Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-140
Retrieval of a Deformed Stent in a Case of STEMI
By Ricky Wang Hei Leung, Frankie Chor Cheung Tam
Presenter
Ricky Wang Hei Leung
Authors
Ricky Wang Hei Leung1, Frankie Chor Cheung Tam1
Affiliation
Queen Mary Hospital, Hong Kong, China1,
View Study Report
TCTAP C-140
Coronary - Complication Management
Retrieval of a Deformed Stent in a Case of STEMI
Ricky Wang Hei Leung1, Frankie Chor Cheung Tam1
Queen Mary Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Our patient is a 73 year-old female with a history of hypertension, managed by multiple anti-hypertensives, and rheumatoid arthritis, treated with DMARDs. She was admitted for a STEMI.
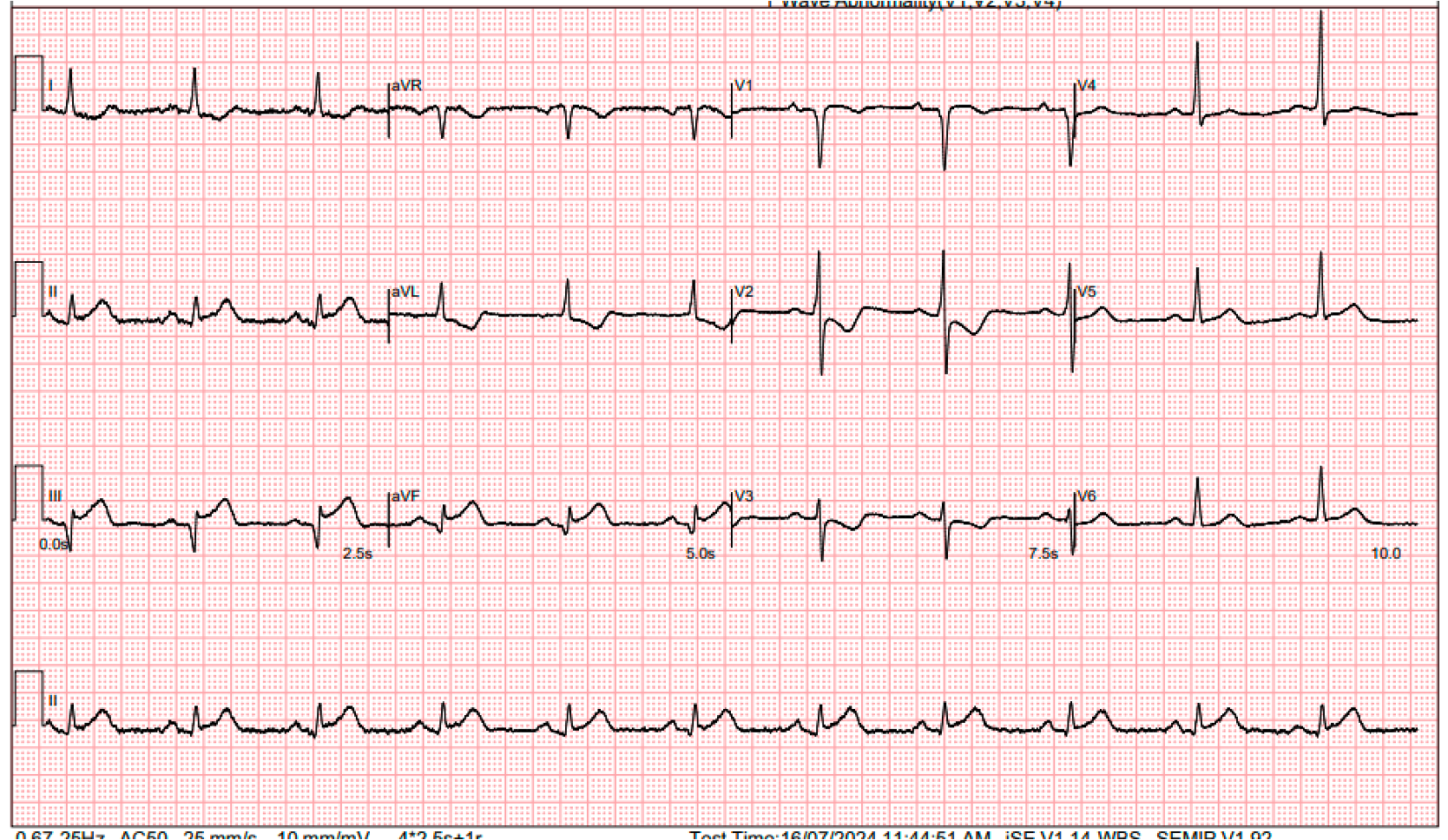
She presented with acute chest pain for 3 hours. In the emergency department, an ECG revealed sinus rhythm with inferior ST elevations. She was still in active chest pain. Physical exam was otherwise unremarkable.
