Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-161
Nightmare - Save a Life
By Elnura Gardashova, Firdovsi Ibrahimov, Oqtay Musayev, Maryam Gafarova, Sona Qasimzade
Presenter
Elnura Gardashova
Authors
Elnura Gardashova1, Firdovsi Ibrahimov1, Oqtay Musayev1, Maryam Gafarova1, Sona Qasimzade1
Affiliation
Central Clinic Hospital, Azerbaijan1,
View Study Report
TCTAP C-161
Coronary - Complication Management
Nightmare - Save a Life
Elnura Gardashova1, Firdovsi Ibrahimov1, Oqtay Musayev1, Maryam Gafarova1, Sona Qasimzade1
Central Clinic Hospital, Azerbaijan1,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
A 65-year-old male patient presented with complaints of acute chest pain, breathlessness and weakness. The patient had a history of hypertension, hyperlipidemia and cigarette smoking. Physical examination revealed a blood pressure of 135/80 mm Hg, heart rate of 40 beats/min, and no sings of congestion. On admission, he was treated with acetylsalicylic acid, clopidogrel, nitrogliserin and morphine hydrochloride.
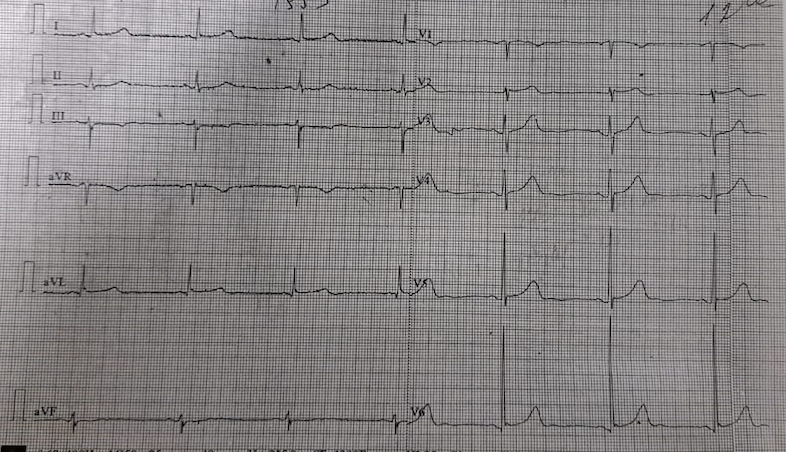
