Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-159
A Case of LAD Perforation During Percutaneous Coronary Intervention After Deployment of Drug-Coated Balloon in a Patient With Wellens Syndrome
By Kee Wei Lee, Muhammad Azlan Aseri, Kok Han Chee
Presenter
Kee Wei Lee
Authors
Kee Wei Lee1, Muhammad Azlan Aseri1, Kok Han Chee1
Affiliation
University Malaya Medical Centre, Malaysia1,
View Study Report
TCTAP C-159
Coronary - Complication Management
A Case of LAD Perforation During Percutaneous Coronary Intervention After Deployment of Drug-Coated Balloon in a Patient With Wellens Syndrome
Kee Wei Lee1, Muhammad Azlan Aseri1, Kok Han Chee1
University Malaya Medical Centre, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 78-year old female with background history of diabetes mellitus, hypertension and dyslipidemia, had been having stable angina for past 1 month with worsening chest pain for 2 days. She was pain-free on arrival to Emergency Department. Physical examination was unremarkable and her vital signs were stable.
Relevant Test Results Prior to Catheterization
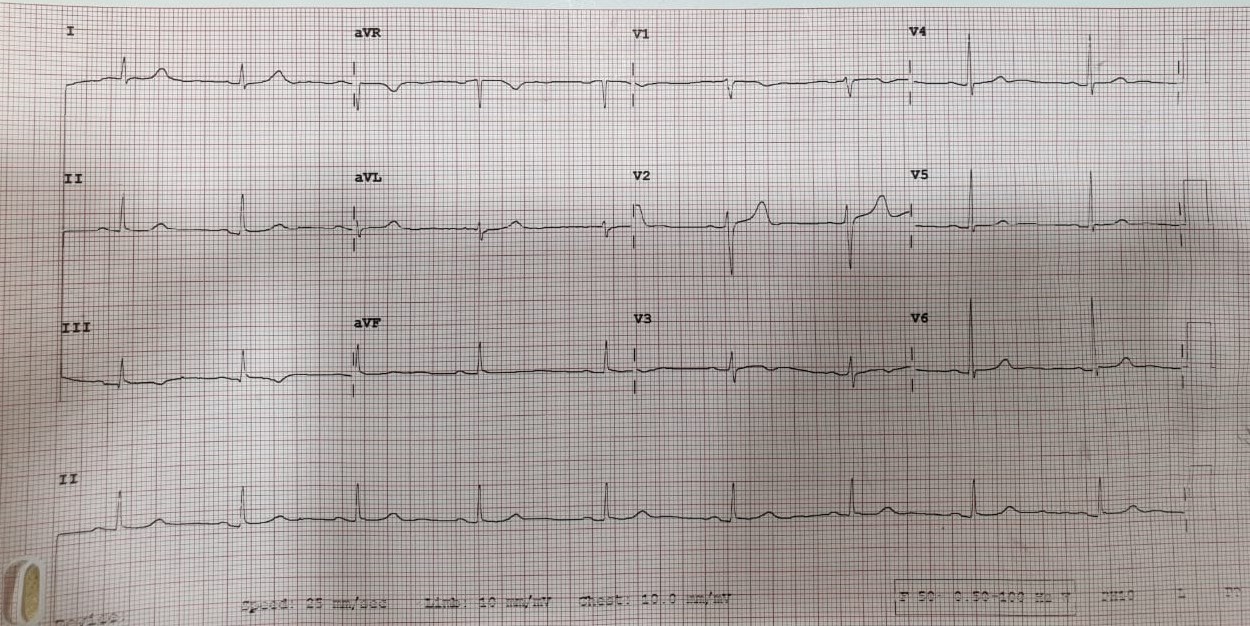
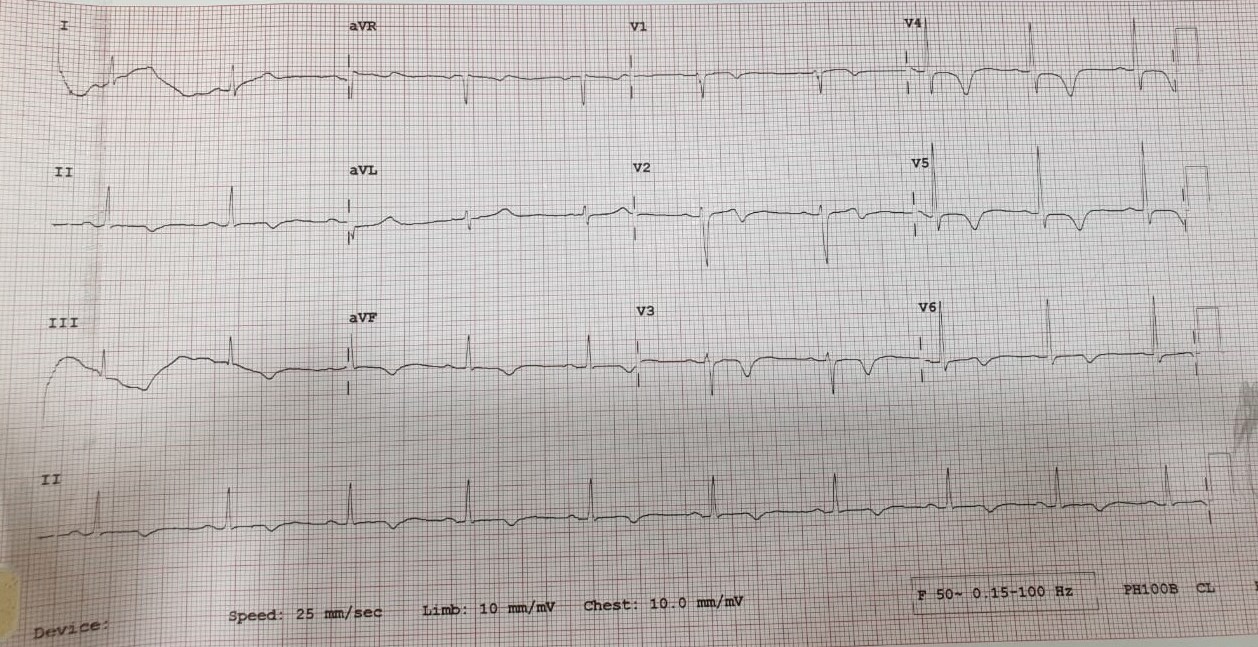
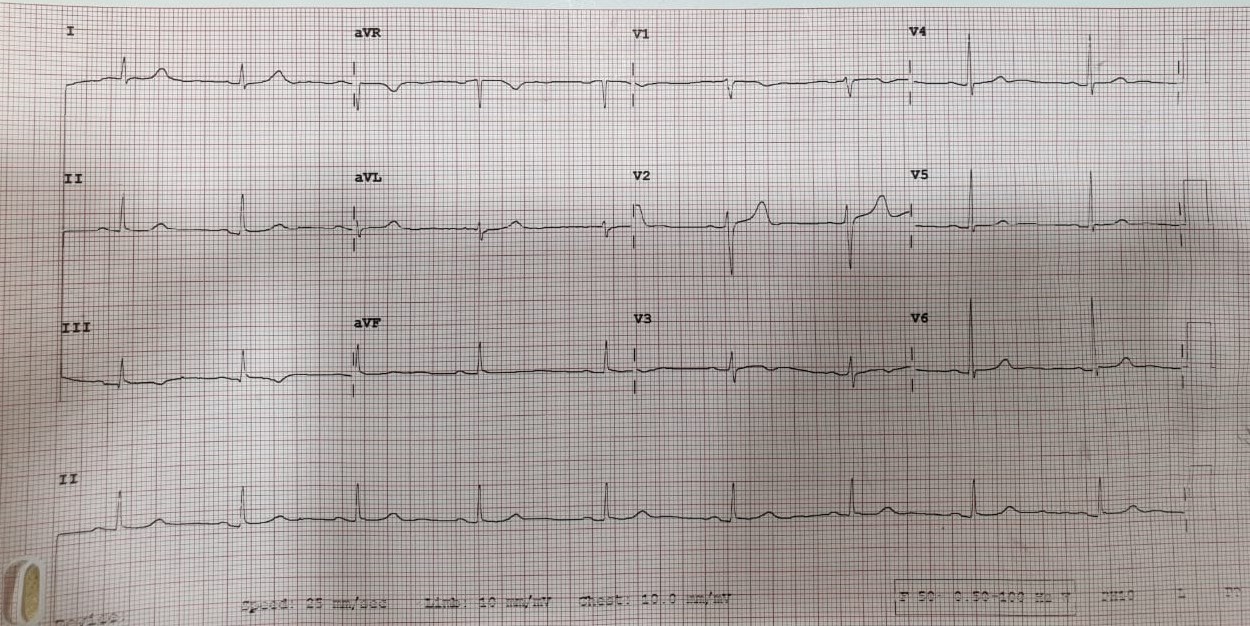
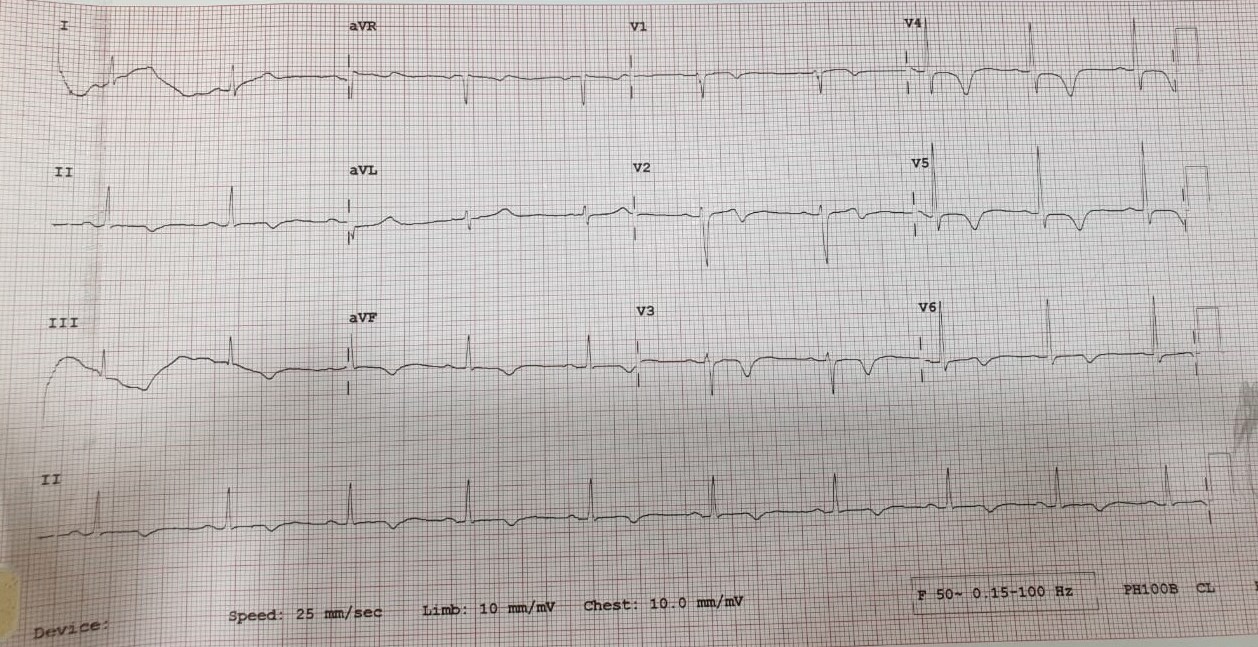
Her hemoglobin, renal and liver function tests were normal. Her troponin I was elevated at 3923 ng/L. Electrocardiogram (ECG) showed sinus rhythm with evolution into Wellens pattern with biphasic T waves in V1-2 and deep T wave inversion in V3-6 and inferior leads as well. 2D-echocardiogram showed preserved ejection fraction.
