Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-157
When It Rains, It Pours!
By Bernard Wong
Presenter
Bernard Wong
Authors
Bernard Wong1
Affiliation
North Shore Hospital, New Zealand1,
View Study Report
TCTAP C-157
Coronary - Complication Management
When It Rains, It Pours!
Bernard Wong1
North Shore Hospital, New Zealand1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 63-year-old man was assessed in the cardiology clinic with crescendo effort angina over the last six months. Past medical history notable for hypertension, dyslipidaemia and ischaemic heart disease; with invasive angiogram 11 years prior showing moderate proximal left circumflex (LCX) stenosis and mild distal left main stem (LMS) stenosis. Vital signs and physical examination were unremarkable.


Relevant Test Results Prior to Catheterization
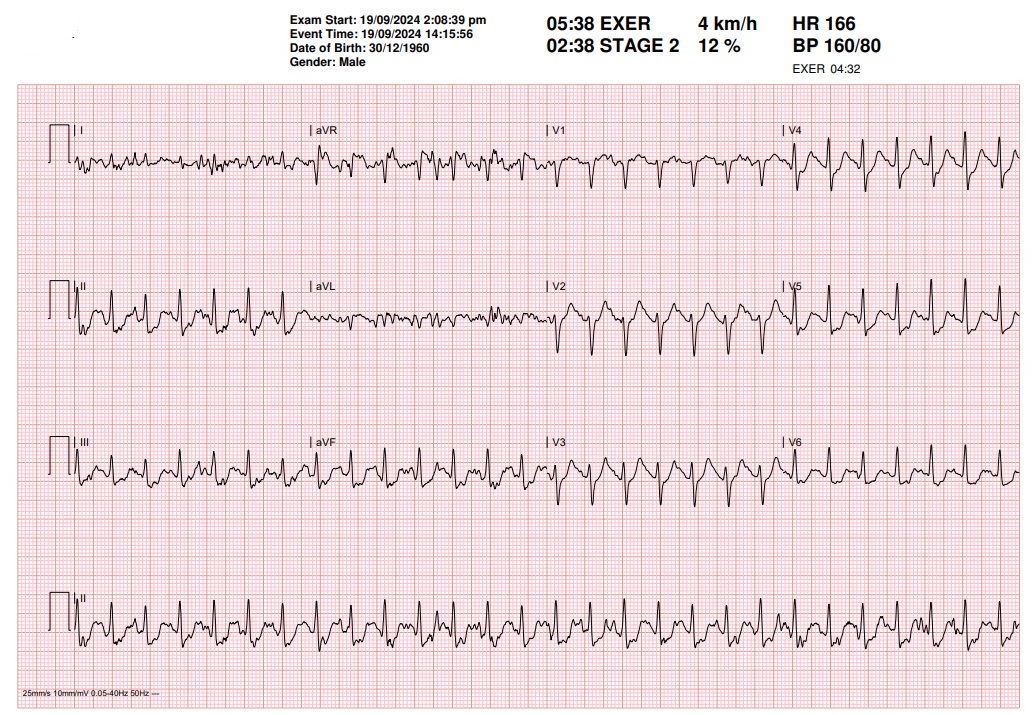
The patient performed 5 minutes and 40 seconds on the exercise treadmill test, which was positive for ischaemic ECG changes and chest pain from stage 2. He was subsequently referred for an invasive coronary angiogram.
