Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-020
No Reflow in Primary PCI: A Disaster in Cath Lab
By Cut Aryfa Andra, Andika Sitepu, Andi Khairul, Hilfan Ade Putra Lubis, Lia Susanti
Presenter
Cut Aryfa Andra
Authors
Cut Aryfa Andra1, Andika Sitepu1, Andi Khairul1, Hilfan Ade Putra Lubis1, Lia Susanti2
Affiliation
Universitas Sumatera Utara, Indonesia1, Adam Malik Hospital, Indonesia2,
View Study Report
TCTAP C-020
Coronary - ACS/AMI
No Reflow in Primary PCI: A Disaster in Cath Lab
Cut Aryfa Andra1, Andika Sitepu1, Andi Khairul1, Hilfan Ade Putra Lubis1, Lia Susanti2
Universitas Sumatera Utara, Indonesia1, Adam Malik Hospital, Indonesia2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 76 year old female patient presented with acute typical angina at rest started 4 hours before arriving at the hospital. The chest pain was described as a heavy, crushing sensation that radiated to the back and it was accompanied by nausea, vomiting and cold sweats. The patient denied any previous history of chest pain. Risk factor for CAD was menopause. There was no history of hypertension, diabetes or smoking. Patient was fully counsious with stable hemodynamics. Basal lung rales were found.
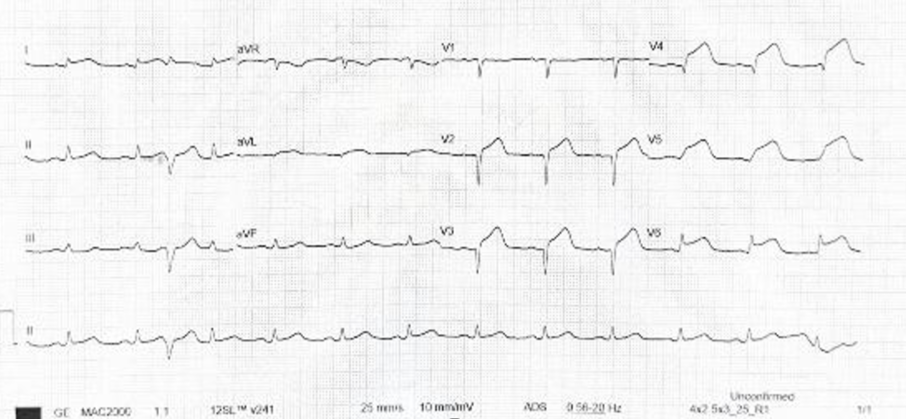
Relevant Test Results Prior to Catheterization
ECG showed sinus rhythm, anteriorextensive STEMI, infrequent PVC. Chest X ray showed cardiomegaly (CTR 