Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-018
A Story of Saphenous Vein Graft Intervention in a Patient With Acute Coronary Syndrome
By Jian Hao Sim, Vicknesan Kulasingham, Hou Tee Lu, Kwang How Ng, Ao Xiang Quek, Jin Kiang Cheng, Waye Young Lau, Wee Pang Ng, Wen Sheng Wong, Nur Hazurreen Harryzan, Gurudevan Mahadevan
Presenter
Jian Hao Sim
Authors
Jian Hao Sim1, Vicknesan Kulasingham1, Hou Tee Lu1, Kwang How Ng1, Ao Xiang Quek1, Jin Kiang Cheng1, Waye Young Lau1, Wee Pang Ng1, Wen Sheng Wong1, Nur Hazurreen Harryzan1, Gurudevan Mahadevan1
Affiliation
Sultanah Aminah Hospital, Malaysia1,
View Study Report
TCTAP C-018
Coronary - ACS/AMI
A Story of Saphenous Vein Graft Intervention in a Patient With Acute Coronary Syndrome
Jian Hao Sim1, Vicknesan Kulasingham1, Hou Tee Lu1, Kwang How Ng1, Ao Xiang Quek1, Jin Kiang Cheng1, Waye Young Lau1, Wee Pang Ng1, Wen Sheng Wong1, Nur Hazurreen Harryzan1, Gurudevan Mahadevan1
Sultanah Aminah Hospital, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
Mr KA is a 42-year-old gentleman with a background history of hypertension, diabetes mellitus, and ischemic heart disease – he had a history of infero-posterior STEMI in 2013 and had undergone Coronary Artery Bypass Grafting (CABG) in 2013. He quit