TCTAP A-092
Vascular Heart Disease and Cardiomyopathies
Efficacy and Safety of Sodium Glucose Cotransporter-2 Inhibitors for the Treatment of Heart Failure: An Updated Systematic Review and Meta-Analysis
Magdi Yacoub1, Eslam Abdelazim2, Karim Wilson3, Pishoy Sydhom3, Nahla Shehata3, Aziza Mahdi3, Nouran Awwad3, Ahmed Sayed3, Tamer El-Nakhal4, Hesham Elzomor1, Shahram Arsang-Jang5, Sherif Sultan6, Kadir Caliskan7, Osama Soliman1
University of Galway, Egypt1, Misr University for Science and Technology, Egypt2, Ain Shams University, Egypt3, University of Leicester Hospitals, Egypt4, Medical College of Wisconsin, Egypt5, University Hospital Galway, Egypt6, Erasmus University Medical Center, Egypt7
Background
Sodium Glucose Cotransporter-2 inhibitors (SGLT2-i) have been found tohave protective and therapeutic properties in Heart Failure (HF) patients,regardless of ejection fraction.
Methods
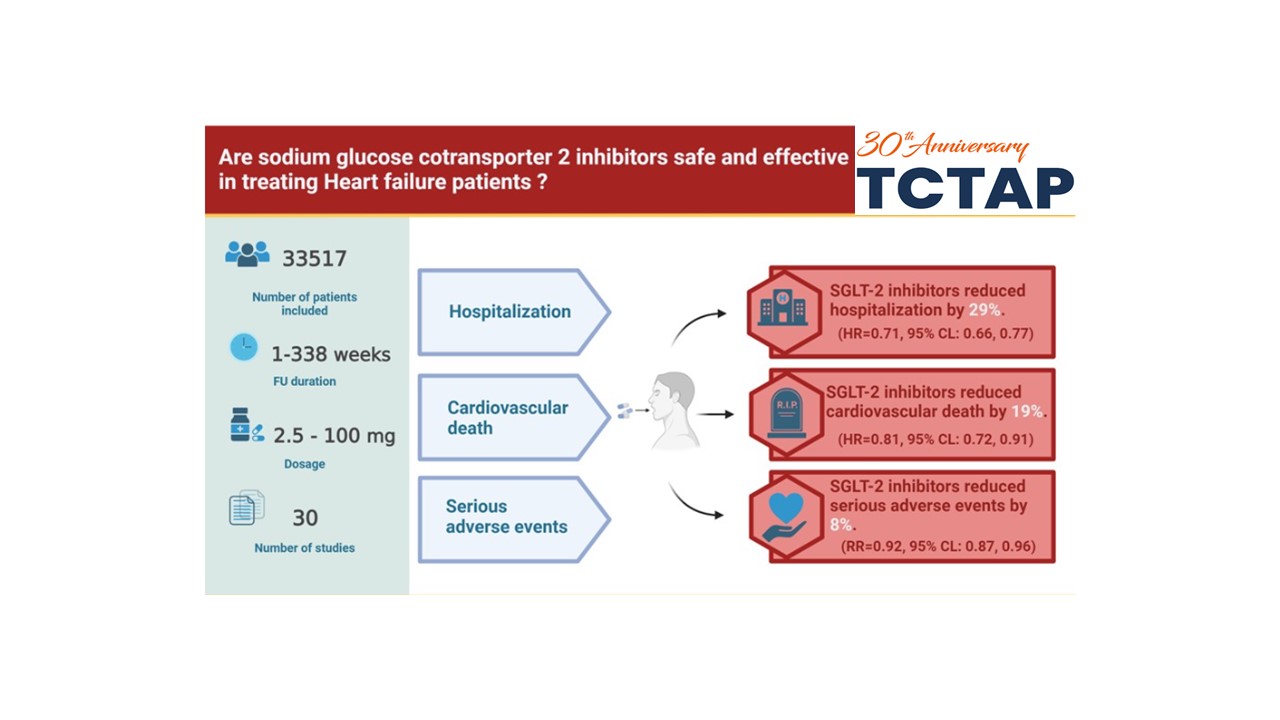
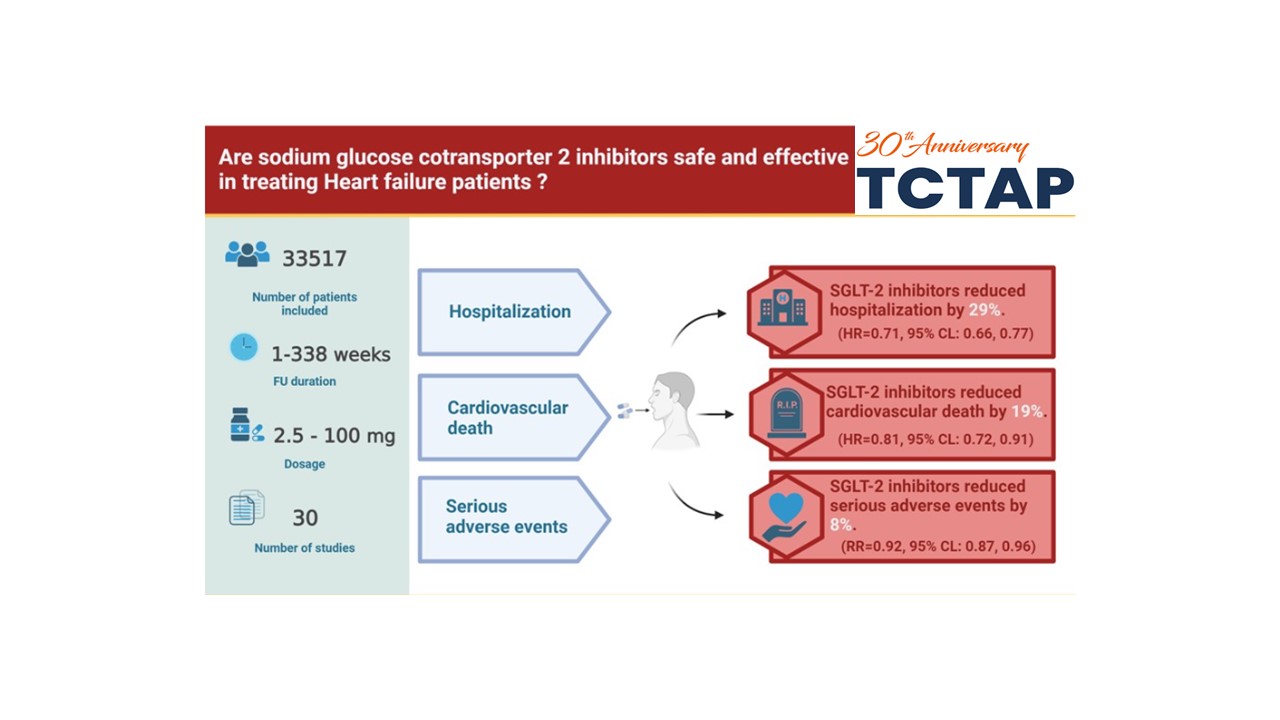
A systematic review and meta-analysis of placebo-controlled randomizedcontrolled trials (RCTs) of SGLT2-i in three groups of HF patients, includingthose with mildly reduced, reduced, or preserved ejection fraction. PubMed,SCOPUS, and Web of Science databases were searched for trials published up tothe 20th of November 2022, using keywords. Data were extracted from publishedreports and bias assessment was performed by the Cochrane risk of bias tool. Wecalculated risk/hazard ratios or mean differences (for dichotomous andcontinuous outcomes; respectively, with corresponding 95% confidence intervals(CI).
