Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-074
Navigate the Winding Path
By Yin Kei Jake Yeung
Presenter
Yin Kei Jake Yeung
Authors
Yin Kei Jake Yeung1
Affiliation
Queen Elizabeth Hospital, Hong Kong, China1,
View Study Report
TCTAP C-074
Coronary - Complex PCI - CTO
Navigate the Winding Path
Yin Kei Jake Yeung1
Queen Elizabeth Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 68-year-old gentleman, a chronic smoker, presented with intermittent exertional chest discomfort over the past six months. His medical history includes hypertension, hyperlipidemia, and a prior non-ST-elevation acute coronary syndrome (NSTE-ACS) in 2001. At that time, he declined coronary angiography and percutaneous coronary intervention (PCI), opting for medical management instead.
Relevant Test Results Prior to Catheterization
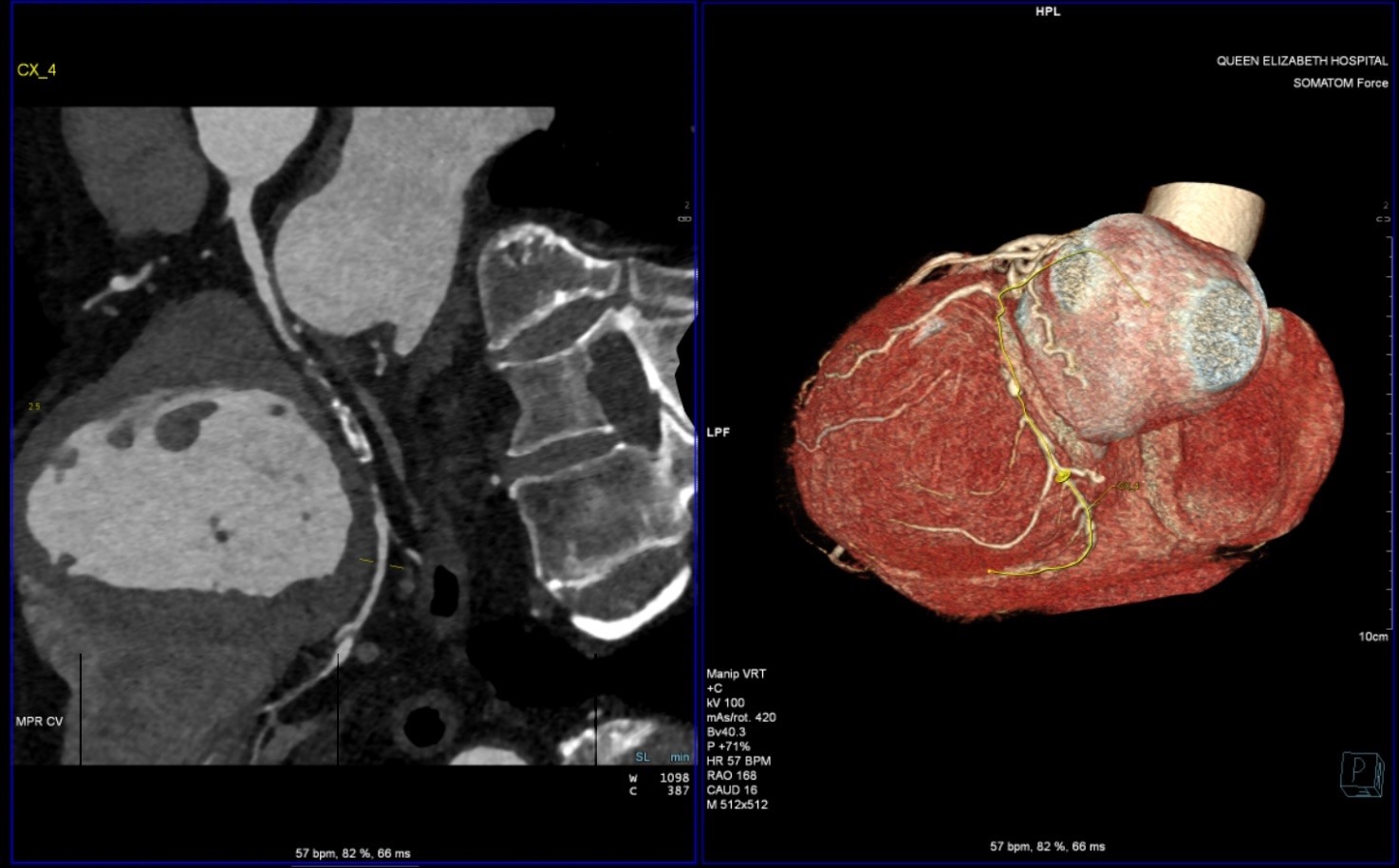
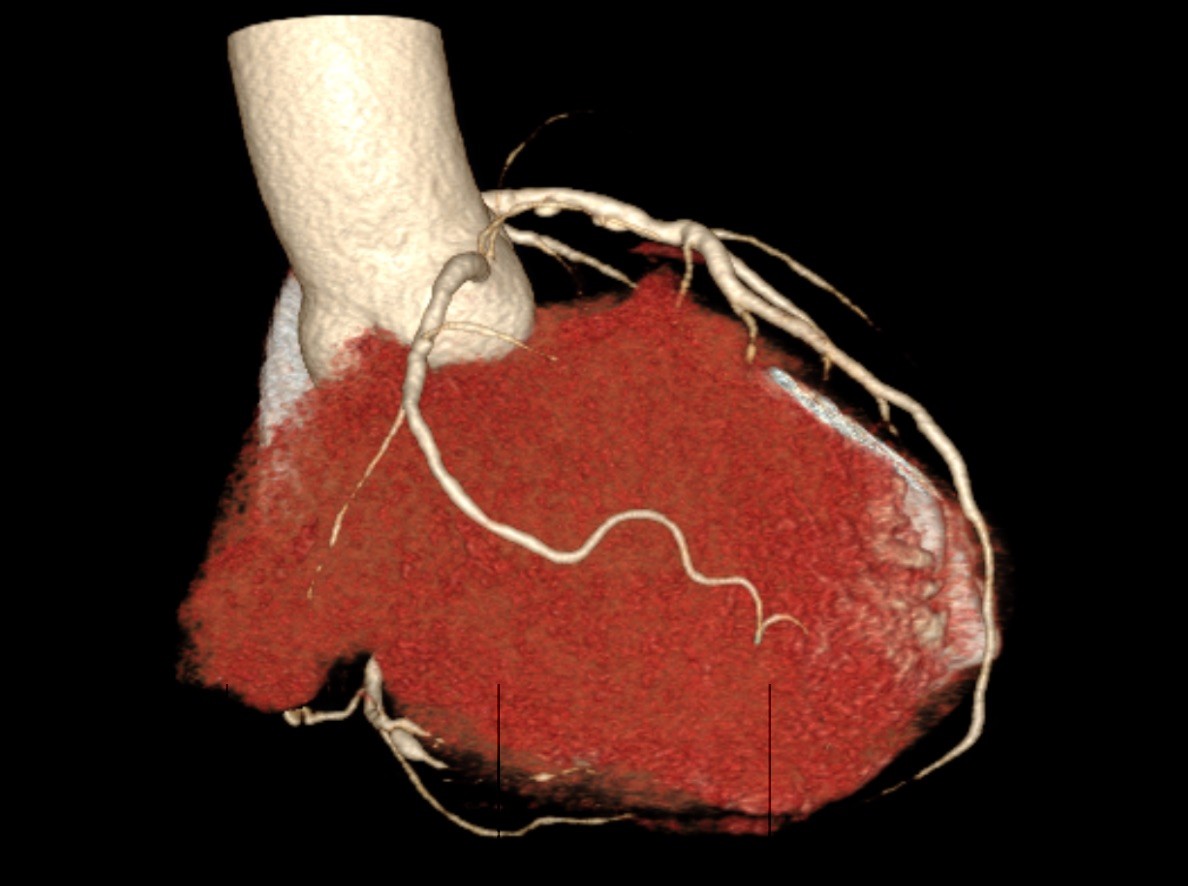
