Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-241
A Stubborn Thrombus in the Leg
By Jeffrey Chun-Yin Lee, Guangming Tan
Presenter
Jeffrey Chun-Yin Lee
Authors
Jeffrey Chun-Yin Lee1, Guangming Tan2
Affiliation
Grantham Hospital, Hong Kong, China1, Prince of Wales Hospital, Hong Kong, China2,
View Study Report
TCTAP C-241
Endovascular - Thrombus Removal Devices and Techniques
A Stubborn Thrombus in the Leg
Jeffrey Chun-Yin Lee1, Guangming Tan2
Grantham Hospital, Hong Kong, China1, Prince of Wales Hospital, Hong Kong, China2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
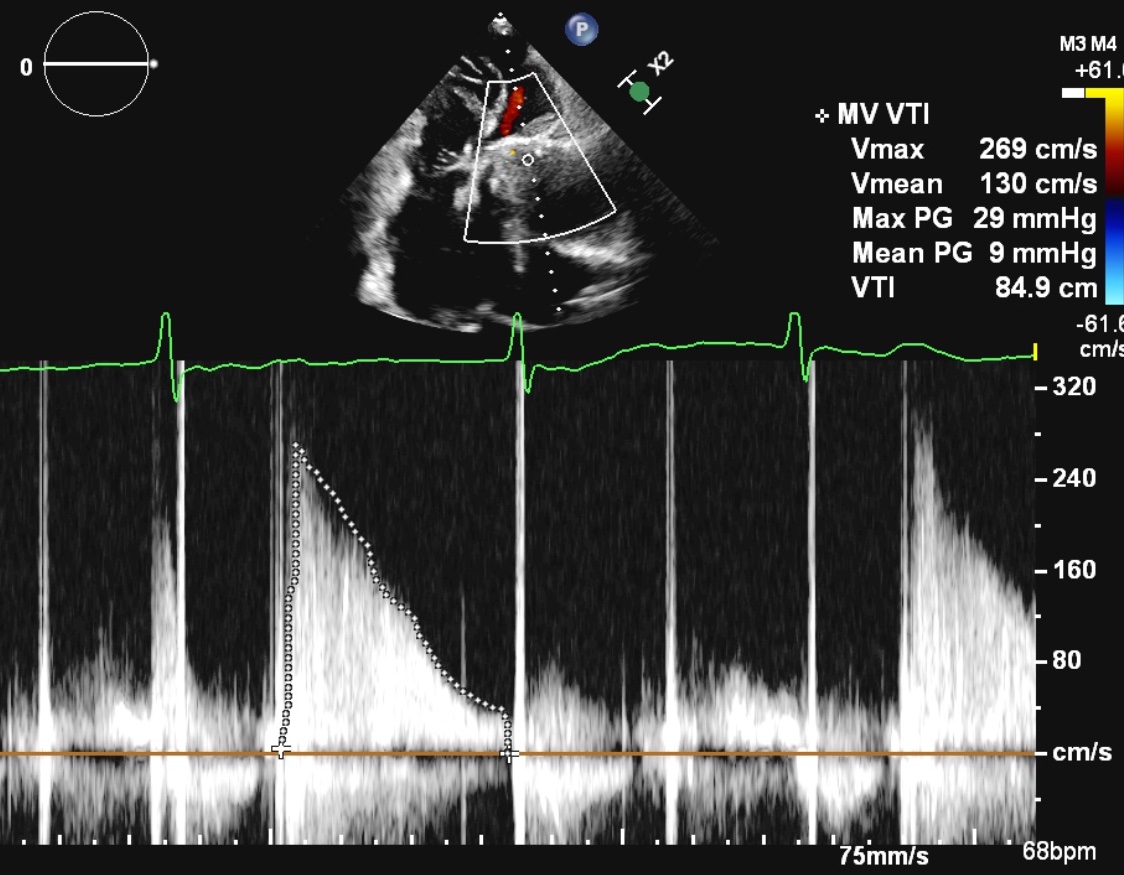
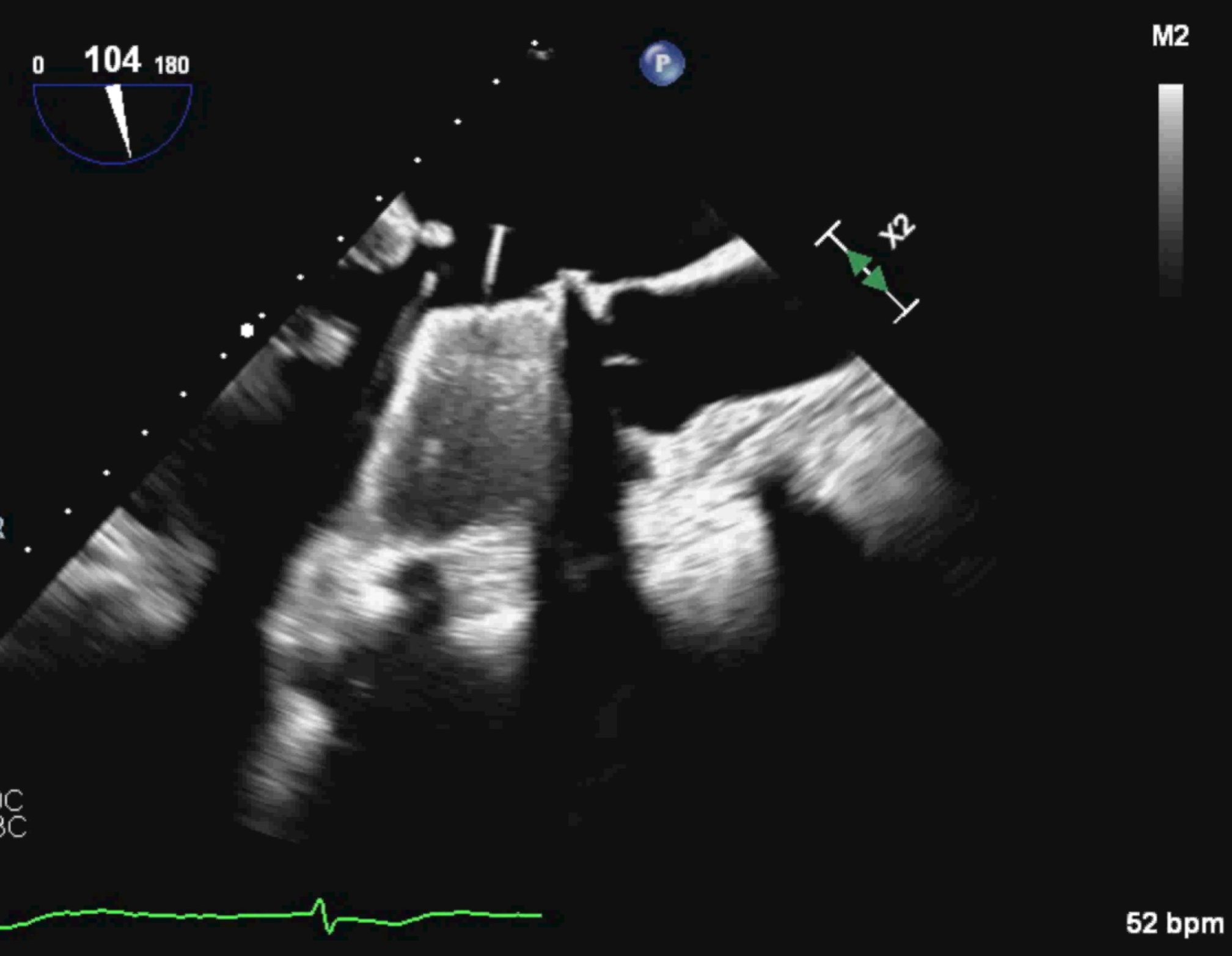
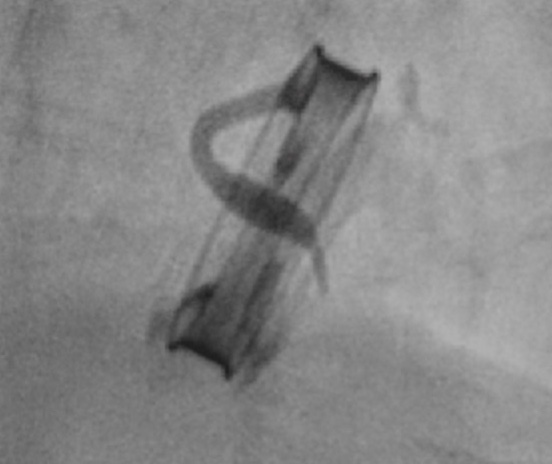
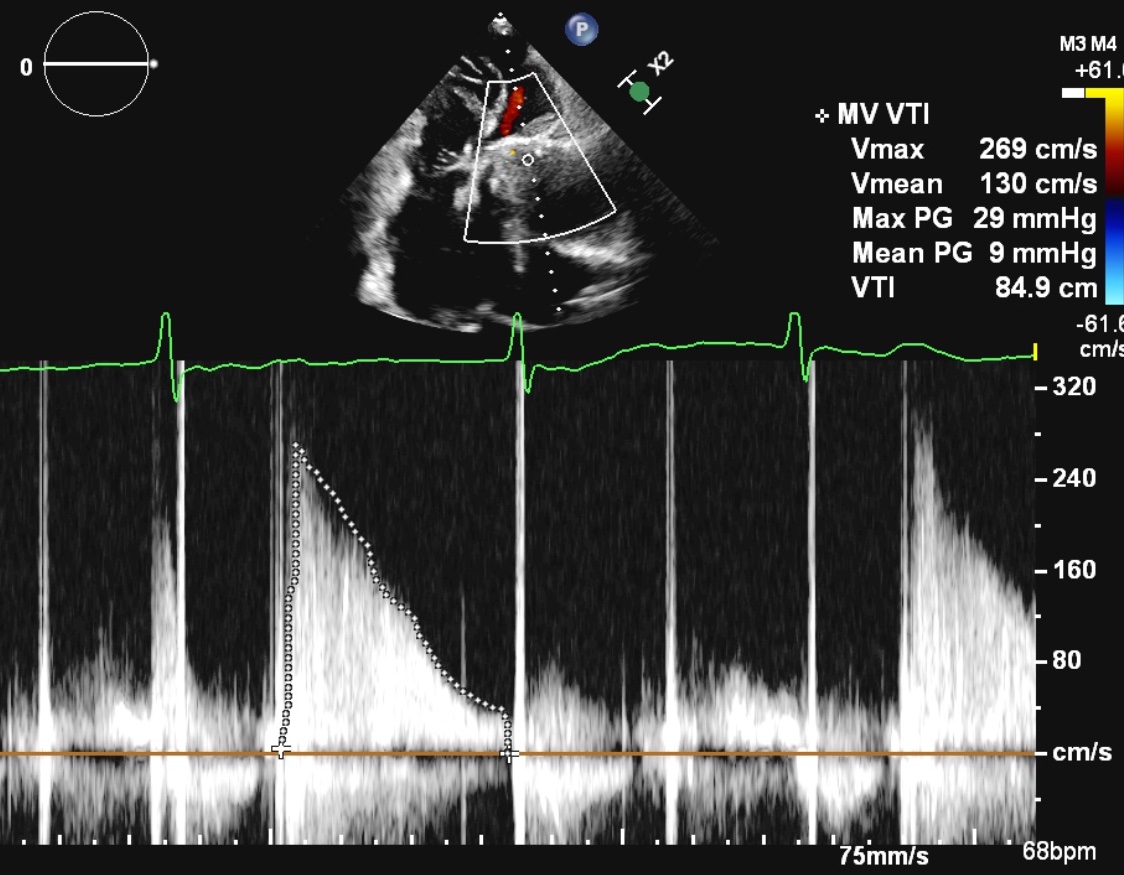
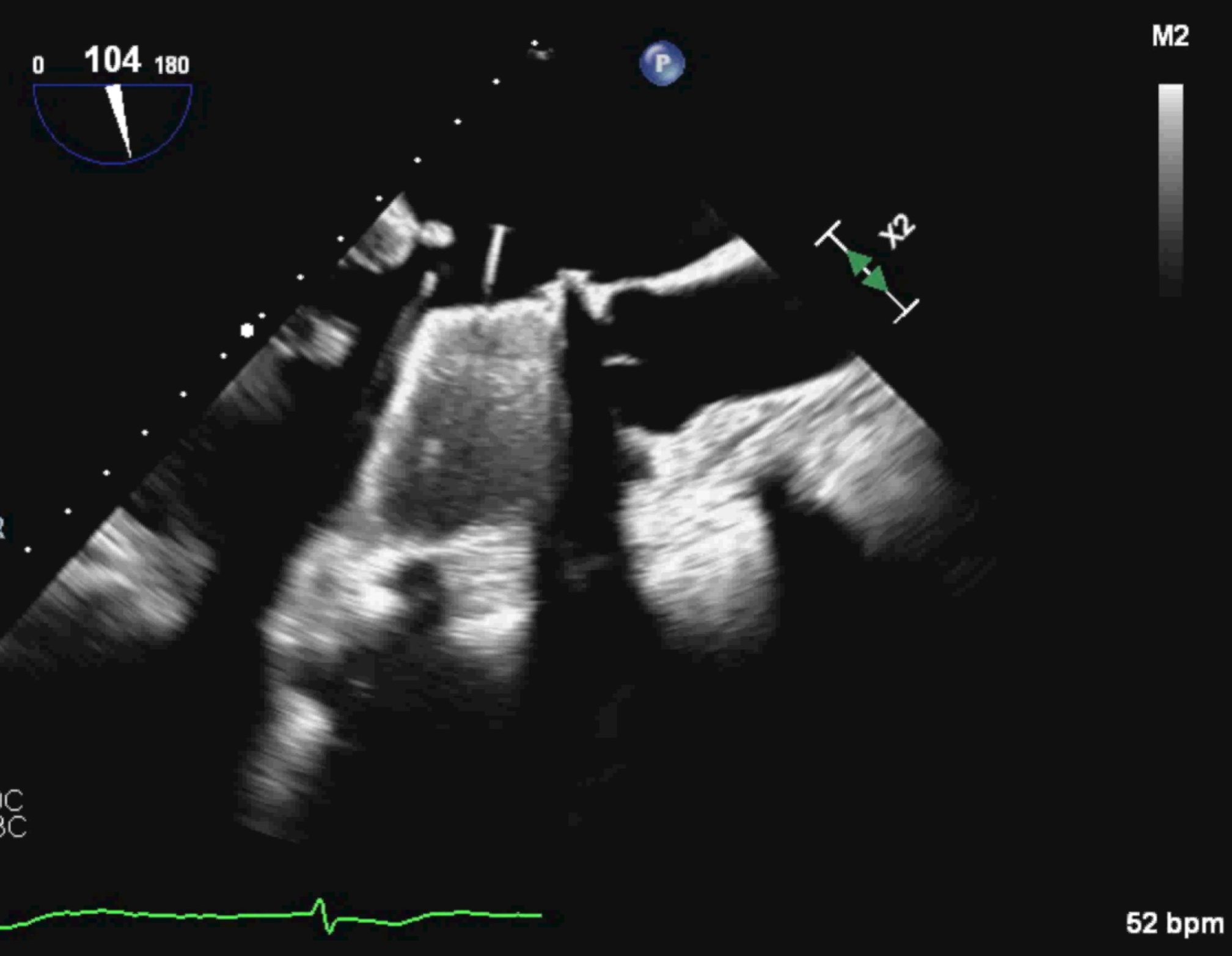
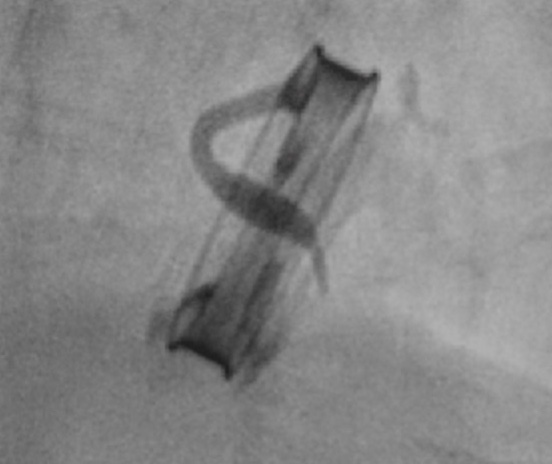
Our patient is a 51 years old woman, with a history of mitral valve replacement, diabetes mellitus and coronary artery disease. She was known to have poor warfarin compliance. Recently she was admitted for heart failure symptoms. Echo showed an intermittently opening prosthesis, which was confirmed by TEE and fluoroscopy. She was discharged after treatment with fibrinolytics. Few months later, she presented to us with right leg claudication. Physical exam showed diminished pulses on the right.
