Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-103
Shattered Barriers: Upfront Rotatripsy in Patient With Refractory In-Stent Restenosis
By I Gede Sumantra, Rajinikanth Rajagopal, Billal Patel, Paula Mota
Presenter
I Gede Sumantra
Authors
I Gede Sumantra1, Rajinikanth Rajagopal2, Billal Patel2, Paula Mota2
Affiliation
Bandung Adventist Hospital, Indonesia1, Gleneagles JPMC, Brunei Darussalam2,
View Study Report
TCTAP C-103
Coronary - Complex PCI - In-Stent Restenosis
Shattered Barriers: Upfront Rotatripsy in Patient With Refractory In-Stent Restenosis
I Gede Sumantra1, Rajinikanth Rajagopal2, Billal Patel2, Paula Mota2
Bandung Adventist Hospital, Indonesia1, Gleneagles JPMC, Brunei Darussalam2,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 63-year-old man presented with worsening angina pectoris. He had a history of PCI to the RCA in 2007 with three DES placements and multiple episodes of ISR in the RCA in 2010, 2012, 2022, and most recently in 2023. The latest PCI was treated with IVL, a cutting balloon, and DEBs. His risk factors include diabetes mellitus, hypertension, and dyslipidemia.
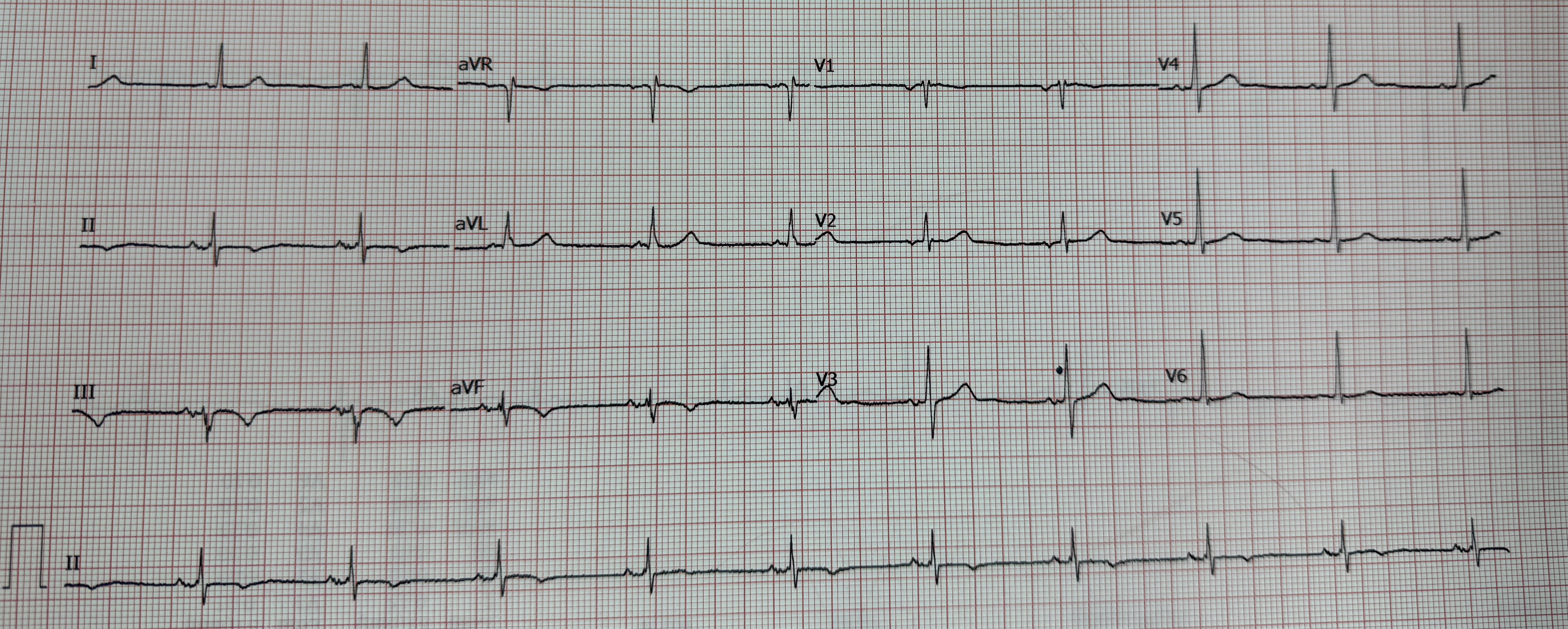
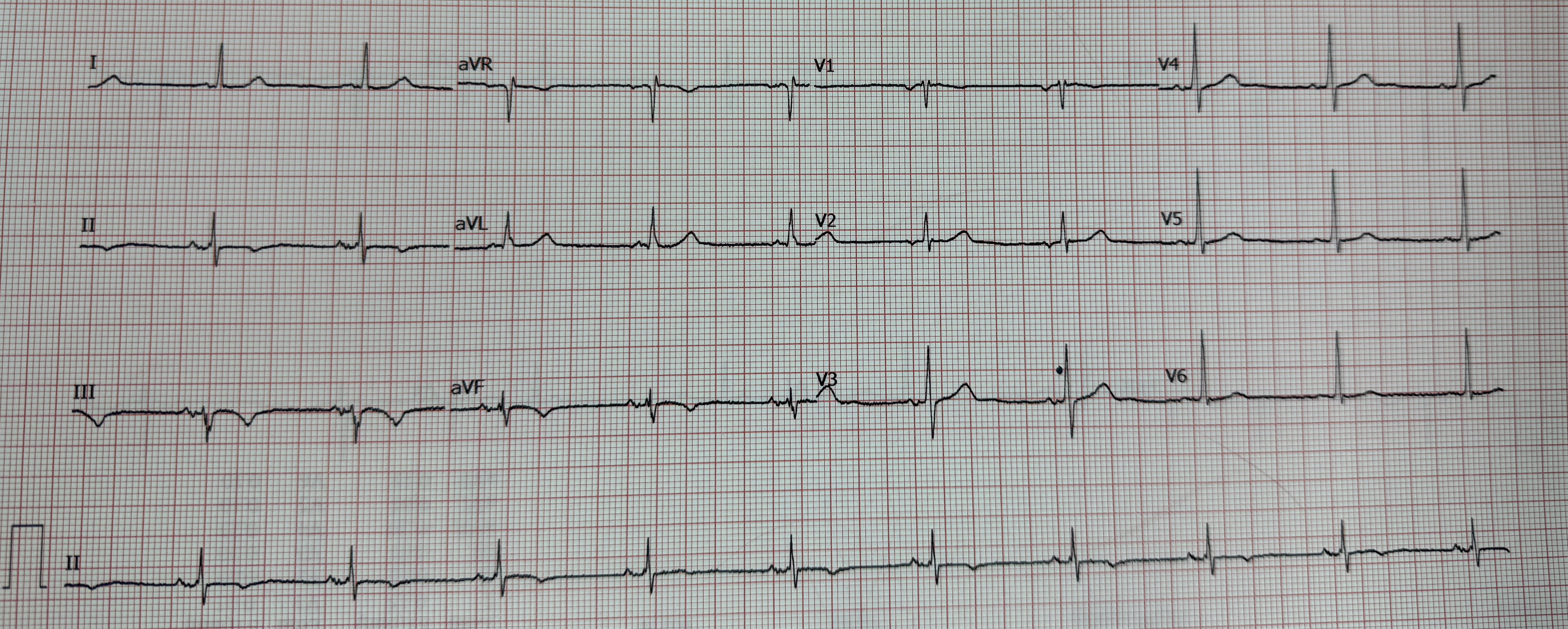
Relevant Test Results Prior to Catheterization
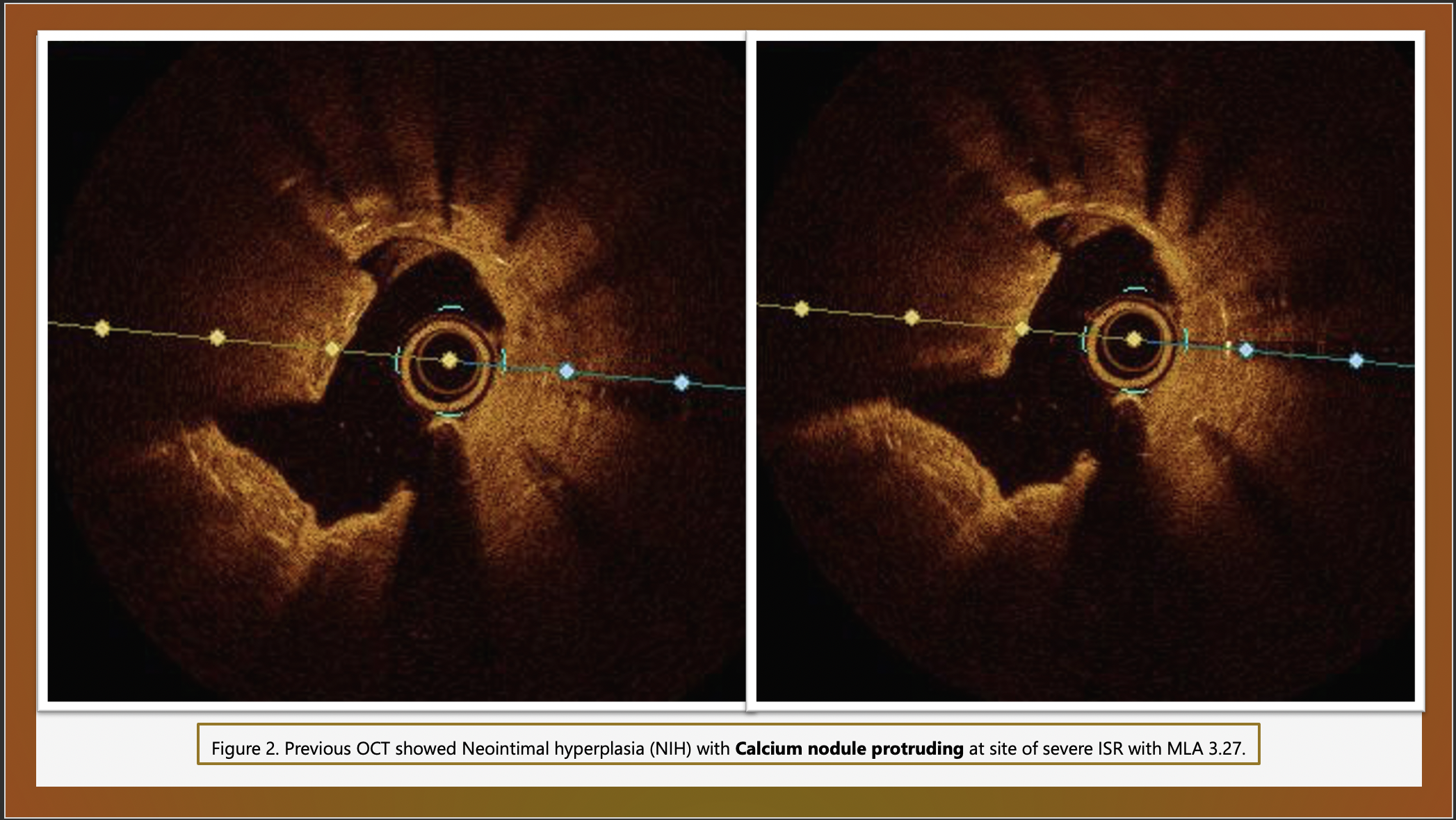