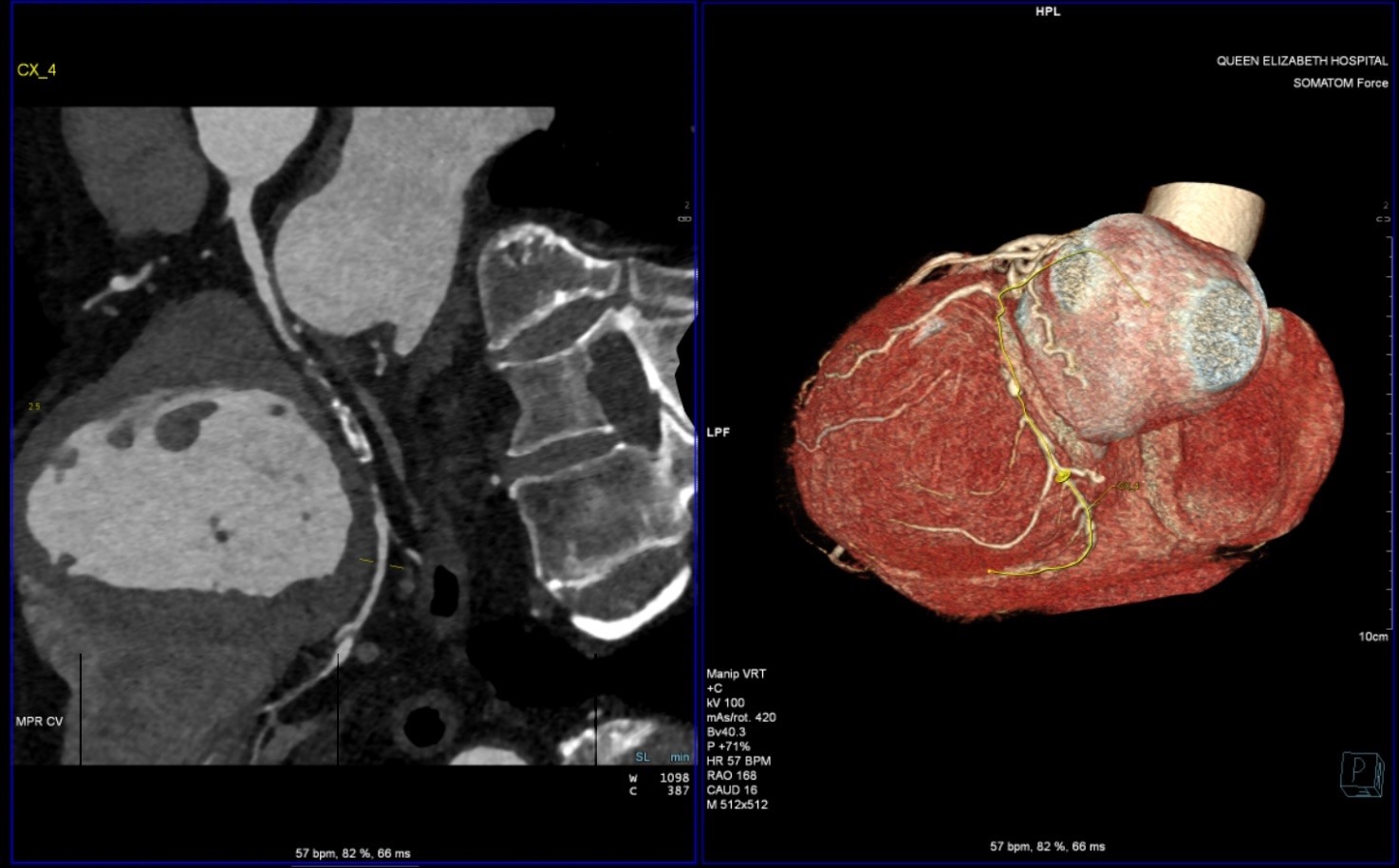
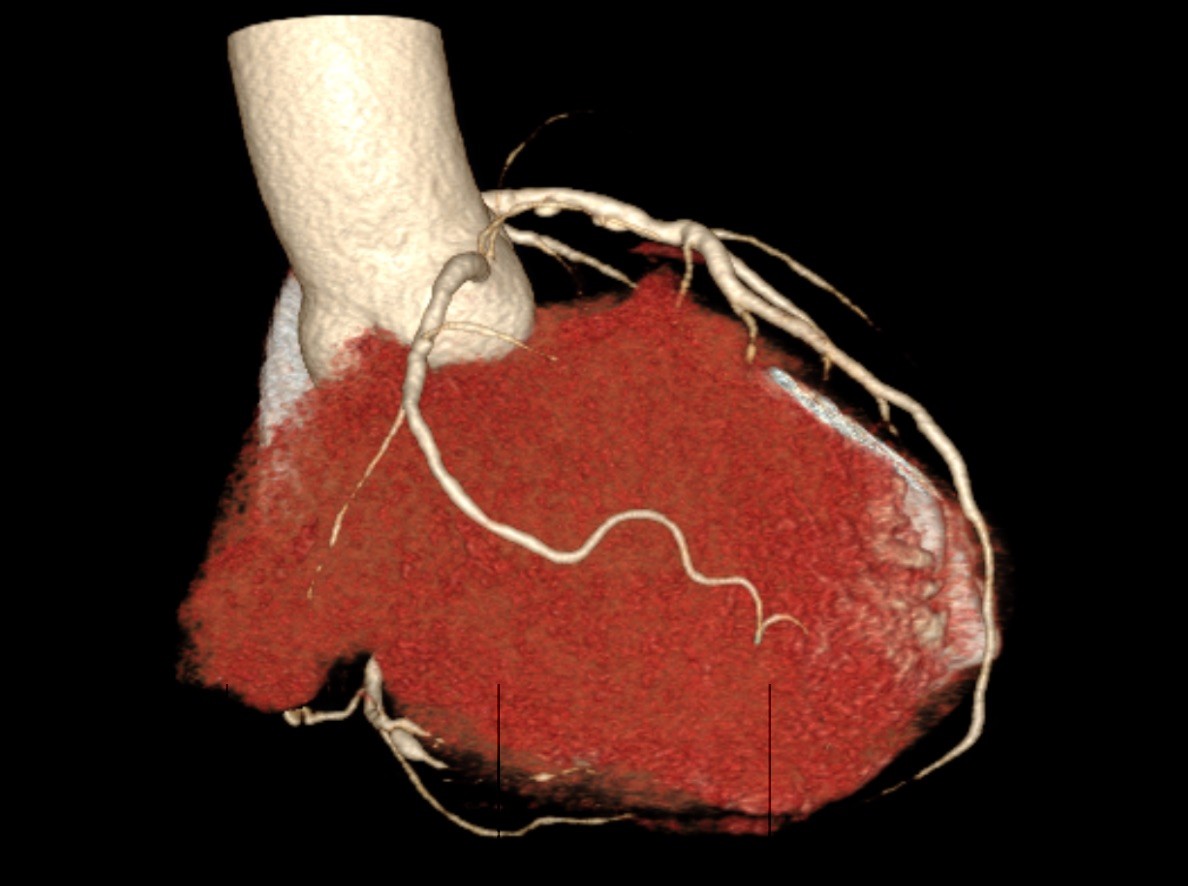
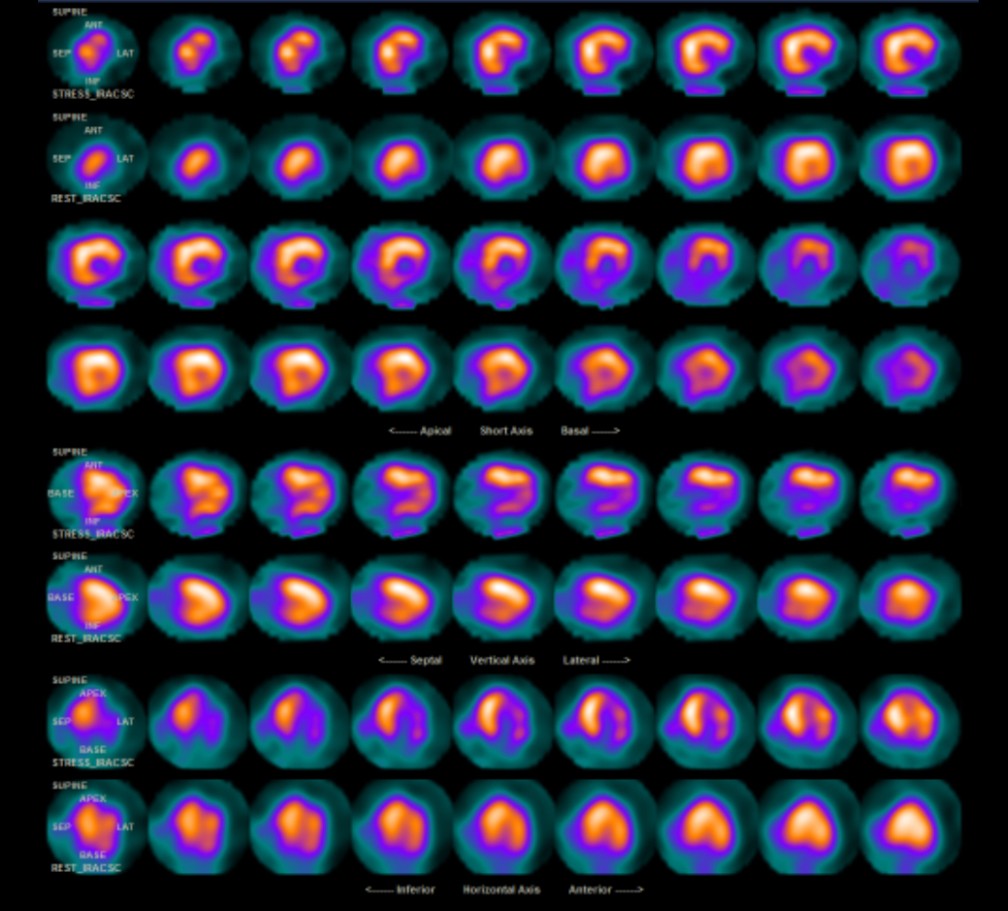
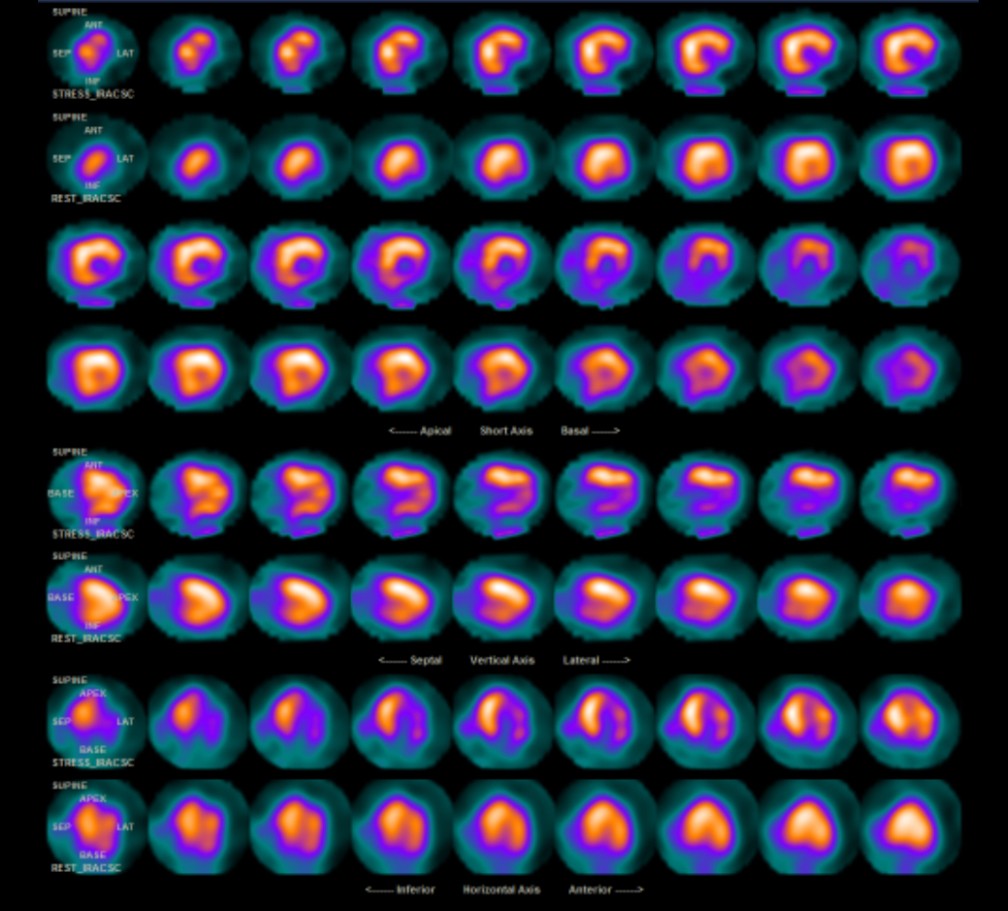
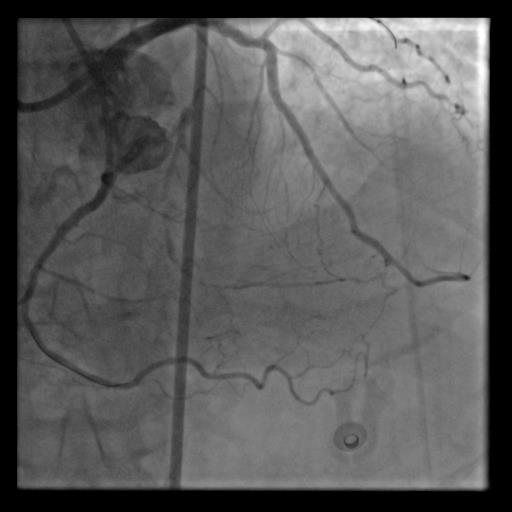
As symptom progressed, CT coronary angiography was arranged which showed chronic total occlusion (CTO) of distal