Relevant Test Results Prior to Catheterization
Ankle-brachial index (ABI) confirmed significant peripheral arterial disease (PAD) on the right, with a value of 0.83. The left ABI was 1.03. Pulse volume recording (PVR) measurements showed a pressure drop at the ankle level. A review of her blood tests showed a labile INR trend. There was also poorly controlled diabetes, as reflected by an HbA1C of 9.0%. Angiogram and angioplasty was offered for revascularisation and to determine the cause of her PAD.
Relevant Catheterization Findings
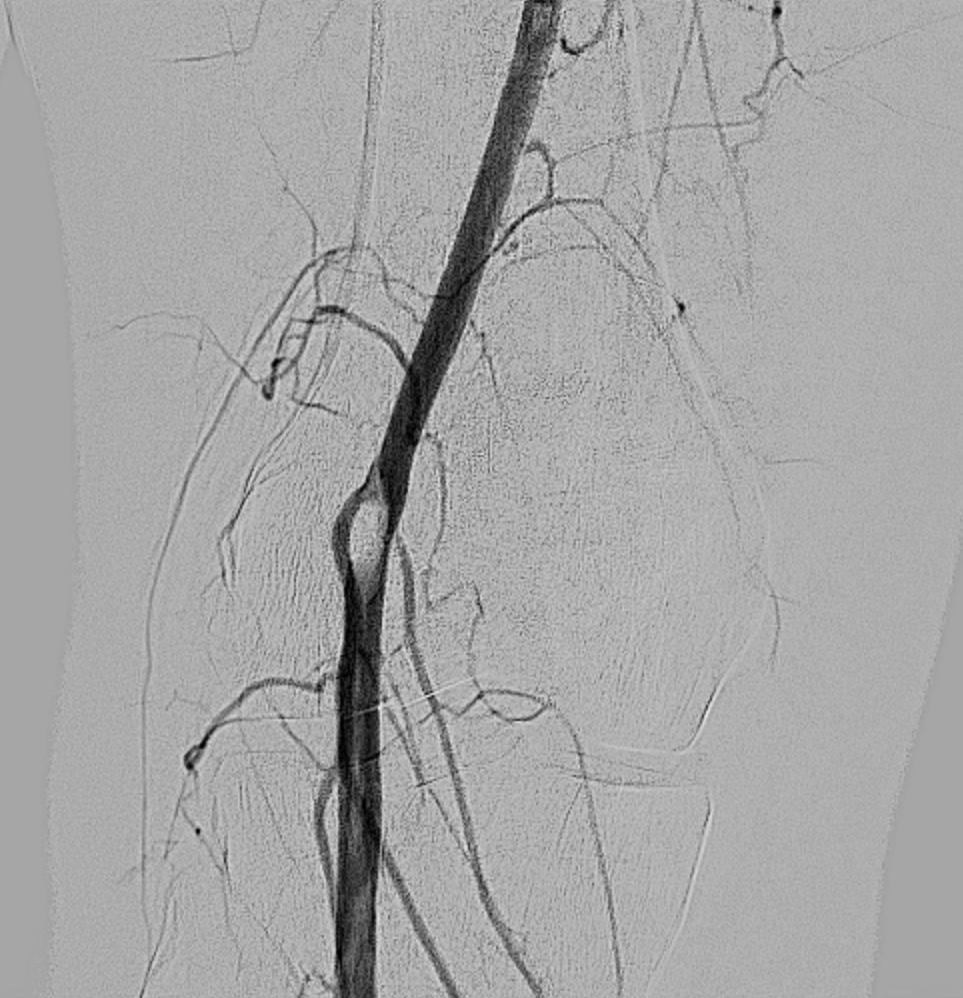
