Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-028
Comparison of Drug Eluting Stents-Only With Drug-Coated Balloons-Only and Hybrid Strategy for Percutaneous Coronary Intervention of Coronary Chronic Total Occlusion Lesion: A Systematic Review and Network Meta-Analysis
By Chiquita Febby Pragitara, Muammar Emir Ananta, Imanita Septianda Taufik, Bayushi Eka Putra, Arief Wibisono
Presenter
Muammar Emir Ananta
Authors
Chiquita Febby Pragitara1, Muammar Emir Ananta2, Imanita Septianda Taufik1, Bayushi Eka Putra1, Arief Wibisono3
Affiliation
Berkah General Hospital, Indonesia1, Cempaka Putih Jakarta Islamic Hospital, Indonesia2, Dr. Iskak General Hospital, Indonesia3
View Study Report
TCTAP A-028
CTO
Comparison of Drug Eluting Stents-Only With Drug-Coated Balloons-Only and Hybrid Strategy for Percutaneous Coronary Intervention of Coronary Chronic Total Occlusion Lesion: A Systematic Review and Network Meta-Analysis
Chiquita Febby Pragitara1, Muammar Emir Ananta2, Imanita Septianda Taufik1, Bayushi Eka Putra1, Arief Wibisono3
Berkah General Hospital, Indonesia1, Cempaka Putih Jakarta Islamic Hospital, Indonesia2, Dr. Iskak General Hospital, Indonesia3
Background
Chronic Total Occlusion (CTO) is observed in approximately 15–25% of patients undergoing coronary angiography. New-generation drug-eluting stents (DES) are currently the most common approach to recanalize CTO. However, this procedure often requires long and multiple stents, which are associated with higher adverse events due to a higher risk of suboptimal stent implantation or delayed endothelialization. Recently, drug-coated balloon (DCB)-based PCI has been introduced as an alternative approach to treat some CTO lesions if deemed suitable (no flow-limiting dissection and TIMI flow grade 3 after predilatation). Compared to DES, DCB-based PCI offers