to debulk the calcium over the rota wire at 190,000-200,000 RPM for 10 runs, but the rota still could not pass the calcium nodule. However, the stent at the lesion was already ablated. A small 1.0 balloon was successfully passed and pre-dilated, followed by a 2.0 balloon. IVUS wasused to check vessel size, and pre-dilation was done with an NC 3.5 balloon. A DES 4.5 x 12 mm was deployed, Post dilate with NC 4.0x15 mm. IVUS show good stent apposition and expansion.


During the second attempt, the operator perform rotational atherectomy with stent placement at the proximal RCA. The operator used a Rota 1.75 burr at 180,000-200,000 RPM for 8 runs and then upsized to a 2.0 burr at 180,000-190,000 RPM for another 8 runs, but the rota burr could not pass the calcium nodule. Attempts to pass a microcatheter were unsuccessful asit got stuck at the lesion. The operator then used a second wire as a buddywire, but even microcatheters such as Finecross and Corsair Pro could not pass. The operator used a 1.25 Rota burr to debulk the calcium over the rota wire at 190,000-200,000 RPM for 10 runs, but the rota still could not pass the calcium nodule. However, the stent at the lesion was already ablated. A small 1.0 balloon was successfully passed and pre-dilated, followed by a 2.0 balloon. IVUS wasused to check vessel size, and pre-dilation was done with an NC 3.5 balloon. A DES 4.5 x 12 mm was deployed, Post dilate with NC 4.0x15 mm. IVUS show good stent apposition and expansion.


Case Summary
Calcium nodules present significant challenges in coronary intervention, particularly in achieving optimal stent deployment. Coronary imaging plays a crucial role in the pre-, peri-, and post-procedural management of calcified lesions, providing insights essential for procedural planning and outcome optimization. Suboptimal stent expansion over underexpanded lesions is strongly associated with TLF, highlighting the importance of lesion preparation. Techniques such as rotational atherectomy are valuable options for debulking calcium nodules prior to stent placement. Comprehensive imaging and lesion preparation strategies are essential in managing calcified lesion to improve patient outcome.