57%). Echocardiography findings indicated LVEF was severely reduced (LVEF24%), diastolic function was also impaired. Wall motion abnormalities were extensive.


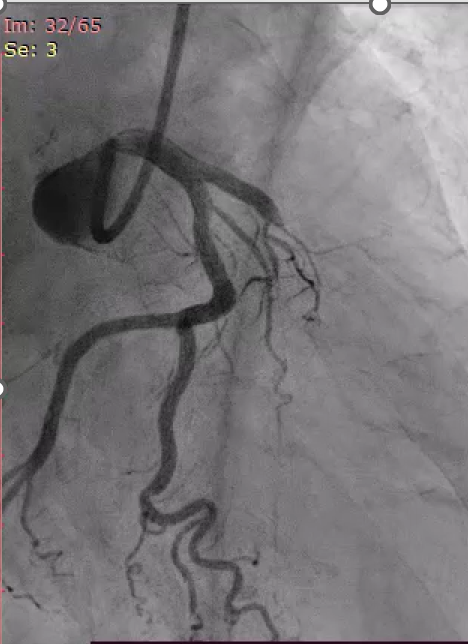
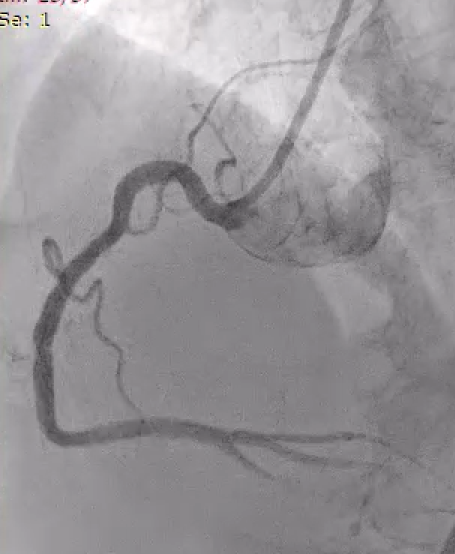
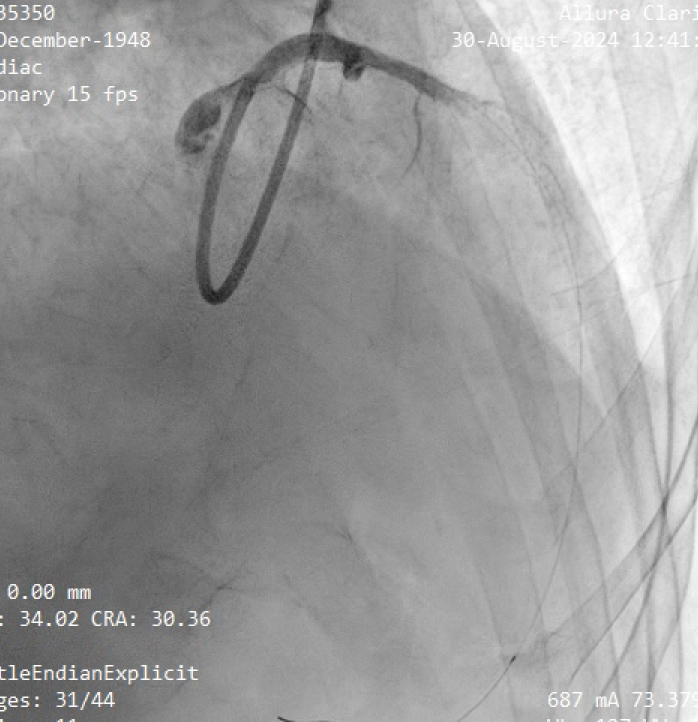
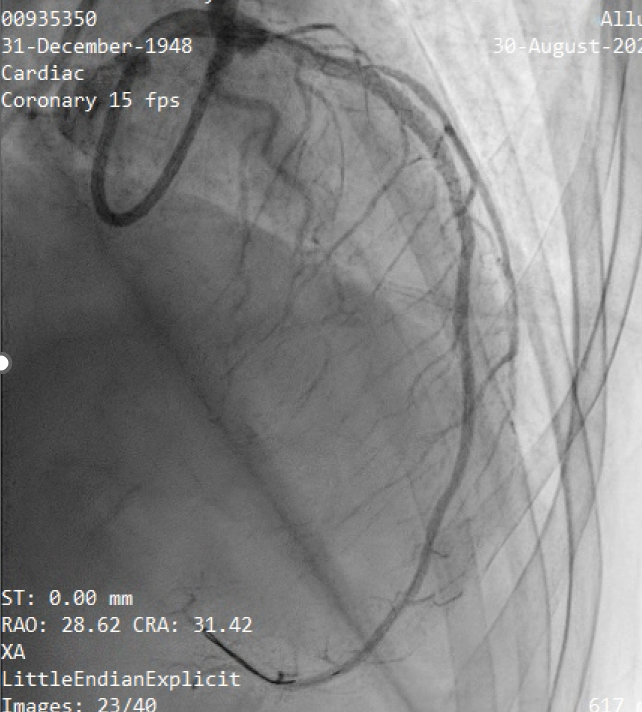
Relevant Catheterization Findings
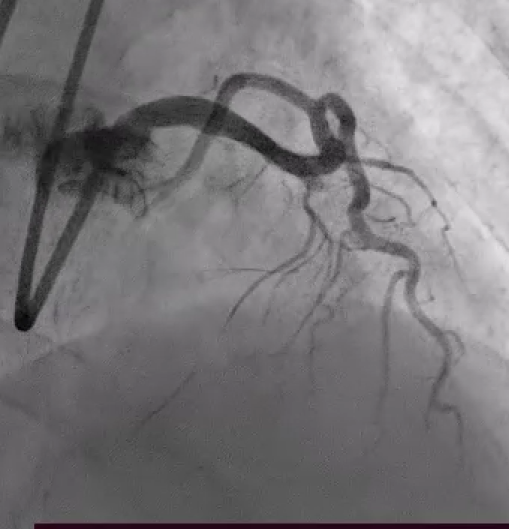
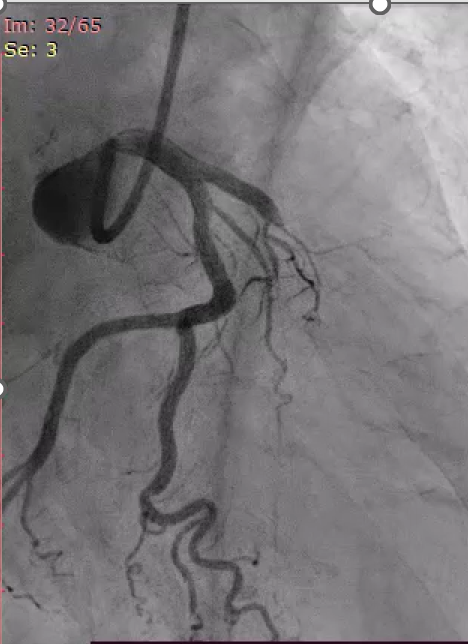
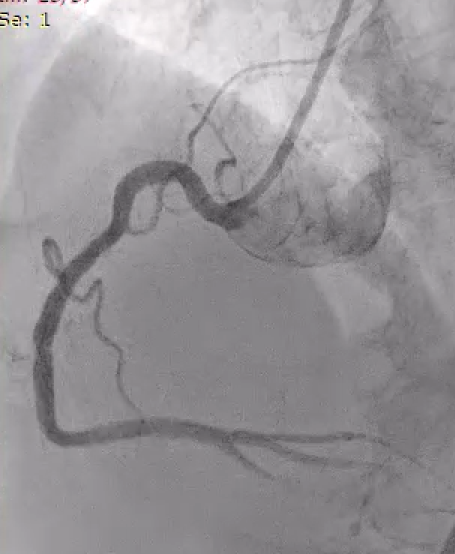
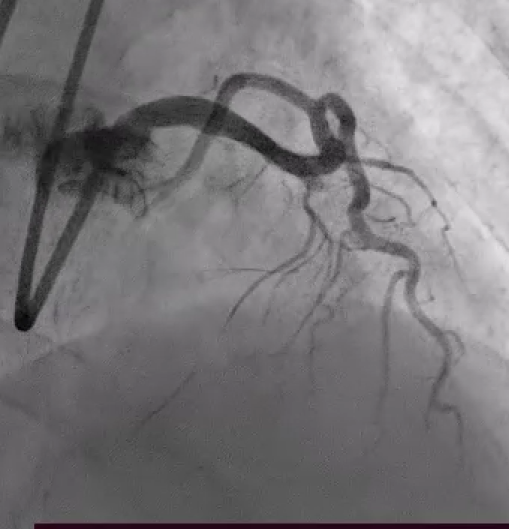
CAG : Single vessel disease. 100% thrombotic stenosis at proximal LAD.
Interventional Management
Procedural Step
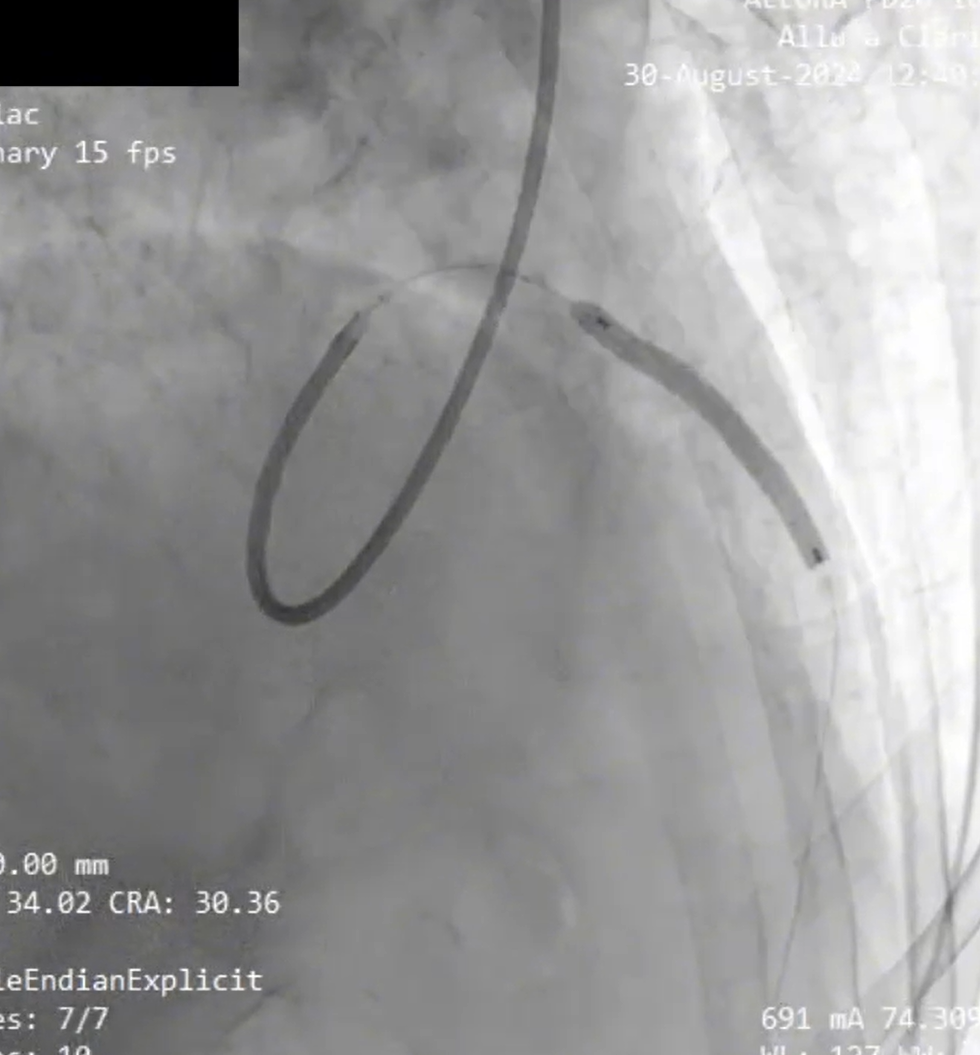
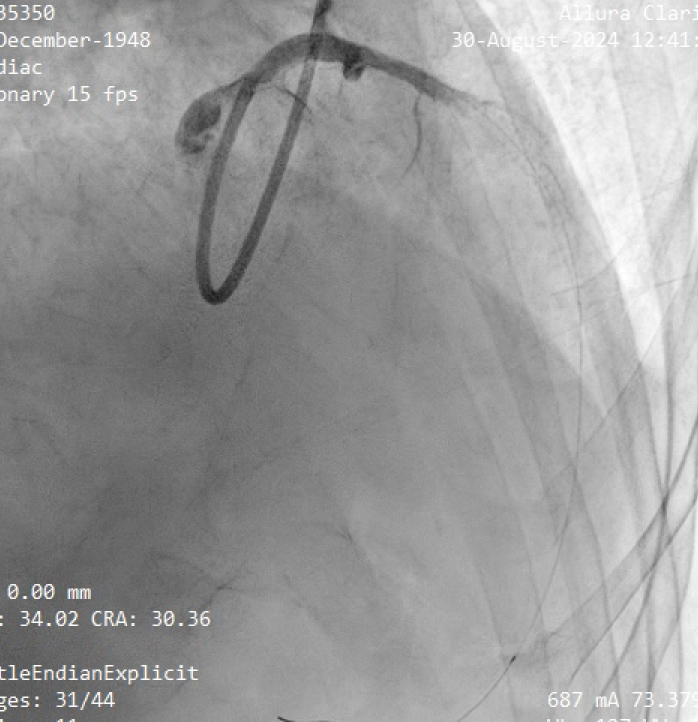
