Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-077
Real Time IVUS Guided Reentry With Tip Detection Method in a CTO Case
By Thomas Tsun Ho Lam, Frankie Chor Cheung Tam
Presenter
Thomas Tsun Ho Lam
Authors
Thomas Tsun Ho Lam1, Frankie Chor Cheung Tam1
Affiliation
Queen Mary Hospital, Hong Kong, China1,
View Study Report
TCTAP C-077
Coronary - Complex PCI - CTO
Real Time IVUS Guided Reentry With Tip Detection Method in a CTO Case
Thomas Tsun Ho Lam1, Frankie Chor Cheung Tam1
Queen Mary Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
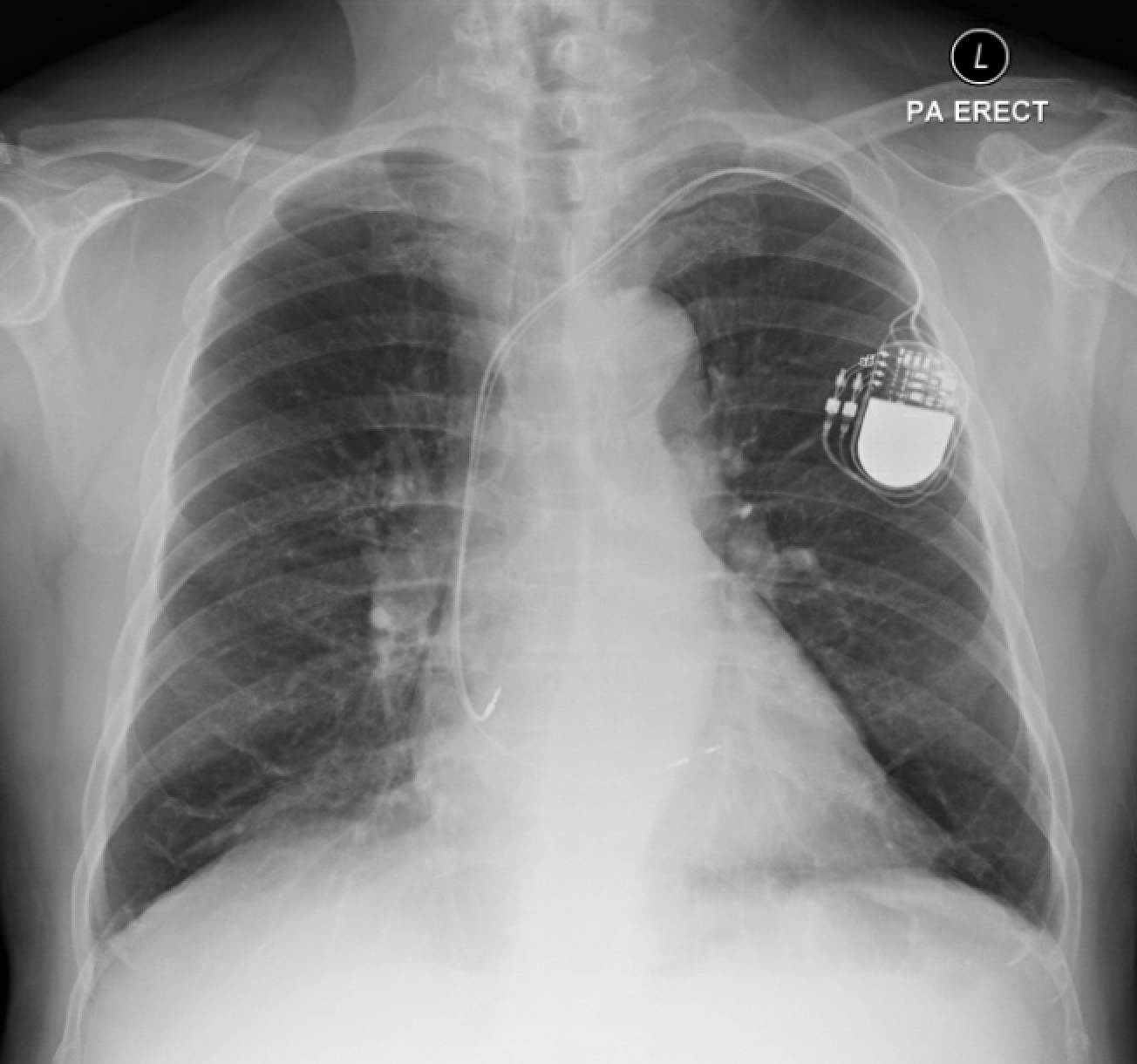
The 71-year-old male patient has a complex medical history, including hypertension, hyperlipidemia, chronic kidney disease (eGFR 30), and complete heart block with a dual chamber pacemaker.