Relevant Test Results Prior to Catheterization
Sinus bradycardia and non-specific changes were recorded in the electrocardiogram. The echocardiogram showed hypokinesia of inferior and lateral left ventricular walls mid, apical segments with an ejection fraction of 45%. Troponin I levels were high.
Relevant Catheterization Findings
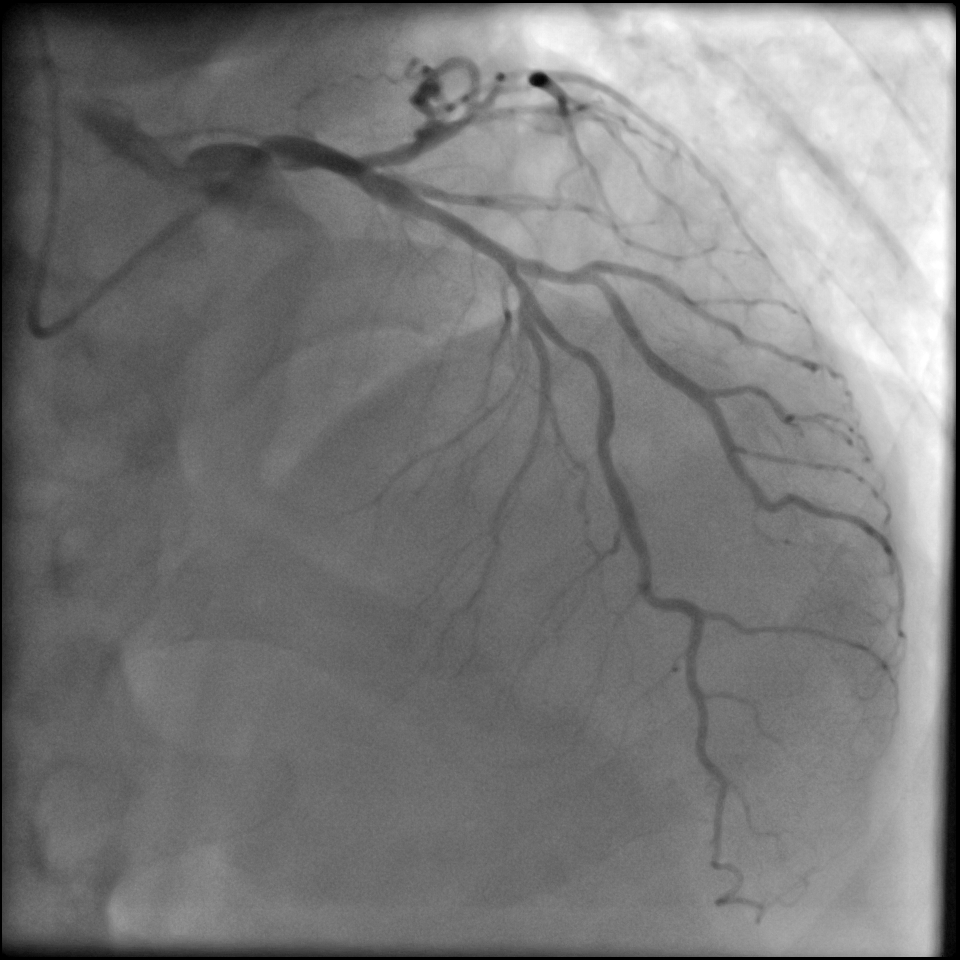
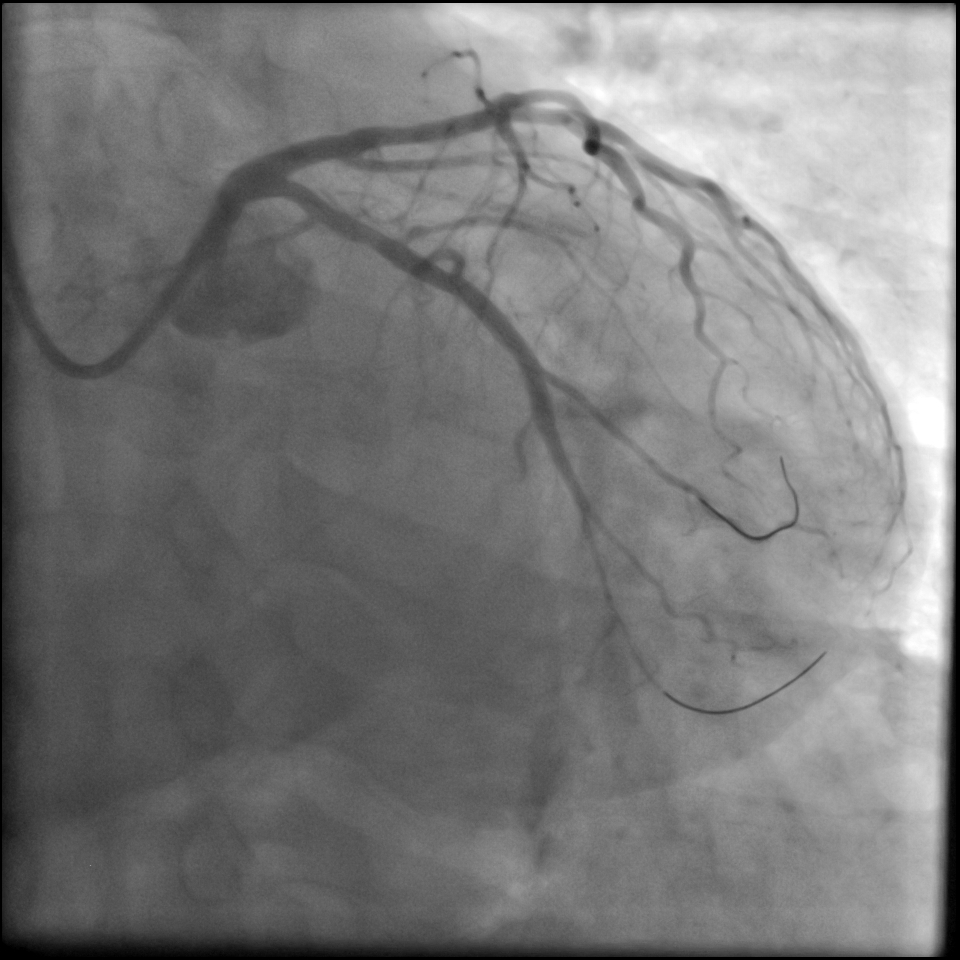
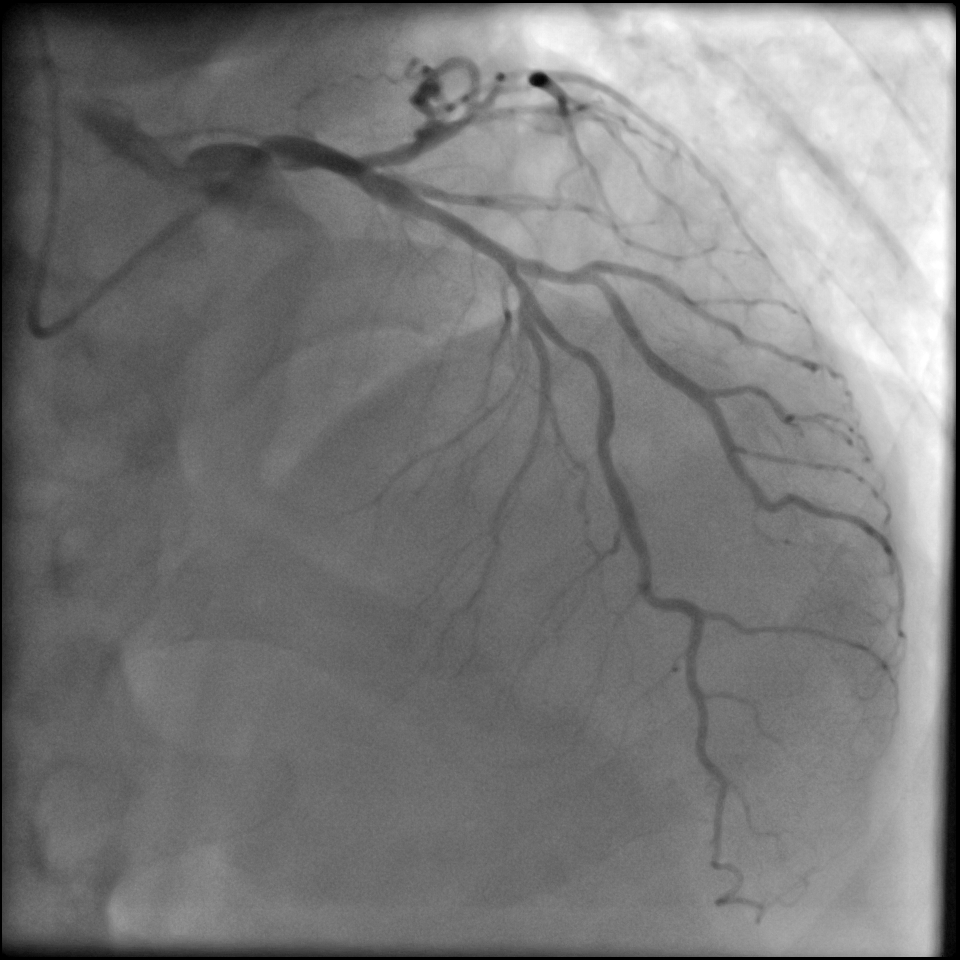
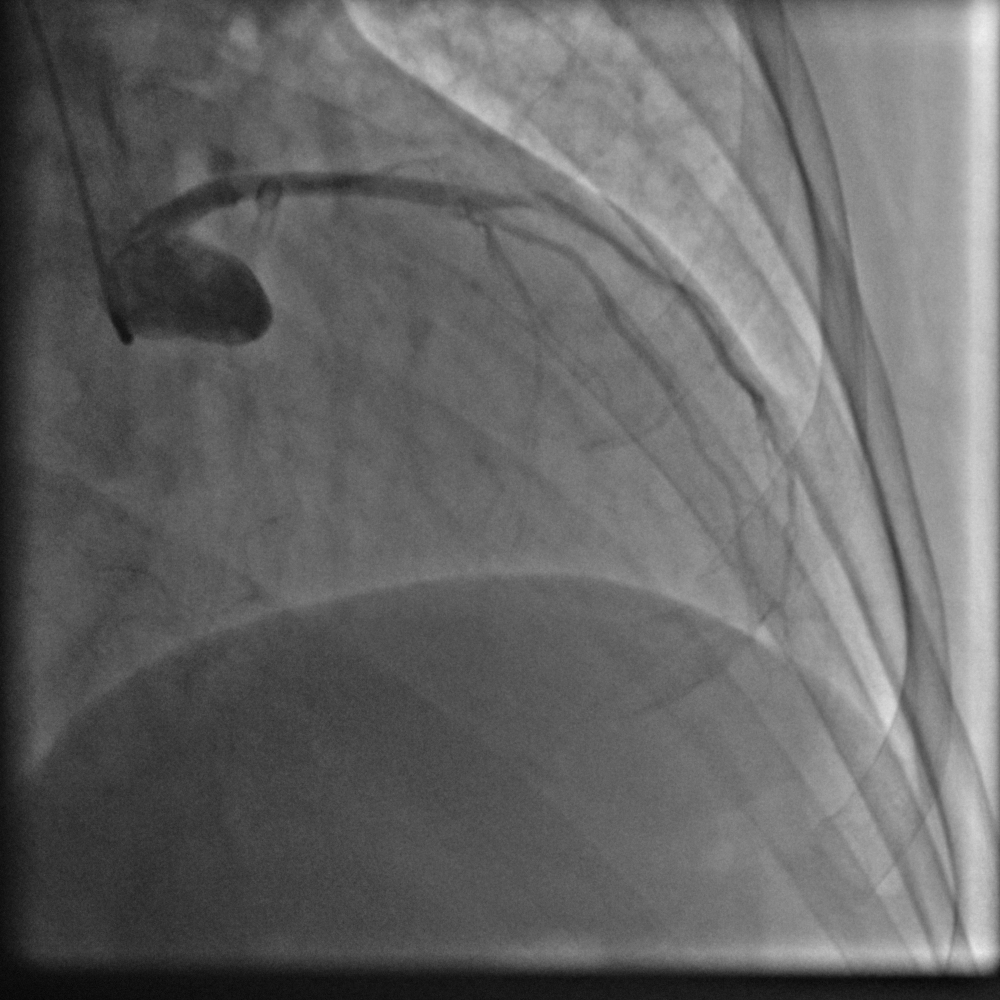