the advantage of delivering antiproliferative drugs promptly to the coronary vessel wall without leaving behind any permanent metal implants, thereby lowering the risk of adverse biological reactions associated with stents, which can contribute to complications such as restenosis and thrombosis. Comparable clinical outcomes between DCB and DES implantations have been reported in patients with in-stent restenosis and de novo small vessel disease. However, data comparing the outcomes of DCB-based PCI (including DCB-only PCI or hybrid strategy) with DES-only PCI for CTO lesions are still scarce. Therefore, we aimed to comprehensively review the literature regarding the outcomes of these strategies in patients with coronary CTO lesions.
Methods
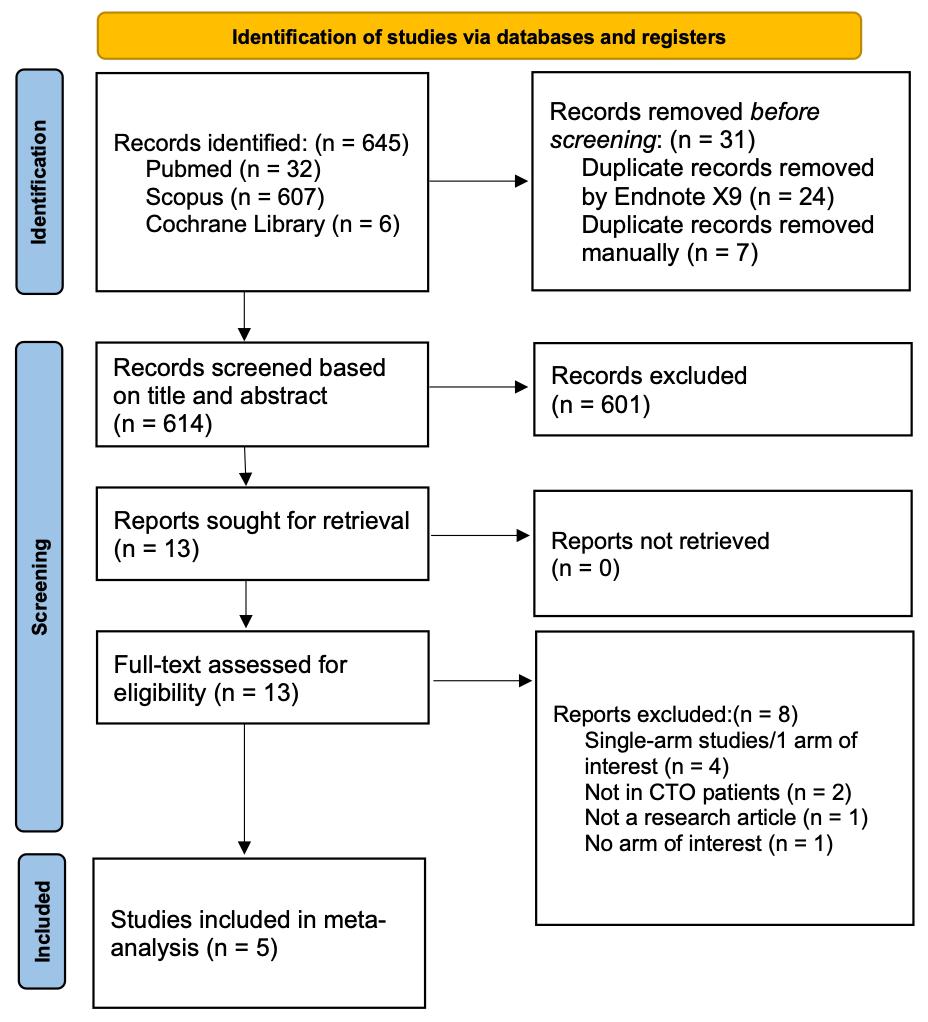
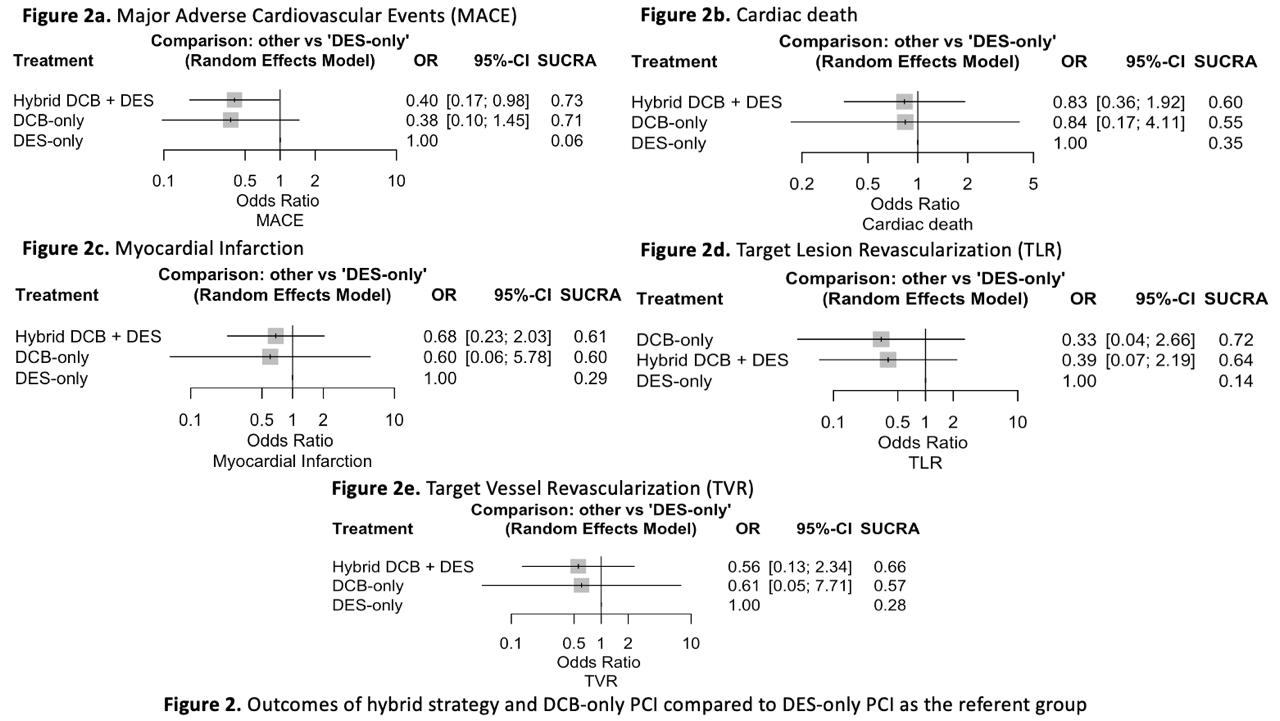
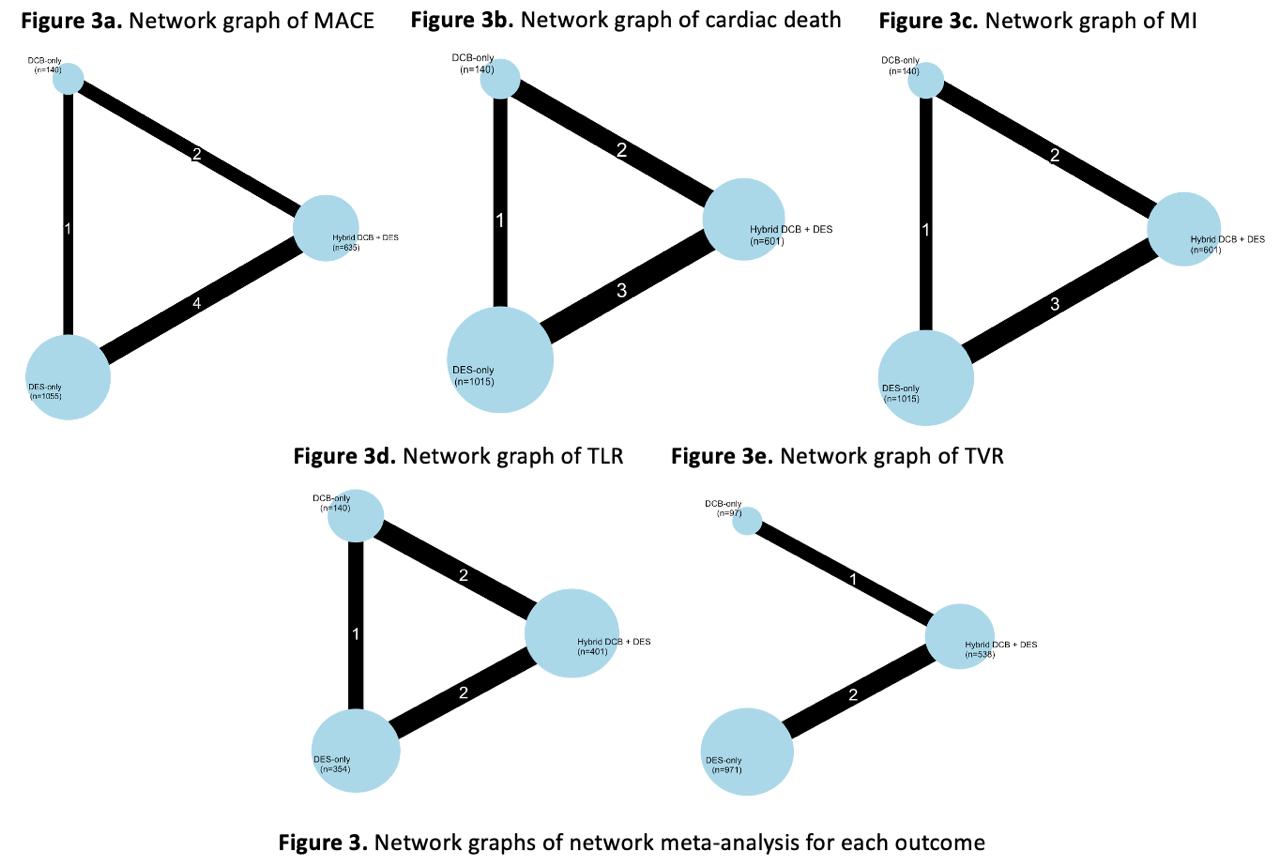
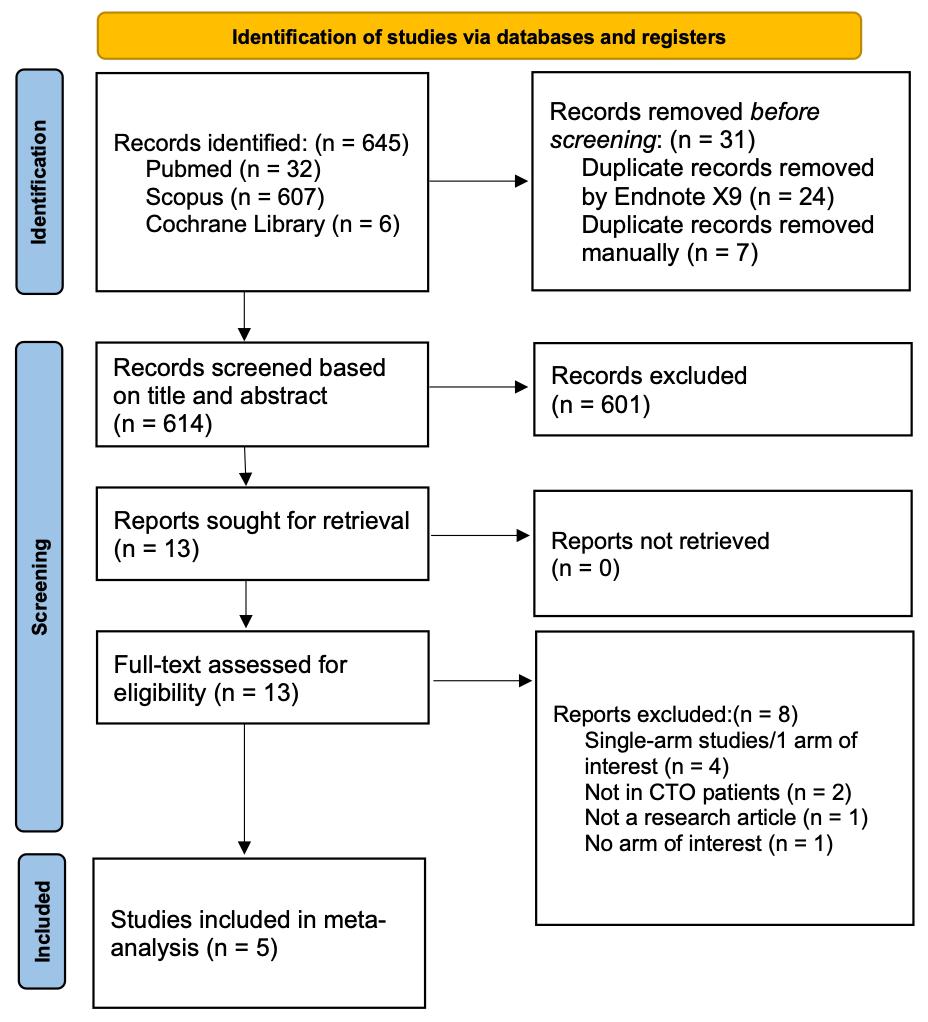