He presented with progressive angina despite medical therapy. Physical examination was unremarkable.
He presented with progressive angina despite medical therapy. Physical examination was unremarkable.
Relevant Test Results Prior to Catheterization
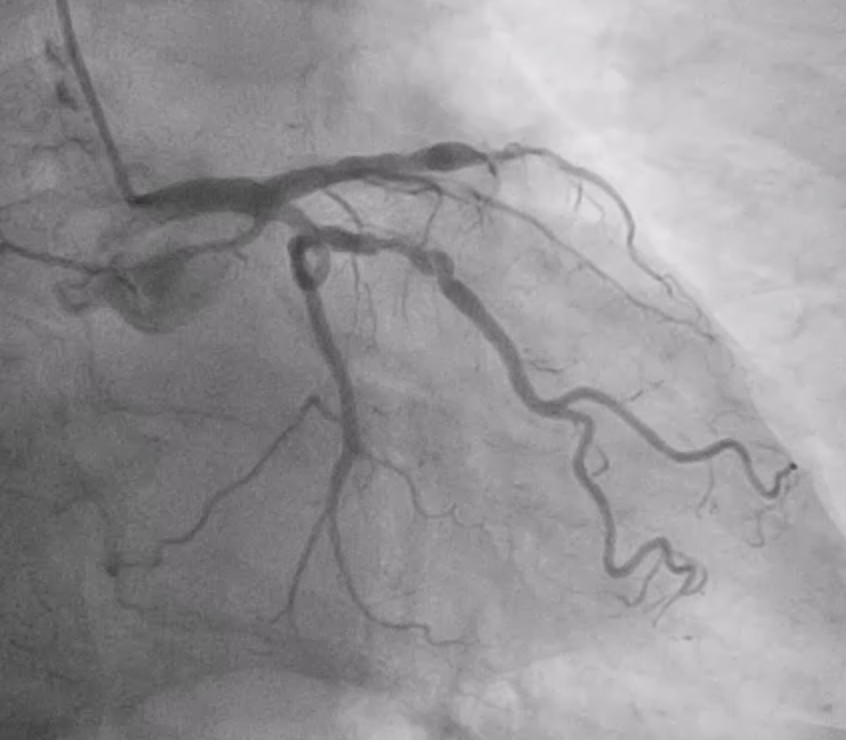
Echocardiogram revealed a preserved biventricular systolic function and normal valvular function. A Coronary Computed Tomography Angiography (CTCA) showed occlusion of the mid portion of left anterior descending artery (mLAD) and severe stenosis in the left circumflex artery (LCx).


Relevant Catheterization Findings
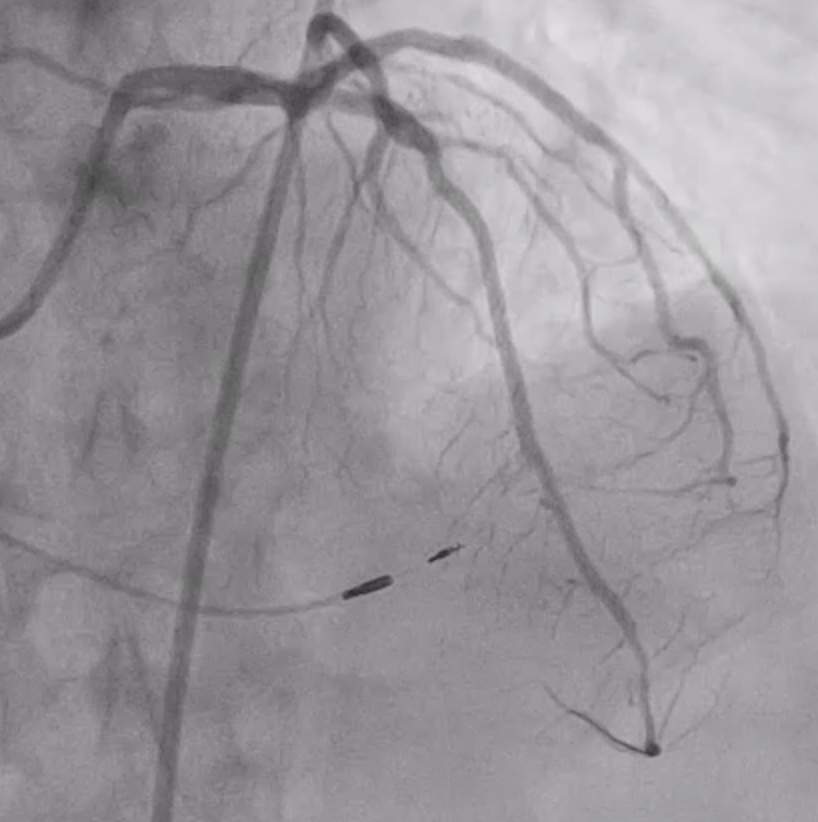
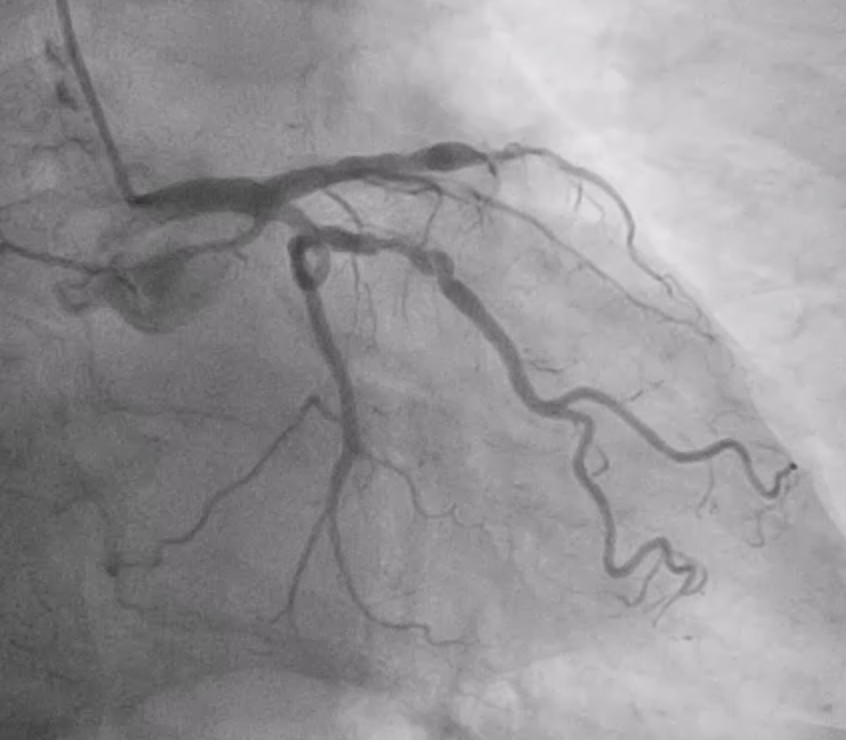
Invasive coronary angiography confirmed a chronic total occlusion (CTO) of the mLAD with right-to-left collaterals, severe stenosis of the proximal LCx, and mild disease in the right coronary artery (RCA). The patient underwent percutaneous coronary intervention (PCI) to the LCx uneventfully. However, he continued to experience refractory angina, prompting a return for PCI to address the mLAD CTO.