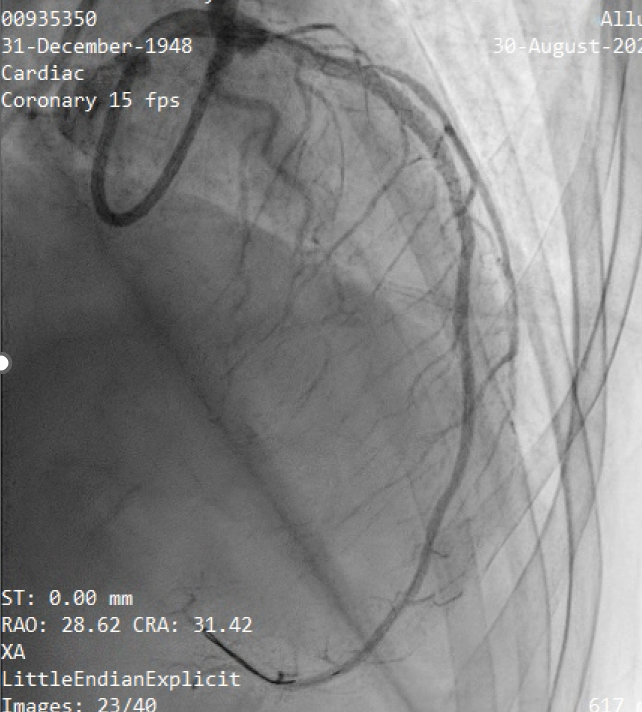
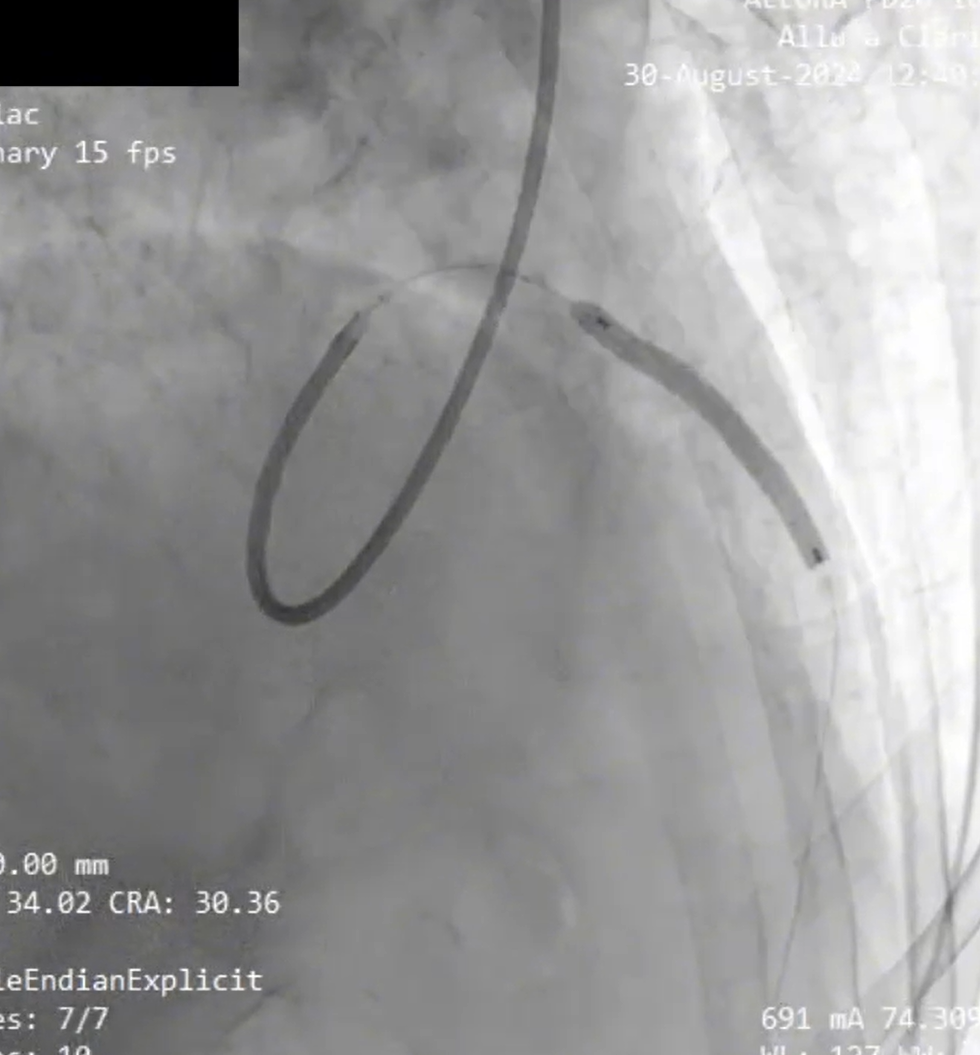
Primary PCI to LAD was done using 6 Fr EBU 3 guiding catheter. BMW wire advanced into distal LAD. CAG showed TIMI 1 flow. Pre dilated was done using SC balloon 2,5 x 15 mm, 14 atm, 10 sec at proximal LAD. CAG showed TIMI 2 flow, multiple stenosis 70-80% from proximal to mid LAD. Proximal to mid LAD was stented with DES 3,0 x 33 mm, 18 atm, 10 sec. CAG showed no reflow. Patient became unresponsive, ECG showed VT pulseless and drop in systolic blood pressure. We started CPR and DC shock. Eptifibatide was administered intracoronary, followed by repeat balloon dilatation at the stent site using SC balloon. The procedure continued with the administration of 1000 IU of heparin intracoronary. The patient achieved ROSC and regained full consciousness. Angiography revealed no residual stenosis or thrombus with TIMI 3 flow.
Case Summary
Patients with STEMI who get Primary PCI frequently experience coronary no reflow, ranging from 5% to 32%. No-reflow during or after primary PCI is a significant complication characterized by inadequate perfusion of the myocardium despite successful epicardial coronary artery revascularization. Managing no-reflow is crucial to improve outcomes. In the management of no reflow during primary PCI, several drugs are commonly used to improve microvascular perfusion.


