Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-176
A Challenging Case: In the Midst of Empty Space
By Joon Soo Chin, Makha Vipanurat, Wittawat Wattanasiriporn, Kay Powpuree
Presenter
Joon Soo Chin
Authors
Joon Soo Chin1, Makha Vipanurat1, Wittawat Wattanasiriporn1, Kay Powpuree1
Affiliation
Rajavithi Hospital, Thailand1,
View Study Report
TCTAP C-176
Coronary - High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
A Challenging Case: In the Midst of Empty Space
Joon Soo Chin1, Makha Vipanurat1, Wittawat Wattanasiriporn1, Kay Powpuree1
Rajavithi Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
56 years old female, U/D HT DLP.Patient was diagnosis as aortic dissection type A with IMH and was transferred to Rajavithi hospital for emergency surgery. After hemi-arch repair with TEVAR and aortic valve replacement, patient developed complete heart block and coudn't wean off heart-lung machine leading to epicardial pacing with central ECMO and high dose inotropic drug. Then intervention cardiologist was consulted to evaluate the cause of poor cardiac function after surgery.


Relevant Test Results Prior to Catheterization
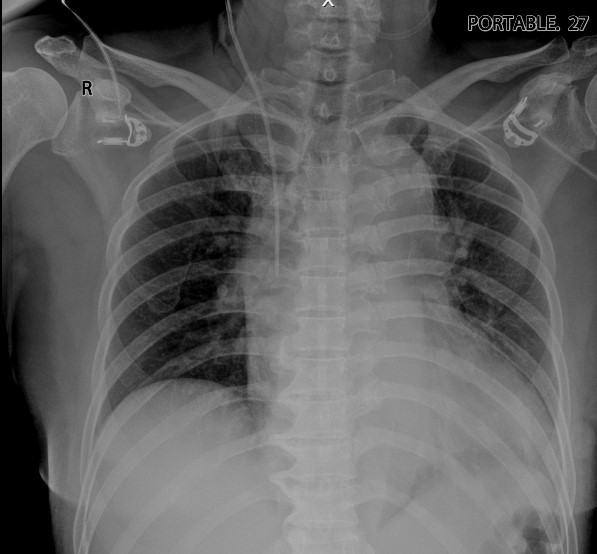
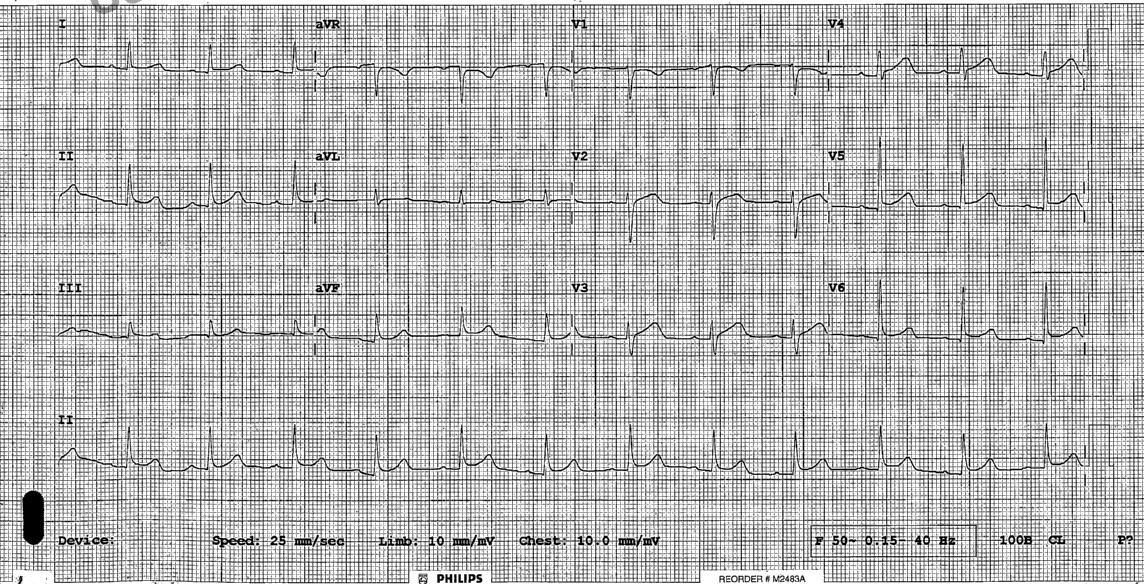
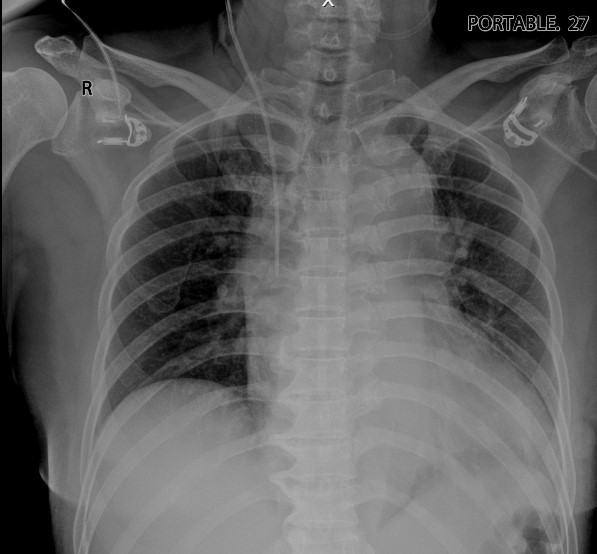
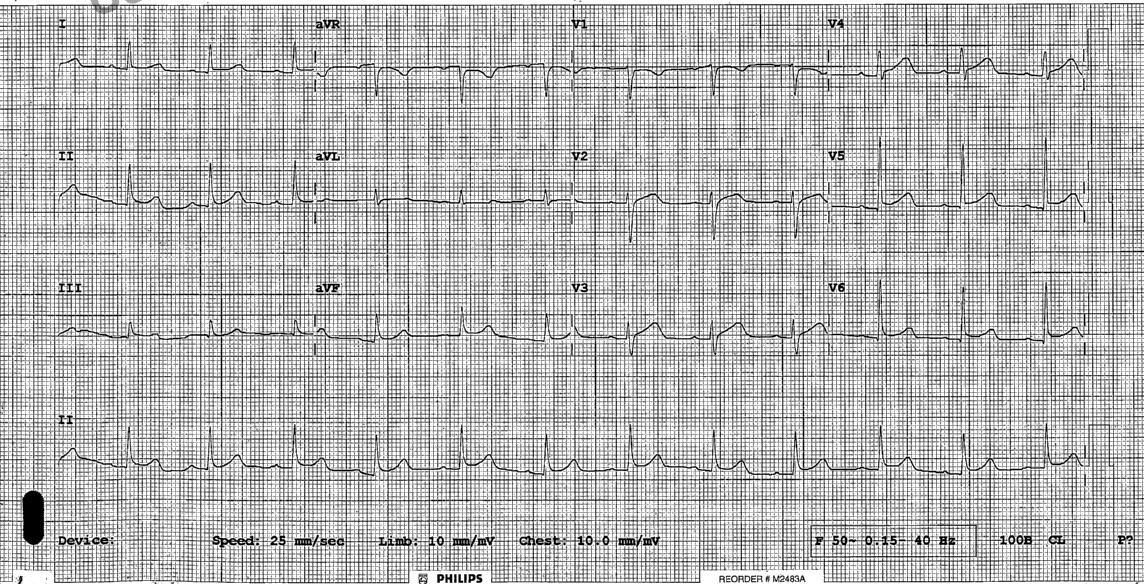
EKG: Normal sinus rhythm rate 74 BPM, Concave ST elevation at lead I, II, III, aVF, V4-V6.
CT Pulmonary artery:
- Aortic dissection from ascending aorta at aortic root extends to abdominal aorta (Stanford type A).
- Extension of dissection into innominate artery.
- The celiac trunk, SMA, right renal artery and IMA are branching from true lumen.
- Left renal artery arise from false lumen.
ECHO (before surgery):
- EF 60% Biplane.
- No RWMA.
- Minimal pericardial effusion, No tamponade.
- Mild AR.
Relevant Catheterization Findings
Left main: Distal left main total occlusion.
LAD: Total occlusion.
LCx: Total occlusion.
RCA: Total occlusion.