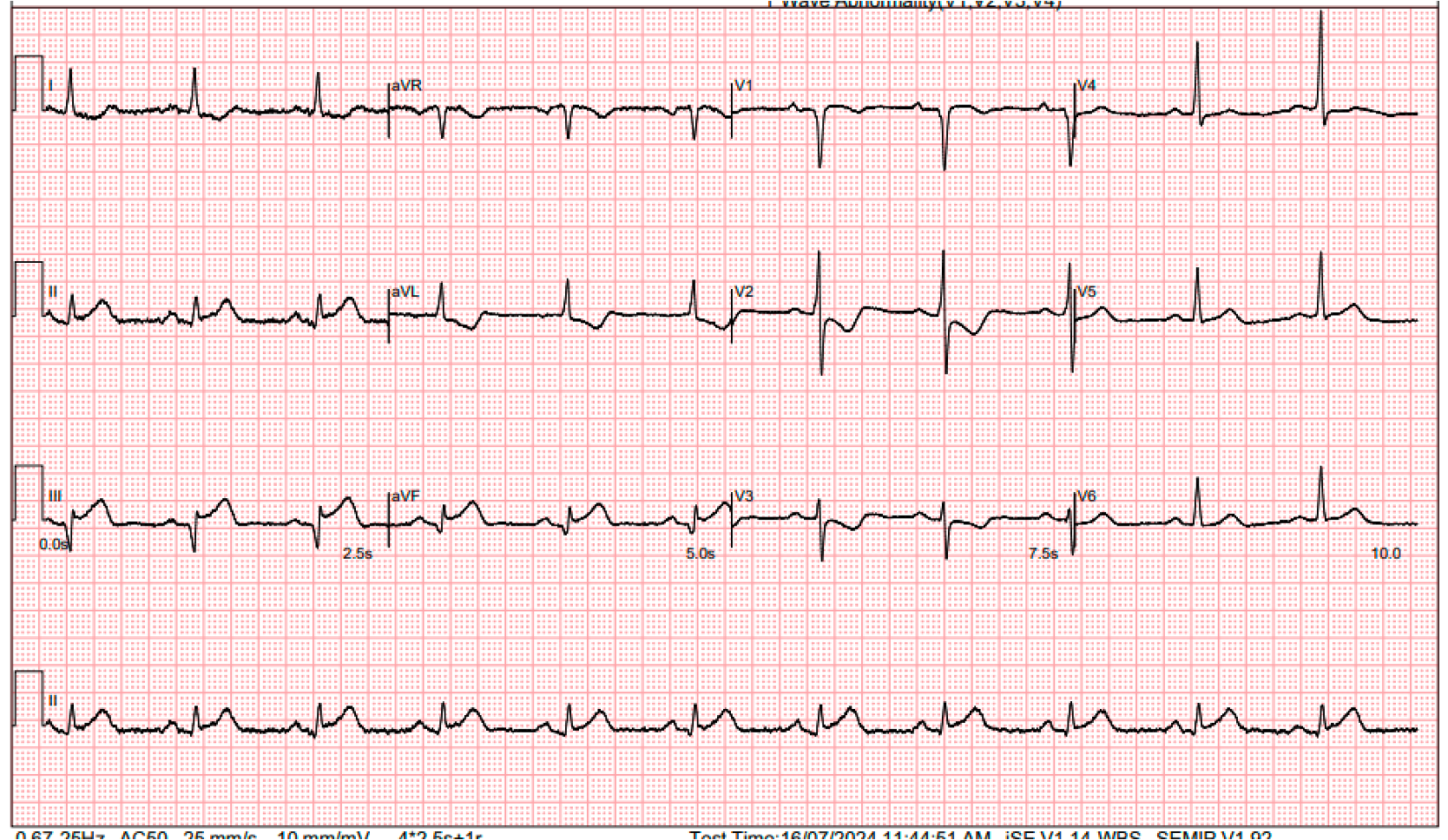
She presented with acute chest pain for 3 hours. In the emergency department, an ECG revealed sinus rhythm with inferior ST elevations. She was still in active chest pain. Physical exam was otherwise unremarkable.
Relevant Test Results Prior to Catheterization
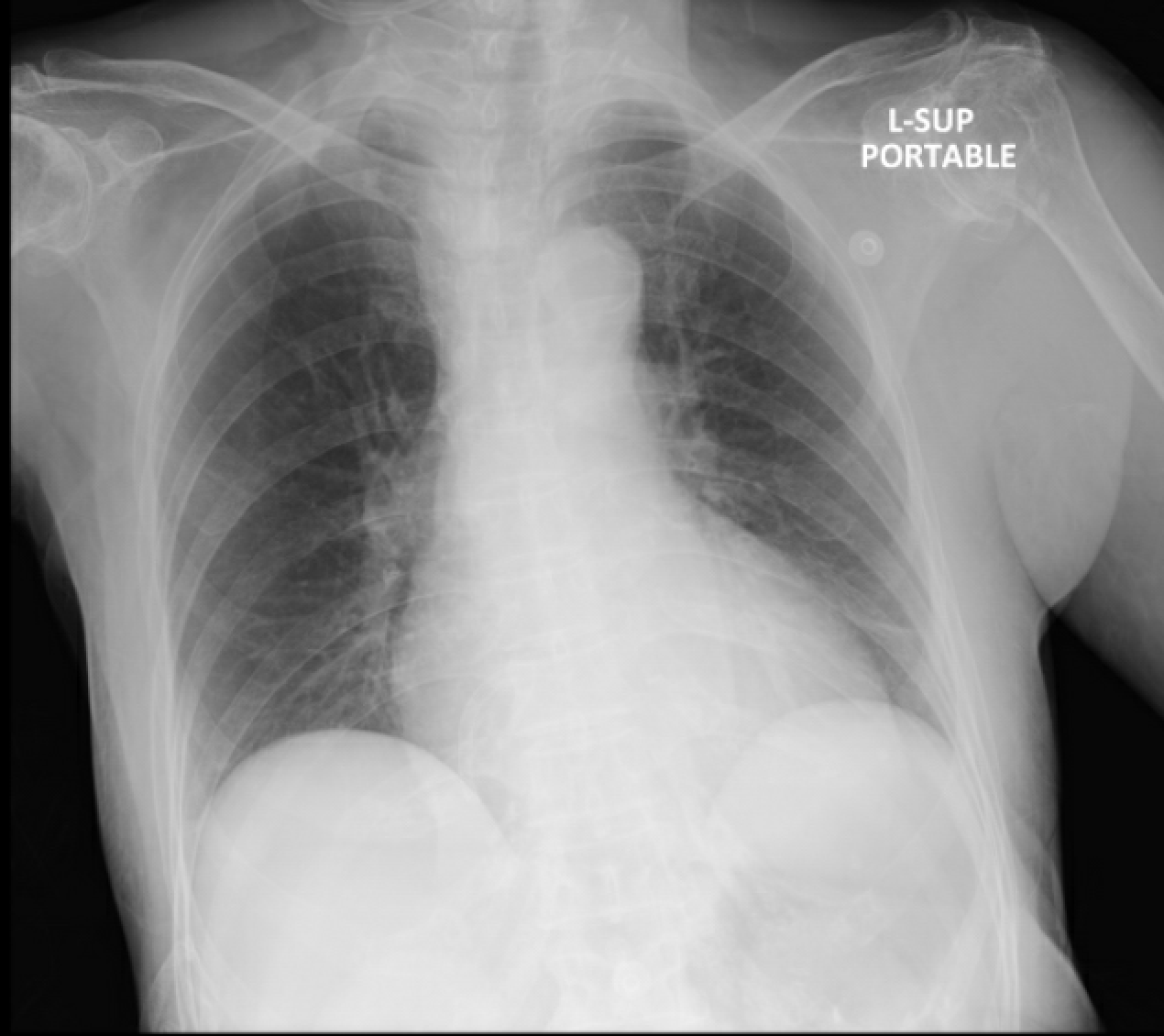