left circumflex artery (LCx). A subsequent stress thallium myocardial perfusion scan indicated a moderate-sized reversible perfusion defect of moderate severity in the inferolateral wall, confirming myocardial ischemia
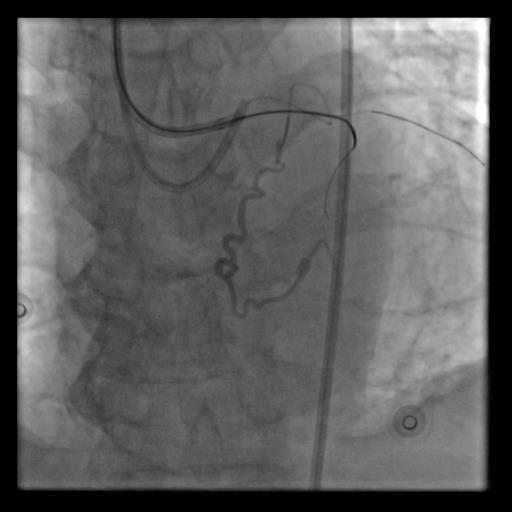
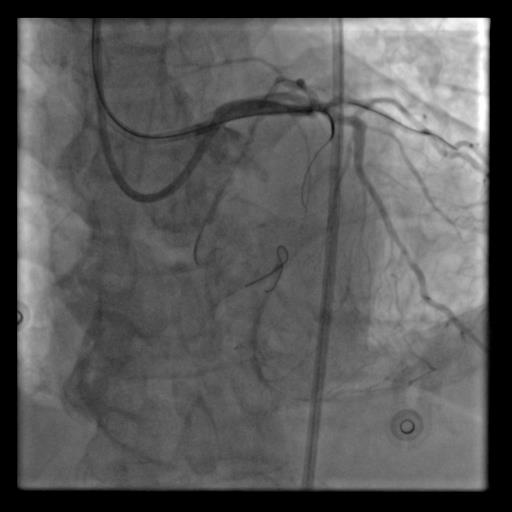