smoking cigarettes in 2013. He presented with worsening angina for a day, associated with diaphoresis, temporarily relieved with sublingual GTN. Physical examination revealed sternotomy scar. BP 144/78mmHg, HR 74bpm, SpO2 98% on room air.
Relevant Test Results Prior to Catheterization
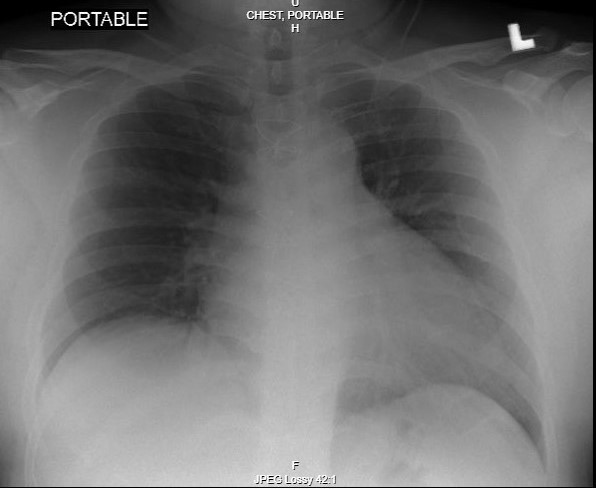
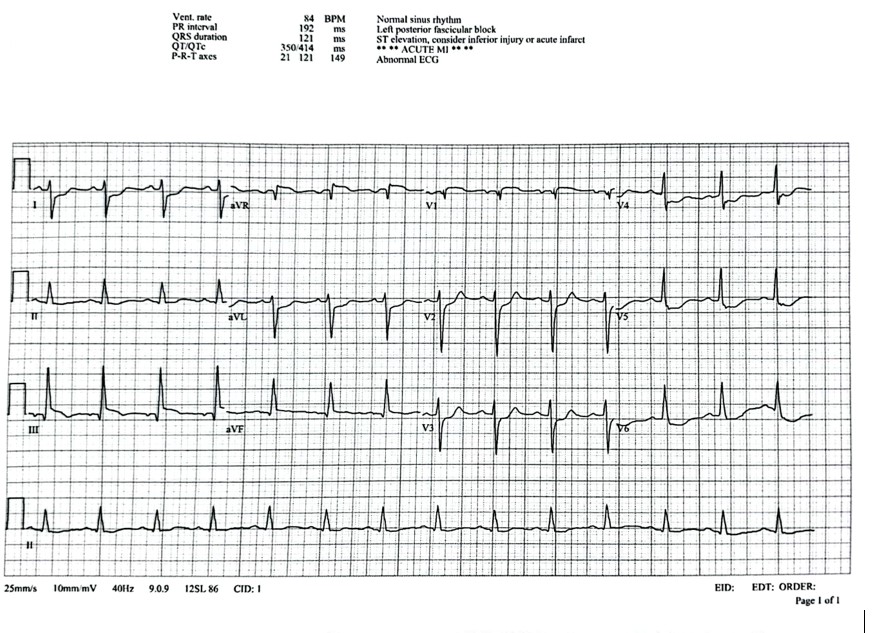
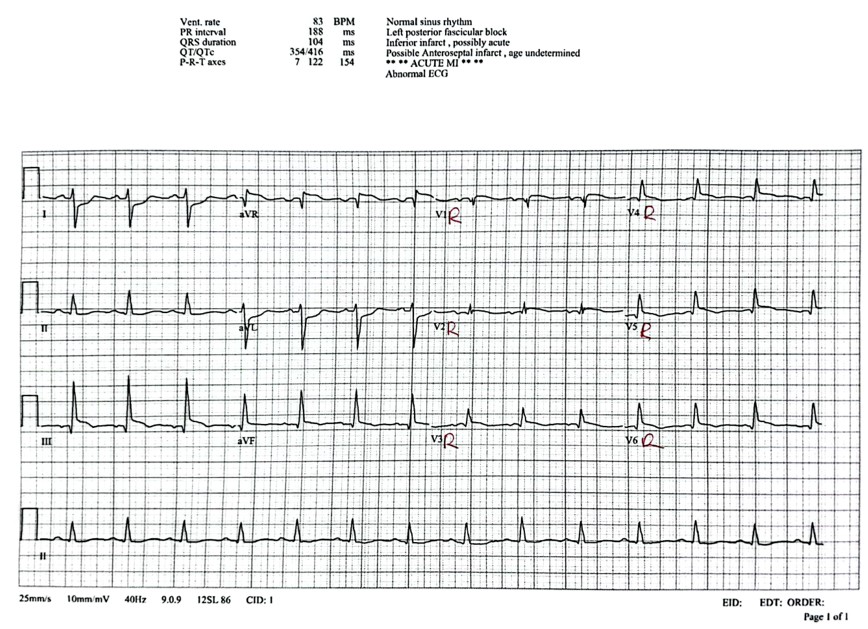
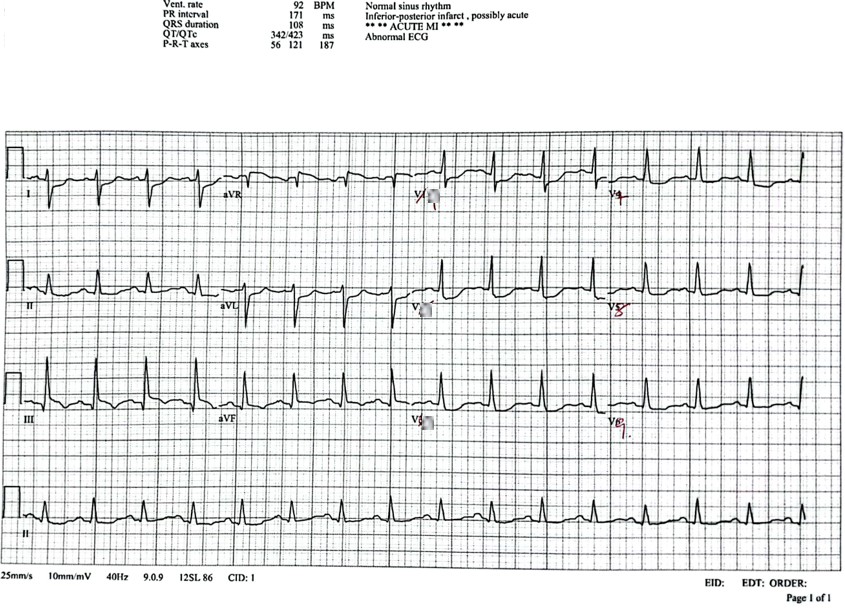
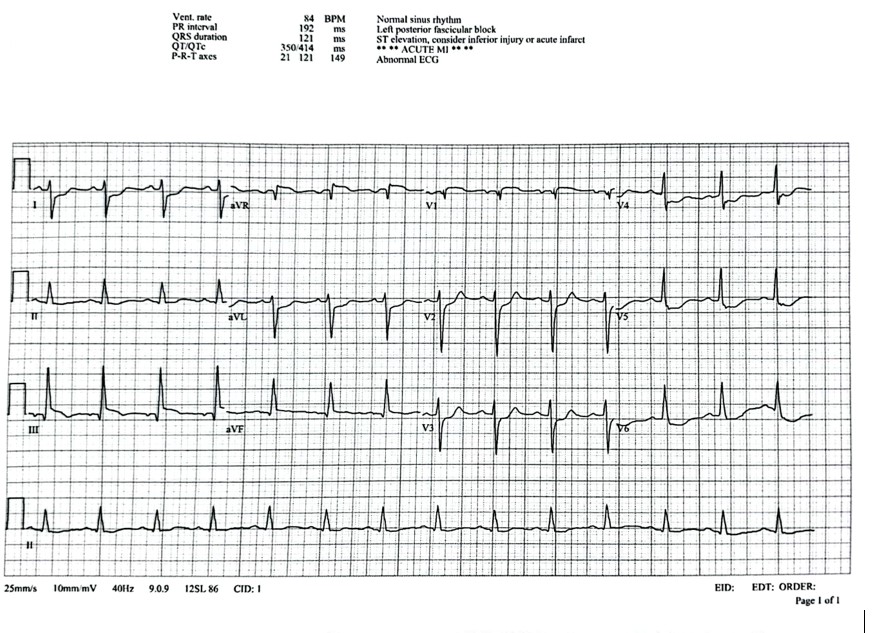
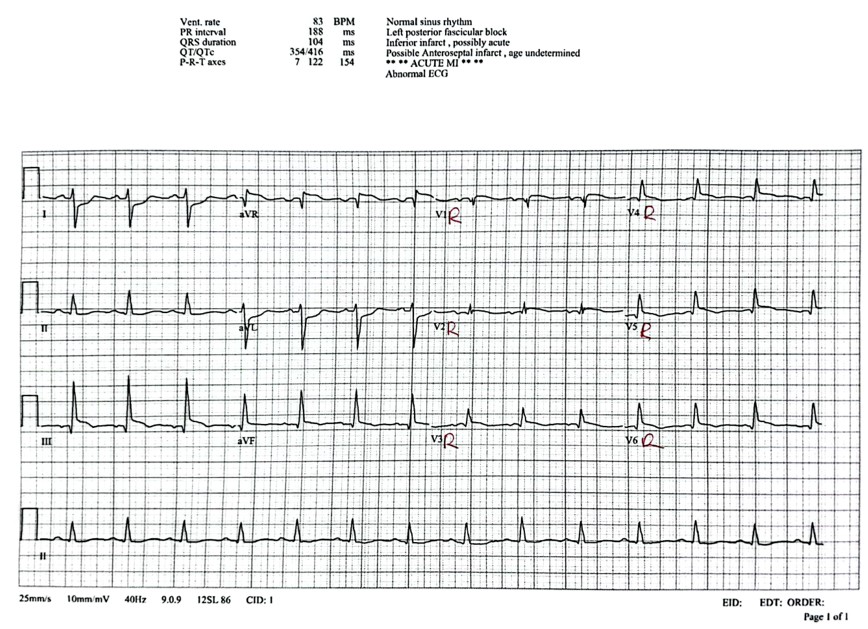
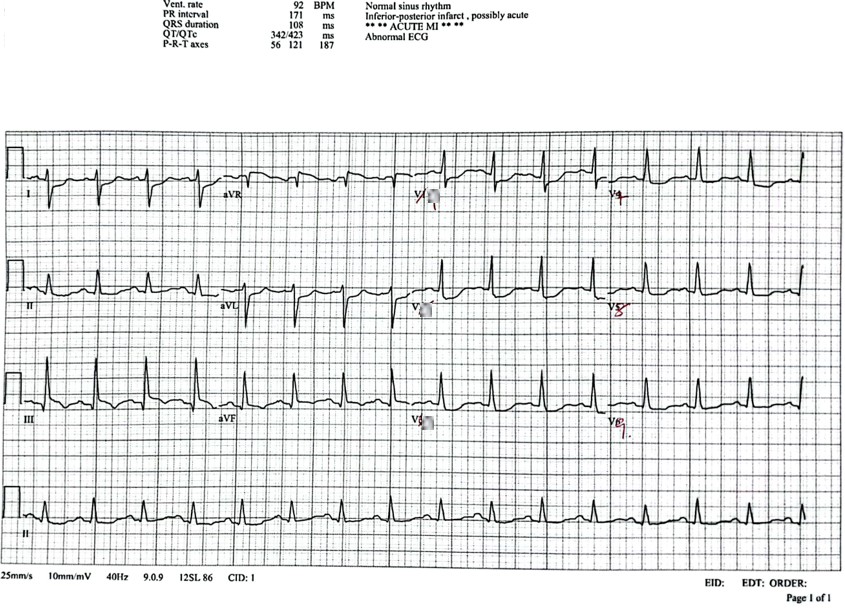