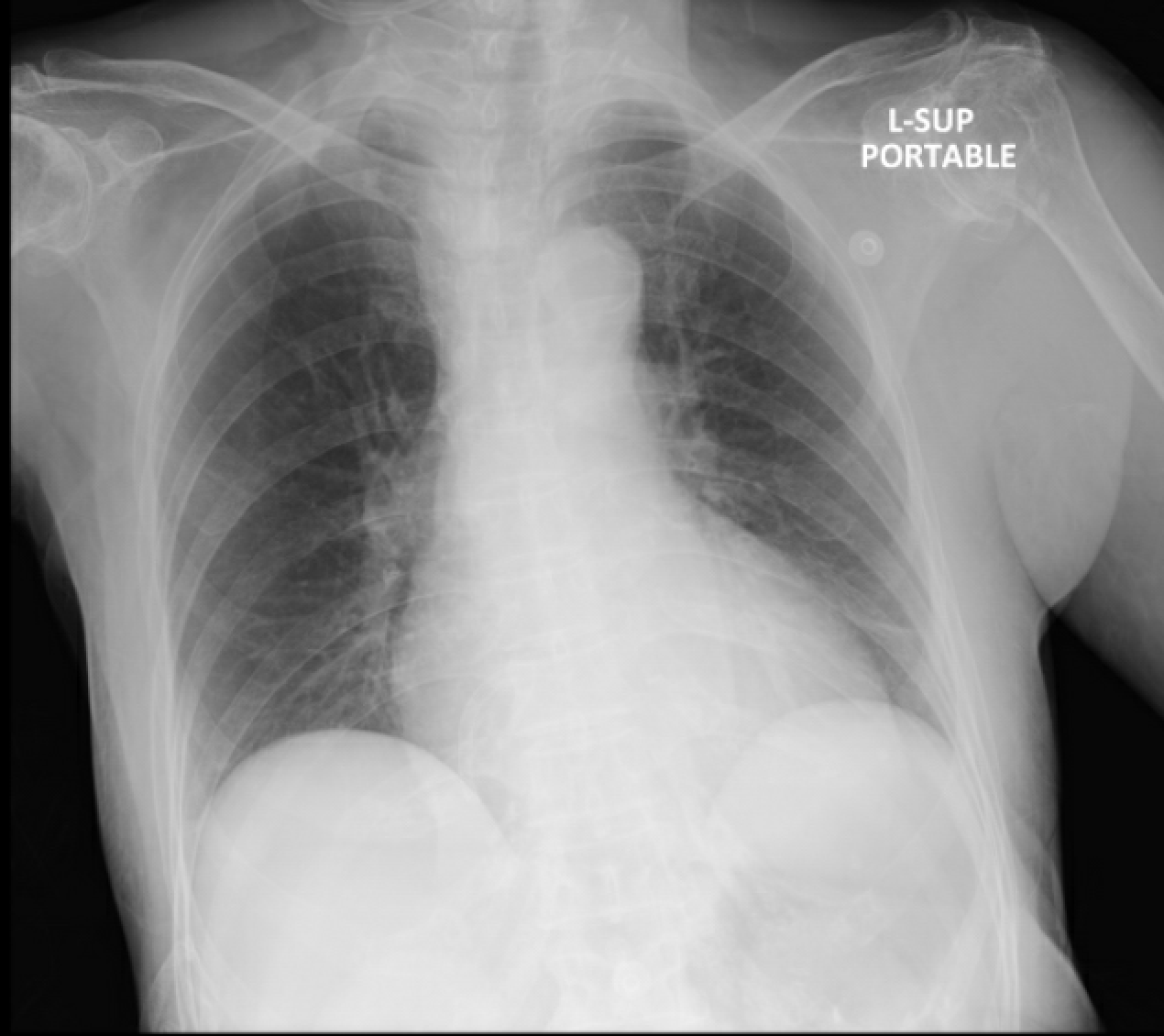
In the emergency department, an ECG revealed sinus rhythm with inferior ST elevations. A bedside echocardiogram indicated an impaired LVEF of 40%, with inferior hypokinesia. There was no pericardial effusion or signs of aortic dissection, and hemodynamics were stable. CXR showed clear lung fields. We proceeded with primary PCI.