Relevant Catheterization Findings
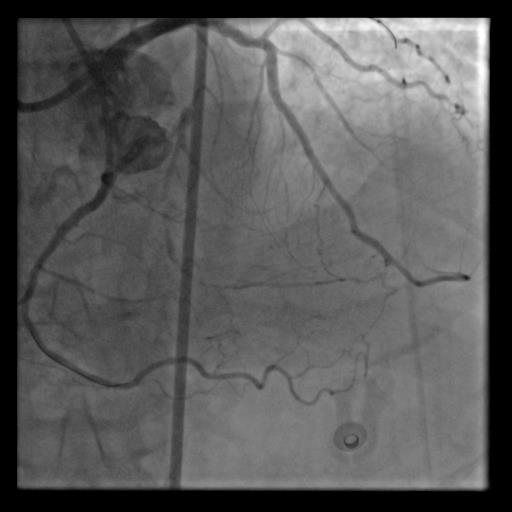
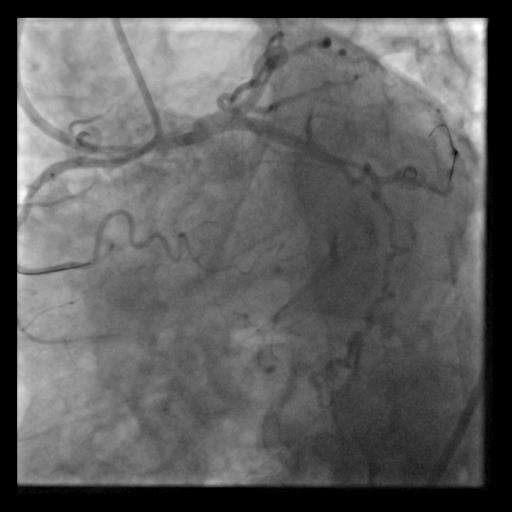
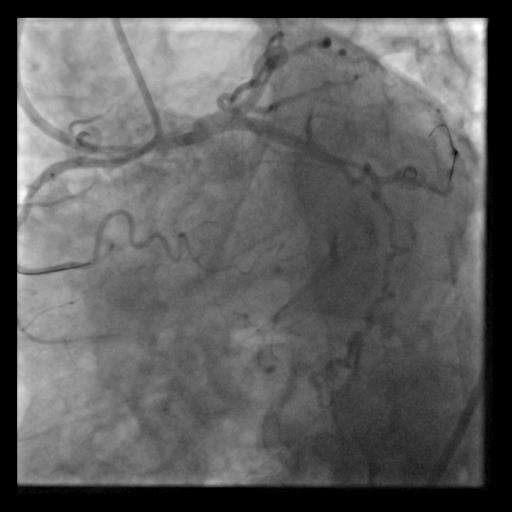
Coronary angiography revealed a left-dominant coronary anatomy with a chronic total occlusion (CTO) of the mid-left circumflex artery (LCx). There was left-to-left retrograde filling from septal collaterals of the left anterior descending artery (LAD) and the atrial branch from the proximal LCx. Additionally, retrograde filling to the distal left posterior descending artery (L-PDA) was noted from the right marginal branch of the right coronary artery (RCA).