Relevant Catheterization Findings
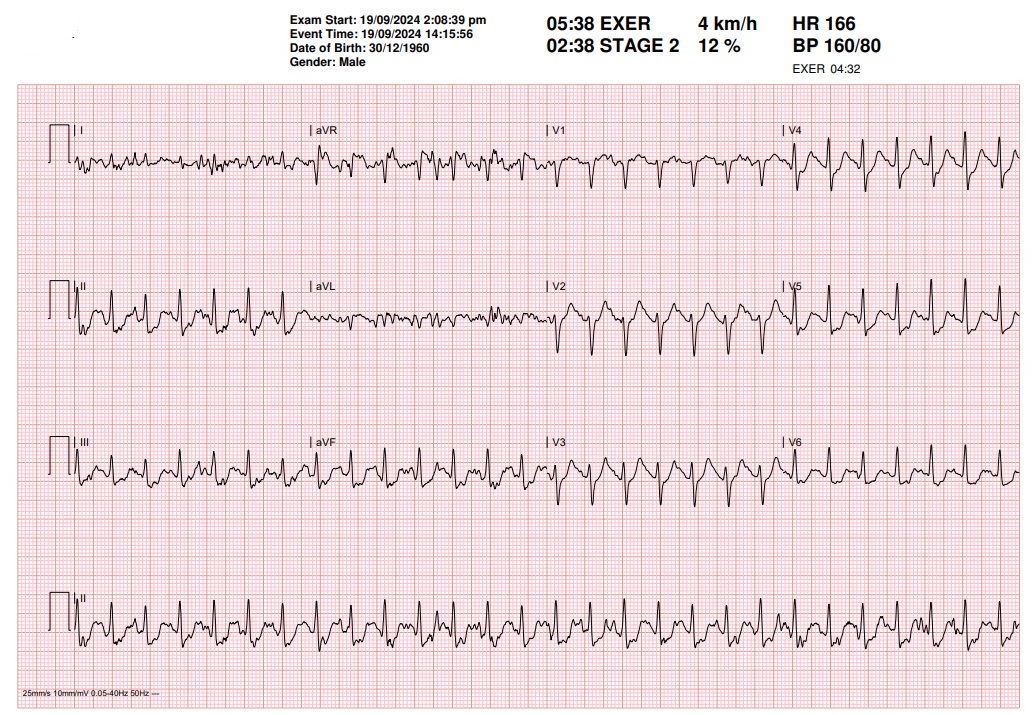
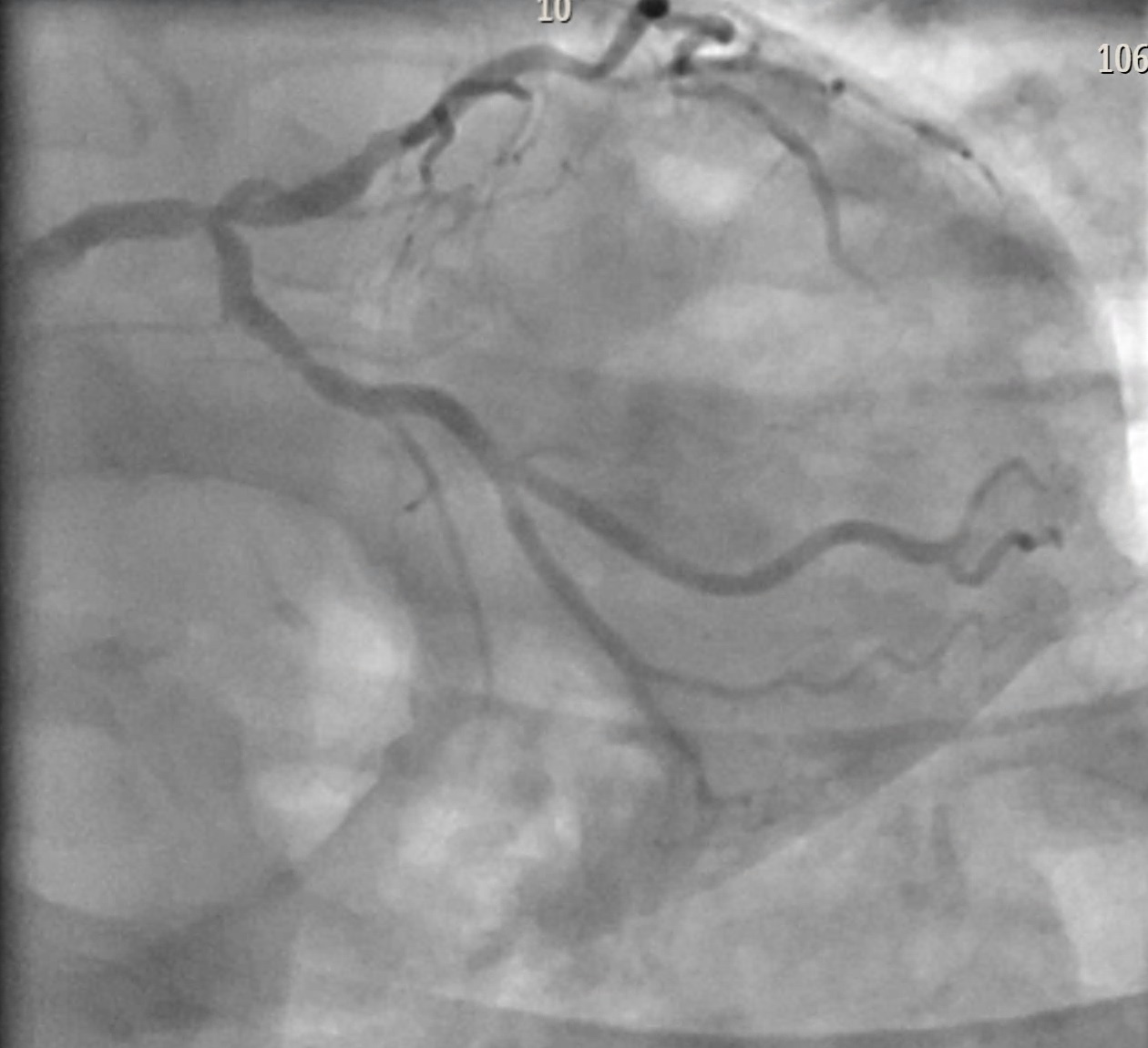
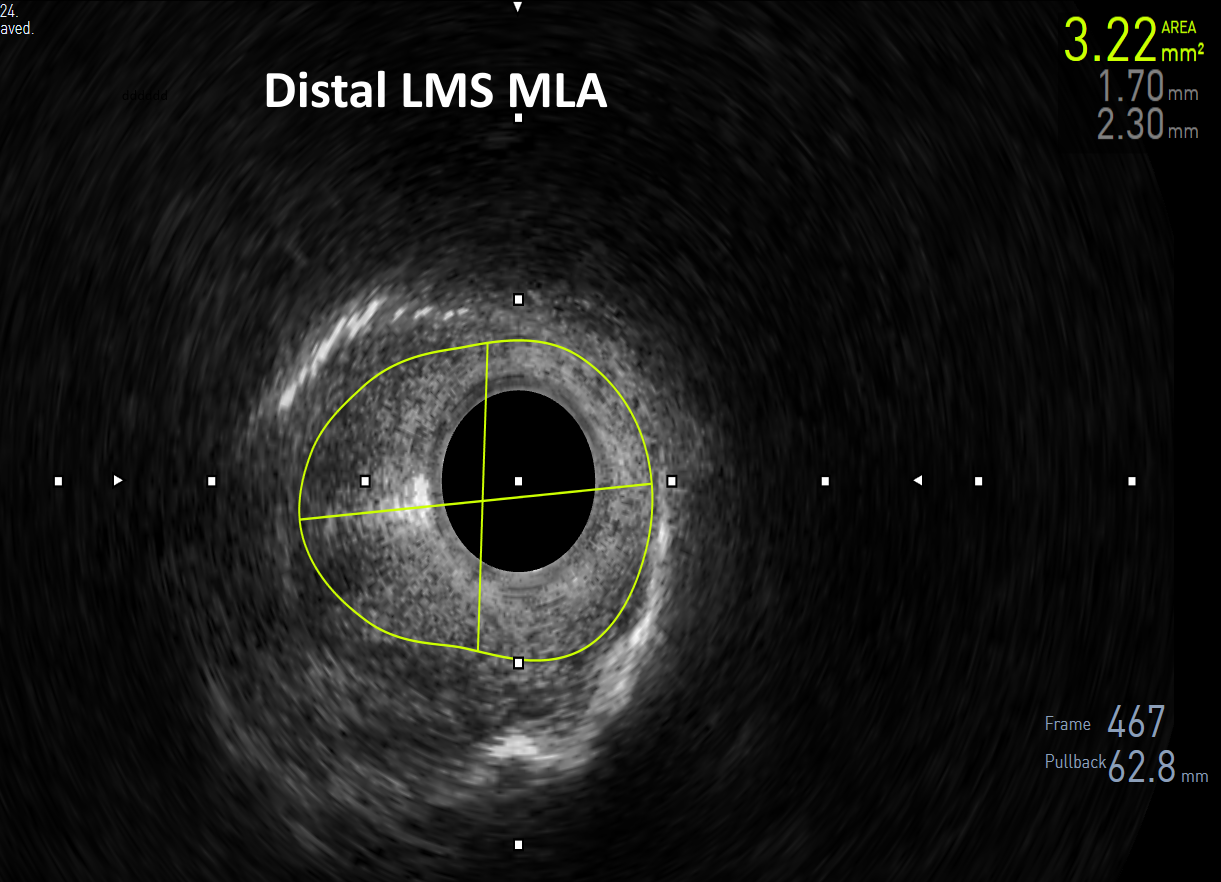