Relevant Catheterization Findings
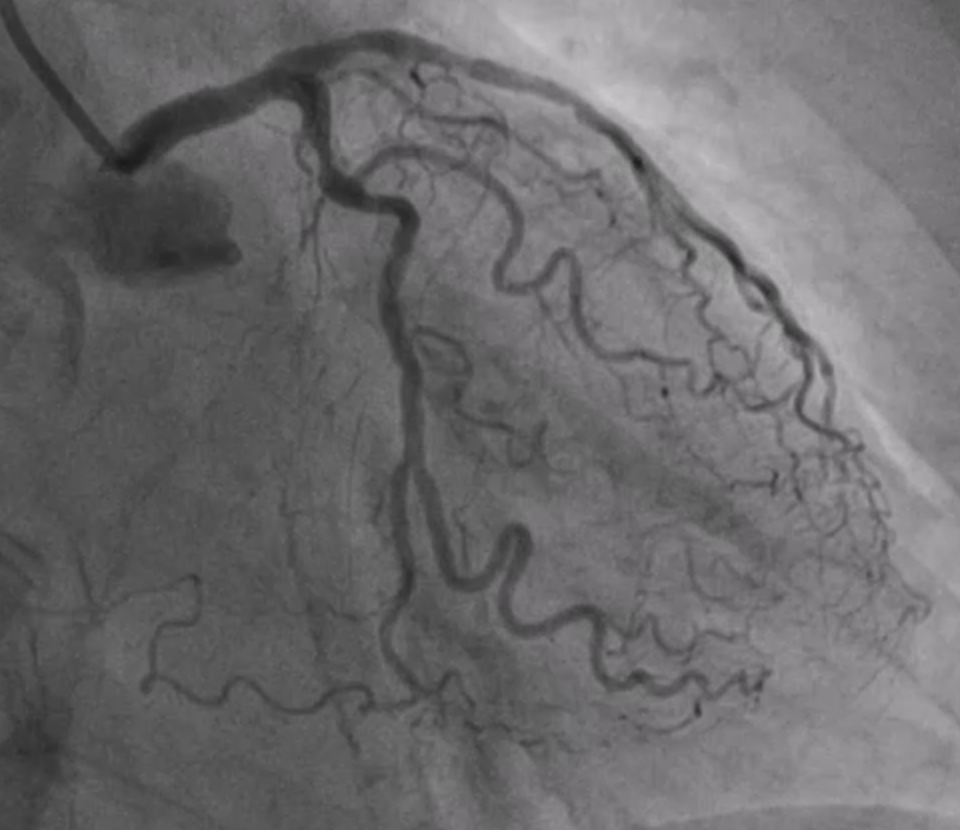
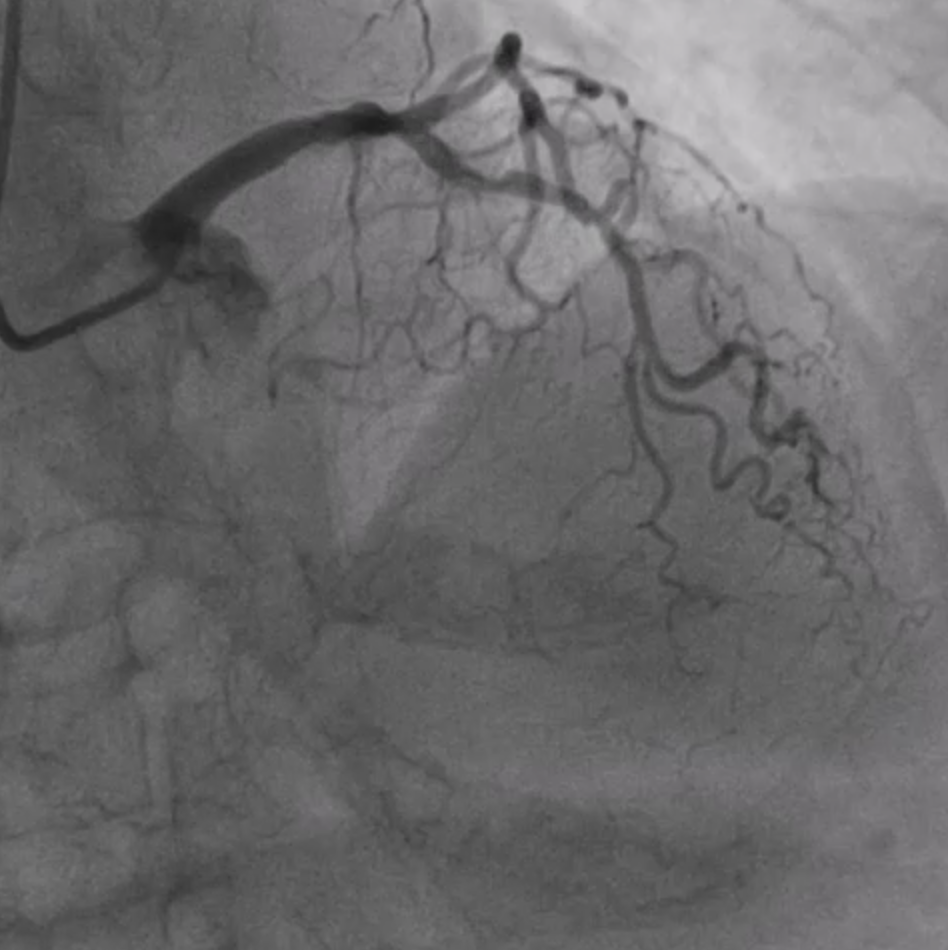
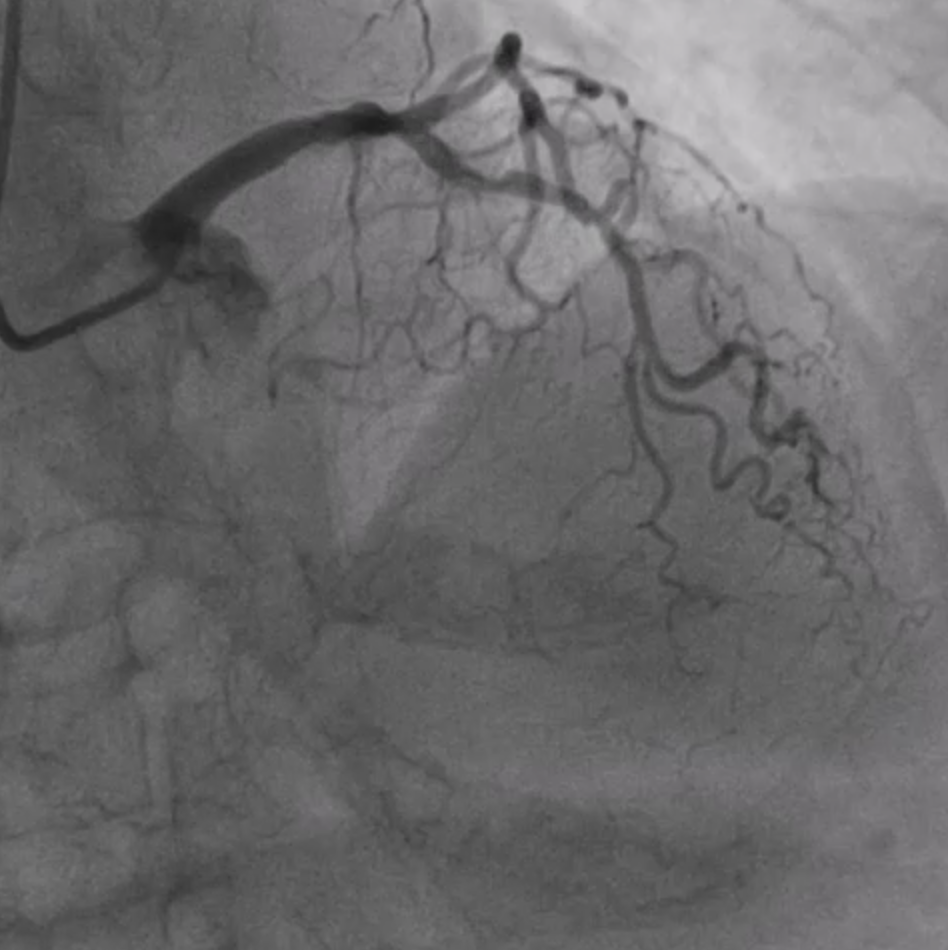
The coronary angiogram, performed via right radial access, revealed a mid-LAD chronic total occlusion (CTO), moderate stenosis in the proximal LCX, and critical stenosis in the mid-RCA. The RCA flow was TIMI 2. We decided to perform PCI on the RCA using the same access route.