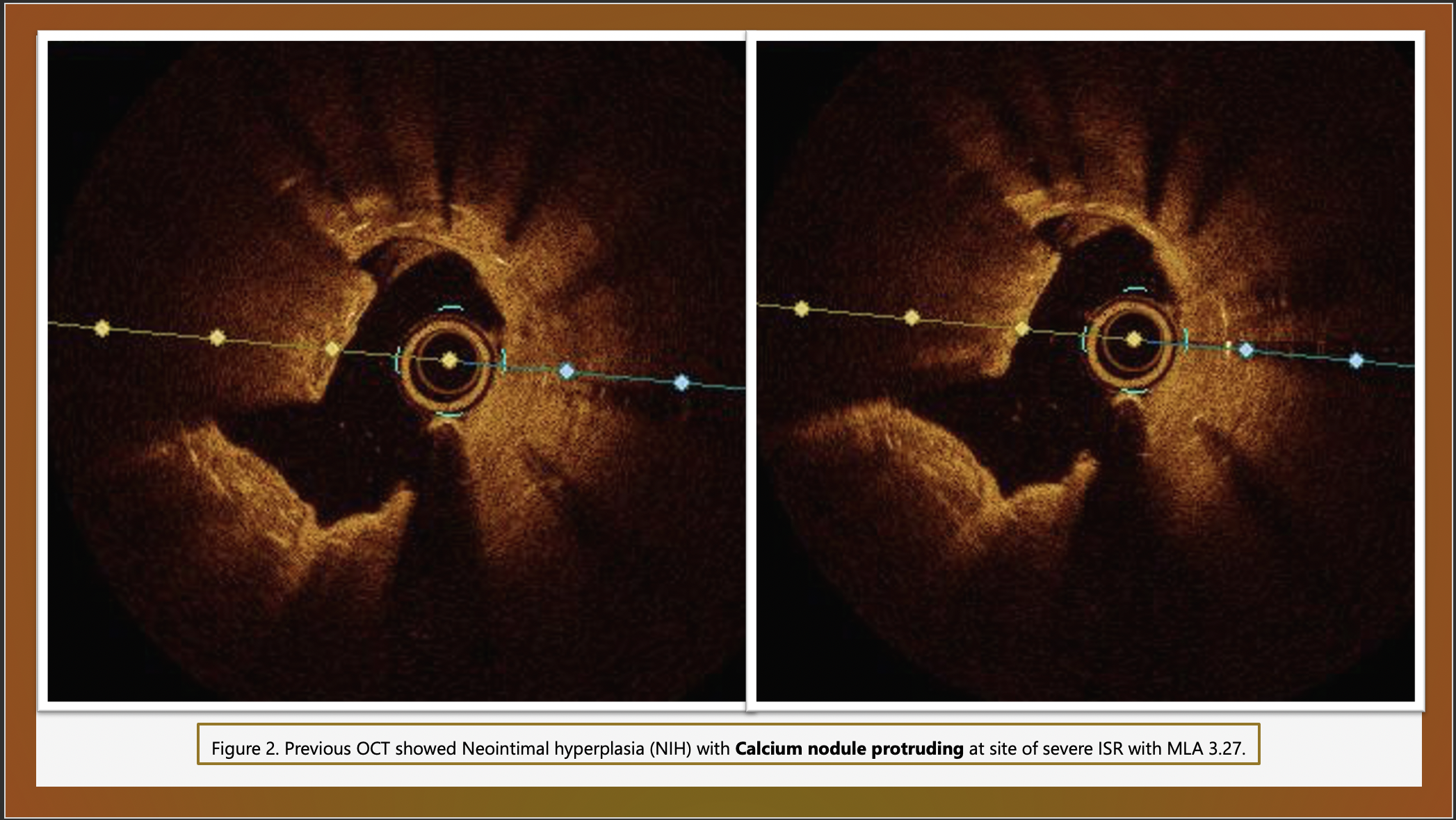
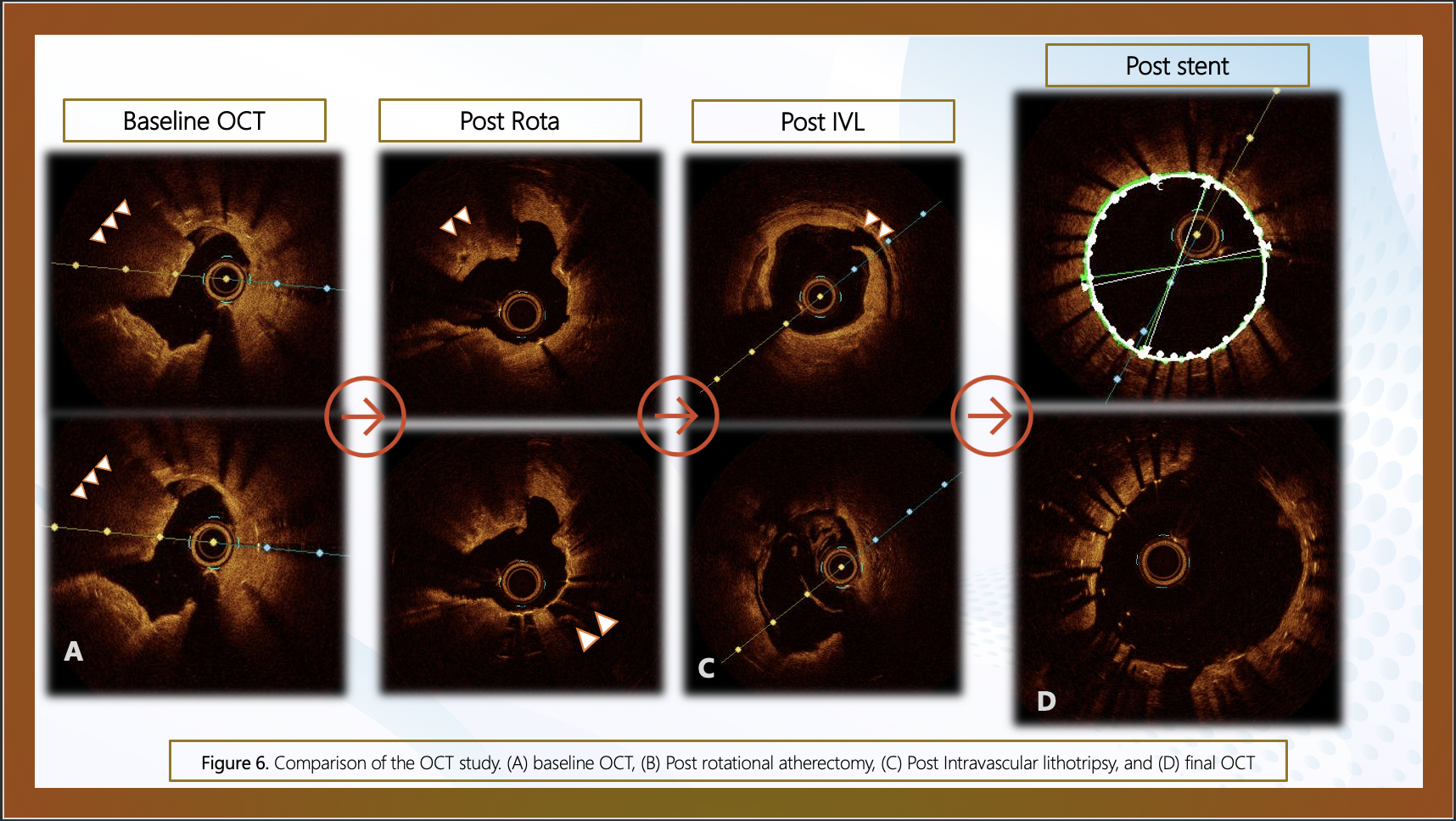
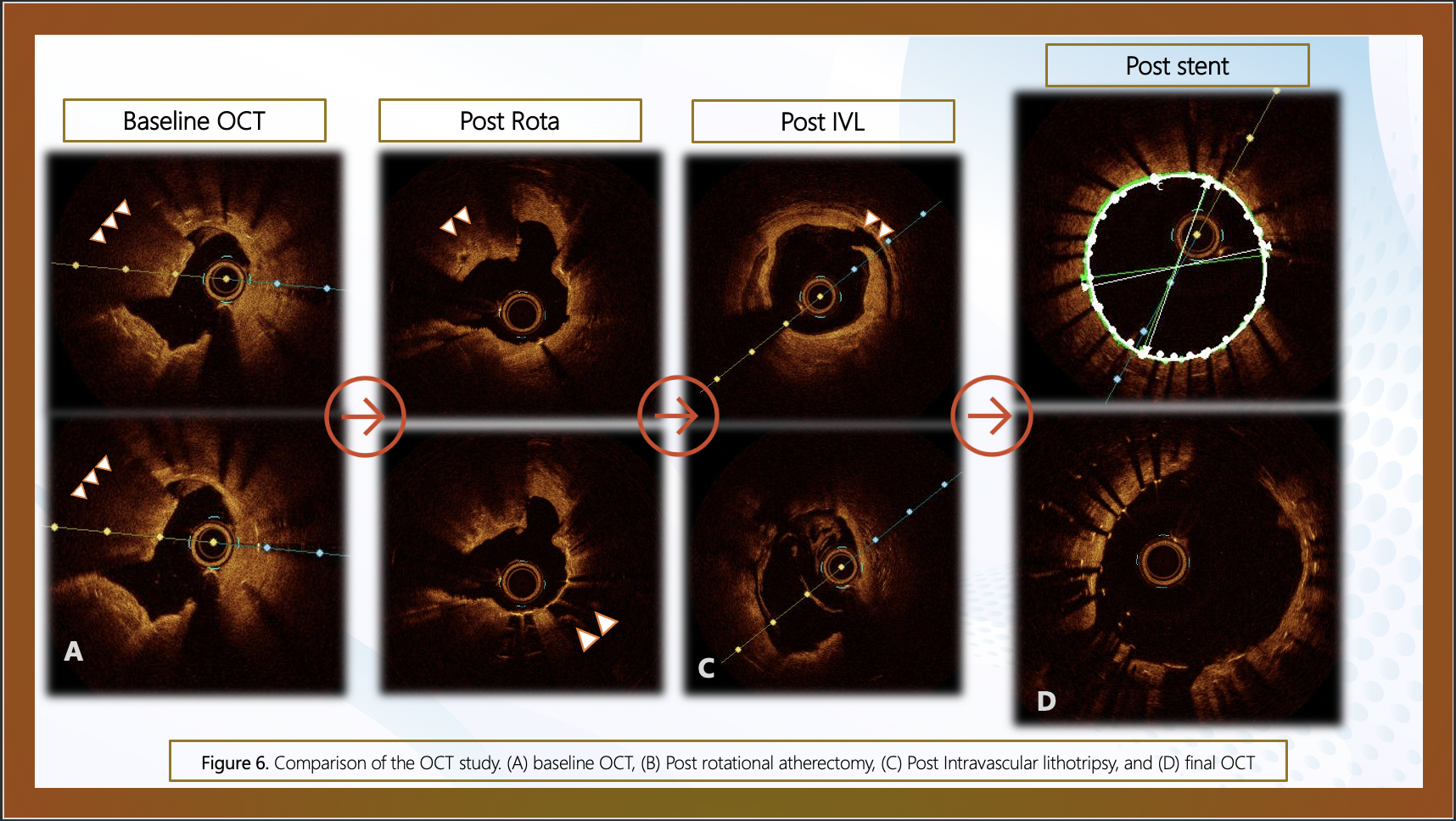
Echocardiography showed preserved LVEF and stress echo which was normal few weeks ago but then developed chest pain with transient lateral ST elevation. In December 2023, OCT showed calcium nodule protruding through stent and some stent under expansion from calcium and treated with IVL, Cutting balloon and DEBs.