ECG: ST elevation lead III, aVR, V1, V4R - V6R; ST depression V2 - V6, I, aVL, V7 - V9. High sensitivity Troponin-I (hs-TropI): 8589.06 ng/L, which rose to 21107.12 ng/L after 2 days. WBC 9.6 x10^3/UL, Hb 12.6g/dL, Platelet 303 x 10^3/UL Urea 5.4 mmol/L, Creatinine 110 umol/LHbA1c 6.6% ECHO: LVEF 32%. Global hypokinesia. LV dilated.
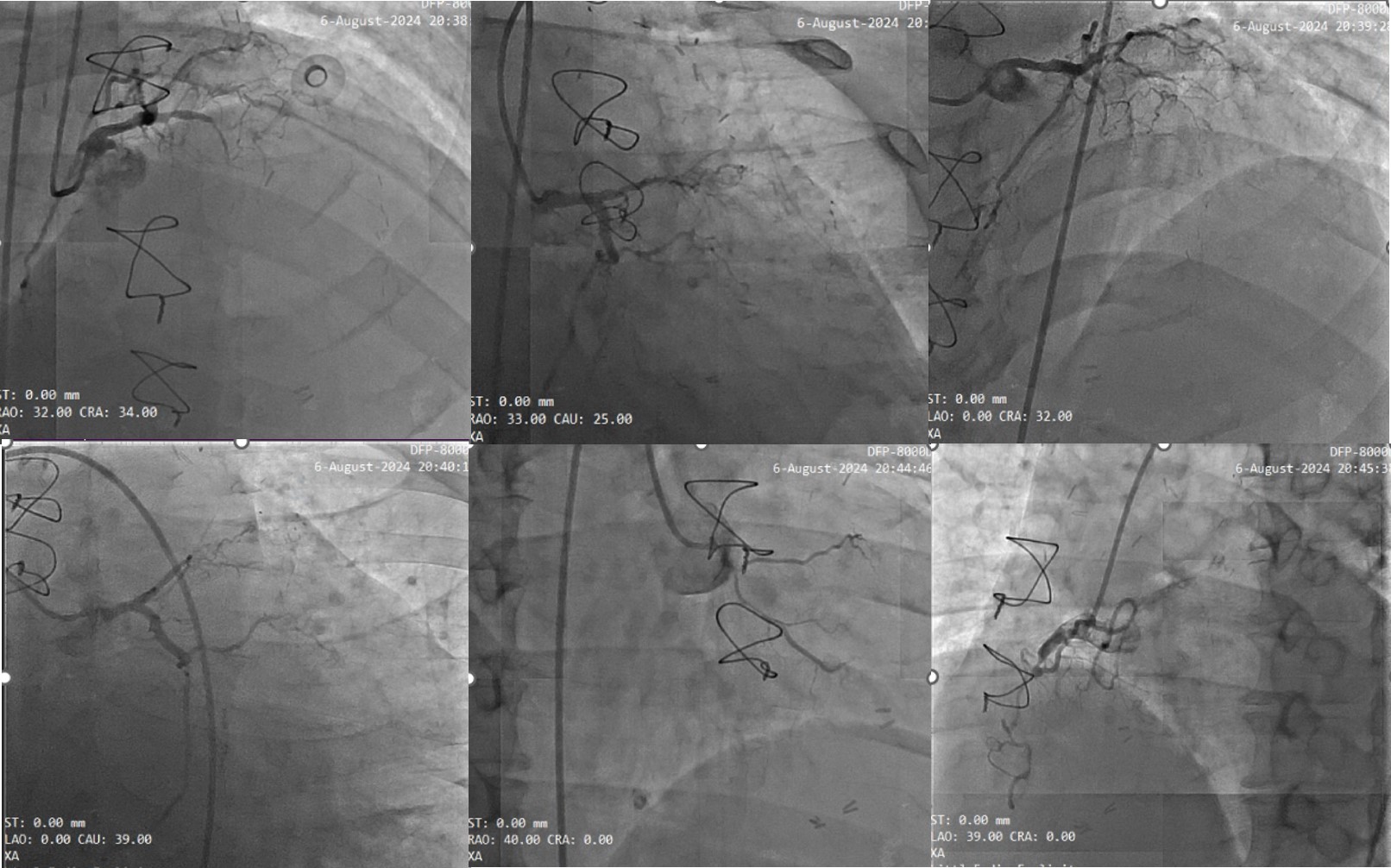
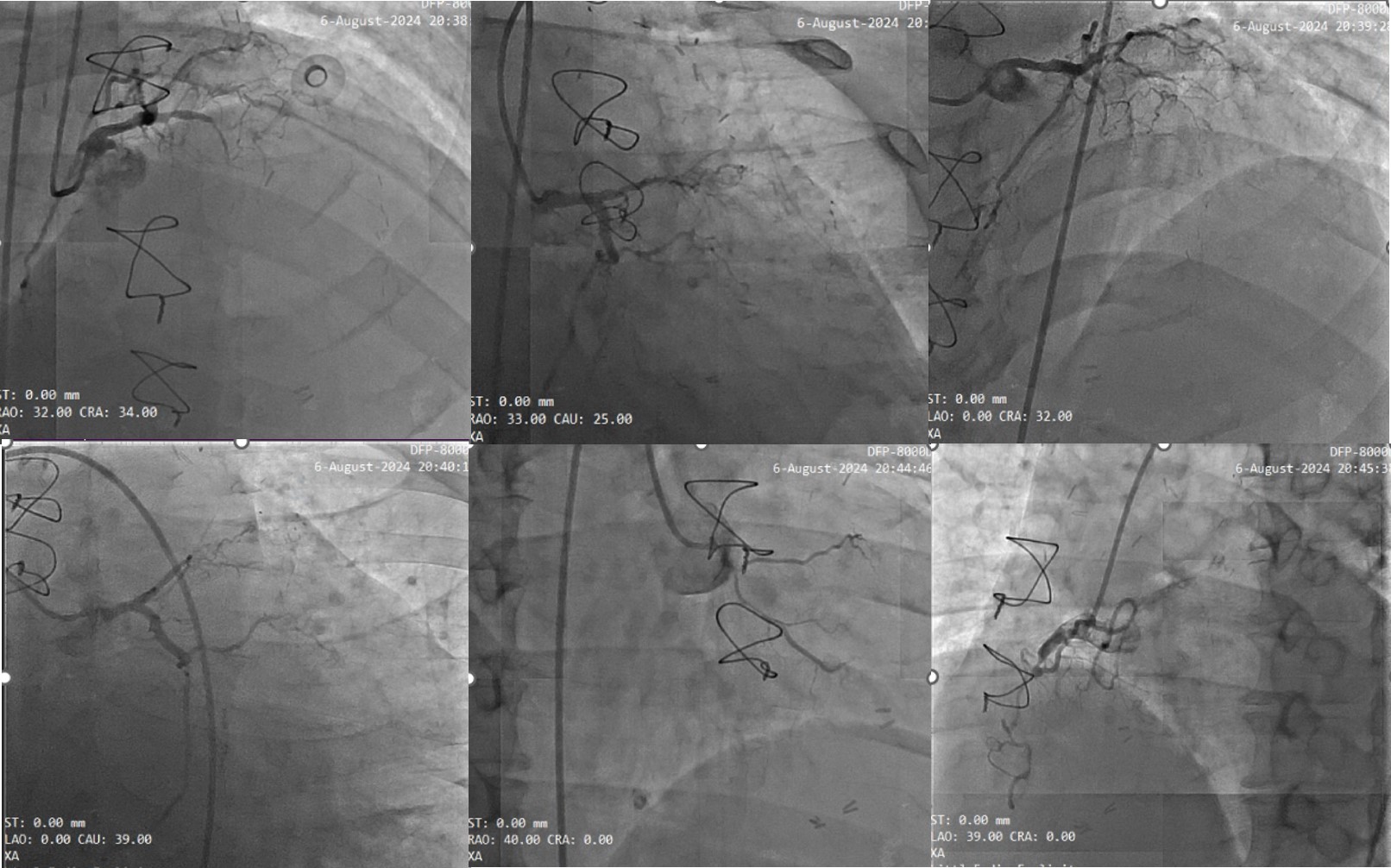
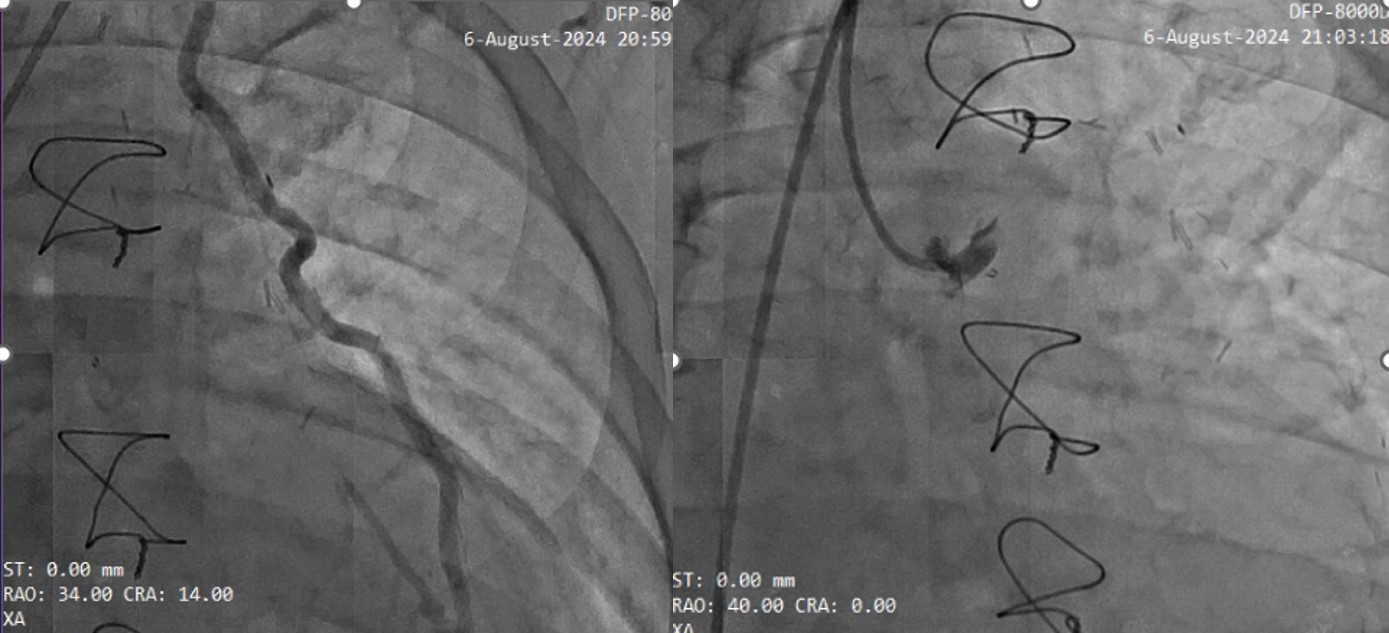
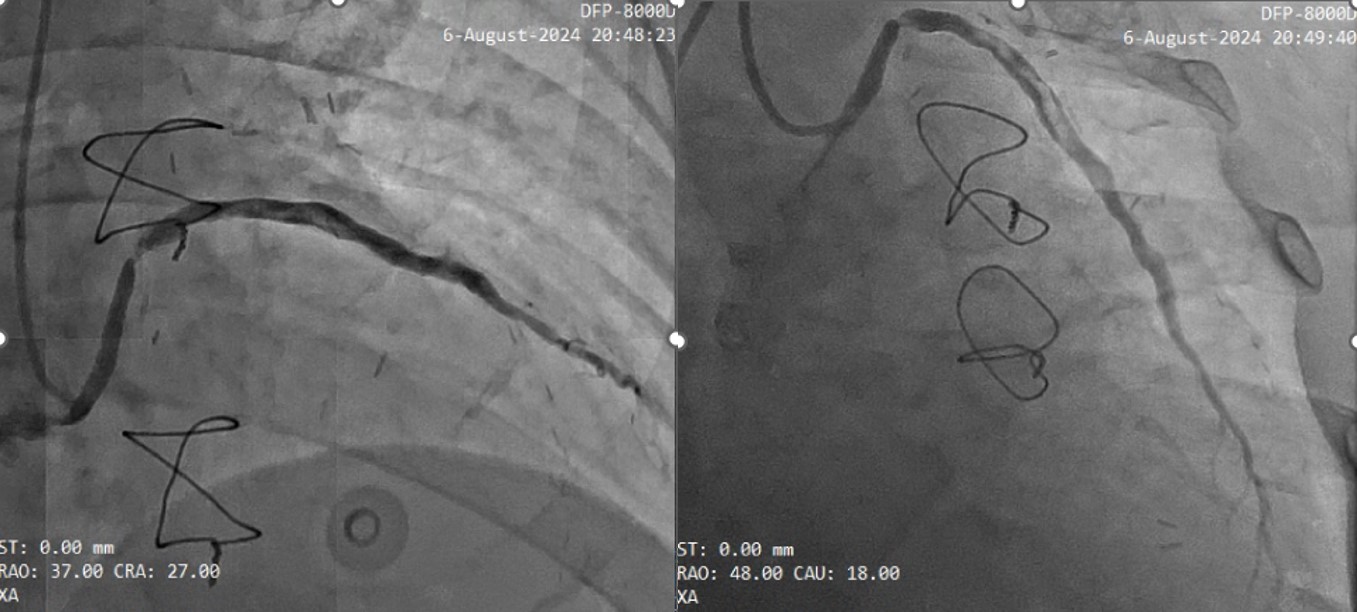
Relevant Catheterization Findings
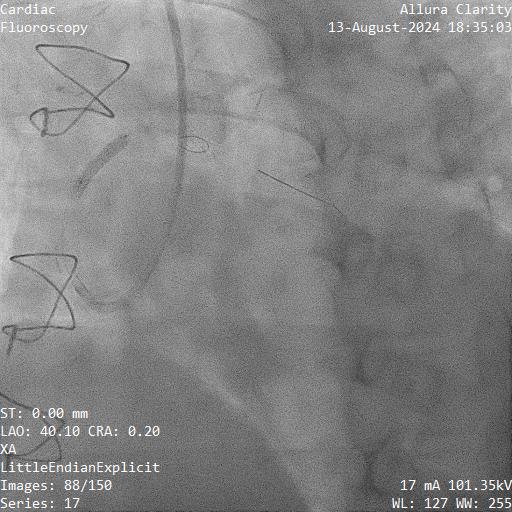
left main stem: distal 30% stenosisLeft Anterior Descending (LAD): proximal Chronic Total Occlusion (CTO)Left Circumflex Artery (LCX): proximal CTO Right Coronary Artery (RCA): proximal CTO Saphenous Vein Graft (SVG) – Obtuse Marginal (OM): 90% with thrombi Left Internal Mammary Artery (LIMA) – Left Anterior Descending (LAD): patentSaphenous Vein Graft (SVG) - Right Coronary Artery (RCA): visible stump; no flow beyond stump - CTO
Interventional Management
Procedural Step
We deferred percutaneous coronary intervention to the Saphenous Vein Graft (SVG) - Obtuse Marginal (OM) in view of the high thrombus burden. We treated the patient with subcutaneous Enoxaparin BD and double antiplatelet with T. Aspirin and T. Clopidogrel in the meantime.