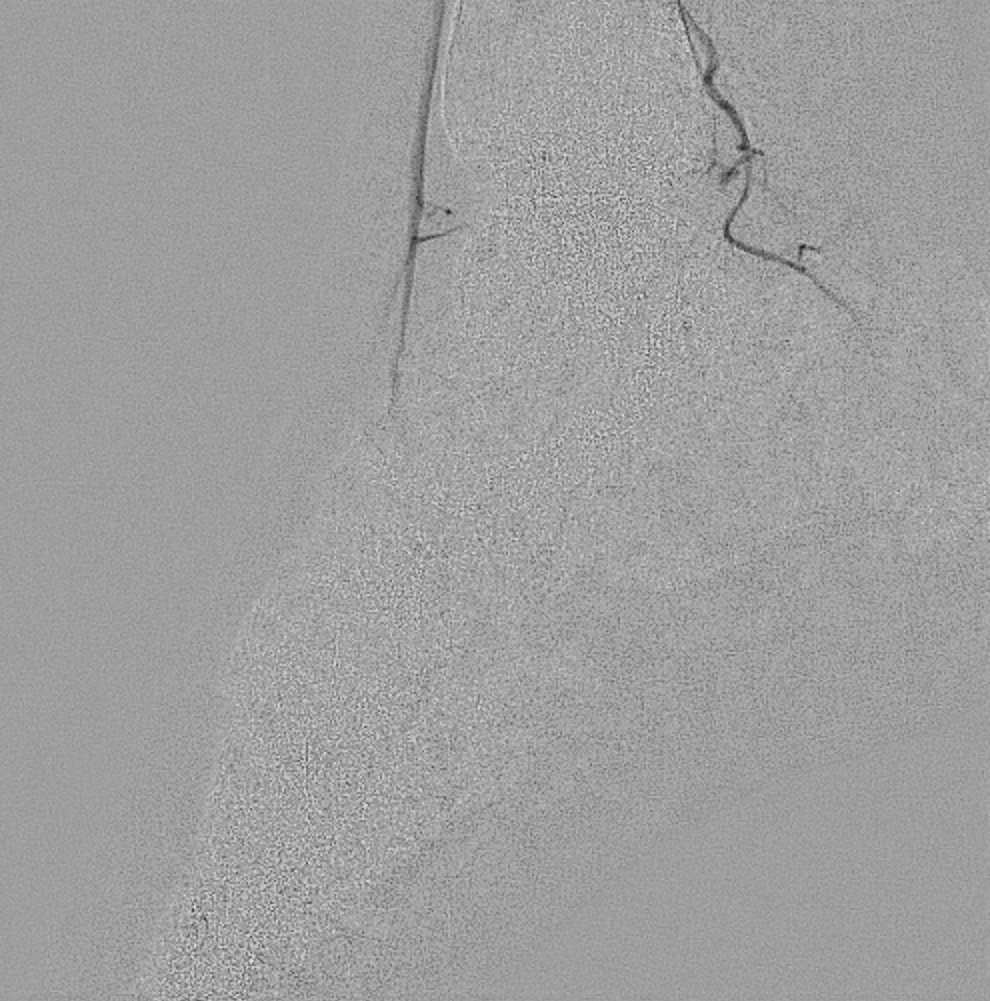
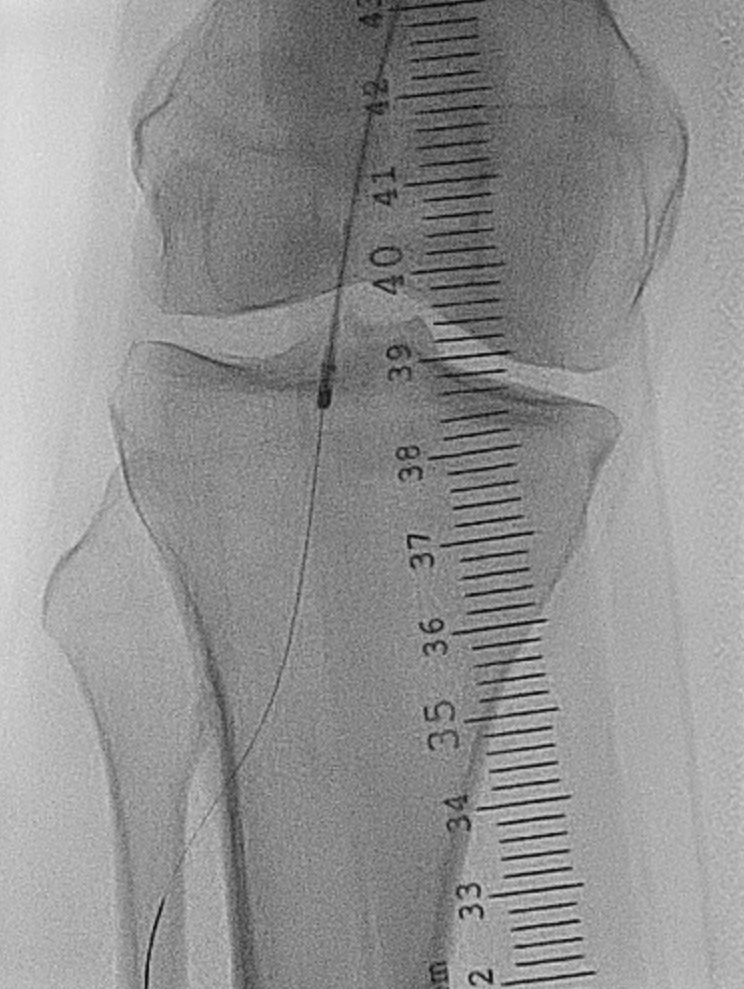
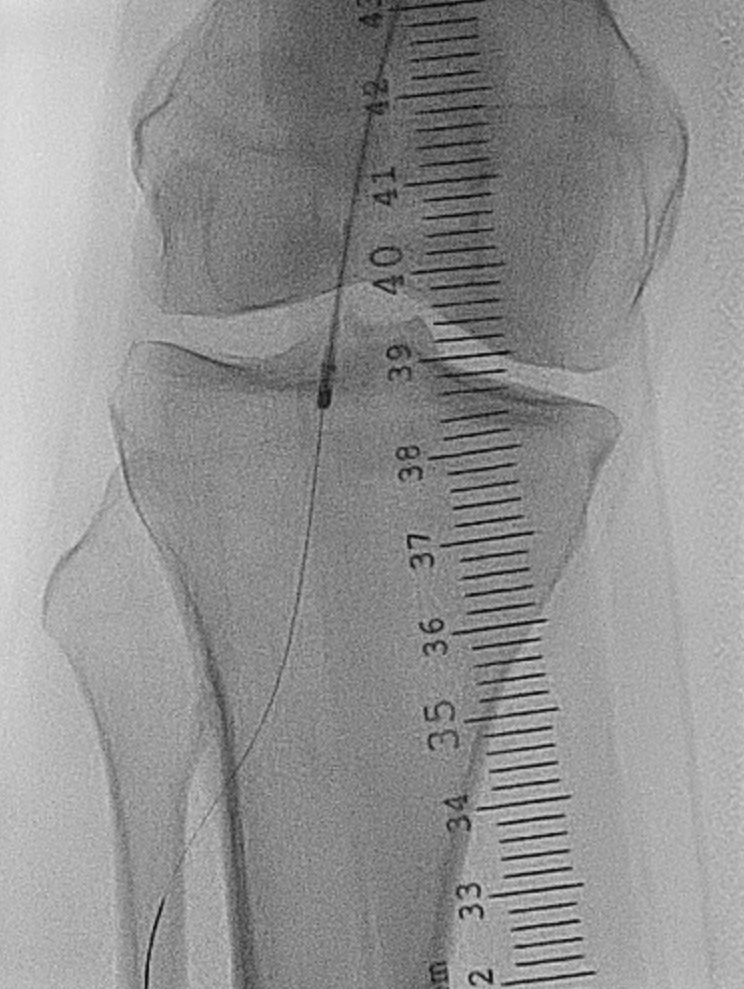
Since the ABI and PVR localised the disease to the popliteal/below-the-knee segment and the left ABI was normal, right leg angiogram was obtained via an ipsilateral antegrade approach. It showed a large organised thrombus at the distal superficial femoral (SFA)/popliteal artery, extending to the anterior tibial (ATA) and tibioperoneal trunk (TPT) bifurcation. There was poor outflow in the anterior tibial and posterior tibial (PTA) arteries, with an incomplete plantar arch.