Interventional Management
Procedural Step
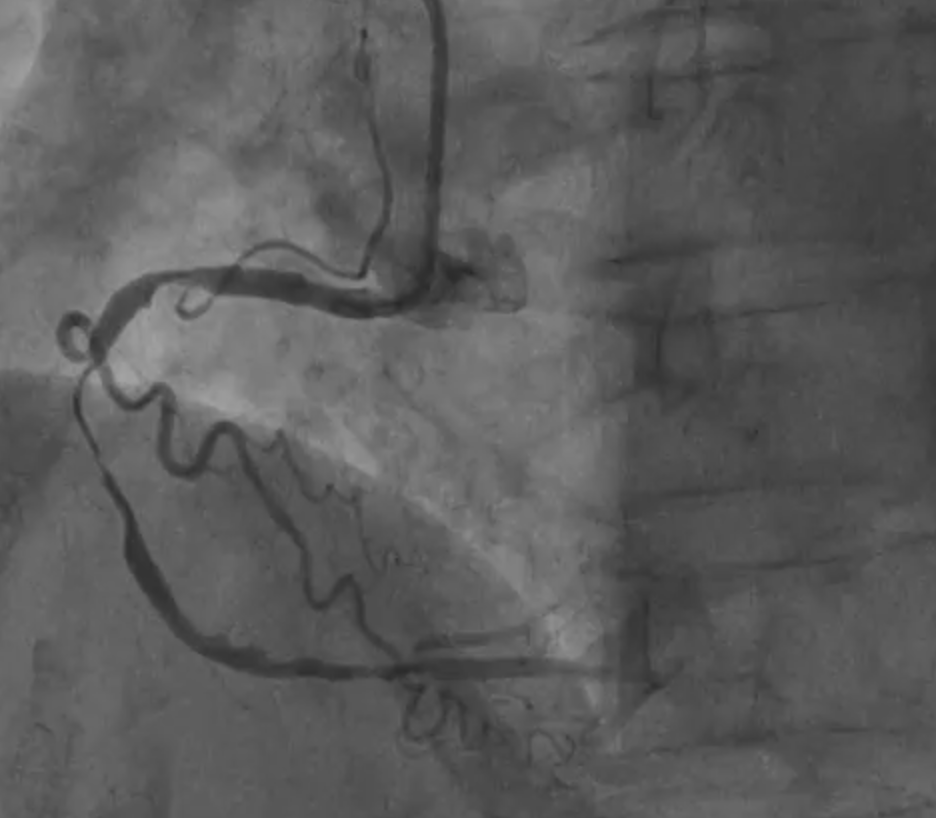
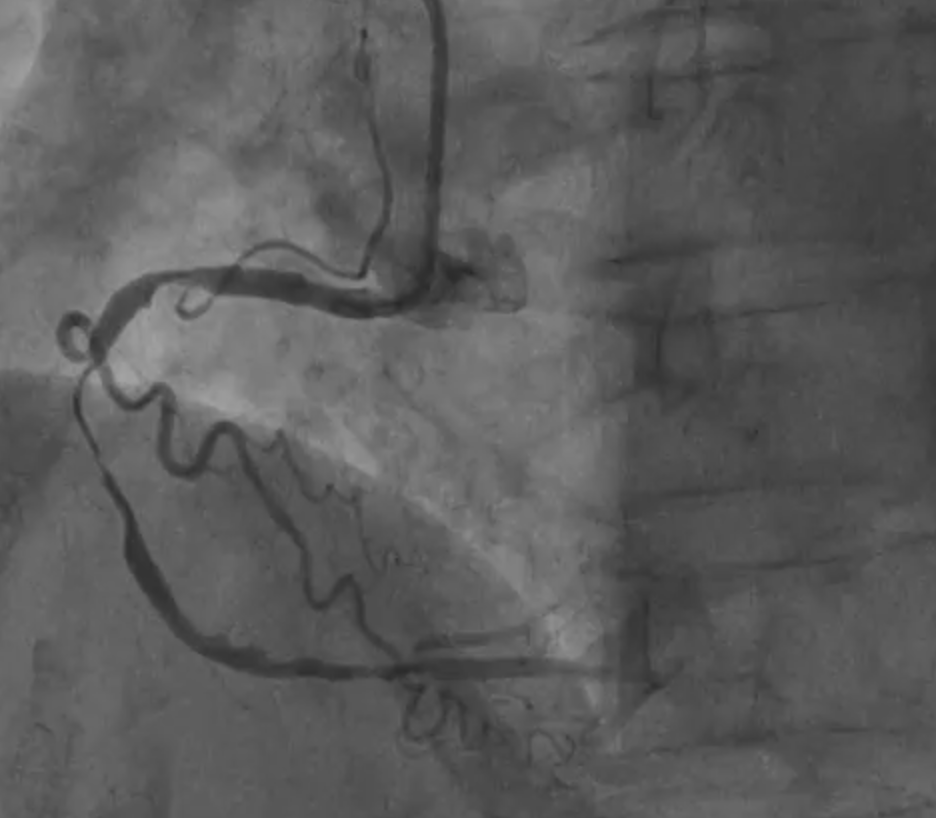
We proceeded with PCI using a 6Fr JR4 guiding catheter. Mid RCA lesions were predilated with an SC 2.0. IVUS revealed severe luminal stenosis and thrombus in the mRCA, along with significant calcified stenosis in the pRCA.