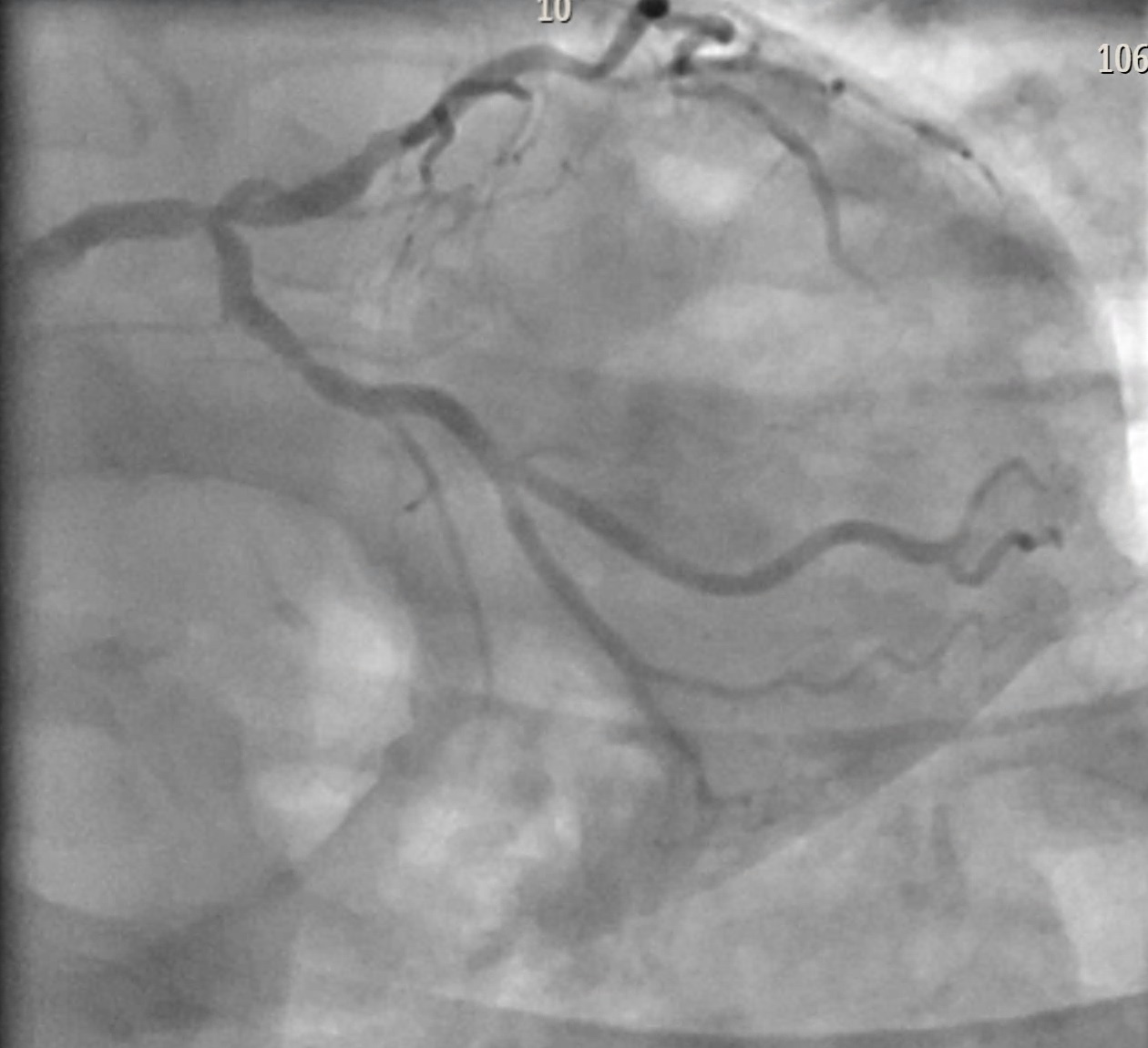
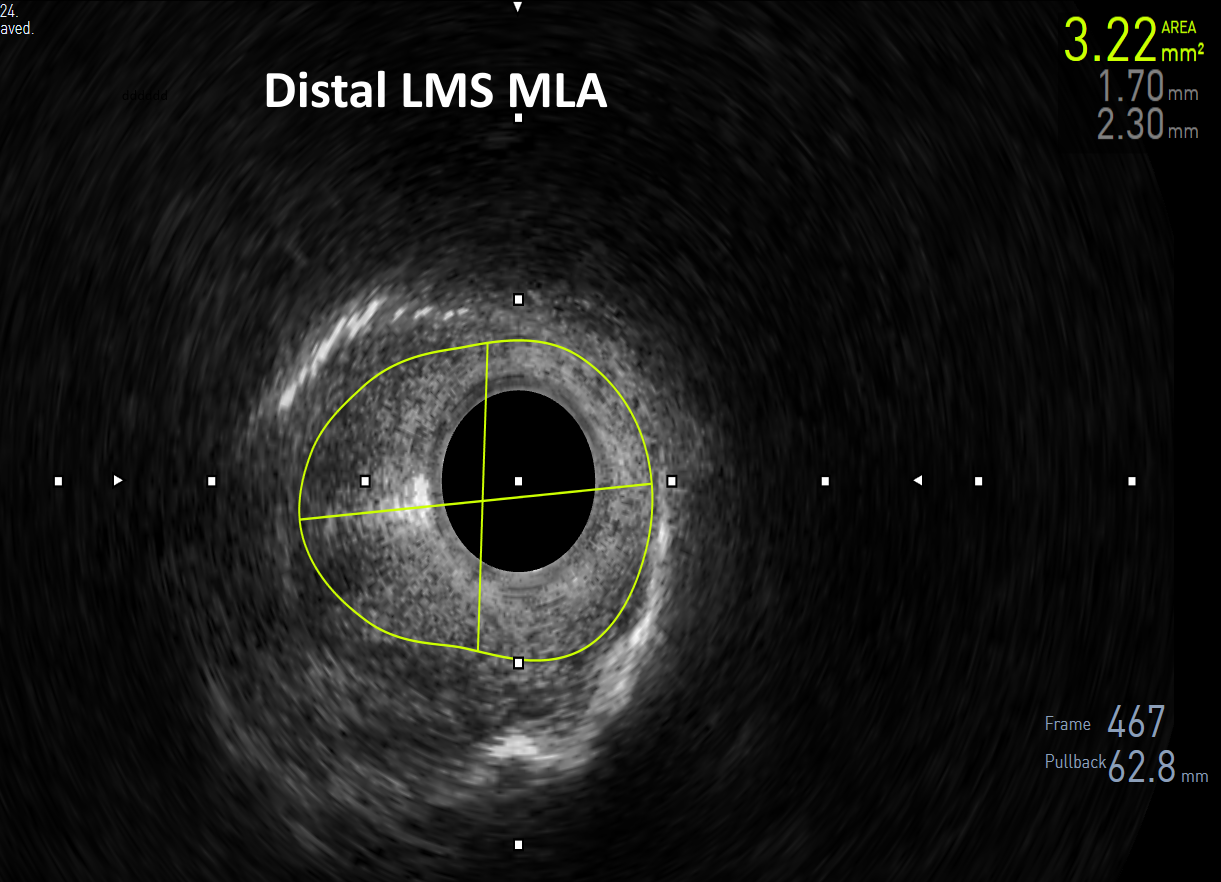
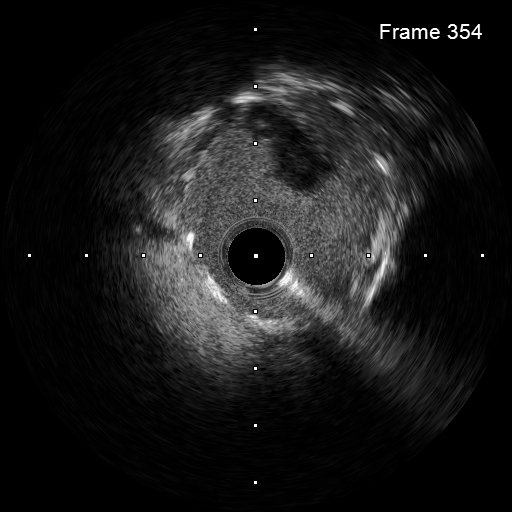
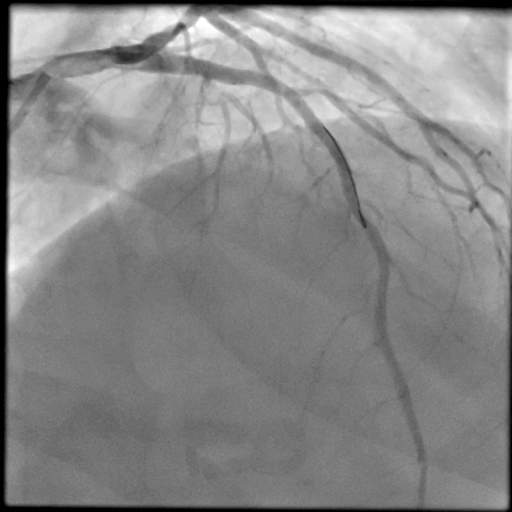
Angiography revealed complex left main bifurcation disease (medina 1,1,1), significant stenoses of the proximal LCX and mid left anterior descending artery (LAD). There was mild disease in the right coronary artery. The SYNTAX score was 30, and the patient opted for revascularization with percutaneous coronary intervention (PCI). IVUS pullback from the LAD and LCX were performed, confirming significant distal LMS stenosis with minimal lumen area of 3.22mm2.


