Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-049
A Prospective Observational Study of Diagnostic Accuracy and Feasibility of Quantitative Flow Ratio When Compared to Fractional Flow Reserve
By Joseph O’Brien, Kelly Easey, Eleanor Redwood, Thomas Ford, Jessica Marathe, Peter Psaltis, Jayant Ravindran, Rajan Rehan, Andy Yong, Derek Chew, Adam Brown, Dennis Wong
Presenter
Joseph O’Brien
Authors
Joseph O’Brien1, Kelly Easey2, Eleanor Redwood2, Thomas Ford2, Jessica Marathe3, Peter Psaltis3, Jayant Ravindran4, Rajan Rehan4, Andy Yong4, Derek Chew1, Adam Brown1, Dennis Wong1
Affiliation
Victorian Heart Hospital, Australia1, Gosford Hospital, Australia2, Royal Adelaide Hospital, Australia3, Concord Hospital, Australia4
View Study Report
TCTAP A-049
Angiography/QCA
A Prospective Observational Study of Diagnostic Accuracy and Feasibility of Quantitative Flow Ratio When Compared to Fractional Flow Reserve
Joseph O’Brien1, Kelly Easey2, Eleanor Redwood2, Thomas Ford2, Jessica Marathe3, Peter Psaltis3, Jayant Ravindran4, Rajan Rehan4, Andy Yong4, Derek Chew1, Adam Brown1, Dennis Wong1
Victorian Heart Hospital, Australia1, Gosford Hospital, Australia2, Royal Adelaide Hospital, Australia3, Concord Hospital, Australia4
Background
Fractional flow reserve (FFR)-guided percutaneous coronary intervention (PCI)has been shown to yield superior outcomes to PCI guided by visual assessmentalone in multiple large scale, well-powered studies. However, physiologicalassessment via FFR relies on invasive, wire-based measurements and hyperemia, bothof which are associated with additional complications over diagnostic coronaryangiography. Routine or indiscriminate FFR use was not demonstrated to providepatients or clinicians with improved outcomes in the RIPCORD-2 trial.Quantitative flow ratio (QFR) is a novel, non-invasive, and angiography-derivedindex