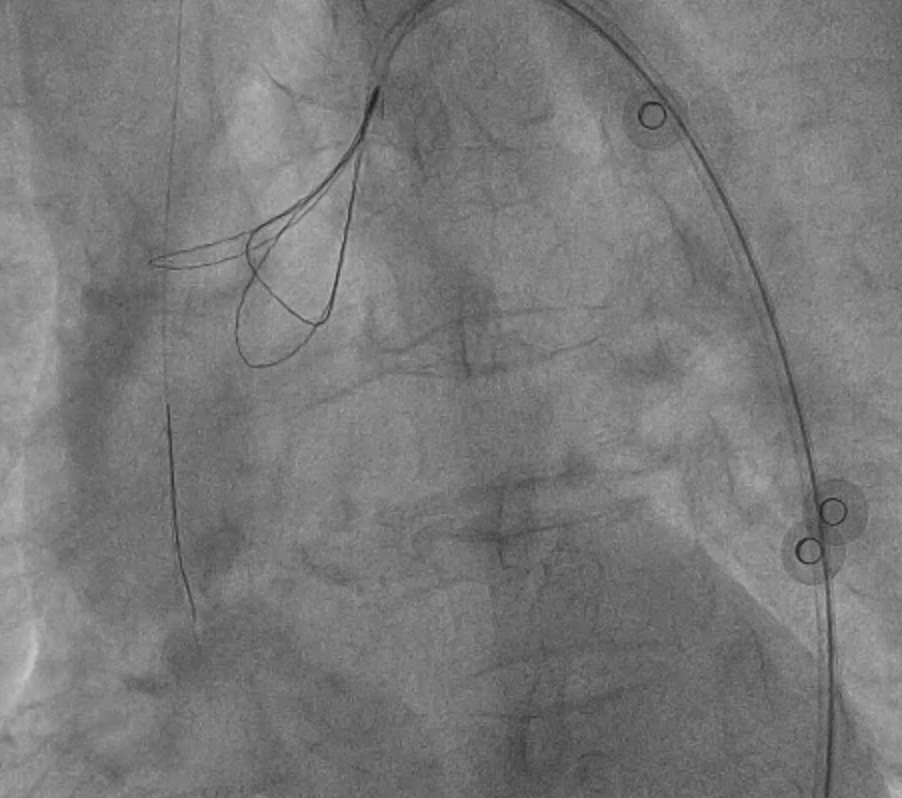
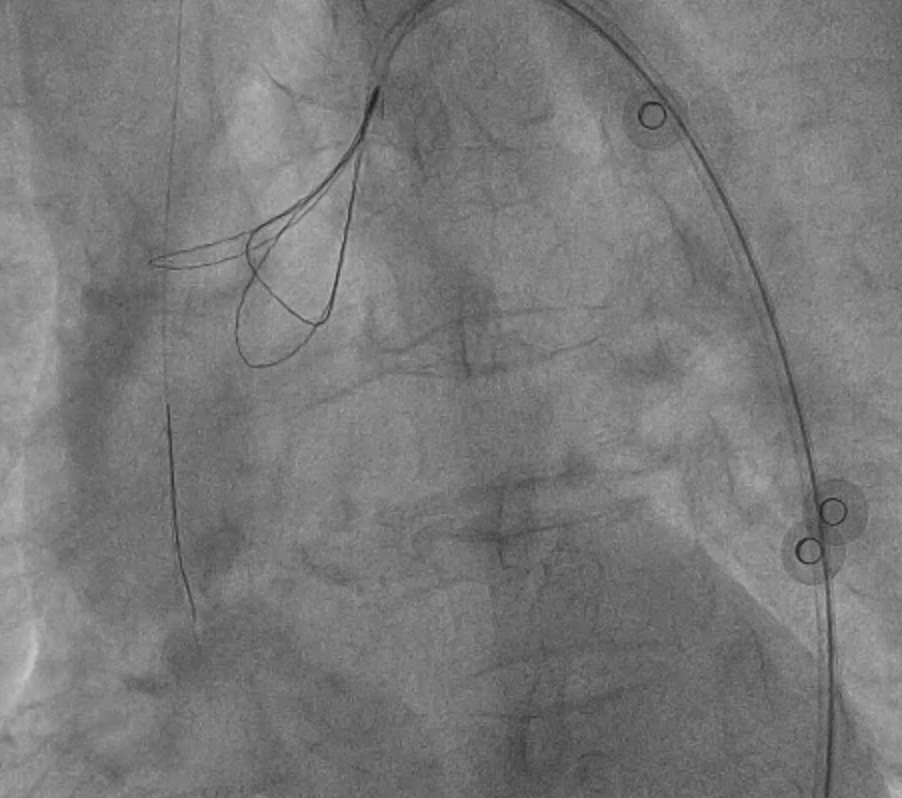
Further predilatation was performed with an NC 3.0, but this was complicated by no-relow. The patient's hemodynamics deteriorated, with bradycardia and hypotension. We administered different medications, followed by temporary pacing lead insertion and penumbra for thrombus aspiration.
