Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-072
Is Left Atrial Appendage Closure an Effective and Feasible Alternative in Patients With End-Stage Renal Disease?
By Juan F. Rodriguez-Riascos, Hema Vemulapalli, Poojan Prajapati, Padmapriya Muthu, Komandoor Srivathsan
Presenter
Juan F. Rodriguez-Riascos
Authors
Juan F. Rodriguez-Riascos1, Hema Vemulapalli1, Poojan Prajapati1, Padmapriya Muthu1, Komandoor Srivathsan1
Affiliation
Mayo Clinic, USA1
View Study Report
TCTAP A-072
LAAO
Is Left Atrial Appendage Closure an Effective and Feasible Alternative in Patients With End-Stage Renal Disease?
Juan F. Rodriguez-Riascos1, Hema Vemulapalli1, Poojan Prajapati1, Padmapriya Muthu1, Komandoor Srivathsan1
Mayo Clinic, USA1
Background
The benefits of oral anticoagulants in patients with end-stage renal disease (ESRD) remain uncertain due to altered drug metabolism and increased bleeding risk. Left atrial appendage closure (LAAC) has emerged as a potential alternative to oral anticoagulation, aiming to reduce stroke risk without the bleeding complications linked to anticoagulants. This study aimed to compare LAAC outcomes between patients with and without ESRD.
Methods
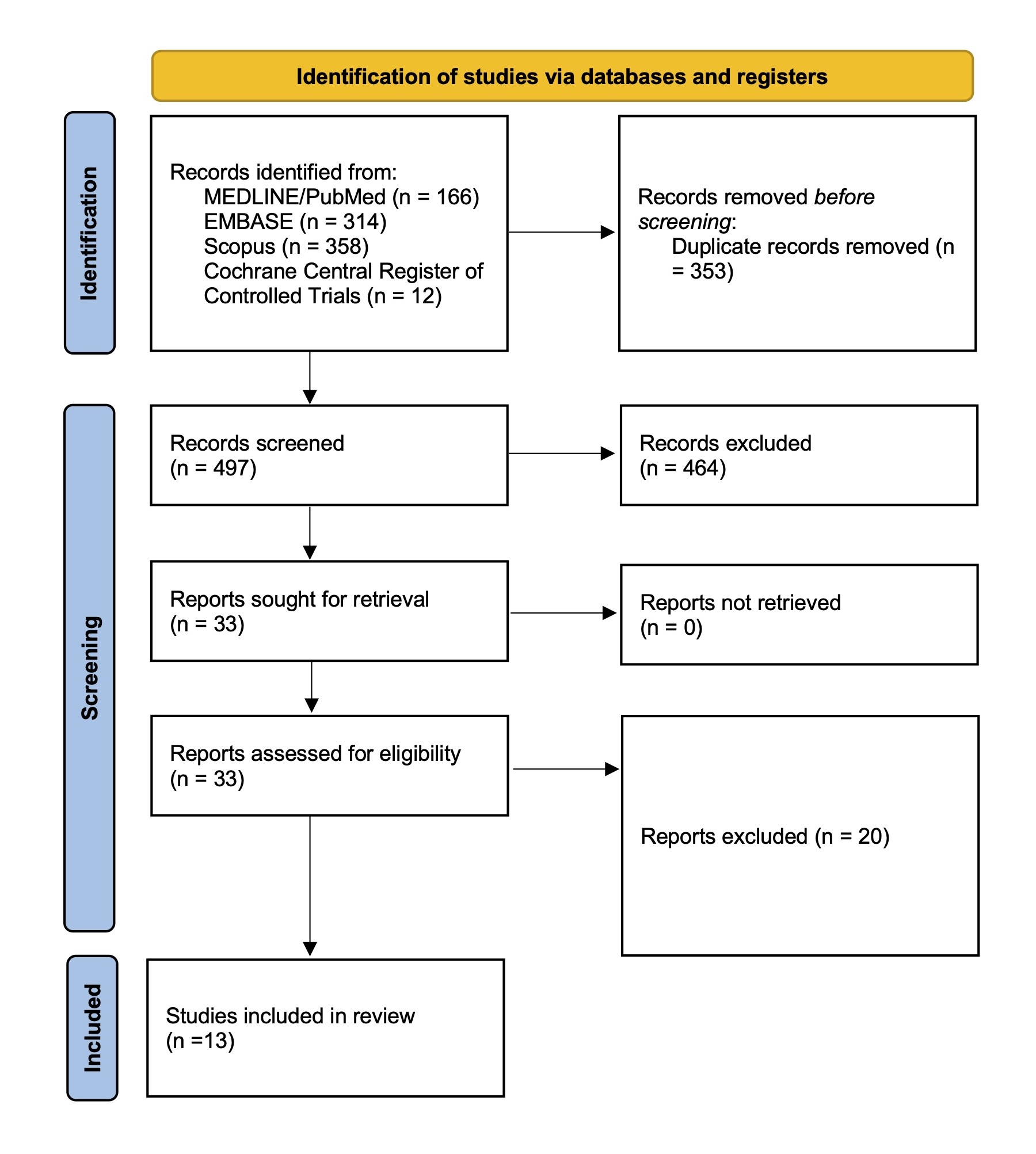
A systematic literature review was conducted according to PRISMA guidelines, searching PubMed, Cochrane, Embase, and Scopus databases up to September 2024. The search included the following terms: “(left atrial appendage) AND (closure OR occlusion) AND (hemodialysis OR dialysis OR end stage renal disease OR end stage kidney disease OR kidney disease OR renal disease)” After duplicates were eliminated, title and abstract screening was performed by two independent blinded reviewers (J.R. and H.V.). Potentially eligible studies were fully reviewed, and