He underwent cardiac catheterization. Coronary angiography showed non significant lesions in LAD and RCA arteries, total occlusion of circumflex (CX) artery. Angiography also revealed diffuse, non obstructive proximal LMCA disease. The decision was made to proceed with a CX intervention.


Interventional Management
Procedural Step
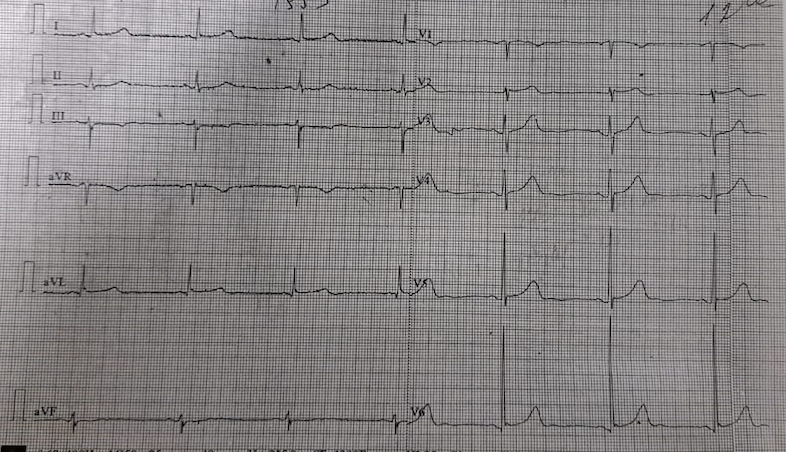
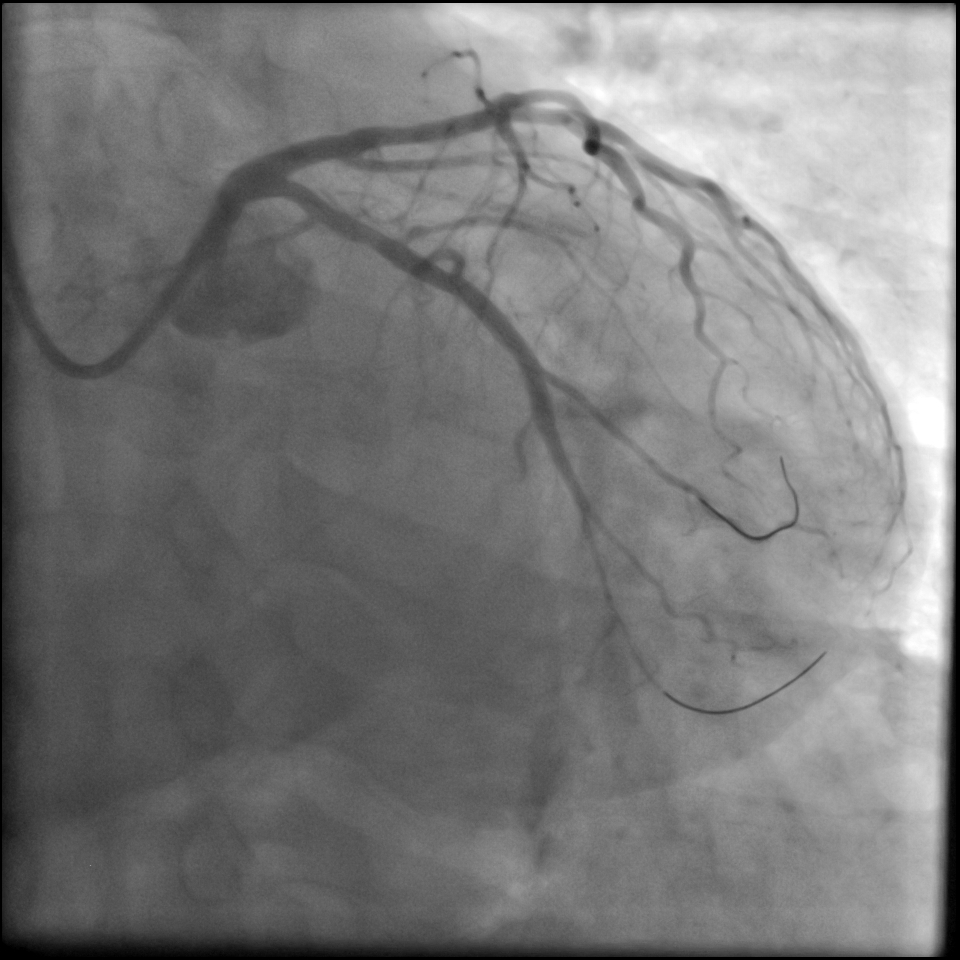
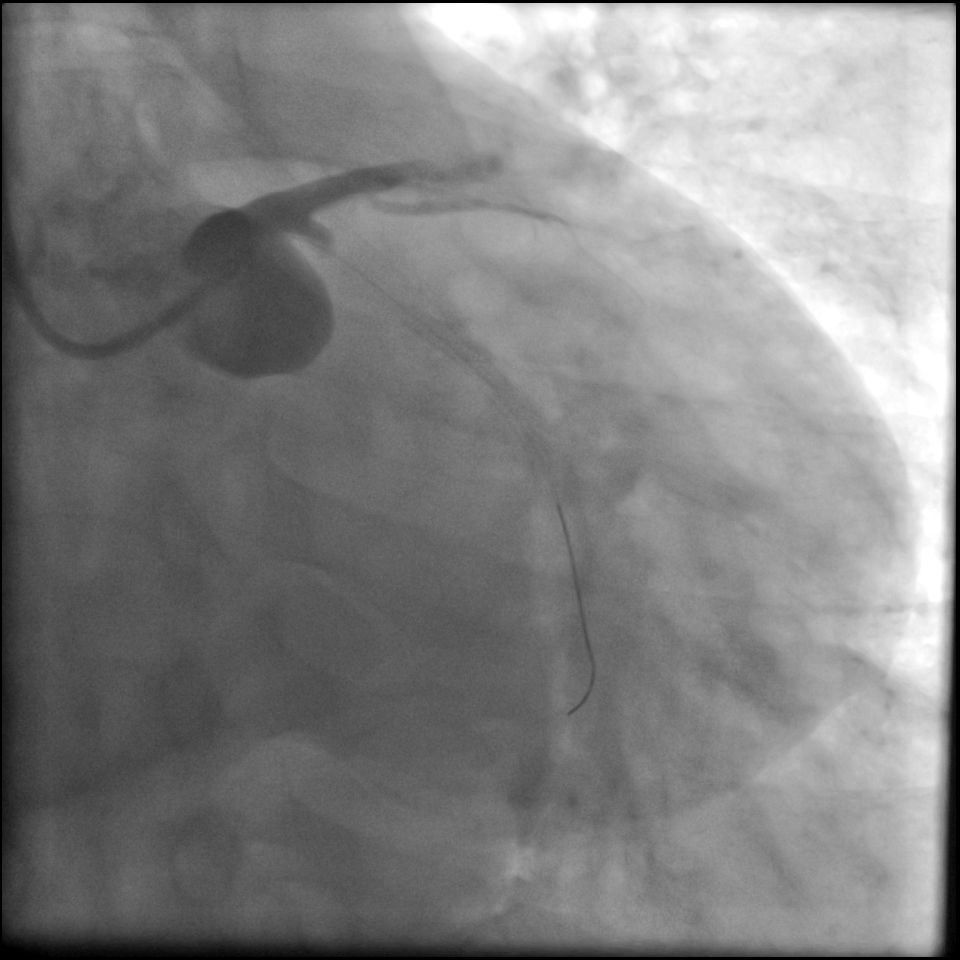
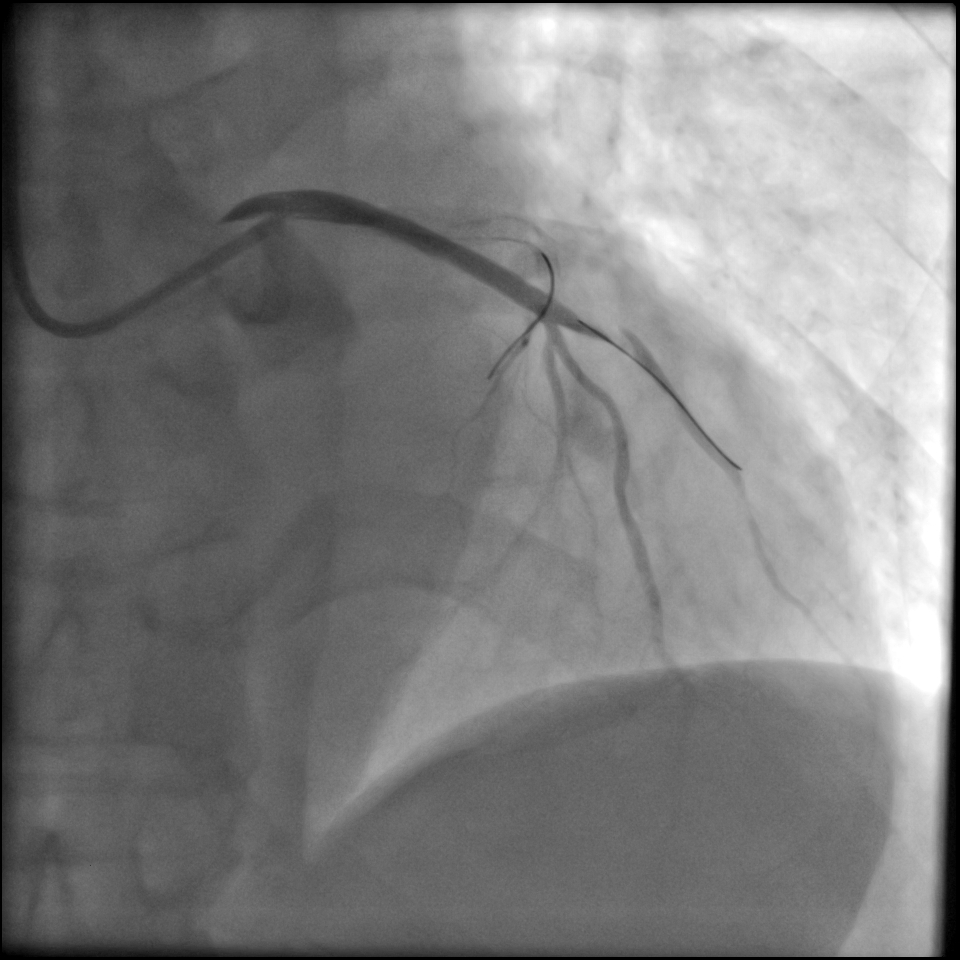
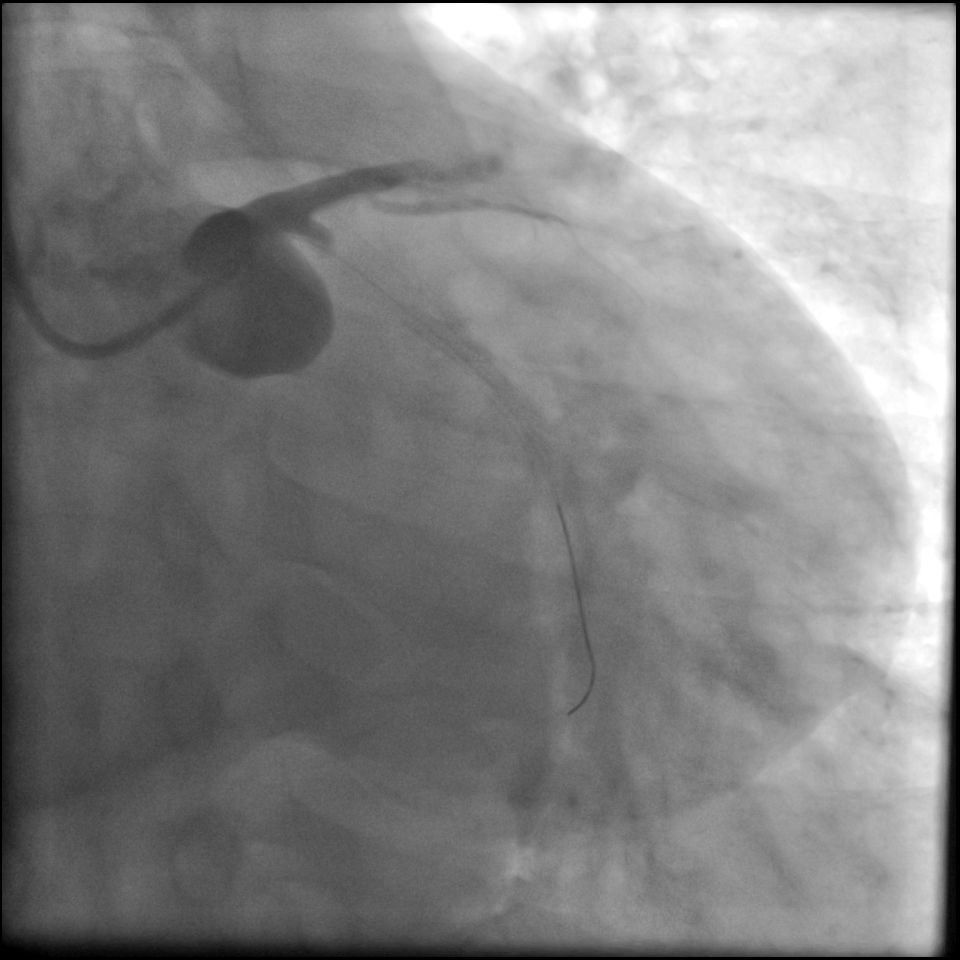
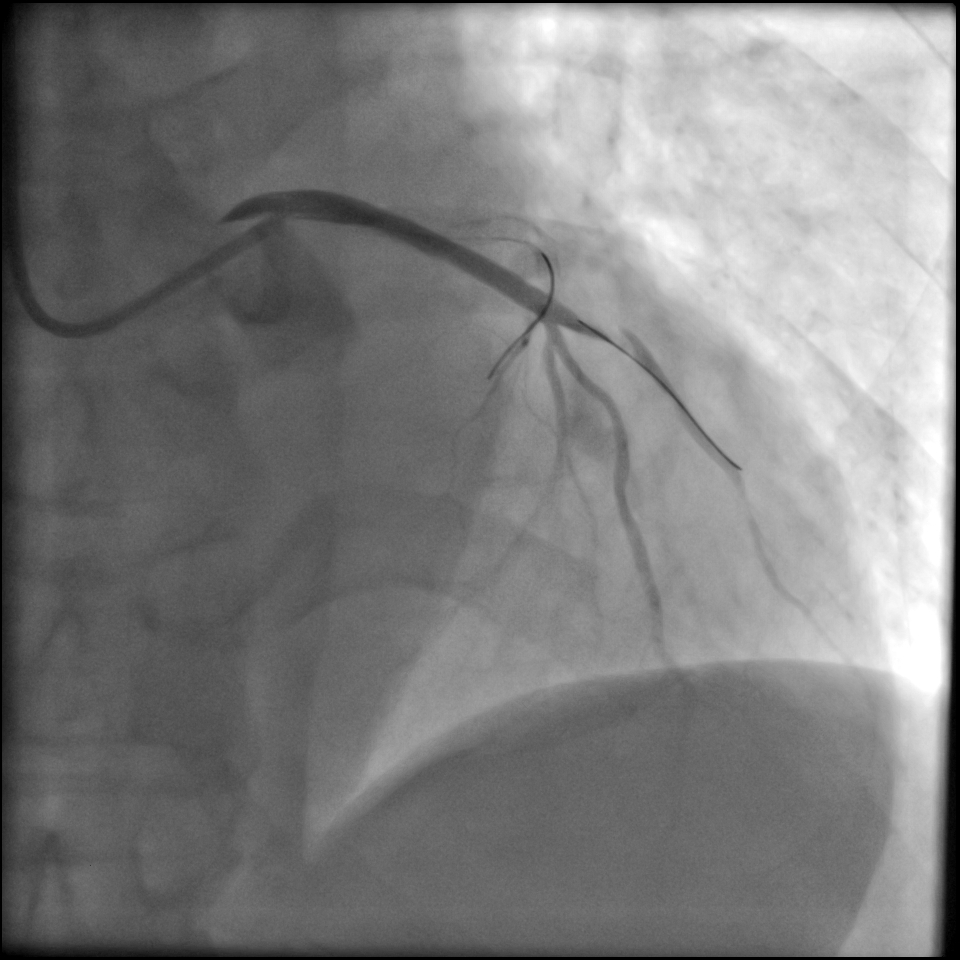
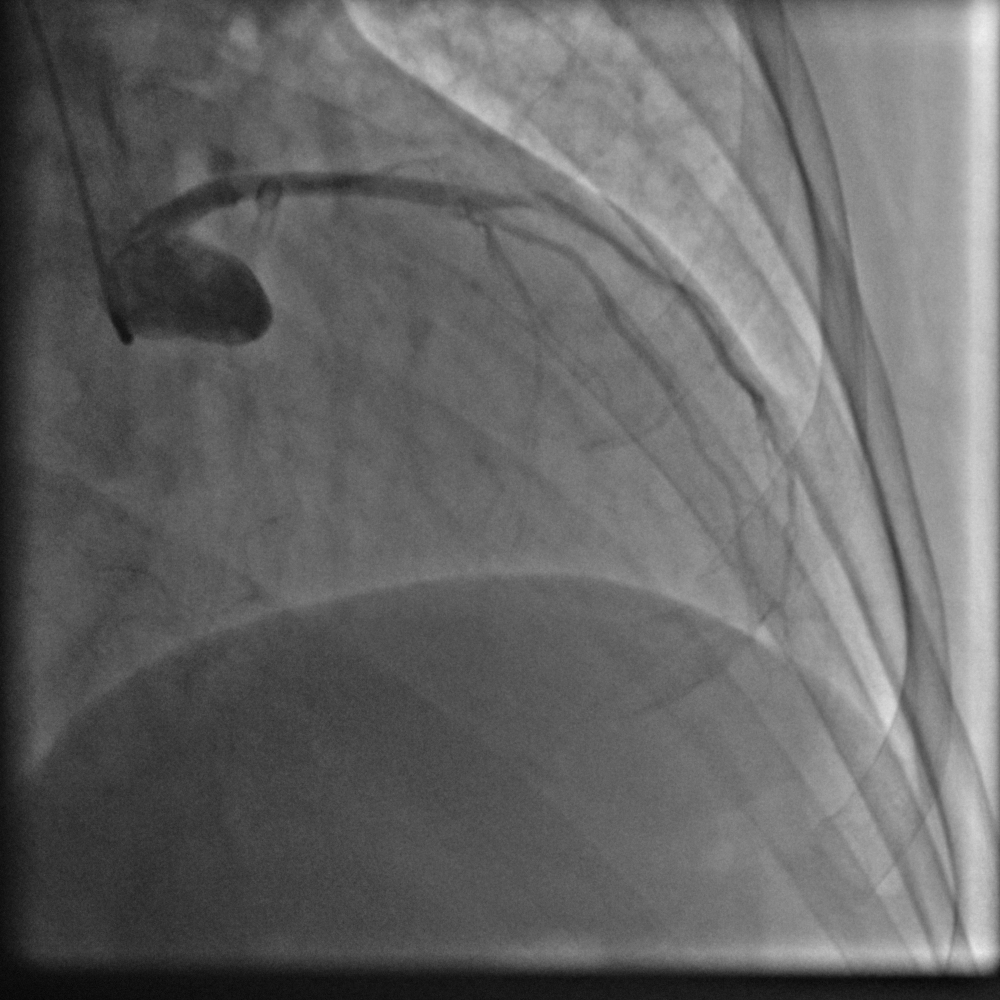