Interventional Management
Procedural Step
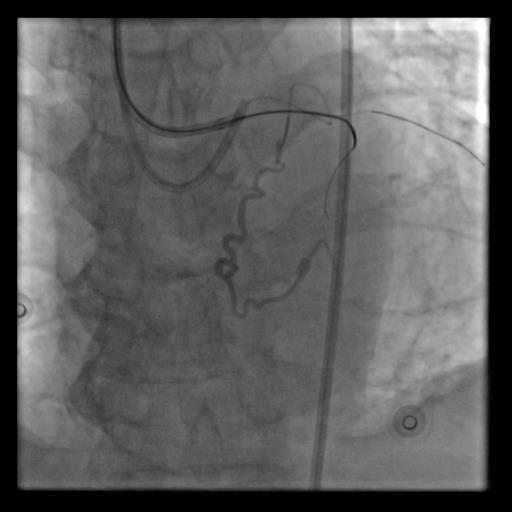
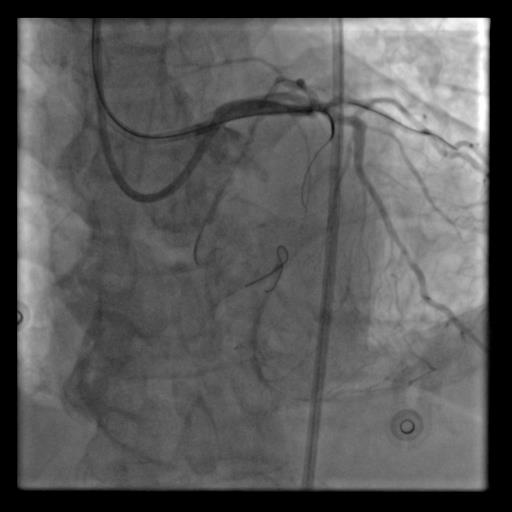
The procedure began with 7 French (F) right radial and 8F right femoral access. The RCA was engaged using a 7F IL 3.5 guiding catheter, while the left coronary artery (LCA) was accessed with an 8F EBU 3.5 catheter. Dual angiography revealed a 50mm mid-LCx CTO with a proximal blunt cap. Retrograde filling involved septal collaterals from the LAD, the atrial branch of the ipsilateral LCx, and the RV branch from the non-dominant RCA, resulting in a J-CTO score of 2. The initial strategy was to attempt antegrade IVUS-guided entry, with a switch to a retrograde approach if necessary.After unsuccessful antegrade punctures with ULTIMATEbros3 (UB3) and Gaia Next 3 wires, the proximal CTO cap was successfully punctured with a Conquest Pro 12 wire (CP12), which was then de-escalated to a Fielder XT-A wire that entered the subintimal space. A retrograde approach was initiated using Ping-Pong guiding catheters to the LCA. While attempts to navigate with Sion and Suoh 03 wires via septal collaterals initially failed, the Sion wire eventually crossed the tortuous ipsilateral left atrial branch into the distal obtuse marginal (OM) branch. A Gladius Ex wire then engaged the distal LCx CTO cap. The antegrade wire met in the mid LCx, and the reverse CART technique was performed. After externalization, IVUS was conducted with a segment of false lumen wiring. A DEB was delivered to L-PDA, and overlapping DES were deployed in the p-mLCx, resulting in satisfactory result.


Case Summary
In conclusion, this case highlights the importance of an algorithmic approach in chronic total occlusion percutaneous coronary intervention (CTO-PCI), which can enhance procedural success rates and patient outcomes. It emphasizes the critical balance between safety, speed, and success during these interventions, noting that this balance is dynamic and requires real-time adjustments. Additionally, the use of appropriate equipment is essential for navigating complex and tortuous lesions, as the right tools significantly improve procedural efficiency and patient safety. Ultimately, a systematic and thoughtful approach is key to achieving optimal results in CTO-PCI.


