Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-108
Breaking Through the Calcified Neoatherosclerosis
By Han Bing Chow
Presenter
Han Bing Chow
Authors
Han Bing Chow1
Affiliation
Tuen Mun Hospital, Hong Kong, China1,
View Study Report
TCTAP C-108
Coronary - Complex PCI - In-Stent Restenosis
Breaking Through the Calcified Neoatherosclerosis
Han Bing Chow1
Tuen Mun Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
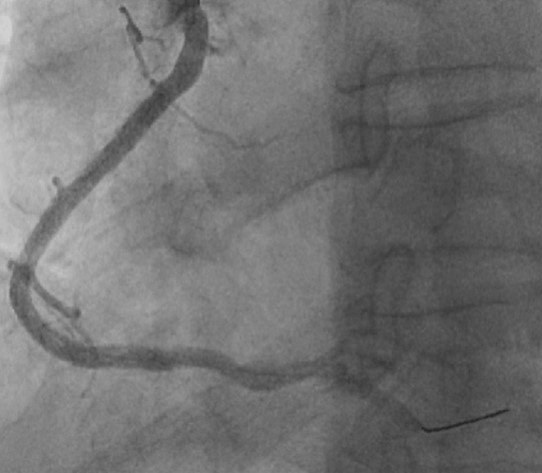
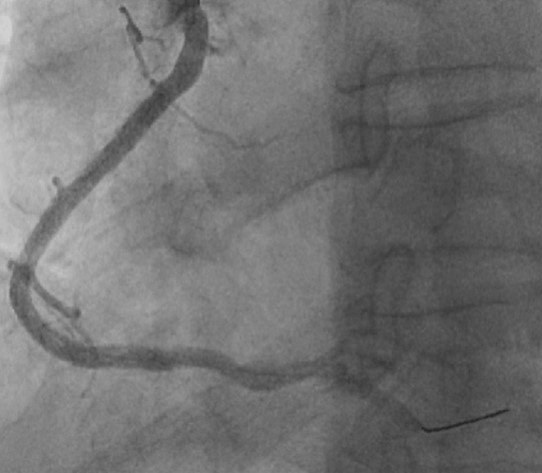
We report an 62-year-old gentleman with history of hypertension, diabetes mellitus, dyslipidemia and history of PTCA to LAD and RCA with DES in 1997. He underwent a computed tomography coronary angiography (CTCA) examination for stable angina which revealed severe in stent restenosis with multiple calcified plaques. Guideline directed medical therapies were optimized. After family conference for mode of revascularization, committed to high-risk percutaneous coronary intervention (PCI) approach.


Relevant Test Results Prior to Catheterization
Echocardiogram
Relevant Catheterization Findings
LMS: Calcified. Minor disease.
Interventional Management
Procedural Step
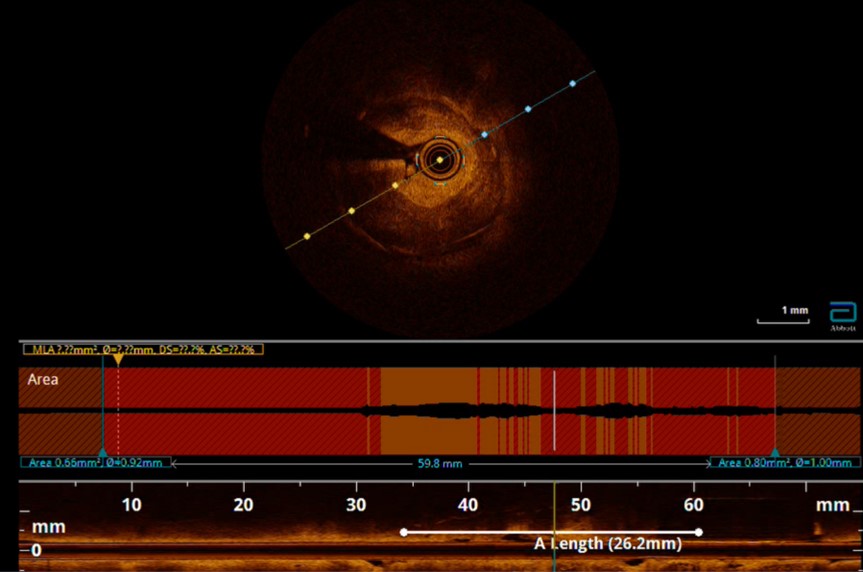
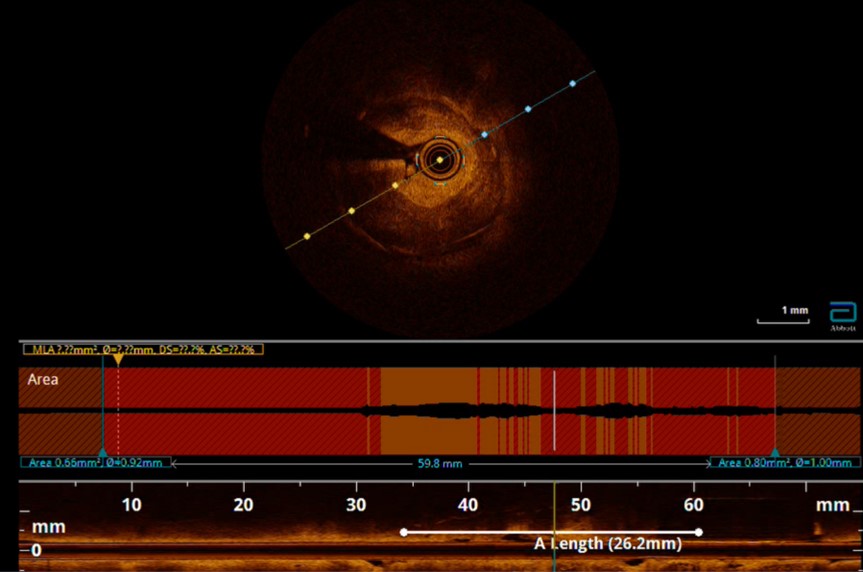
Contralateral injection approach PCI. Difficulty in wiring occluded LAD segment with Fielder XT-A and Gaia Next 2nd despite with Corsair Pro XS support. Wiring of LAD was successful after escalation to Gaia Next 3rd. After failed attempts to deliver microcatheter, 0.9mm excimer coronary laser atherectomy (ELCA) was performed for 12 cycles (60/80, blood medium) followed by predilatation with Sapphire 3 0.85/10 and Sapphire 1.5/10. Delivery of the