Interventional Management
Procedural Step
During the procedure, bifemoral access were obtained for a 7Fr EBU 3.5 guide catheter and a Tiger diagnostic catheter for contralateral injection. A Turnpike 135 microcatheter was used alongside an Fielder XT-A guidewire, which was unable to cross the chronic total occlusion (CTO). Intravascular Ultrasound (IVUS) with Terumo Anteowl IVUS catheter was performed to resolve proximal cap ambiguity.
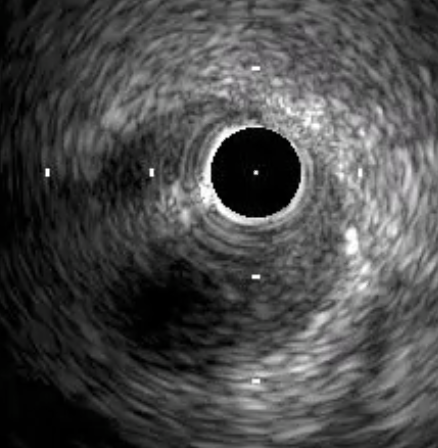
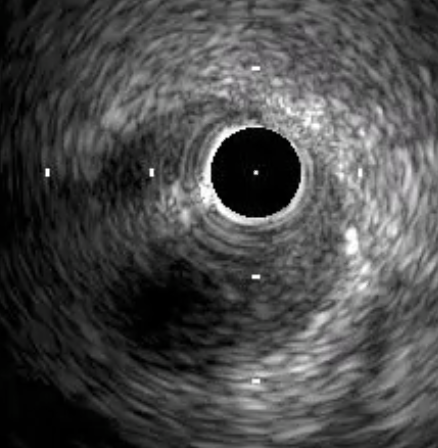
Antegrade wire escalation technique was used. Gaia Next 2 went into distal LAD extraplaque space, but attempts to re-enter the true lumen were unsuccessful. A parallel wire technique was employed with a Gaia Next 3 guidewire on a Sasuke dual lumen microcatheter which successfully entered the distal true lumen. A 1.5 mm balloon was then used to dilate the LAD. Subsequent IVUS imaging confirmed that the distal wire was in the true lumen, while a long segment of subintimal wire position was noted.