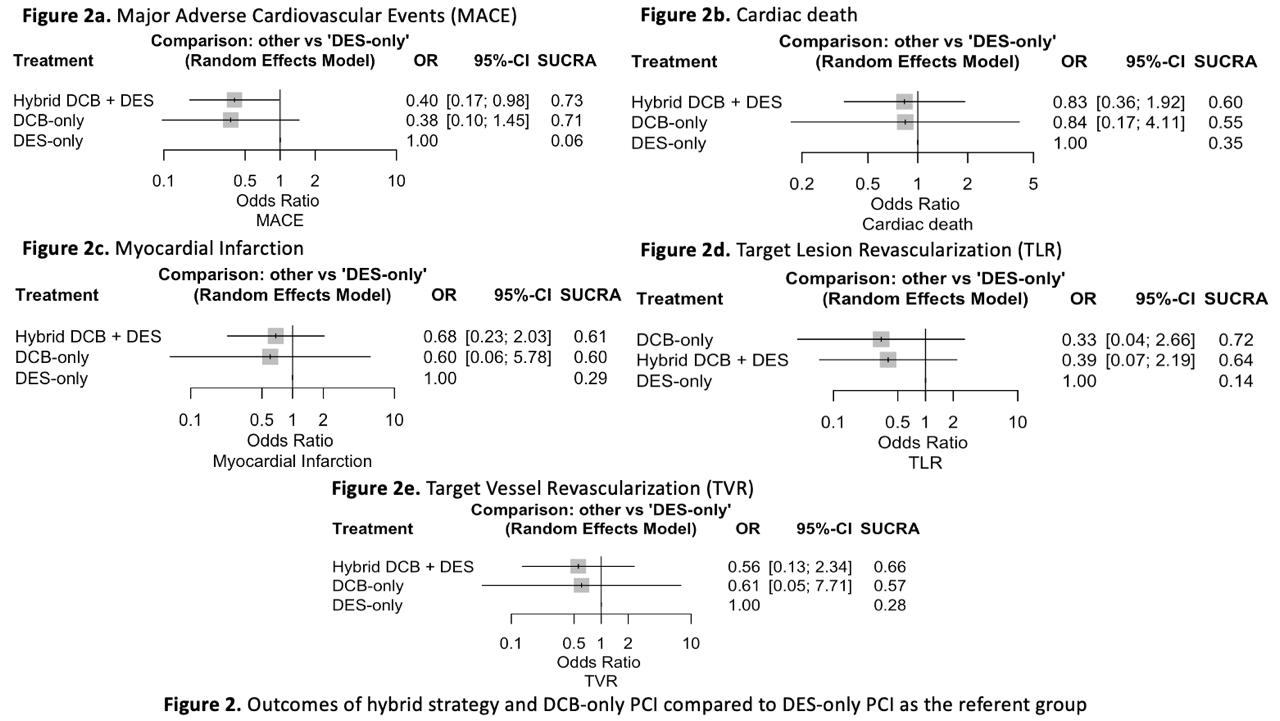
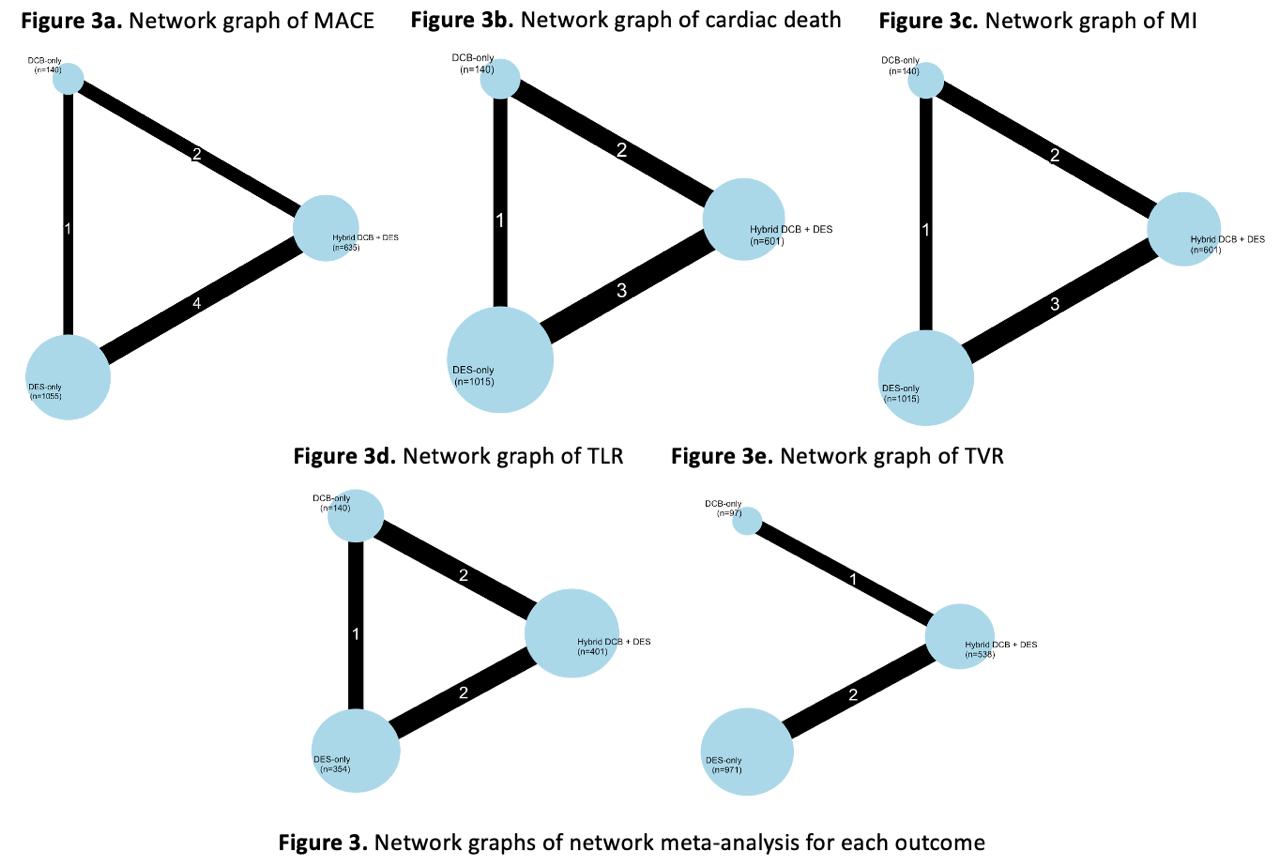
Pubmed, Scopus, and Cochrane Library were searched for studies that compare the outcomes among DCB-only strategy, DES-only strategy, or hybrid strategy (DCB-based strategy with the possibility of planned or bailout DES implantation) in patients with a CTO lesion treated with PCI. The primary endpoint was Major Adverse Cardiovascular Events (MACE) as defined by each study or the primary composite endpoint, which was customarily defined as the composite of cardiac death, myocardial infarction, Target Vessel Revascularization (TVR), and/or Target Lesion Revascularization (TLR). Secondary endpoints were components of the primary endpoint. Random-effects network meta-analysis using the frequentist approach was employed to calculate pooled Odds Ratio (OR) with 95% Confidence Interval (95% CI) using the DES-only strategy as the referent