Relevant Catheterization Findings
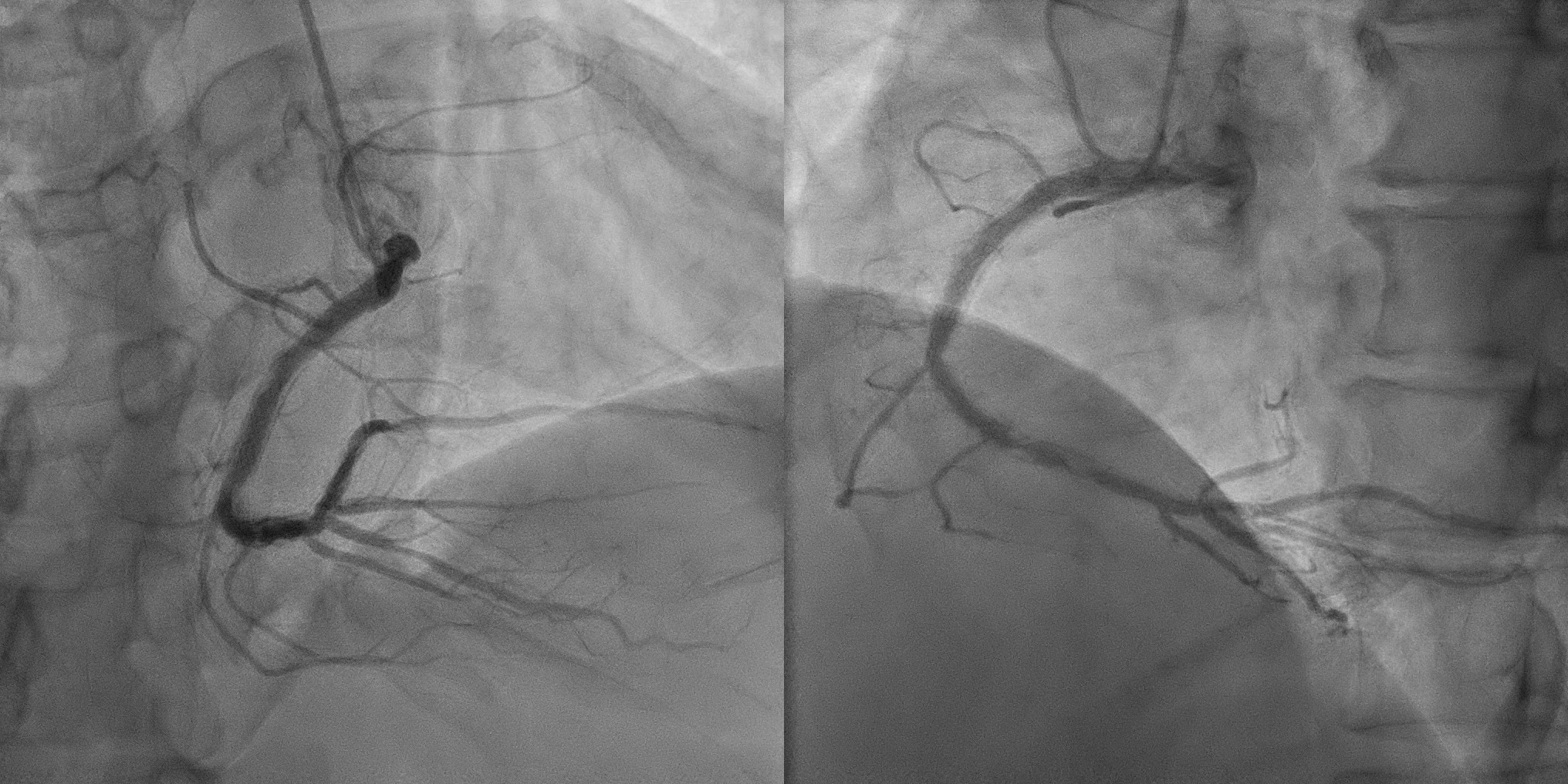
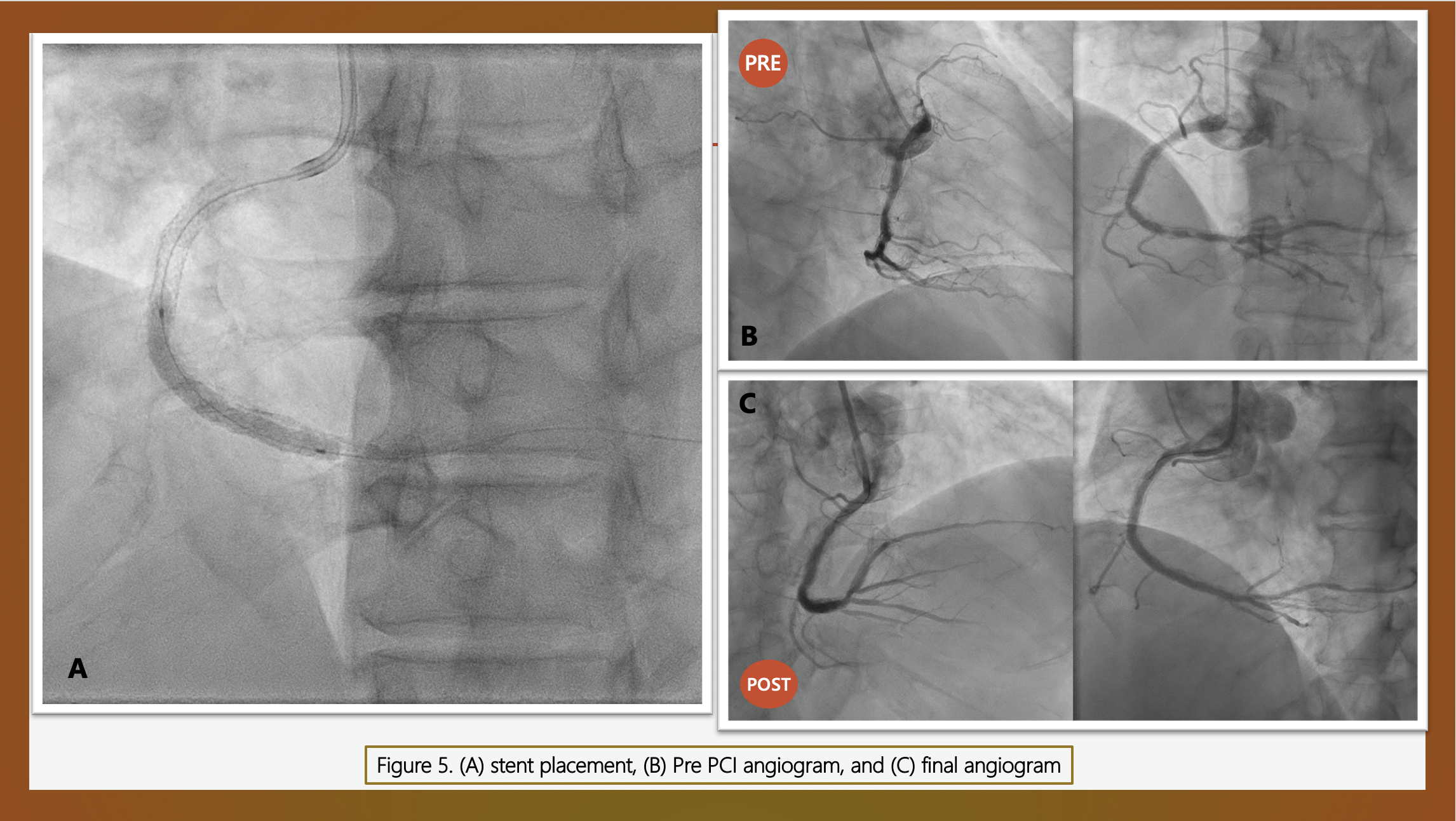
Coronary angiogram confirmed patent stents in proximal and distal vessels, with severe in stent restenosis (ISR) of the distal RCA stent.
Interventional Management
Procedural Step
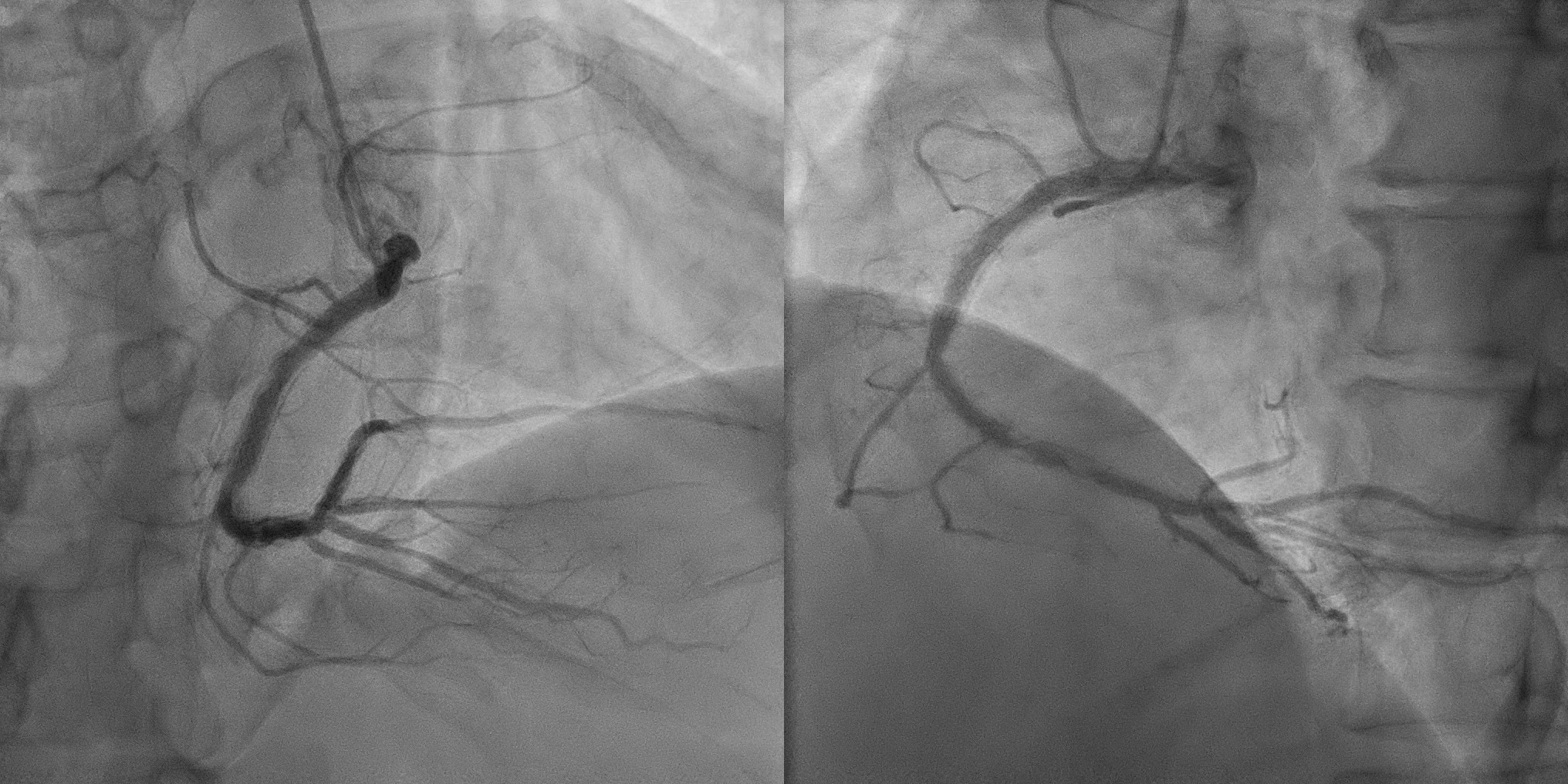
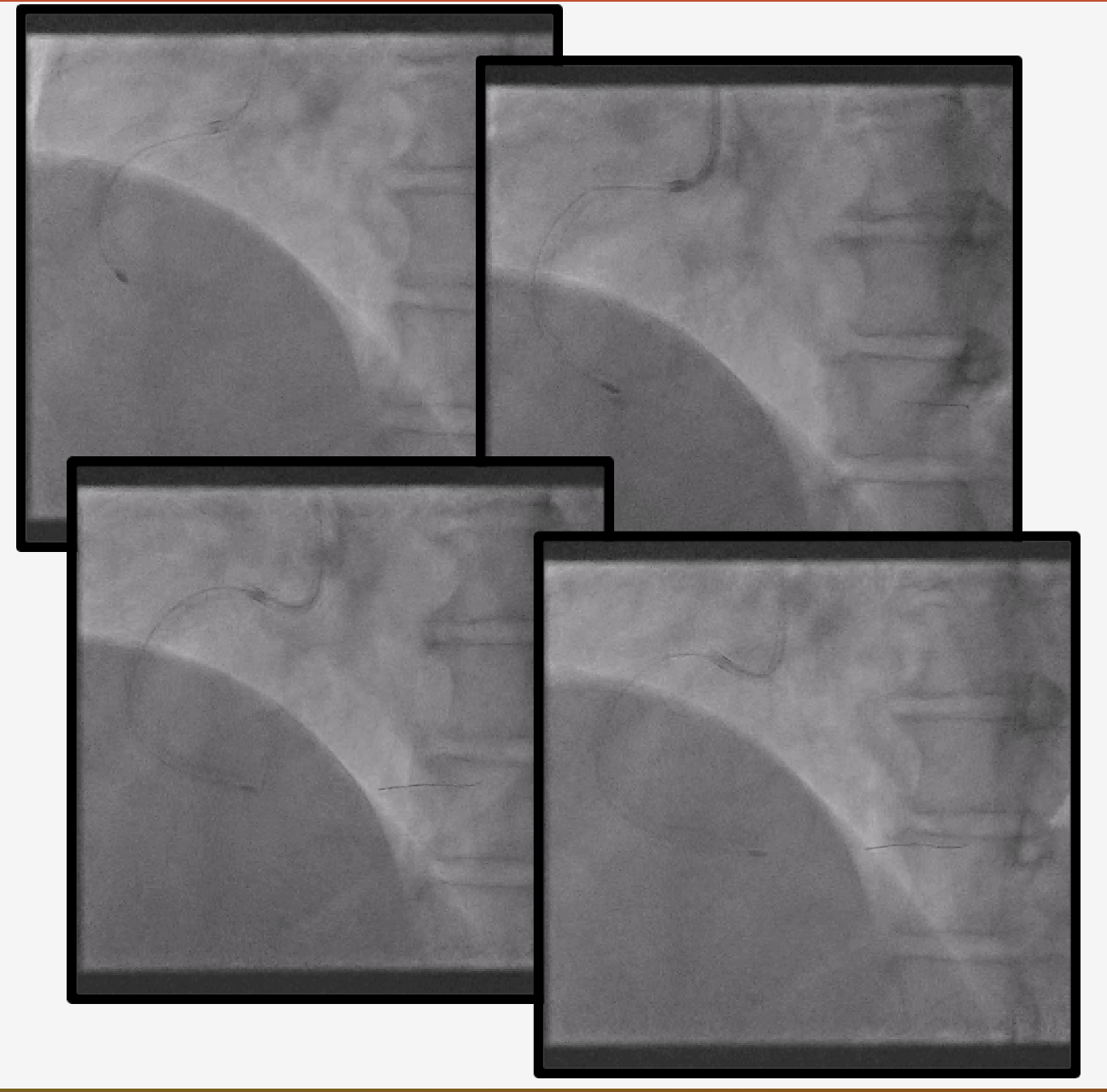
We then performed PCI using a 7-Fr guiding system via the right radial artery. Based on the previous evaluation OCT that ISR was caused by slight stent deformation due protrusion of calcium and we decide to performing upfront rotatripsy. We performed debulking of this calcified ISR with RA 1.75 burr at 170,000 rpm and downsize 1.5 burr at 160,000 rpm in order to obtain further acute luminal gain with the current system. OCT evaluation showed tight distal RCA stenosis with stent struts seen, under expanded half of stent secondary to calcium , compared to OCT in 2022, calcium nodule protruding through stent has been ablated and there was calcium nodule uncovered (no stent). After these sufficient debulking. Balloon angioplasty with a 3.5 mm and 4.0 NC balloon deployed in mid and distal RCA. Repeat OCT good expansion but still eccentric calcium nodule distally where calcium nodule was. Further combination with 3.5 mm IVL 80 bursts in distal RCA and 40 bursts in mid RCA. A DES 3.5x38 deployed in mid-distal RCA overlapped with old stents and OCT guide optimisation with 4.0 mm NC balloon could achieve large lumen gains and optimal stent expansion. Final angiogram and OCT showed optimal results without any coronary flow disturbance.