Interventional Management
Procedural Step
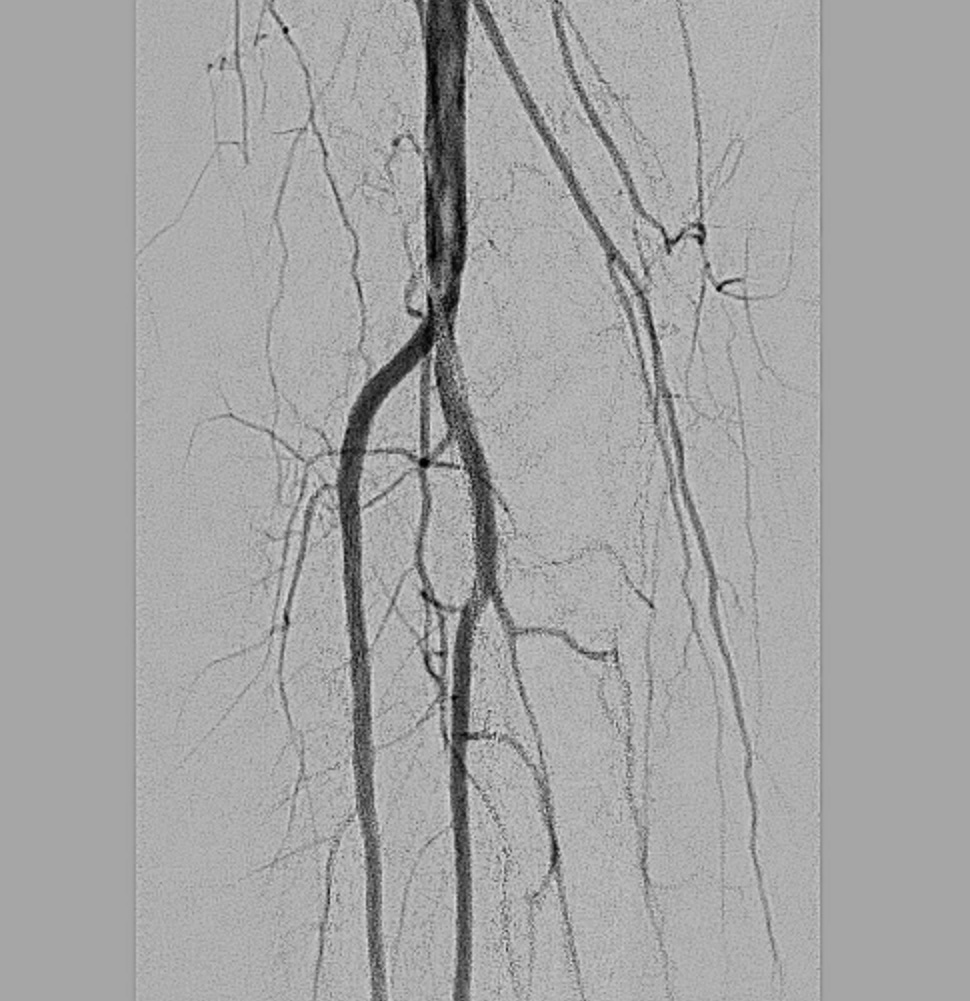
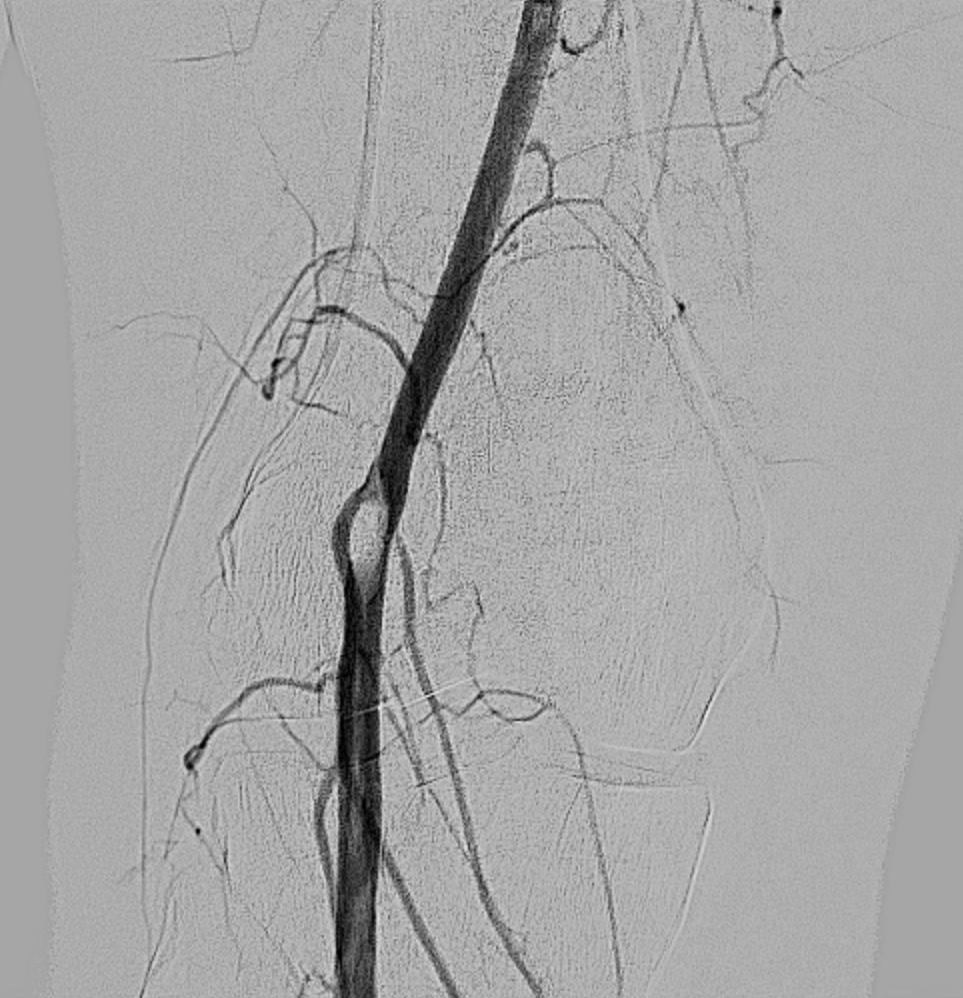
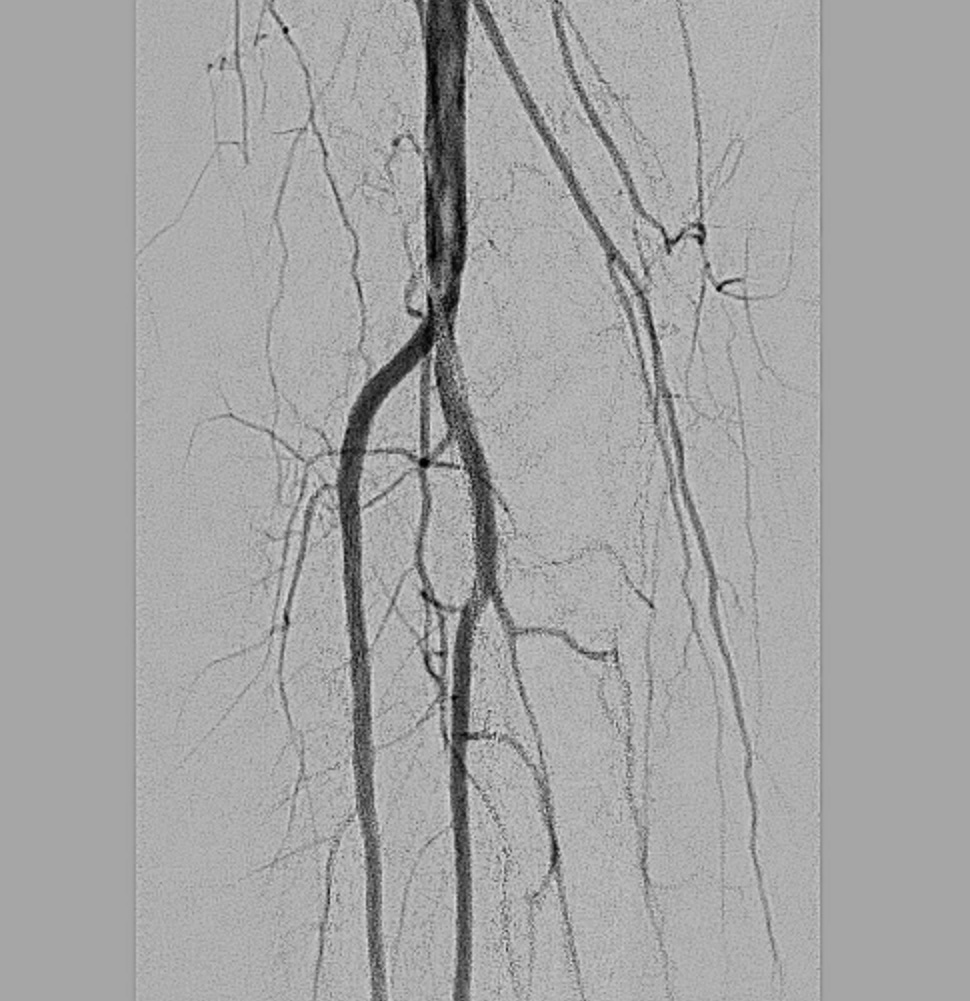
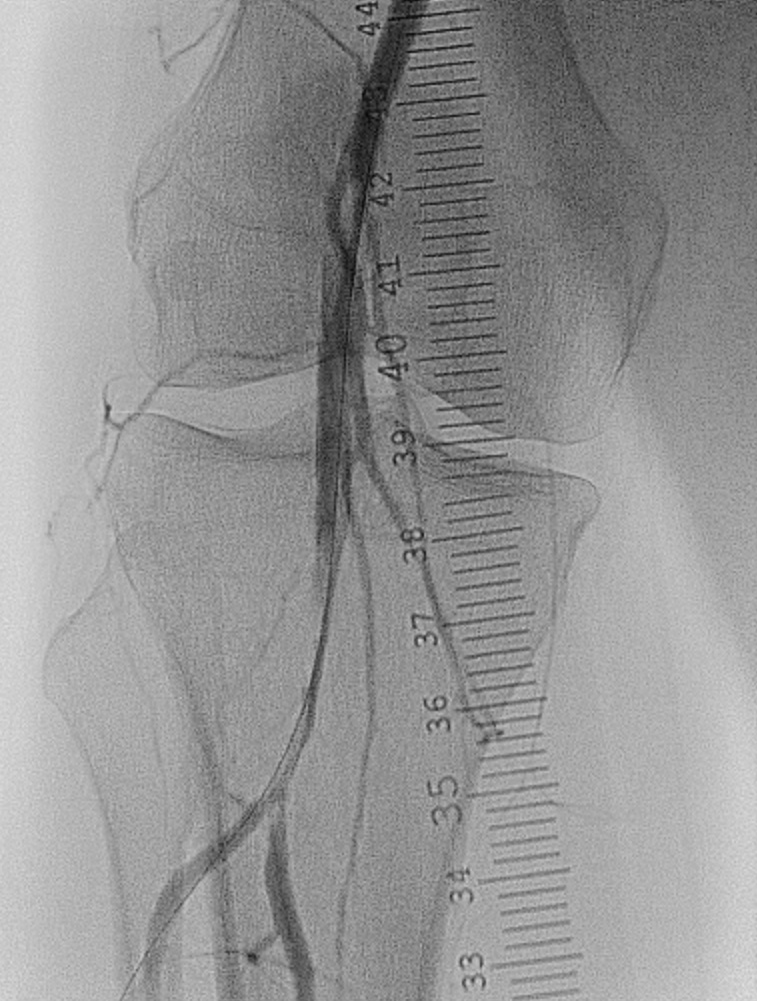
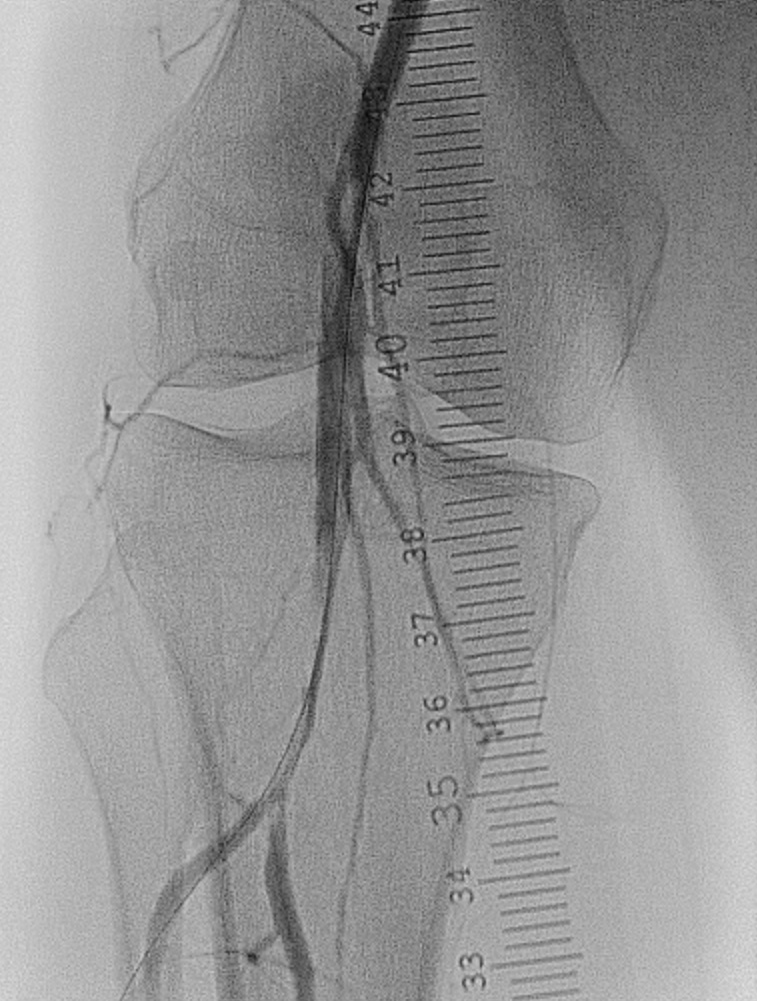
Right common femoral antegrade access was obtained. A 7 Fr, 45 cm Destination sheath (Terumo) was inserted into the mid-SFA, and the lesion was crossed using a 0.018" Glidewire Advantage (Terumo) into the TPT. IVUS (Phillips) was done. It showed a 10cm eccentric thrombus without any plaque, confirming a thromboembolic event rather than local arterial atherosclerosis. In view of this, we decided to first try manual aspiration through a multipurpose guiding catheter (Medtronic), but to no avail. Since we had anticipated preoperatively a need for either