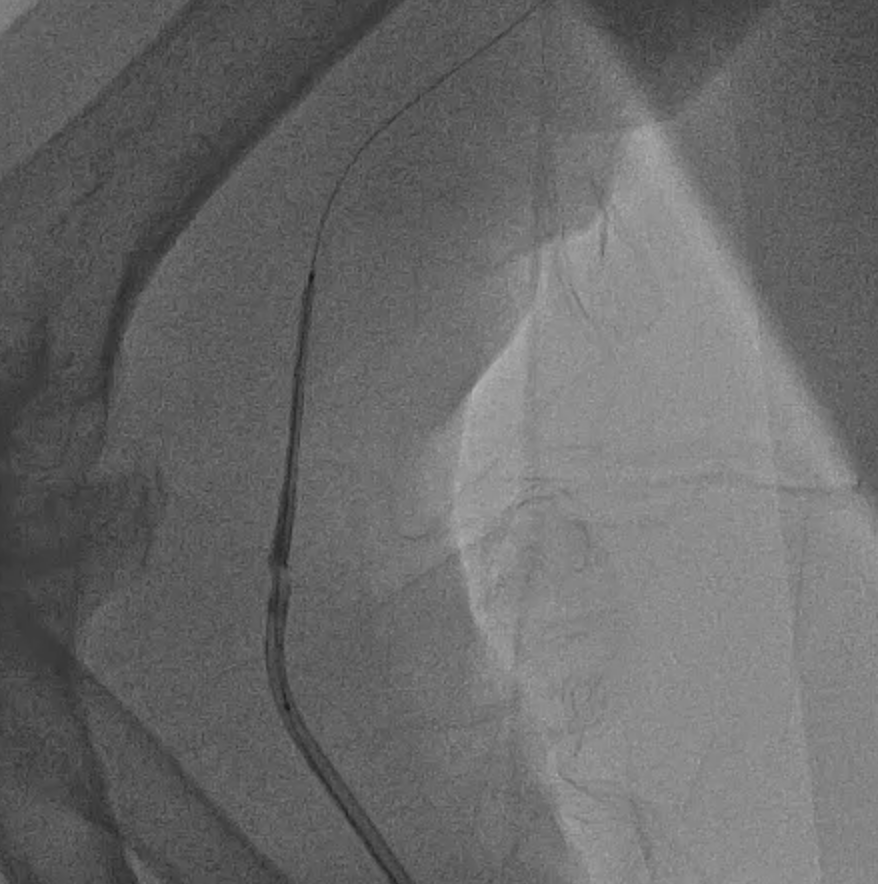
We attempt to pass a 50 mm long stent to cover both lesions, but encountered difficulty due to pRCA calcification. Manipulation with the guiding catheter led to partial stent dislodgement from the balloon.