that provides functional assessment of coronary stenoses through advancedmathematical modeling and known coronary flow dynamics, most saliently withoutthe need for wiring nor hyperemia. It has shown superiority toangiography-guided PCI in FAVOR-III China, and has received a class 1brecommendation in the European Society of Cardiology guidelines for chroniccoronary syndromes. However, the diagnostic accuracy of QFR has never beenassessed at a low framerate, with previous trials universally using framerates ≥15 frames/second to perform their analyses. This is an important considerationas laboratories move to reduce framerates to minimize radiation exposure to bothpatients and staff.
Methods
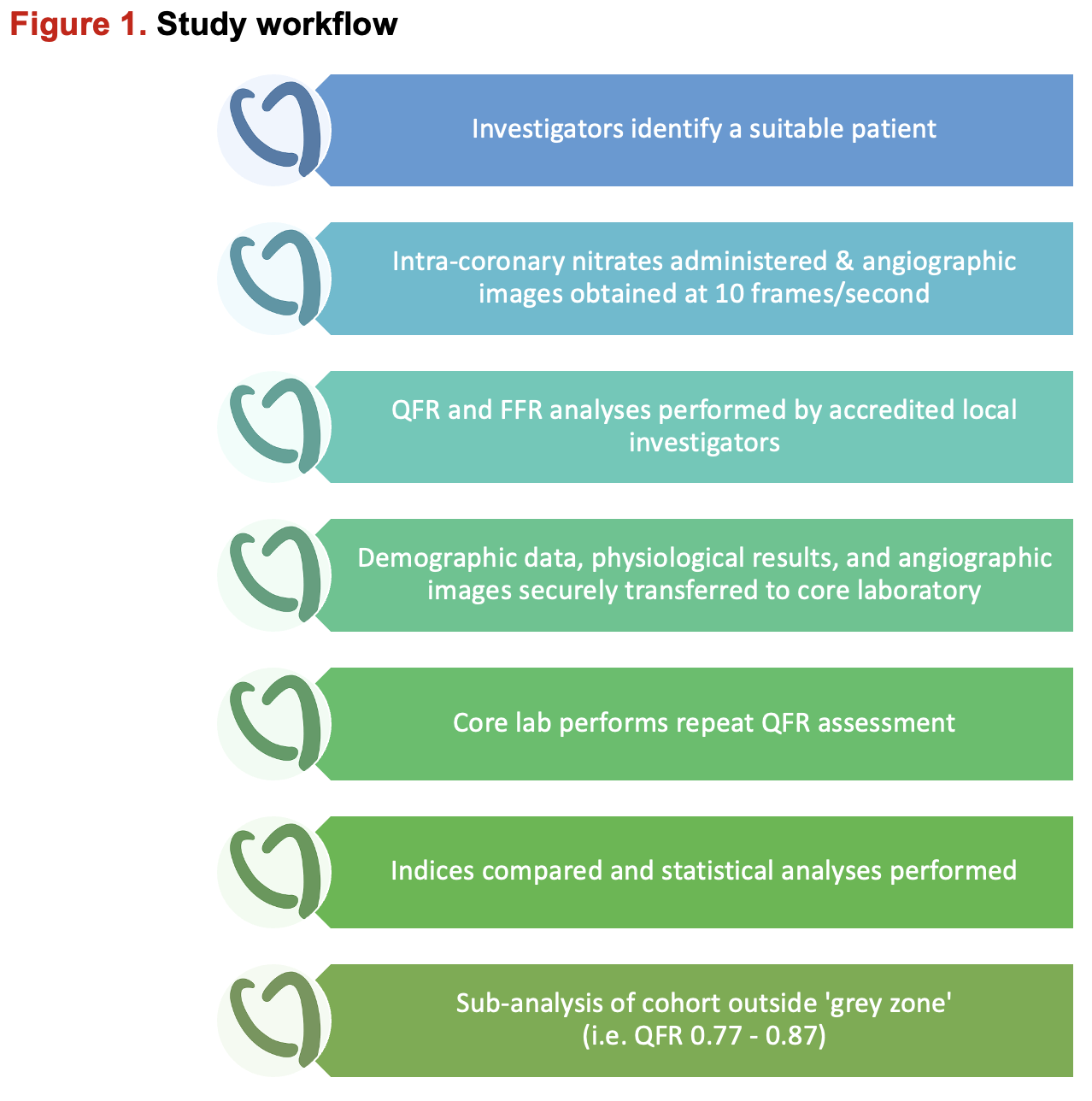
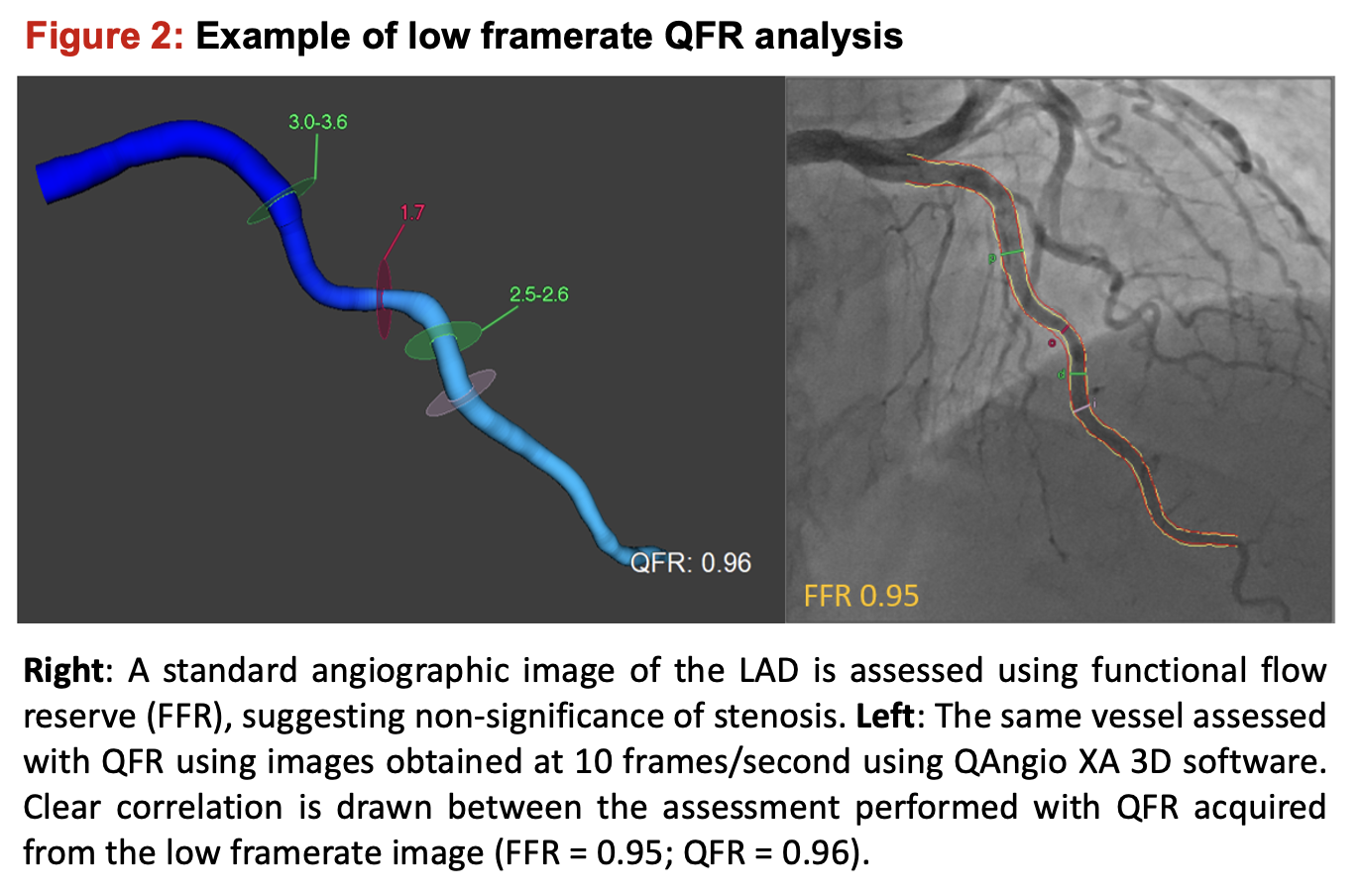
Patients across four major Australian hospitals undergoing invasivecoronary angiography (ICA) for the indication of angina were prospectivelyrecruited. All underwent angiography at maximum 10 frames/second with a minimumof two orthogonal views ≥ 25º apart before undergoing both clinically-indicatedFFR assessment with physiology wires using piezo-electric sensors and QFRanalysis using the QAngio XA 3D version 2.2.0 software (Medis Medical ImagingSystem, Leiden, The Netherlands). All investigators had completed QFR softwaretraining by the vendor, including a minimum of twenty cases submitted forappraisal and feedback. Repeat QFR evaluations were performed by investigators atthe core lab, blinded to both initial results and clinical outcomes. Asignificant FFR indicative of ischemia was defined as < 0.80, with ananalogous QFR cut-off of < 0.80. Demographic data including age, proceduralindication, and cardiovascular risk factors were recorded.
Results