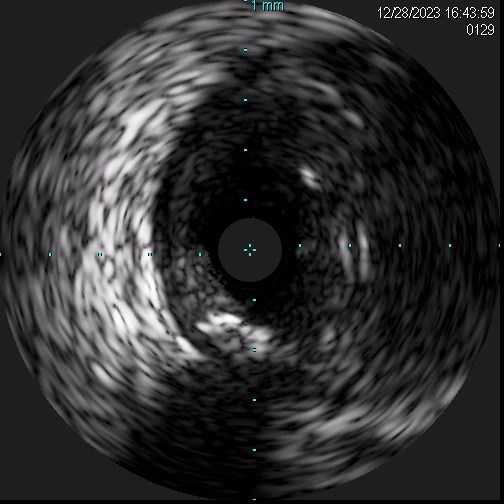
IVUS image revealed mixed plaque with two lumens at left main. The IVUS catheter was in true lumen with three-layered and ellipsoid appearance and other lumen was suspected to be a false lumen with hematoma (noted with out three-layered), compatible with coronary dissection with hematoma.
Interventional Management
Procedural Step
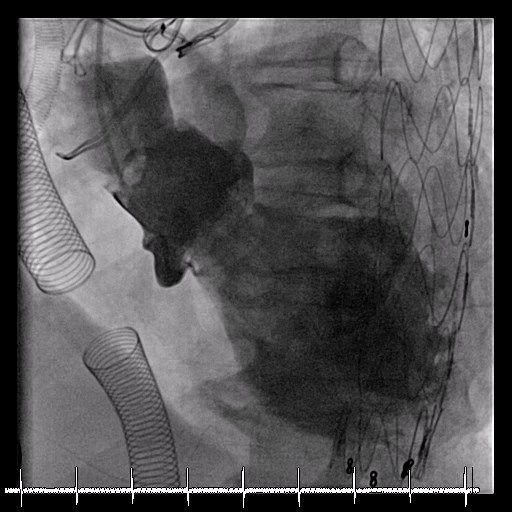
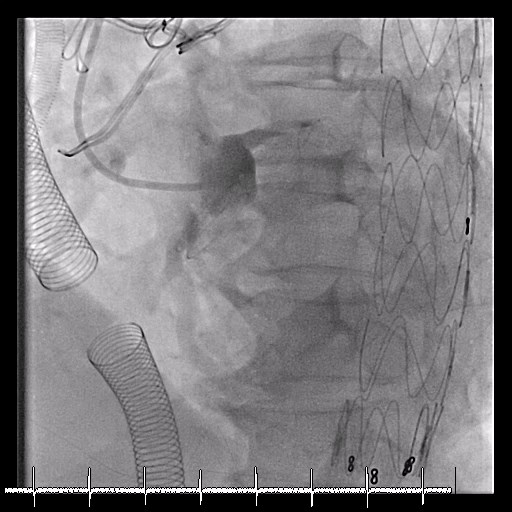
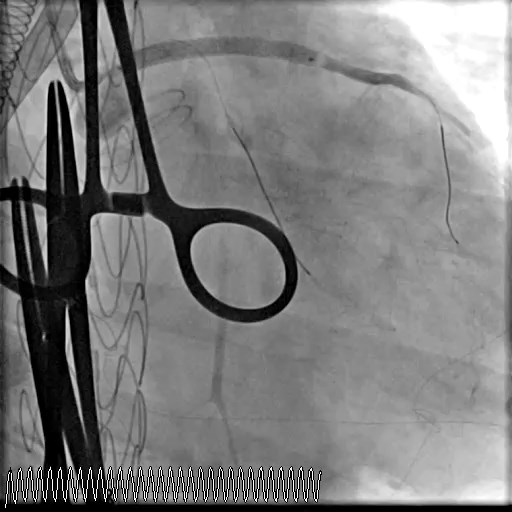
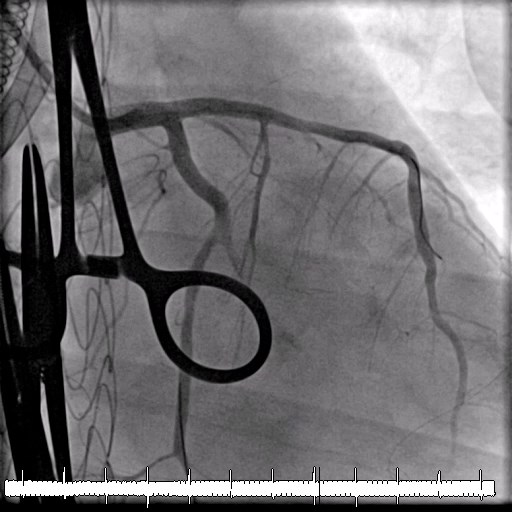
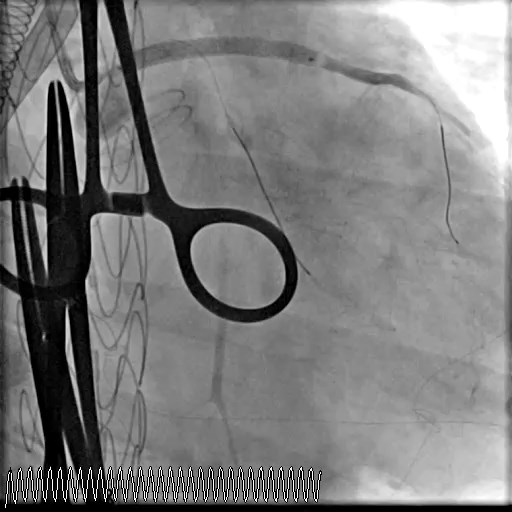
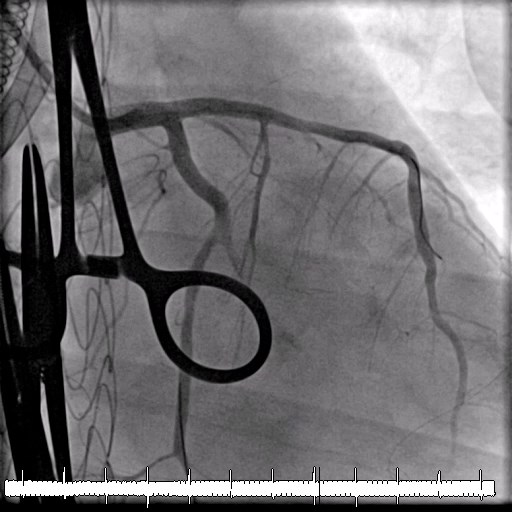
We used 6 Fr radial sheath inserted via right radial artery. A brachial artery angiogram was performed to guide delivery of a catheter due to tortuous vessel. A 5 Fr Outlook catheter failed to identify both LCA and RCA. Consequently, we switched to a 5 Fr pigtail catheter and delivered it to non-coronary cusp to perform an aortogram using an injector. The ostial LM was then identified.We used a JL 6 Fr 3.5 as the guiding catheter to engage LM. Two Turntrac wires were delivered to distal LAD and LCx. Pre-dilate was performed at LM-LAD/LCx with a semi-compliant balloon 2.5x20 mm inflated to 10 atm. After that, thrombectomy was done but no clot was retrieved. IVUS was then performed; however, the catheter could not be delivered beyond distal LM, so pullback from LM was done. Coronary dissection with hematoma in false lumen was suspected, then ad hoc PCI to