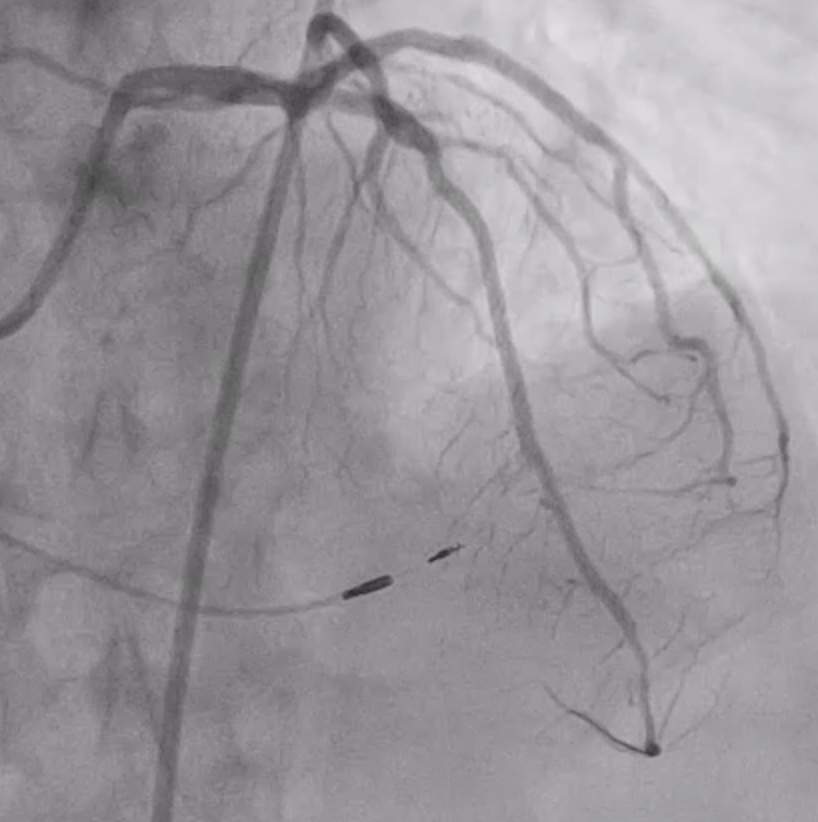
A real time IVUS-guided wire re-entry was performed, with the Anteowl IVUS identifying the optimal site for re-entry. A Hightrack 1.7 microcatheter loaded with Conquest pro 12 guidewire successfully re-entered the intraplaque space under IVUS guidance. Microcatheter was advanced into the intraplaque space, and the wire was stepped down to Sion Black, allowing entry back into the true lumen of the distal LAD. Further dilatation and stenting with Third generation Drug Eluting Stent were performed. IVUS showed residual very short segment of subintimal stenting with preservation of side branches.

Antegrade wire escalation technique was used. Gaia Next 2 went into distal LAD extraplaque space, but attempts to re-enter the true lumen were unsuccessful. A parallel wire technique was employed with a Gaia Next 3 guidewire on a Sasuke dual lumen microcatheter which successfully entered the distal true lumen. A 1.5 mm balloon was then used to dilate the LAD. Subsequent IVUS imaging confirmed that the distal wire was in the true lumen, while a long segment of subintimal wire position was noted.
A real time IVUS-guided wire re-entry was performed, with the Anteowl IVUS identifying the optimal site for re-entry. A Hightrack 1.7 microcatheter loaded with Conquest pro 12 guidewire successfully re-entered the intraplaque space under IVUS guidance. Microcatheter was advanced into the intraplaque space, and the wire was stepped down to Sion Black, allowing entry back into the true lumen of the distal LAD. Further dilatation and stenting with Third generation Drug Eluting Stent were performed. IVUS showed residual very short segment of subintimal stenting with preservation of side branches.