A total of 1321 patients were enrolled. Once cases with insufficientangiographic angles, incomplete physiological data, or poor-quality imagingwere removed, 797 vessels underwent analysis, of which 312 vessels (39%) wereFFR positive. The mean FFR and QFR values were both calculated at 0.81 ± 0.1. Theparticipants’ mean BMI was 28.8 kg/m2, with the average patient inthe 7th decade of life with two or more cardiovascular risk factors.The left anterior descending artery was the most commonly assessed vessel(67.8%). Amongst the entire cohort a QFR < 0.80 demonstrated high predictiveaccuracy for significant FFR (< 0.80), with a sensitivity of 85%,specificity of 89%, PPV of 83%, NPV of 90%, and overall diagnostic accuracy of87%. The area under the curve (AUC) for QFR to predict significant FFR was0.92. QFR showed both excellent inter-observer variability, with an interclasscorrelation coefficient of 0.92 (p < 0.001), and robust intra-observervariability with an intraclass correlation coefficient of 0.93 (p < 0.001).Sub-analysis of the 463 vessels (58%) which fell outside the pre-defined greyzone revealed a significantly improved diagnostic accuracy of 93.5%(sensitivity 94%, specificity 93%, PPV 90%, NPV 96%).
Conclusion
Our prospective, multi-center study demonstrated that QFR retained its previouslyreported diagnostic accuracy in predicting a significant FFR when angiographic imageswere acquired at a low framerate. These findings suggest QFR-guided deferral ofFFR could safely occur with a high diagnostic accuracy of > 90%. QFR canthus serve as a gatekeeper for FFR using a QFR-FFR hybrid approach regardlessof acquisition framerate, with only indeterminate or borderline resultsrequiring further characterization via invasive physiological assessment. QFRvalues outside the pre-defined grey zone are associated with excellentdiagnostic accuracy and will reduce FFR usage by 58%, consistent with the 60%reduction in invasive wiring demonstrated in previous studies.