Relevant Catheterization Findings
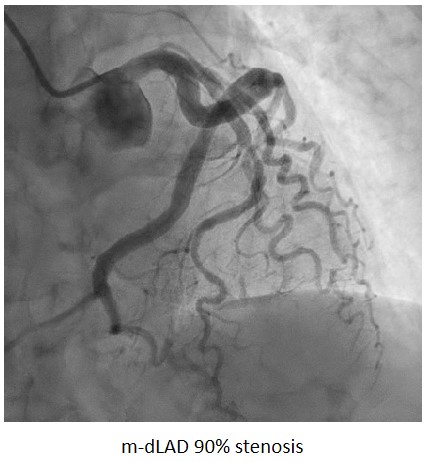
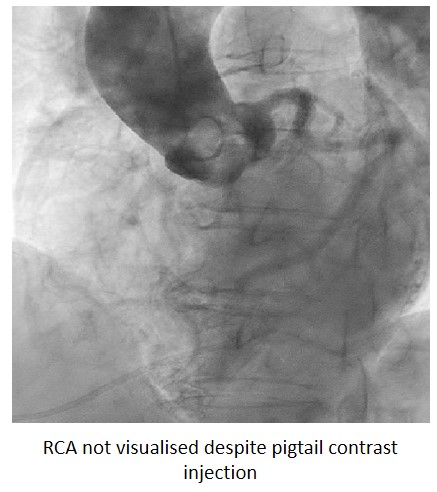
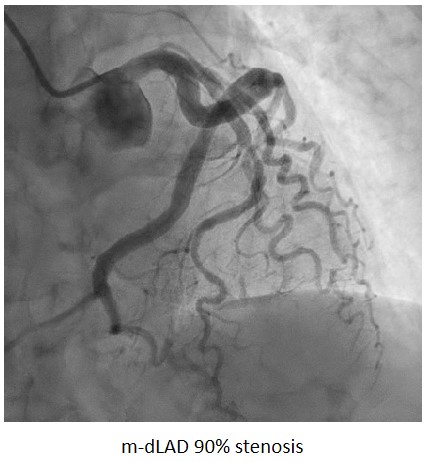
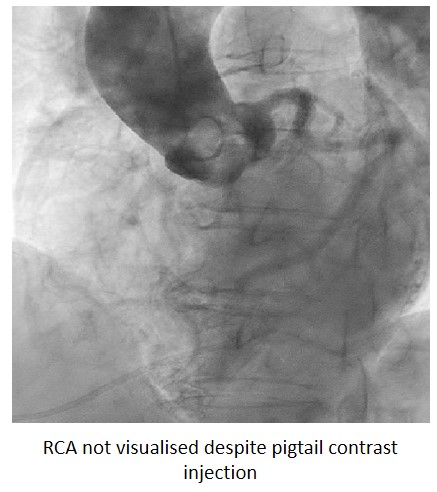
Urgent coronary angiography showed smooth LMCA. There was calcified, critical stenosis at mid- and distal segment of LAD. RCA ostium could not be identified despite pigtail contrast injection. LCx was normal and dominant, supplying the RCA territory as well.
Interventional Management
Procedural Step
Vascular access was obtained with transradial puncture with 6 Fr sheath. Guiding catheter Judkins Left 3.5 (Cordis, USA) 6 Fr was used to engage the left coronary ostium. Runthrough Floppy (Terumo, Japan) coronary wire was wired down LAD with distal vessel tortuosity. Distal-mid LAD lesions were pre-dilated with SC Sapphire (OrbusNeich, China) 2.5 x 15 mm with good vessel preparation. PCI to distal LAD with drug-coated balloon (DCB) SeQuent Please NEO (B. Braun, Germany) 2.75 x 25 mm was performed with inflation up till 6 atm, which was complicated with LAD perforation. Hemodynamics were unstable and emergent bedside ECHO showed massive global pericardial effusion. Immediate bail-out covered stent PK Papyrus (Biotronik, Germany) 2.5 x 20 mm was utilized to seal the perforation and pericardial drain was inserted to relieve cardiac tamponade. Vitals were stabilized after pericardial drainage and PCI to remaining LAD was resumed. Mid LAD lesion was stented with drug-eluting stent (DES) Orsiro Mission (Biotronik, Germany) 3.5 x 18 mm with post-dilatation done with NC Pantera Leo (Biotronik, Germany) 3.0 x 12 mm. Post PCI results were acceptable and bedside ECHO showed no more pericardial effusion. Patient was admitted to CCU for observation and drain was removed 2 days later. She was discharged well with no further complication.
