Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-132
A Delicate Divide: The Challenges of the Unexpected. A Case of an Iatrogenic Aortocoronary Dissection in an Asian Male With ACS-NSTEMI
By Phil Iver Guevarra
Presenter
Phil Iver Guevarra
Authors
Phil Iver Guevarra1
Affiliation
Chung-Ang University Gwangmeyong Hospital, Philippines1,
View Study Report
TCTAP C-132
Coronary - Complication Management
A Delicate Divide: The Challenges of the Unexpected. A Case of an Iatrogenic Aortocoronary Dissection in an Asian Male With ACS-NSTEMI
Phil Iver Guevarra1
Chung-Ang University Gwangmeyong Hospital, Philippines1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 57-year-old obese male with no known ASCVD comorbidities and occasional alcohol use presented to the ER with intermittent, squeezing, midsternal chest pain lasting 30 minutes, non-radiating, aggravated by light activity, and associated with exertional dyspnea and light-headedness. On physical exam, the patient was diaphoretic and tachycardic at 105bpm. Other systems were essentially unremarkable. Initial assessment was acute coronary syndrome.


Relevant Test Results Prior to Catheterization
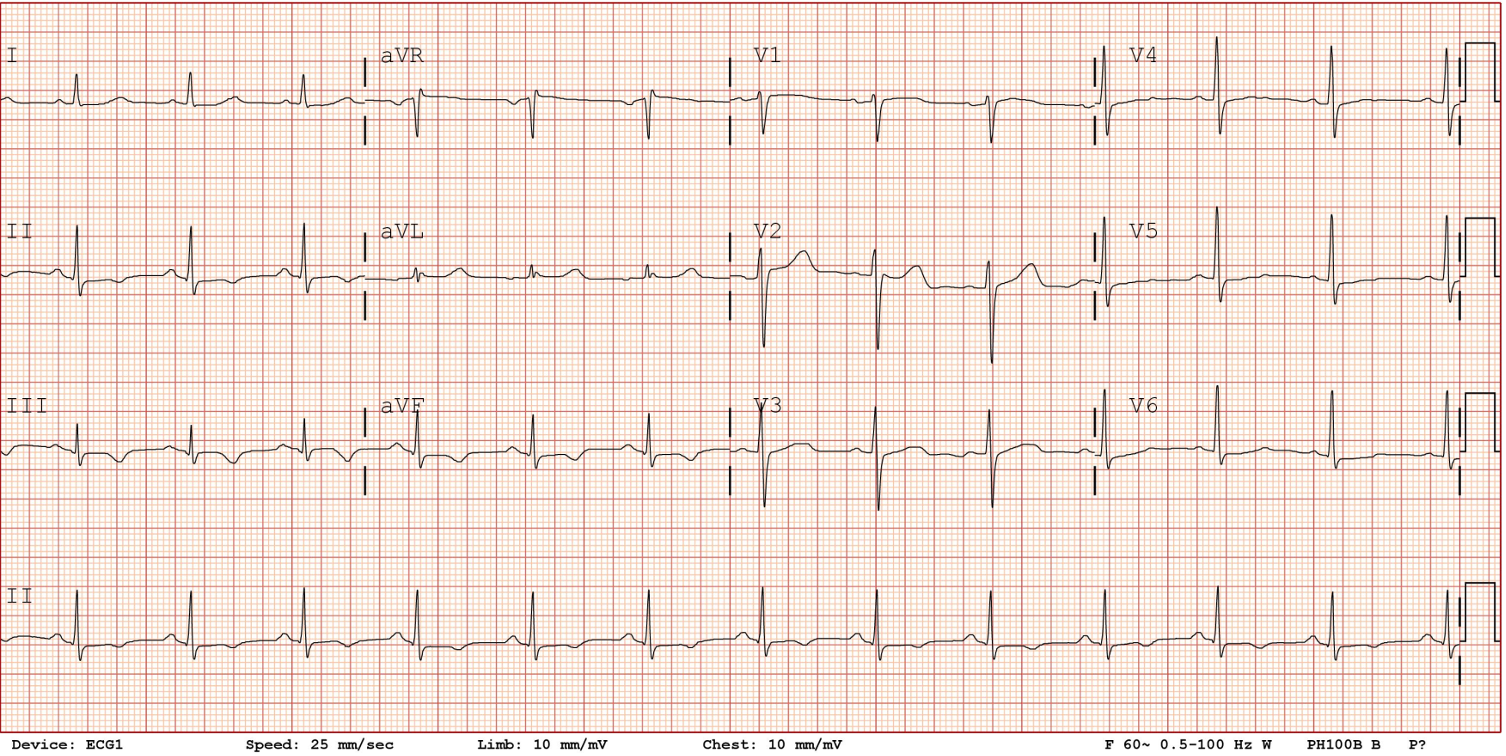
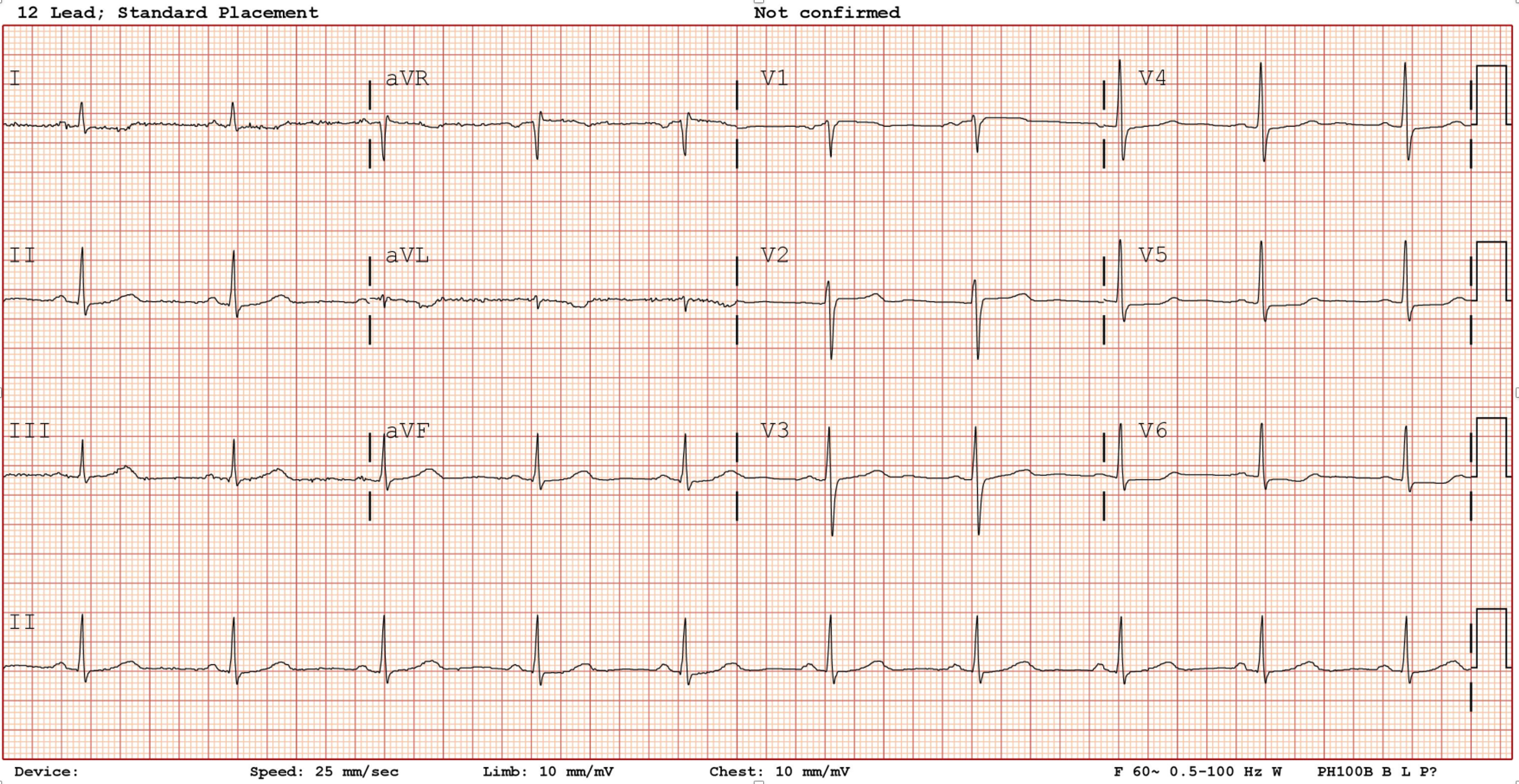
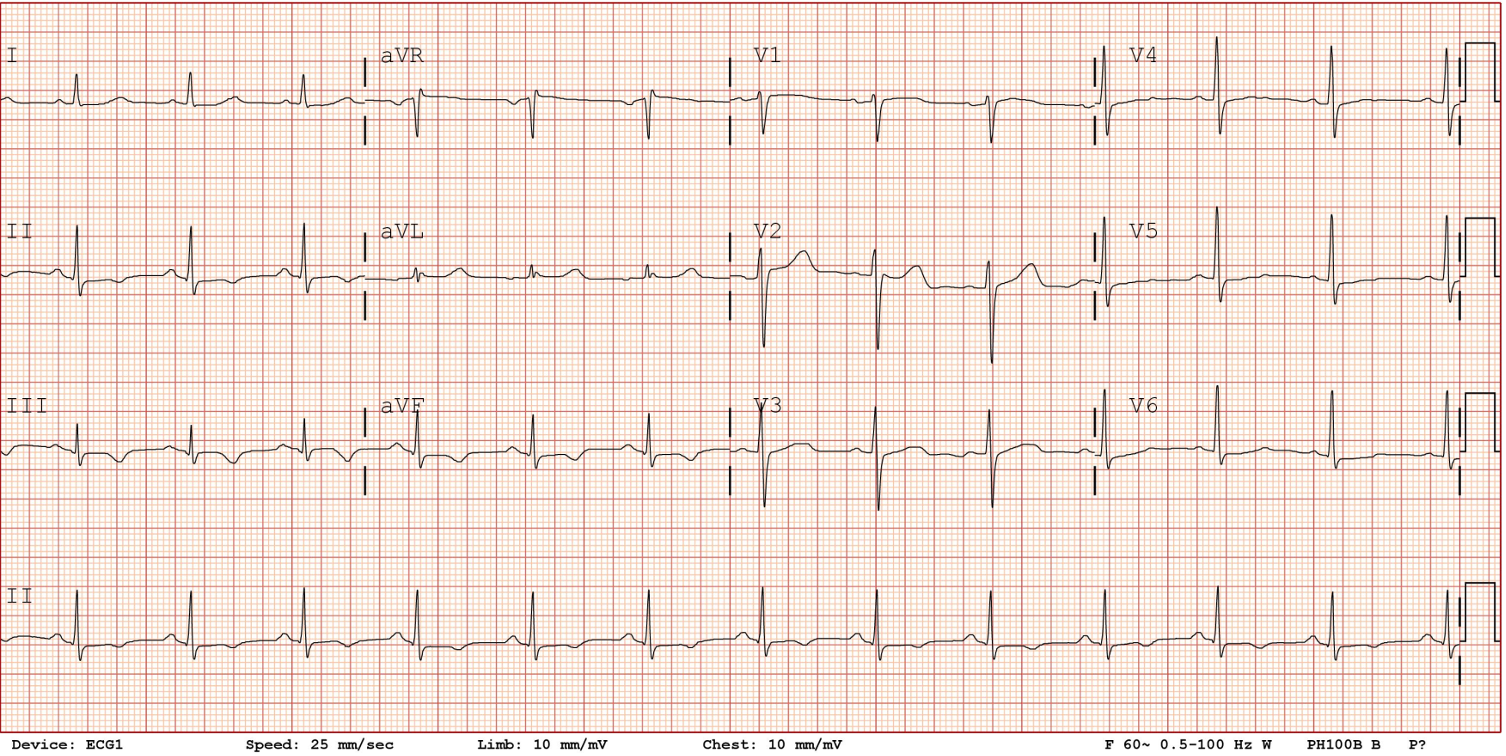
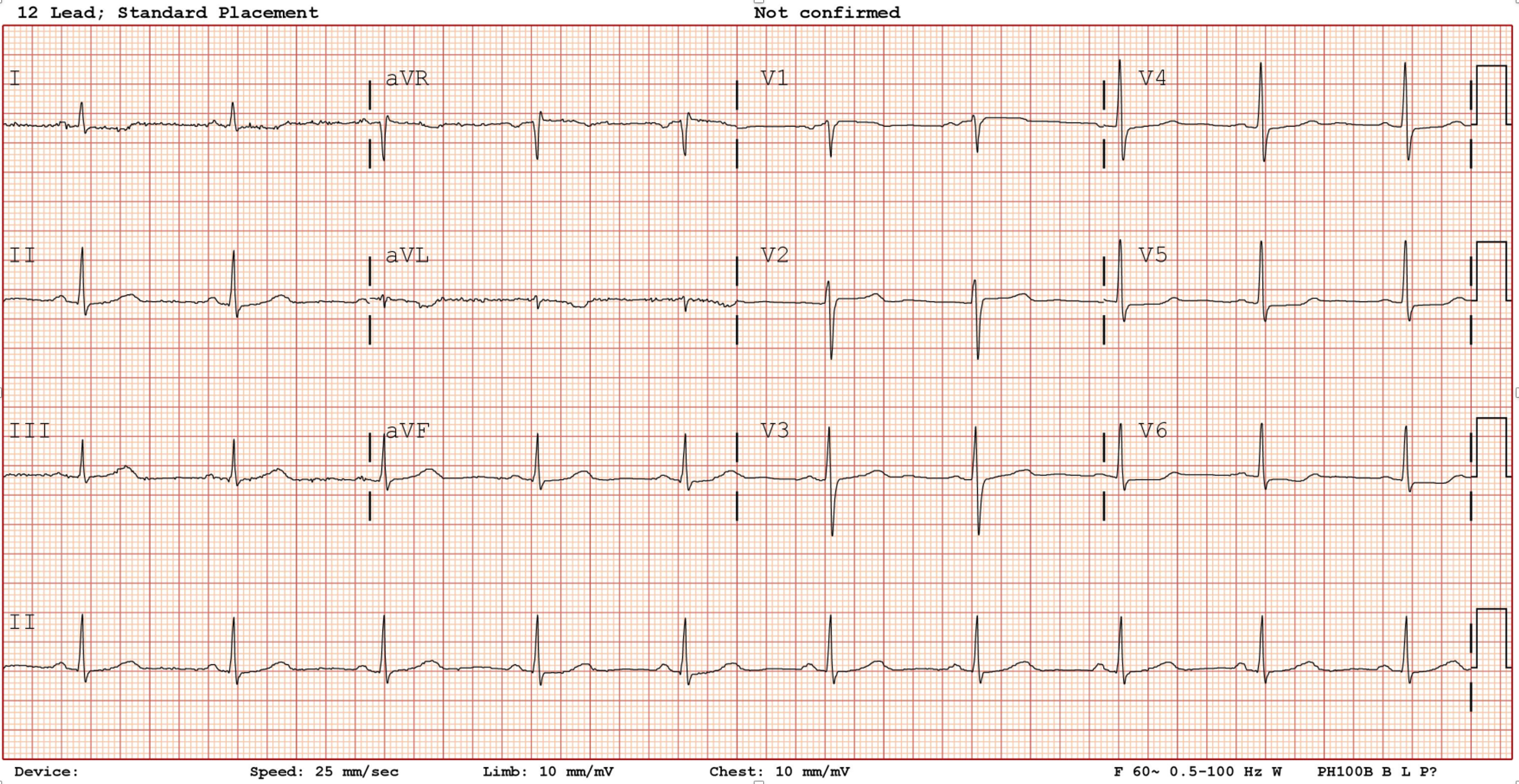
Pertinent findings include a 12L-ECG showing ST depressions in leads V5-V6, I, elevated HS-troponin I of 72.28pg/ml, but with a normal bedside echo (EF 65%, no wall motion abnormality).