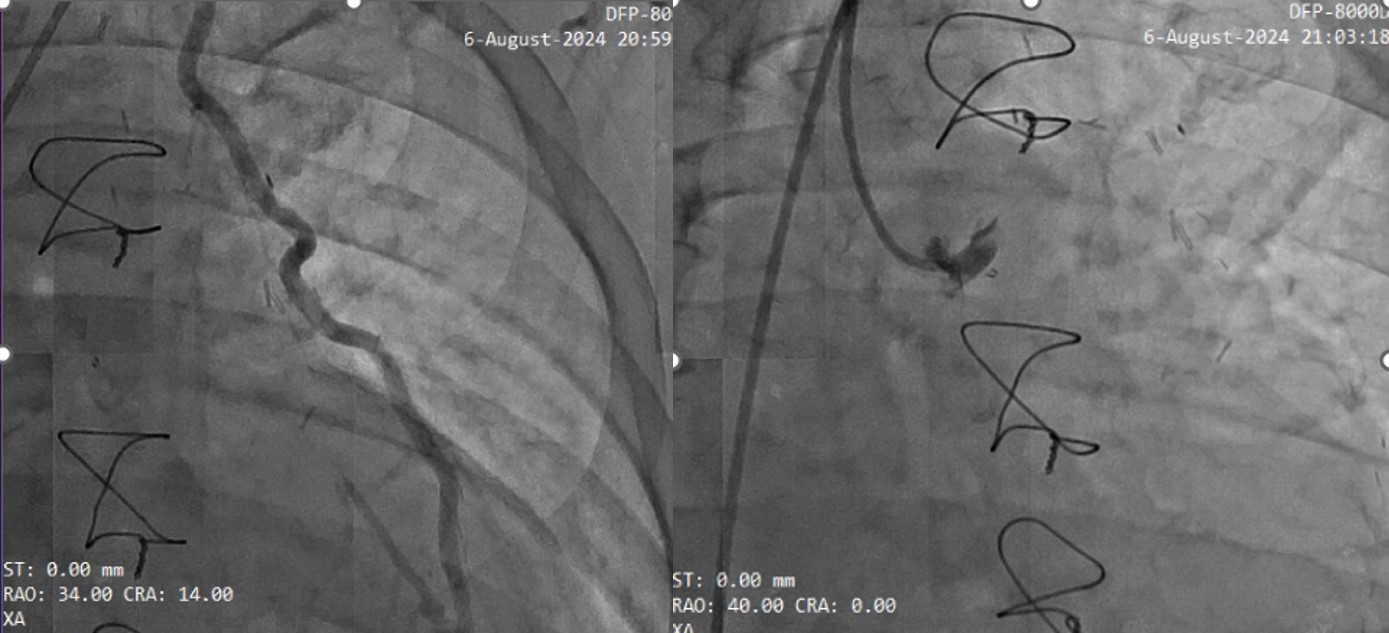
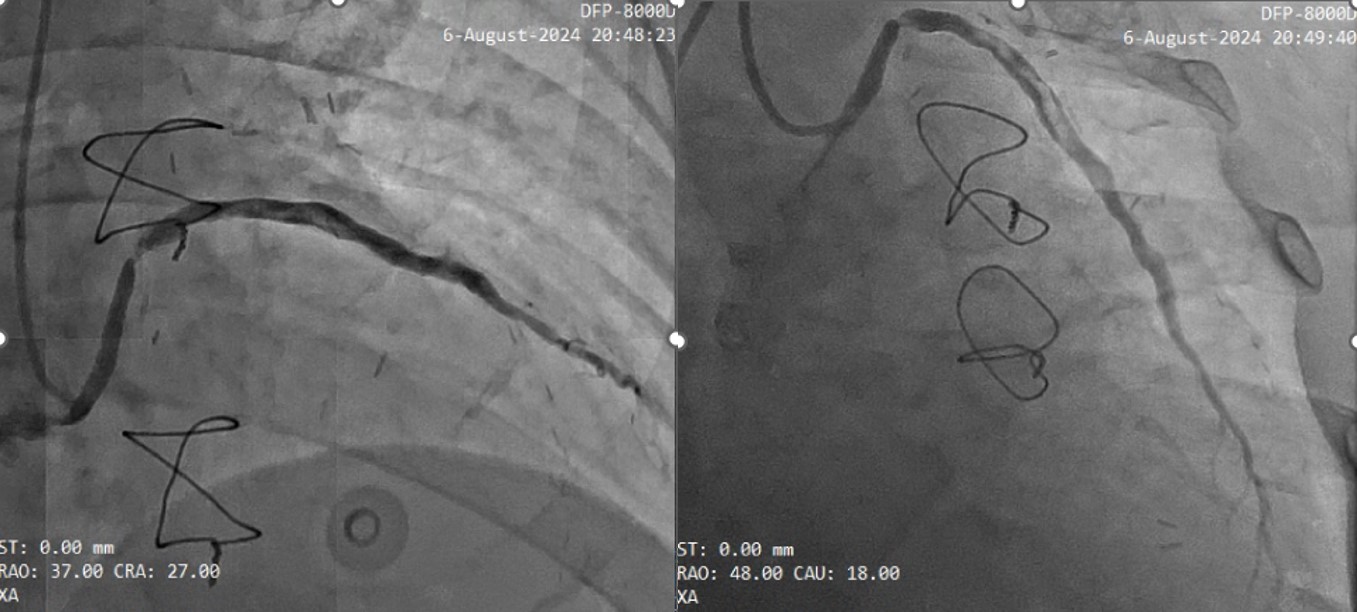
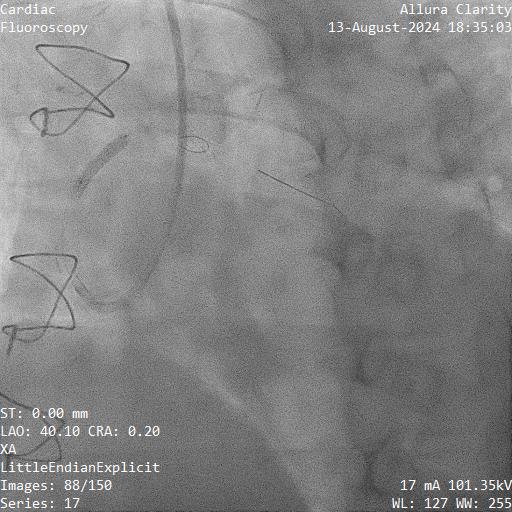
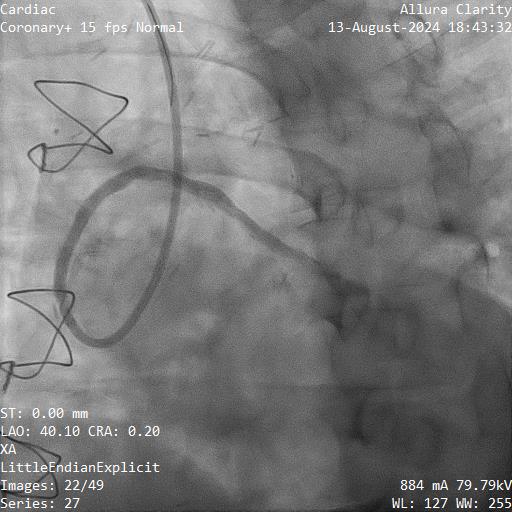
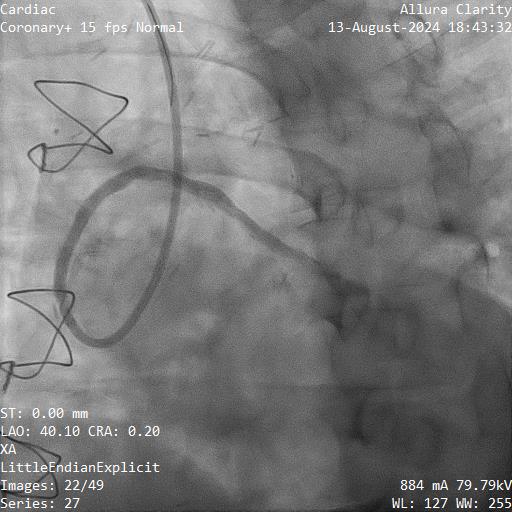
We brought the patient back to the catheterization lab after 1 week of subcutaneous Enoxaparin for percutaneous coronary intervention to the Saphenous Vein Graft (SVG) - Obtuse Marginal (OM). We gained vascular access through the right radial artery with slender sheath. We engaged the SVG - OM with JR4 7Fr. Coronary angiography showed minimal residual thrombus in the SVG - OM. We wired into the SVG - OM with Runthrough NS Floppy. We performed pre-dilatation at the tightest lesion with NC Emerge 2.0 x 12mm, up to 18 atm. In view of high risk of slow flow or no reflow phenomenon in SVG intervention, we inserted FilterWire EZ™ Embolic Protection System and removed Runthrough NS Floppy. We further prepared the lesion with NC Genoss 3.0 x 8mm, up to 14 - 20atm. The SVG - OM was stented with Abluminus 3.5 x 16mm (Drug Eluting Stent), deployed at 10 atm. The Abluminus Drug Eluting Stent (DES) was then post-dilated with NC Genoss 3.75 x 12mm, at 14 - 18atm. FilterWire EZ™ was removed.