Results
A total of 30 RCTs were included. Collectively, 33,517 HF patients,irrespective of the Ejection (EF), were included. Initiation of SGLT2-i inpatients with HF significantly reduced the risk of hospitalization for heartfailure (HHF) (RR=0.74, 95% CI: 0.69, 0.79) and cardiovascular death (RR=0.84,95% CI: 0.77, 0.92). SGLT2-i significantly lowered the death rates and firsthospitalization for heart failure (RR=0.78, 95% CI: 0.74, 0.83). Theysignificantly improved Kansas City clinical summary scores (Meandifference=1.67, 95% CI: 0.56, 2.78) and KCCQ-Total symptom score(MD=3.88, 95%CI: 3.28, 4.47). There was a statistically significant decrease in all-causemortality (RR=0.89, 95% CI: 0.83, 0.96). SGLT2-i reduced the rate of seriousadverse events (RR = 0.92, 95% CI: 0.87, 0.96). SGLT2-i showed bothsimilarities and variations across EF groups. On one hand, the magnitude ofreduction of cardiovascular death was to some extent similar across patientswith HFrEF, HFpEF, and Acute HF (15%, 11%, and 11% relative risk reduction,respectively). But on the other hand, the risk of hospitalization varied acrossthese groups, with reductions of 27%, 19%, and 33%, respectively.
Conclusion
SGLT2inhibitors are safe and effective drugs that reduce the risk of cardiovasculardeath and hospitalization and improve the quality of life of heart failure inpatients with heart failure, irrespective of ejection fraction, supportingtheir role as a foundational therapy for heart failure.