Relevant Catheterization Findings
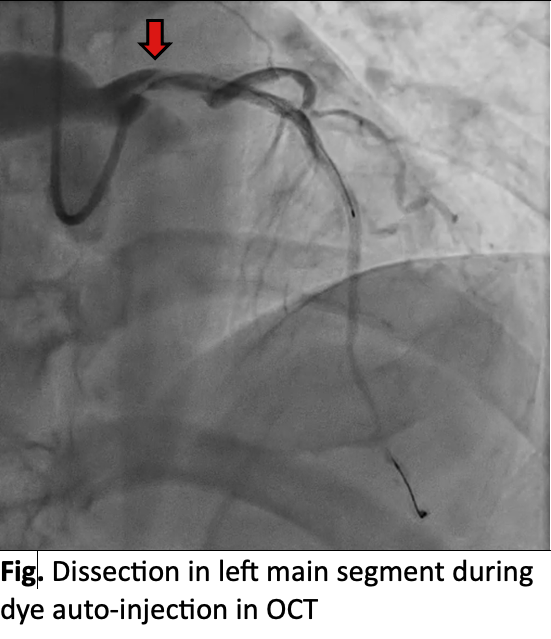
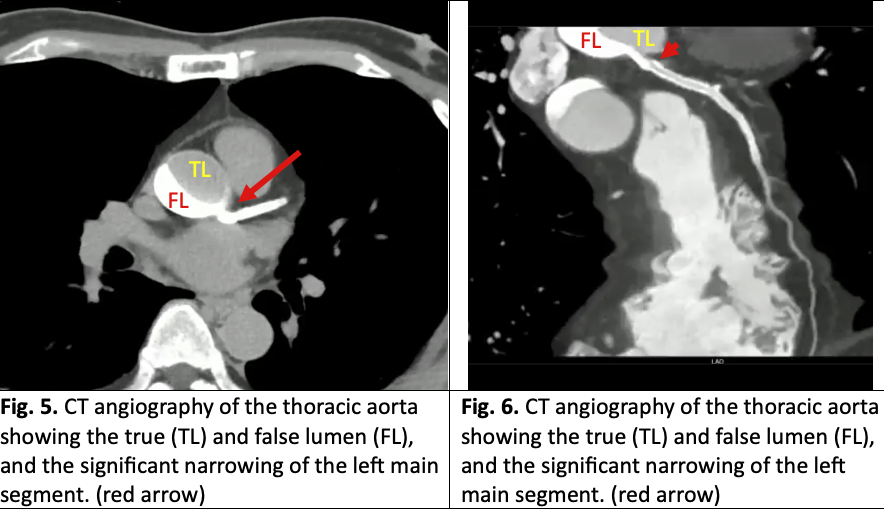
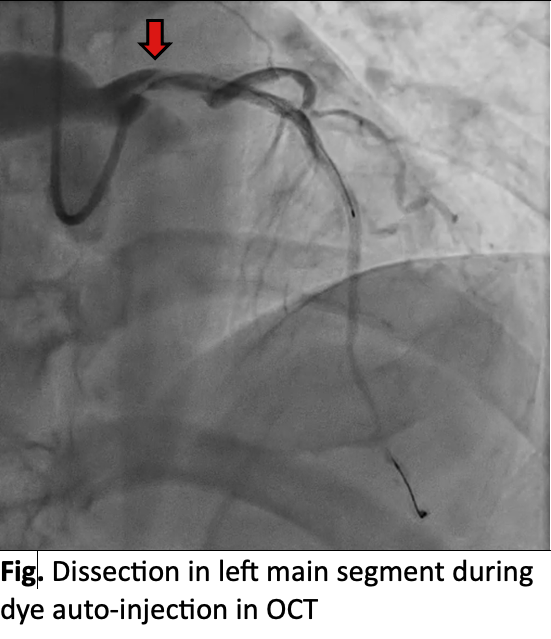
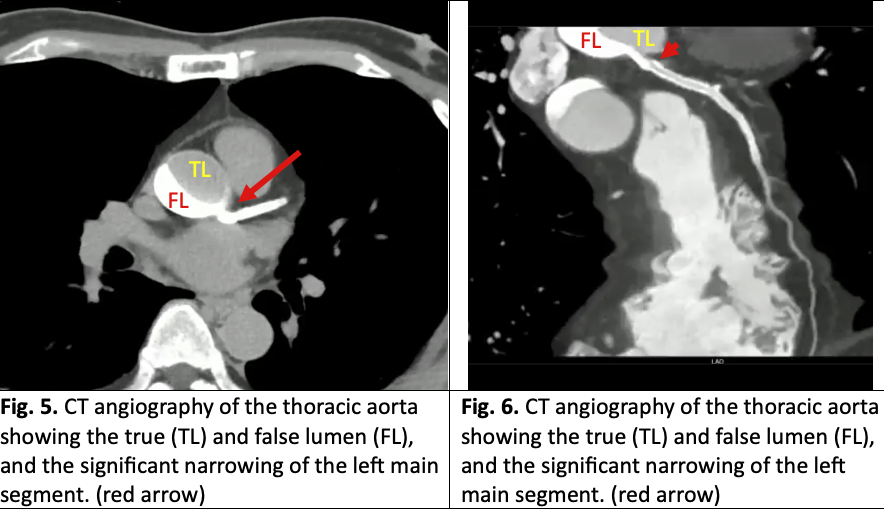
Three-vessel disease, specifically involving a 70% stenosis of the proximal to mid LAD, 70% stenosis of the mid LCx, and a 95% stenosis of the mid RCA. PCI of RCA and LAD was successful with OCT guidance. Post-PCI OCT, on auto-injection of the dye, a type D/E dissection was seen in the left main, causing significant luminal narrowing and staining of the false lumen. Patient remained stable with minimal chest pain and no ECG changes. CT angiography confirmed a Stanford type A aortic dissection
Interventional Management
Procedural Step
The mid RCA and proximal to mid LAD were successfully revascularized with OCT-guided PCI using POBA Asahi Kamui followed by stenting with an Orsiro mission. No complications were observed.