Final result was acceptable and TIMI Flow III was observed post-procedure.
Adjunctive use of glycoprotein (GP) IIb/IIIa antagonists in SVG intervention has not been shown to be beneficial and thus it was not prescribed in this case.
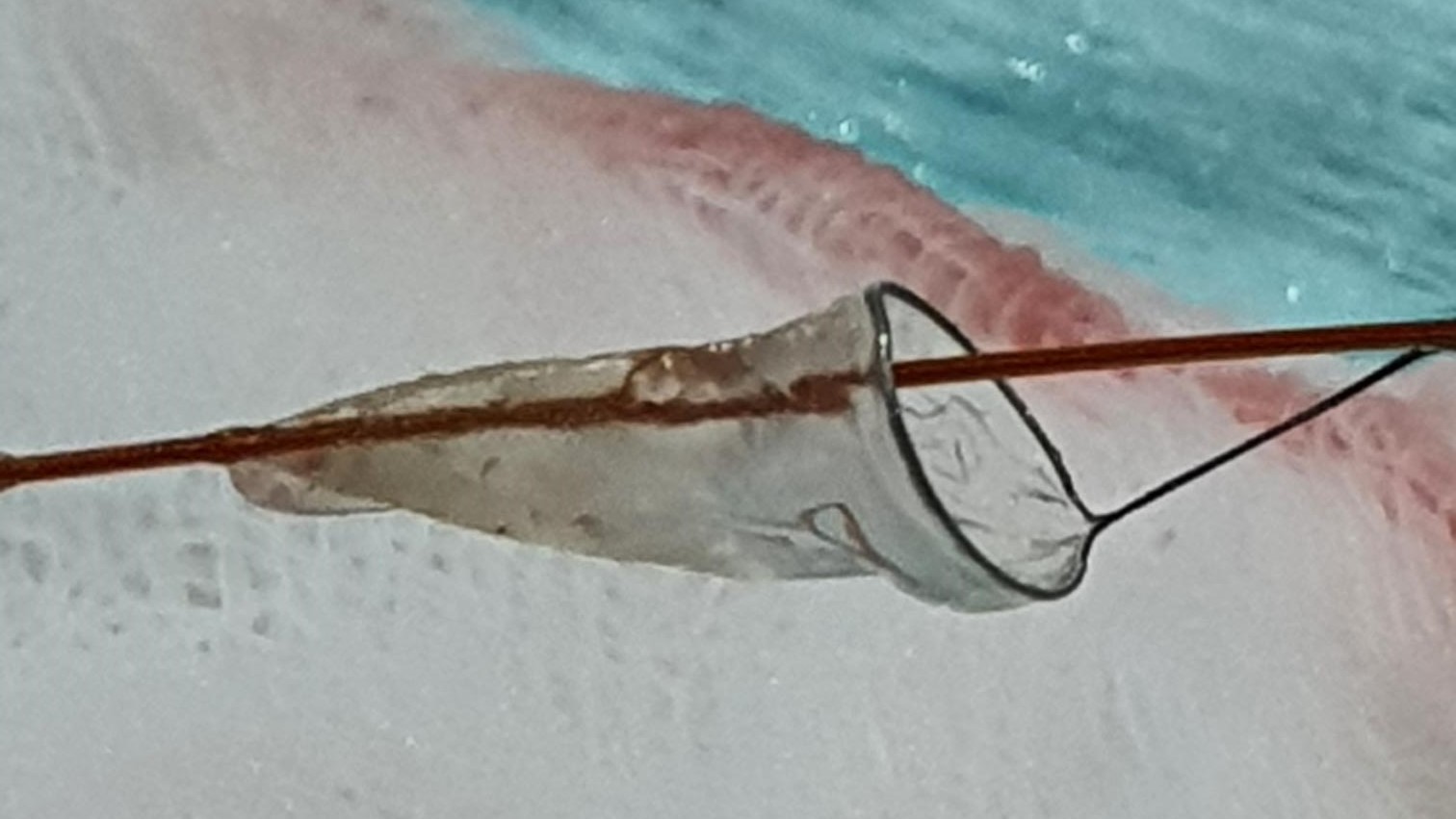
We brought the patient back to the catheterization lab after 1 week of subcutaneous Enoxaparin for percutaneous coronary intervention to the Saphenous Vein Graft (SVG) - Obtuse Marginal (OM). We gained vascular access through the right radial artery with slender sheath. We engaged the SVG - OM with JR4 7Fr. Coronary angiography showed minimal residual thrombus in the SVG - OM. We wired into the SVG - OM with Runthrough NS Floppy. We performed pre-dilatation at the tightest lesion with NC Emerge 2.0 x 12mm, up to 18 atm. In view of high risk of slow flow or no reflow phenomenon in SVG intervention, we inserted FilterWire EZ™ Embolic Protection System and removed Runthrough NS Floppy. We further prepared the lesion with NC Genoss 3.0 x 8mm, up to 14 - 20atm. The SVG - OM was stented with Abluminus 3.5 x 16mm (Drug Eluting Stent), deployed at 10 atm. The Abluminus Drug Eluting Stent (DES) was then post-dilated with NC Genoss 3.75 x 12mm, at 14 - 18atm. FilterWire EZ™ was removed.