LM-LAD and provisional LCx was planned.A rapamycin-eluting stent 3.5x33 mm was deployed at LM-LAD inflated to 12 atm, then post-dilated with same stent balloon inflated to 18 atm. POT was performed with non-compliant balloon 5.0x12 mm inflated to 12 atm. LCx was rewired by Sion, then trap wire was removed. We open strut with a semi-compliant balloon 2.5x20 mm inflated to 8 atm, but LCx flow remained compromised. As a result, a bailout two-stent TAP technique was planned. A rapamycin-eluting stent 3.0x23 mm was deployed at LCx inflated to 10 atm (TAP technique). Final angiogram demonstrated an acceptable result.
 STENT LAD RAO CAU.mp4_snapshot.jpg
STENT LAD RAO CAU.mp4_snapshot.jpg

 STENT LCX 2 LAO CAU.mp4_snapshot.jpg
STENT LCX 2 LAO CAU.mp4_snapshot.jpg
 FINAL RAO CAU.mp4_snapshot.jpg
FINAL RAO CAU.mp4_snapshot.jpg

Case Summary
Learning points1) We report a rare case of coronary dissection with total occlusion of the LCA and RCA after aortic surgery it presents both a diagnostic and therapeutic challenge.2) Other than CT, Intra-vascular imaging is also beneficial to diagnosis retrograde coronary dissection or determine mechanism of disease, inform therapeutic strategy, and confirm effective treatment of PCI.3) TAP stenting is a valuable technique for both bail-out side branch stenting and for PCI in complex bifurcation lesion.4) Adequate mechanical circulatory support can help stabilize patients for multi-vessel revascularization in complex and high-risk PCI.