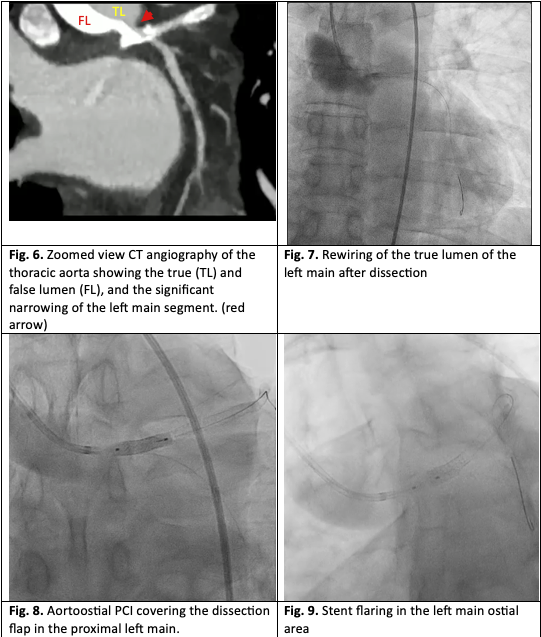
During the post-PCI OCT, however, a type D/E dissection was noted in the left main, causing significant luminal narrowing and staining of the false lumen. Fortunately, the patient remained stable with minimal chest pain and no ECG changes were noted. CT angiography confirmed a Stanford type A aortic dissection involving the aortic root and proximal ascending aorta. The decision was made, together with the cardiothoracic team, to treat the dissection percutaneously.
The left main was recannulated using a 6 french JR 4.0 catheter with relative ease. IVUS-guided PCI was successfully done with a Synergy XD 4.0 x 12mm, extending the stent towards the aorto-ostial area to cover the dissection flap. Repeat IVUS showed improved lumen size of the left main with good stent apposition. Final angiography showed resolution of the coronary dissection.
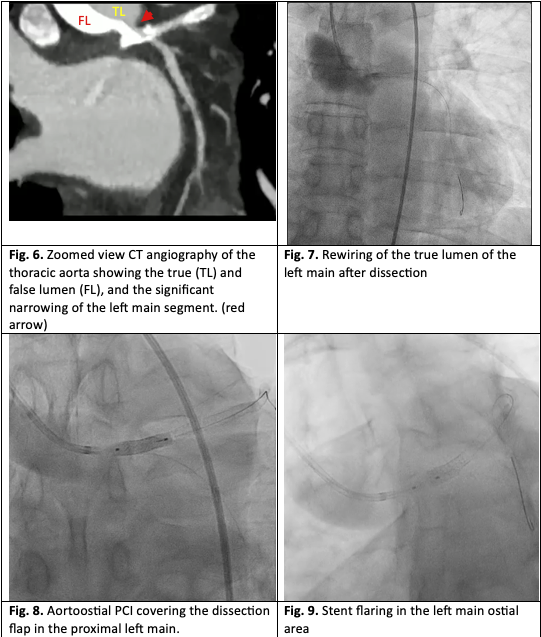


During the post-PCI OCT, however, a type D/E dissection was noted in the left main, causing significant luminal narrowing and staining of the false lumen. Fortunately, the patient remained stable with minimal chest pain and no ECG changes were noted. CT angiography confirmed a Stanford type A aortic dissection involving the aortic root and proximal ascending aorta. The decision was made, together with the cardiothoracic team, to treat the dissection percutaneously.
The left main was recannulated using a 6 french JR 4.0 catheter with relative ease. IVUS-guided PCI was successfully done with a Synergy XD 4.0 x 12mm, extending the stent towards the aorto-ostial area to cover the dissection flap. Repeat IVUS showed improved lumen size of the left main with good stent apposition. Final angiography showed resolution of the coronary dissection.


Case Summary
Follow-up CT angiography was done after 24 and 72 hours which revealed no extension of the aortic dissection and with evidence of beginning resolution of the intramural hematoma. The patient was hospitalized for a total of 6 days and was then discharge stable and ambulatory. After one month, the patient followed-up in the outpatient clinic with normal chest x-ray and 12L-ECG findings, and full resolution of his symptoms.