The LMCA was engaged with 6 Fr Extra Back-up (EBU) 3.75 Guiding catheter, using a Runthrough guide wire was successful in crossing CX and OM arteries. After predilatation 3.0 x 38 mm DES was implanted. We performed postdilatation with use of a 3.0 x 12 mm NC balloon. However, a final enjection revealed severe left main coronary artery dissection with antegrade extension, causing LAD, CX occlusion and a retrograde dissection toward the aortic root. The patient complained of chest pain and his electrocardiogram showed ST segment elevation and ventricular tachycardia episodes. Immediately, LAD artery were wired using Runthrough wire. The LAD and LMCA were stented using 4.0 x 38 mm DES. Since the dissection in the aorta was still ongoing, we implanted a second 4.0 x 18 mm DES extended to the aorta. The CX artery could not be wired through the stent sitrats. Since the patient’s hemodynamics could not tolerate long term intervention, we followed up the patient in the intensive care unit. Transthoracic echocardiography did not show any complication such as aortic dissection, regurgitation or pericardial effusion and ejection fraction was 45%. After an hour, the patient’s chest pain and ST segment elevation were resolved. Repeat angiography after a day revealed total occlusion of CX artery, dissection extended from the aorta to the D1 artery under the stent. And we made decision of CABG. After a week he underwent CABG operation. The patient was discharged a week after the operation.
Case Summary
Iatrogenic aorta-coronary dissection is a rare but life-threatening event and one of the most fatal complication of PCI. Deep engagement of the extra support guiding catheter and the use of hydrophilic wires were contributing factors to the LMCA dissection. It should be managed quickly, and requires the coordinated efforts of both cardiologists and surgeons. Bailout PCI for iatrogenic LMCA dissection appears to be safe and feasible with acceptable short and long term outcomes. CABG is a valid treatment strategy in patients without hemodynamic instability or when percutaneous intervention can not be successfully performed promptly.