thrombectomy or atherectomy based on the patient's history, we then decided to treat the lesion with the Rotarex Rotational Excisional Atherectomy system (BD), which has been approved for both uses. Forward and backward passes were done, but with no improvement. We put our wire into the ATA to try to alter the wire bias, and performed another run. However, the angiogram showed dissection, intramural haematoma and distal extension of the clot into the TPT. Hence we decided not to use Rotarex any further, and to try a clot maceration strategy. A SpiderFX embolic protection device (Medtronic) was placed into the PTA, and a 5.0 mm x 100 mm balloon was deployed. Filling defects were still seen despite improvement in flow. There was no choice but to stent the distal SFA-popliteal segment with a Supera 6.5 mm x 120 mm stent (Abbott). The final angiogram showed a good straight line flow, 3 vessel run off and a complete plantar arch.


Case Summary
Our case illustrates the importance of careful angiographic and IVUS examination to determine the etiology and the best treatment strategy for each PAD patient. It also demonstrates IVUS is essential in peripheral interventions. We should be well acquainted too with the commercially available technologies to make sure procedures are time and cost efficient. Bailout plans should be formulated. Lastly, when stenting in the femoro-popliteal segment (e.g. across the knee joint) is unavoidable, one should take into account the clinical evidence to ensure a good stent patency rate and minimise the chance of stent fracture at the same time.