microcatheter over the lesion was then successful. Gaia Next 3rd wire then exchanged to NS Runthrough. Predilatation of the lesion with NC Sapphire 2.0/15 and NC Trek 2.5/15, however noted balloon severe underexpansion. Optical Coherent Tomography (OCT) performed with Dragonfly Opstar showed severely calcified neoatherosclerosis. Four runs of 1.5mm burr rotational atherectomy was then performed at 180,000rpm, followed by another three runs of 1.75mm burr rotablation at 180,000rpm. We then deployed DES Xcience Skypoint 2.5/38 to m-dLAD and another DES 3.5/28 Xcience Skypoint to the LM-pLAD region due to dissection flap evident in OCT. Lesion segment between DES was subsequently prepared with intravascular lithotripsy (IVL) 3.0/12 for 80 shocks and NC Pantera Leo 3.0/15 before deploying Xcience Skypoint 3.0/15. DES optimization was then performed under OCT guidance. Finally, DCB 3.0/20 Sequent Please Neo DCB was deployed to mLAD ISR for 60 seconds. Staged PCI to RCA was performed with IVL followed by DES deployment under imaging guidance.


Case Summary
Despite recent breakthroughs in treatment, ISR remains the most common cause of stent failure, accounting for 5–10% of all PCI procedures in contemporary clinical practice with increasing volume and procedure complexity. In addition to identifying mechanical factors that predispose to ISR, intracoronary imaging; OCT in particular provides unique insights into the tissue (ISR substrate) inside the stent to predict response to different therapeutic approaches. For ISR in the setting of calcification and stent underexpansion, multiple calcium modification techniques may be required to modify calcium and facilitate stent expansion.