Interventional Management
Procedural Step
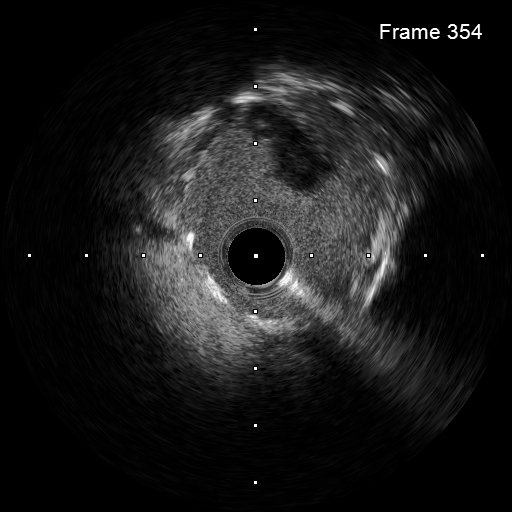
The mid-LAD was predilated first using a 3.0mm non-compliant balloon. During predilatation of the LMS bifurcation and proximal LCX, hold up of contrast was seen in the mid-LAD, and during positioning of the mid-LAD stent, extensive spiral dissection was seen in the distal LAD with TIMI 0 flow, as well as significant left main dissection. Due to chest pain and ST-elevation, the stent was deployed approximately 15mm distal to the originally planned landing zone. Unfortunately, TIMI 0 remained in the distal LAD, and IVUS revealed the dissection extensing 25mm beyond the distal stent edge. The operator was reluctant to do a full metal jacket in the LAD which would limit future CABG options, so a 2.5mm cutting balloon and 2.5 x30mm drug coated balloon was used. However, this was unsuccessful to restore flow, and IVUS revealed distal extension of the dissection. A 2.25 x 16mm DES was deployed to cover the distal end of the dissection, and the cutting balloon was inflated numerous times in the dissected segment between the stents to fenestrate the haematoma to restore flow. PCI of the LMS bifurcation was completed using a TAP 2-stent technique with good final results.
An hour after the procedure, the patient developed acute chest pain with anterior ST-elevation. Repeat angiography which revealed extensive acute stent stent thrombosis in the LMS and LAD. Additional heparin was given, as well as bolus doses of eptifibatide, successfully restoring TIMI 3 flow.

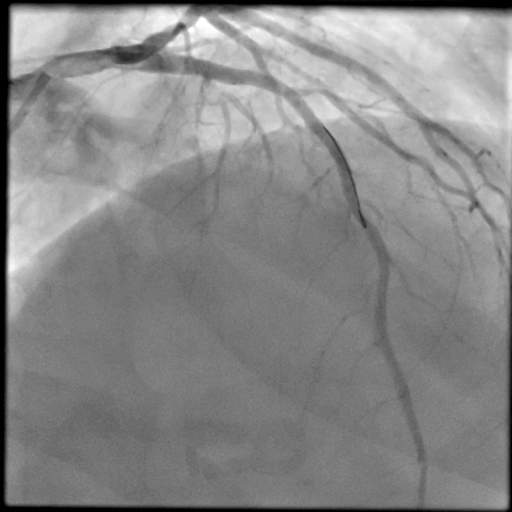
An hour after the procedure, the patient developed acute chest pain with anterior ST-elevation. Repeat angiography which revealed extensive acute stent stent thrombosis in the LMS and LAD. Additional heparin was given, as well as bolus doses of eptifibatide, successfully restoring TIMI 3 flow.

Case Summary
This case demonstrates extensive balloon-related dissections of the LMS and LAD in a vessel which was not significantly calcified. The use of IVUS to identify the distal extent of the spiral dissection allowed the operator to seal the exit with a short stent, while fenestrating the subintimal haematoma with a cutting balloon to restore TIMI 3 flow and maintaining future CABG options. The extensive acute stent thrombosis highlights the patient's thrombogenic state given the dissections and multiple stents. In hindsight, upfront IIB/IIIA inhibitors such as eptifibatide should be used during the first procedure to reduce the risk of this occurring.