Final result was acceptable and TIMI Flow III was observed post-procedure.
Adjunctive use of glycoprotein (GP) IIb/IIIa antagonists in SVG intervention has not been shown to be beneficial and thus it was not prescribed in this case.
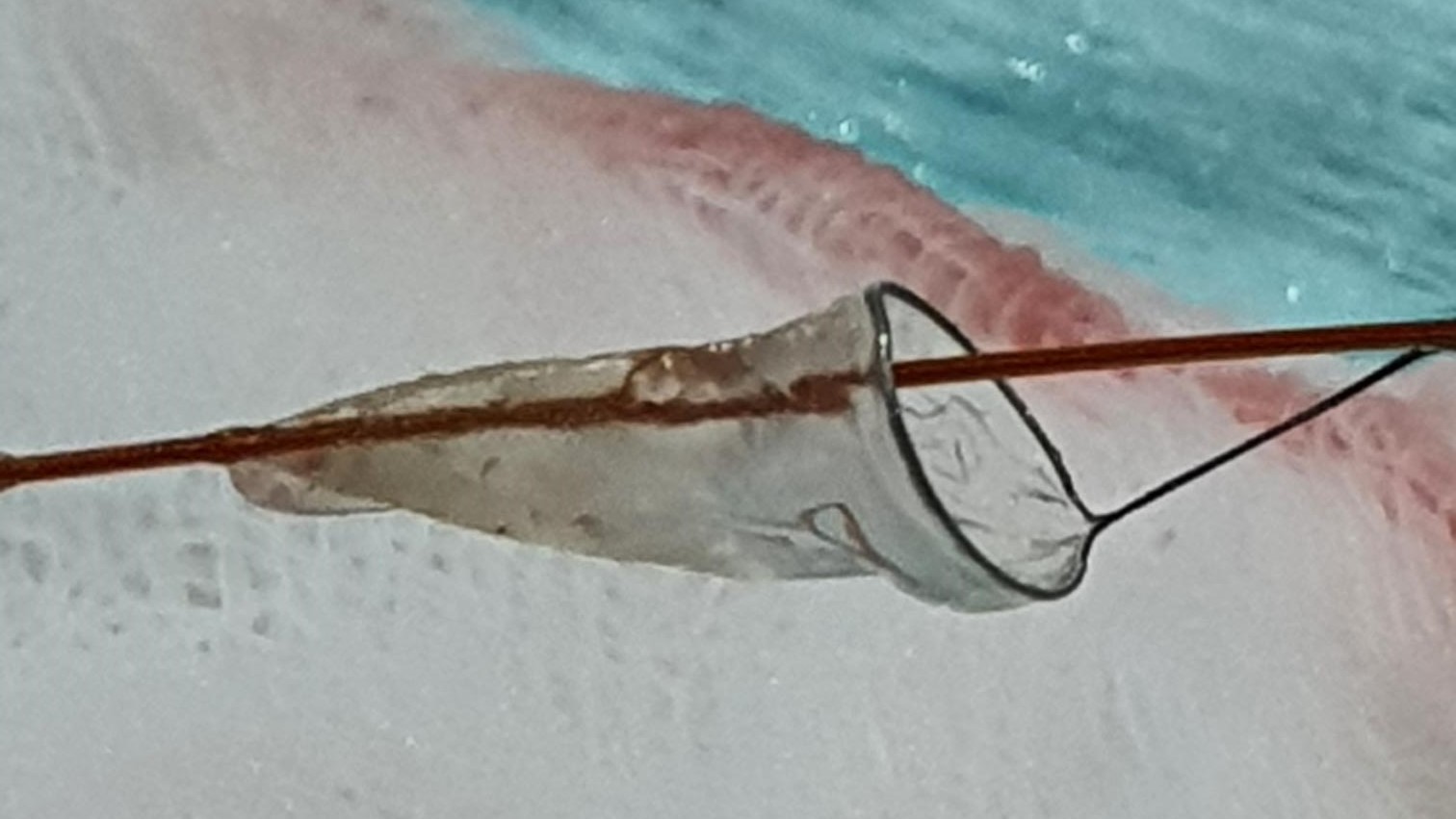
Case Summary
Saphenous vein graft (SVG) intervention remains a challenging revascularization procedure, with a higher risk of slow reflow or no reflow phenomenon and periprocedural myocardial infarction, due to the higher risk of distal embolization of atherothrombotic debris within the degenerated SVG. In SVG with heavy thrombus burden, deferred stenting is an important strategy and prescription of subcutaneous anticoagulant is effective in reducing the thrombus load and ameliorate the risk of slow flow or no reflow phenomenon. Embolic protection system proved to be effective and provides better outcome in SVG intervention.