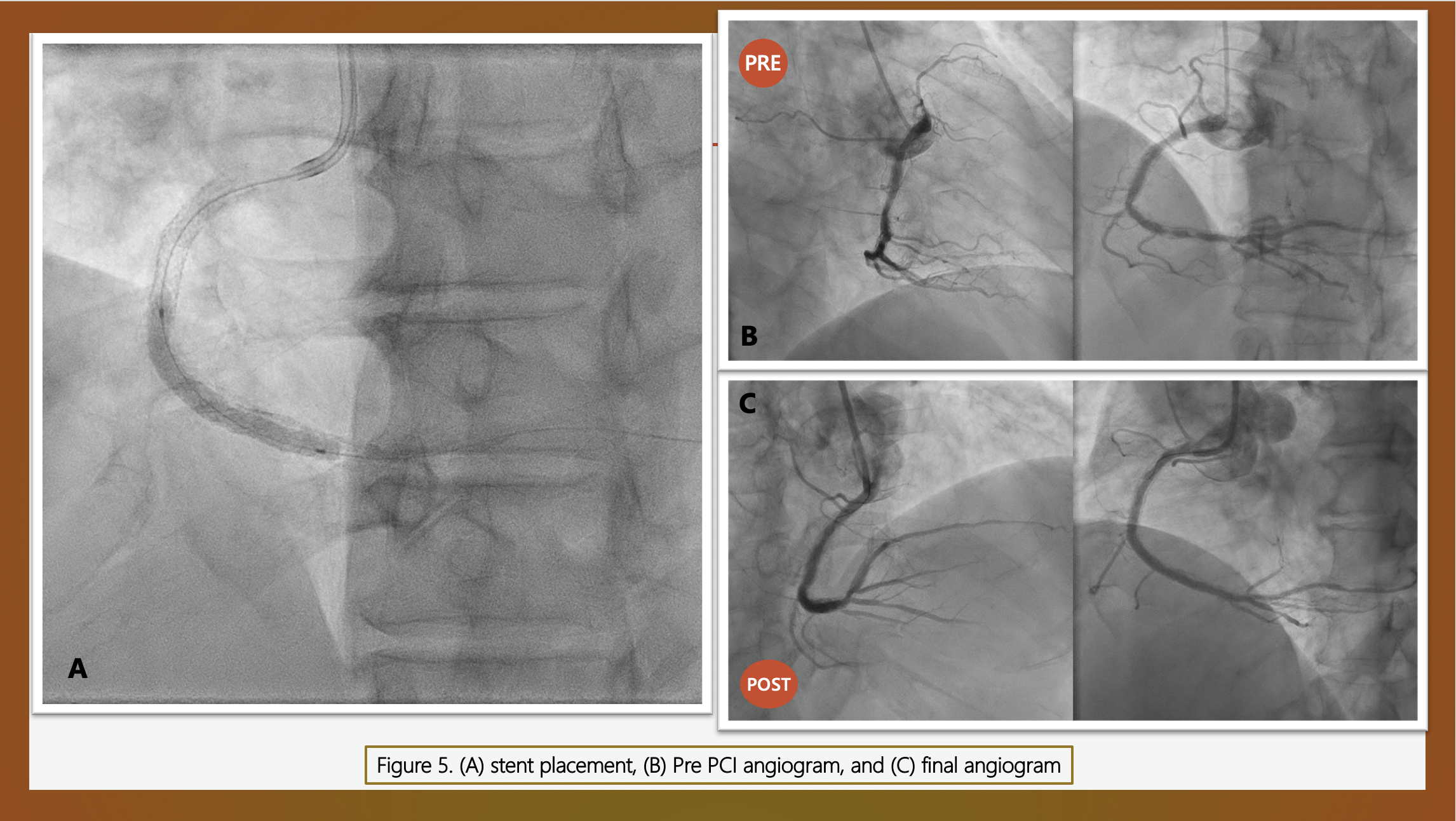
Case Summary
We described a case of refractory ISR caused by calcium nodule in which both RA and IVL were done for calcium modification. “RotaTripsy” technique can be the therapy of choice in critical lesions with deep coronary calcification. Both, RA and IVL are complementary tools, as the intimal ablation of the RA could be not enough to achieve proper balloon expansion, but enables to deliver the IVL balloon that optimize lesion preparation with deep calcium fractures assuring optimal stent implantation.