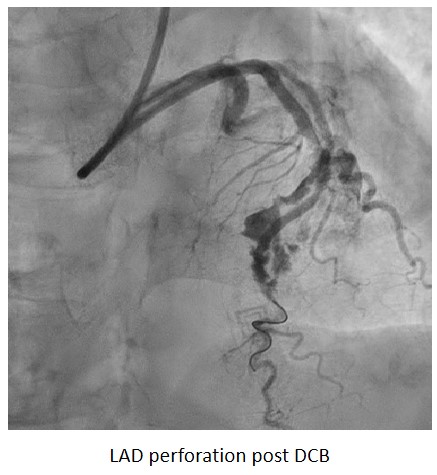
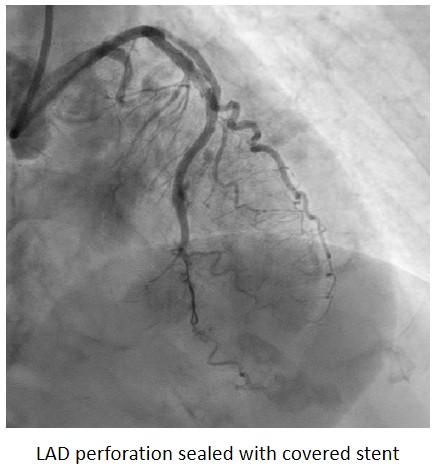
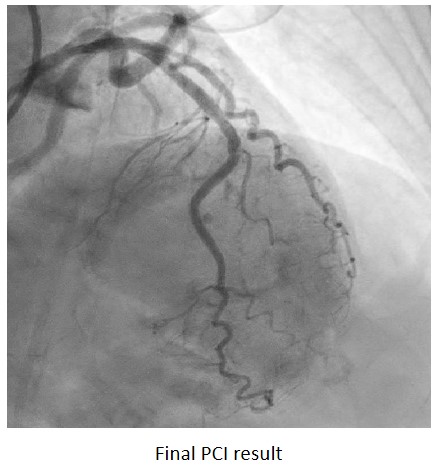
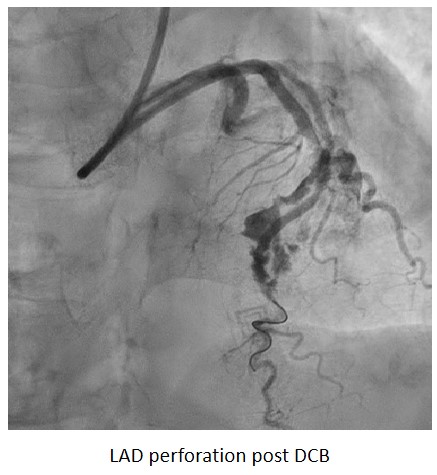
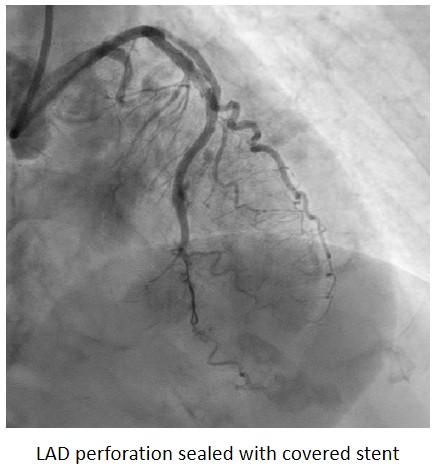
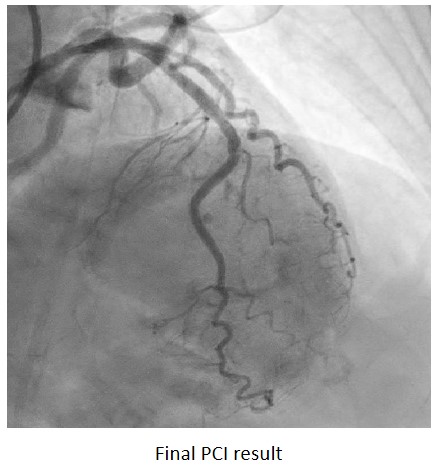
Case Summary
Coronary artery perforation is infrequent but potentially life-threatening complication of PCI. Prompt recognition and bail-out intervention to address this complication is essential to ensure successful outcomes. Stepwise treatment approach for coronary perforation depends on the type, size and mechanism of perforation. For large vessel perforation, use of covered stent provides the definitive treatment which comes with the risk of side branch occlusion. Thus, the availability of covered stent and familiarity of interventionist with its use has enabled this catastrophic complication to be treated percutaneously, avoiding the need for coronary artery bypass surgery.