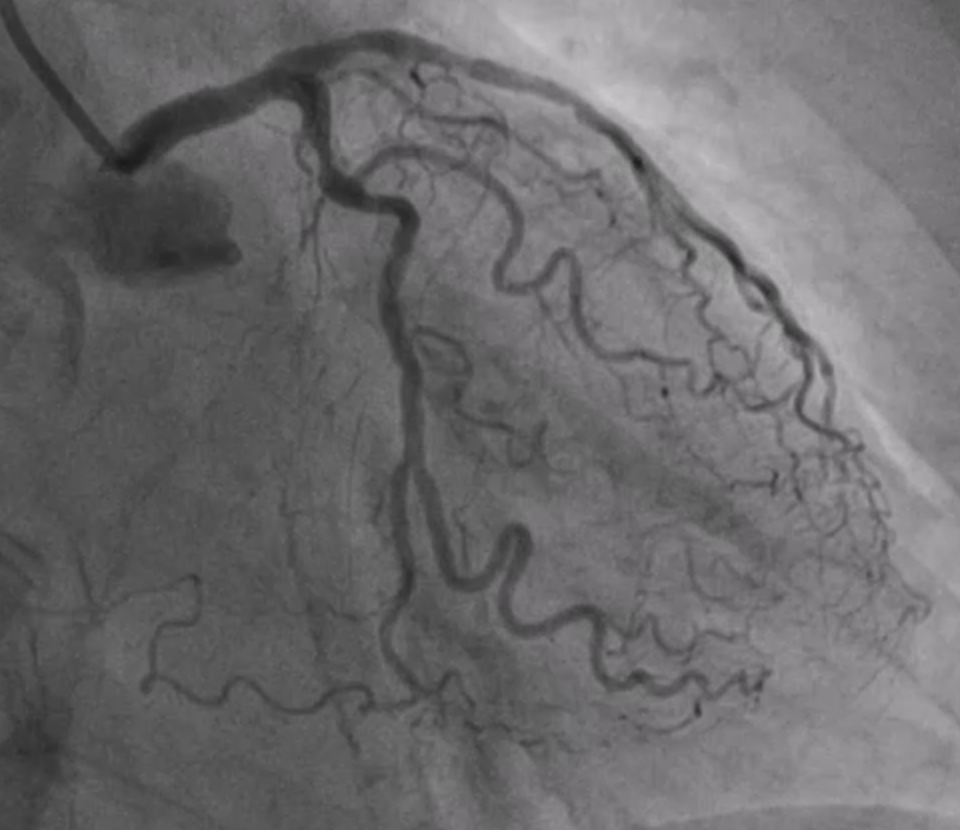
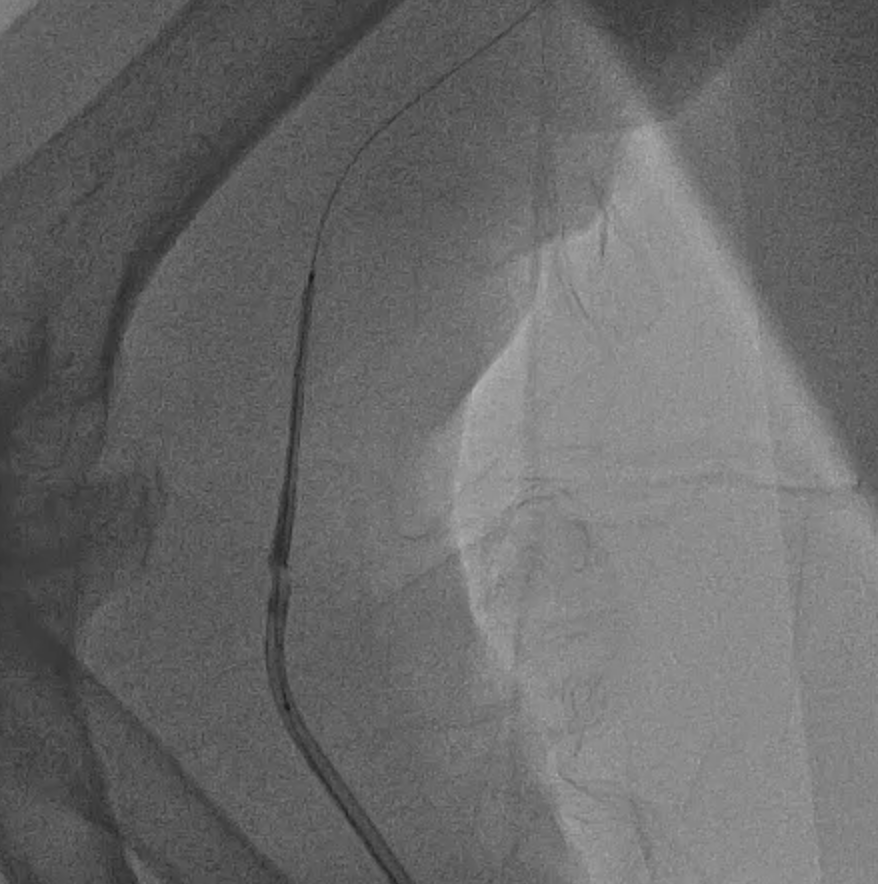
Given the unstable hemodynamics, we retracted the system to the brachial artery and established a new setup via the right femoral. Instead of a long stent, we implanted two shorter stents, with the assistance of a guide extension. After successful deployment, we peformed post-dilation.
Then we proceeded to retrieval of the dislodged stent. We pushed the old system back to the aorta and we snared the wire with ENsnare. The proximal portion of the stent was significantly deformed and could not go into the JR4 guiding catheter from femoral side. We tried different methods including using a larger and longer sheath, manipulations to optimise alignment, changing to a different snare but we still failed. At last, we successfully retrieved the stent with the use of biopsy forceps.

Further predilatation was performed with an NC 3.0, but this was complicated by no-relow. The patient's hemodynamics deteriorated, with bradycardia and hypotension. We administered different medications, followed by temporary pacing lead insertion and penumbra for thrombus aspiration.
We attempt to pass a 50 mm long stent to cover both lesions, but encountered difficulty due to pRCA calcification. Manipulation with the guiding catheter led to partial stent dislodgement from the balloon.
Given the unstable hemodynamics, we retracted the system to the brachial artery and established a new setup via the right femoral. Instead of a long stent, we implanted two shorter stents, with the assistance of a guide extension. After successful deployment, we peformed post-dilation.
Then we proceeded to retrieval of the dislodged stent. We pushed the old system back to the aorta and we snared the wire with ENsnare. The proximal portion of the stent was significantly deformed and could not go into the JR4 guiding catheter from femoral side. We tried different methods including using a larger and longer sheath, manipulations to optimise alignment, changing to a different snare but we still failed. At last, we successfully retrieved the stent with the use of biopsy forceps.

Case Summary
The patient was transferred to the CCU post-procedure, and vasopressors and inotropes were successfully weaned off the next day.
In conclusion, retrieving a deformed stent can be challenging, especially in a STEMI scenario with unstable hemodynamics and potential complications like no-reflow. Familiarity with various tools, including snares and biopsy forceps, is essential for managing such complex cases effectively.
In conclusion, retrieving a deformed stent can be challenging, especially in a STEMI scenario with unstable hemodynamics and potential complications like no-reflow. Familiarity with various tools, including snares and biopsy forceps, is essential for managing such complex cases effectively.