group. Surface Under Cumulative Ranking Area (SUCRA) score was used to rank the interventions from best to worst, with higher numbers representing better treatment.
Results
In total, 5 observational studies consisting of 1,830 patients with CTO lesion were included in the meta-analysis (Hybrid strategy: 635 patients; DCB-only PCI: 140 patients; DES-only PCI: 1,055 patients). In the hybrid group strategy, DCB-only PCI was performed in 40.07% of the patients, while bailout with DES was reportedly performed in 2.66 % of the patients due to suboptimal DCB angioplasty. The rest of the patients in the hybrid strategy group were treated with a combination of DCB and DES. The follow up period ranged from 470 days to 3 years after discharge. Hybrid DCB + DES strategy significantly lowers MACE compared to DES-only PCI (OR 0.40; 95% CI 0.17–0.98), but DCB-only PCI does not (OR 0.38; 95% CI 0.10–1.45). For the secondary endpoints, in the hybrid strategy group, there was a trend towards lower risks of cardiac death (OR 0.83; 95% CI 0.36–1.92), myocardial infarction (OR 0.68; 95% CI 0.23–2.03), TLR (OR 0.39; 95% CI 0.07–2.19), and TVR (OR 0.56; 95% CI 0.13–2.34), although the difference was not statistically significant. Compared to DES-only PCI, in the DCB-only PCI, there was also a trend towards lower risk of cardiac death (OR 0.84; 95% CI 0.17–4.11), myocardial infarction (OR 0.60; 95% CI 0.06–5.78), TLR (OR 0.33; 95% CI 0.04–2.66), and TVR (OR 0.61; 95% CI 0.05–7.71), but none of the endpoints were significantly different.
Conclusion
Pooled data from observational studies in the literature found a lower risk of MACE with the hybrid strategy compared to DES-only PCI for coronary CTO lesions, which suggests that the hybrid strategy should be preferred over DES-only PCI for coronary CTO lesions whenever feasible.