the final selection was made by consensus. Figure 1 summarizes the flowchart for the selection of included studies. The primary outcome was thromboembolic events or stroke following the procedure. Secondary outcomes included post-procedural major bleeding, mortality, device-related thrombosis, acute success, and procedural complications. Heterogeneity across the included studies was assessed by the I2 test, considering an I2 > 50% significant. For analyses demonstrating significant heterogeneity, a random-effects model was employed. Conversely, for those with non-significant heterogeneity, a fixed-effects model was utilized. Incidence rate ratios (IRRs) were used as measures of association for time-dependent outcomes, while risk ratios (RRs) were reported for non-time-dependent outcomes.
Results
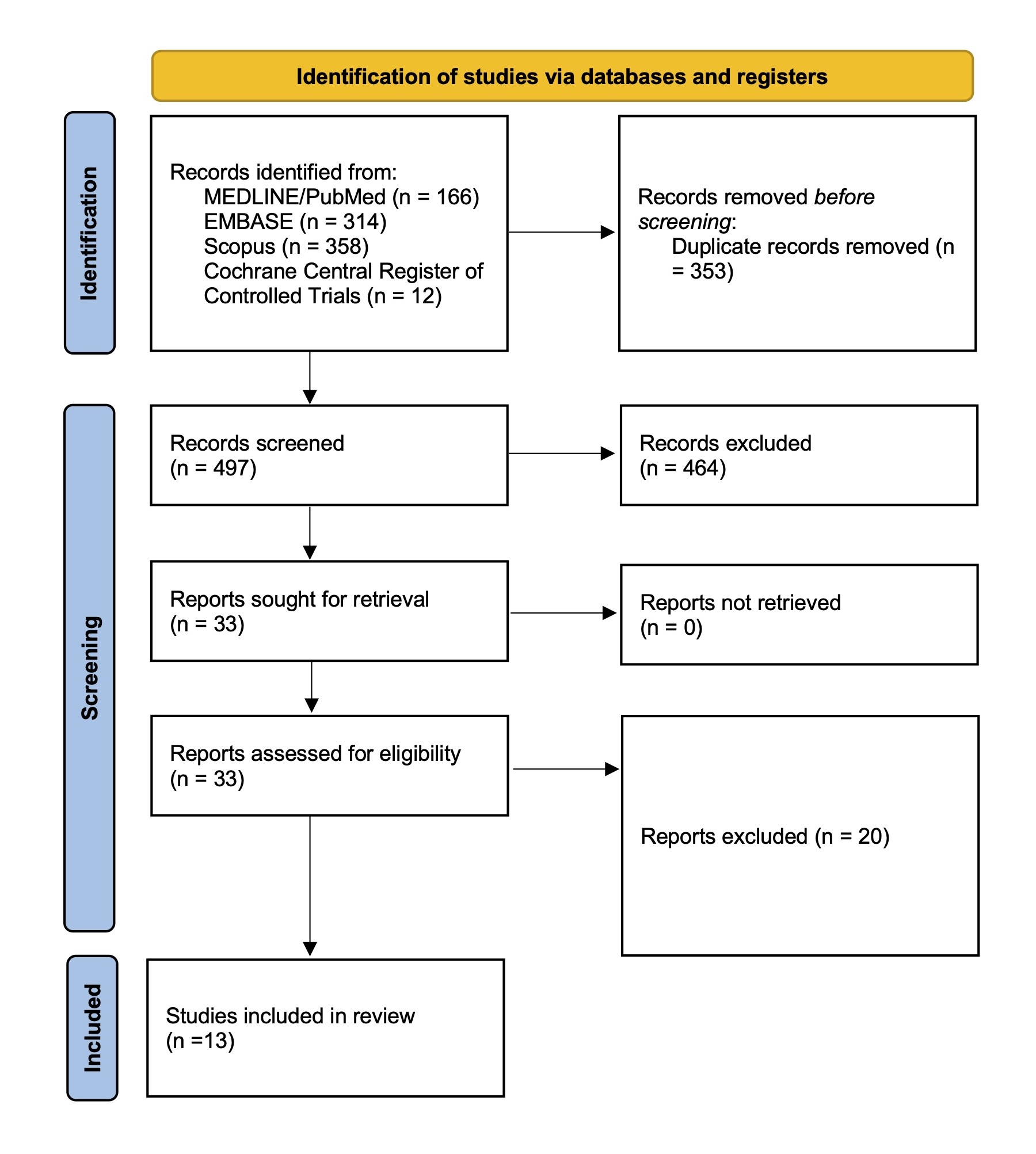
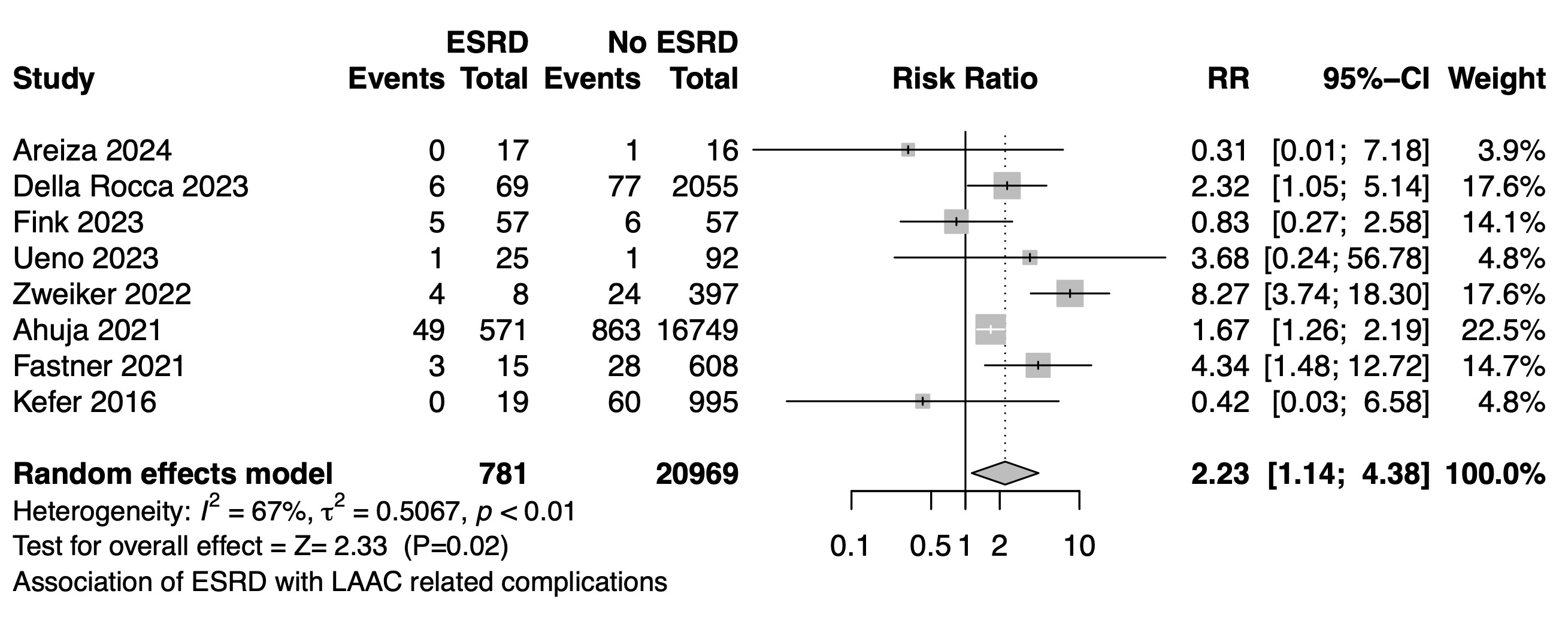
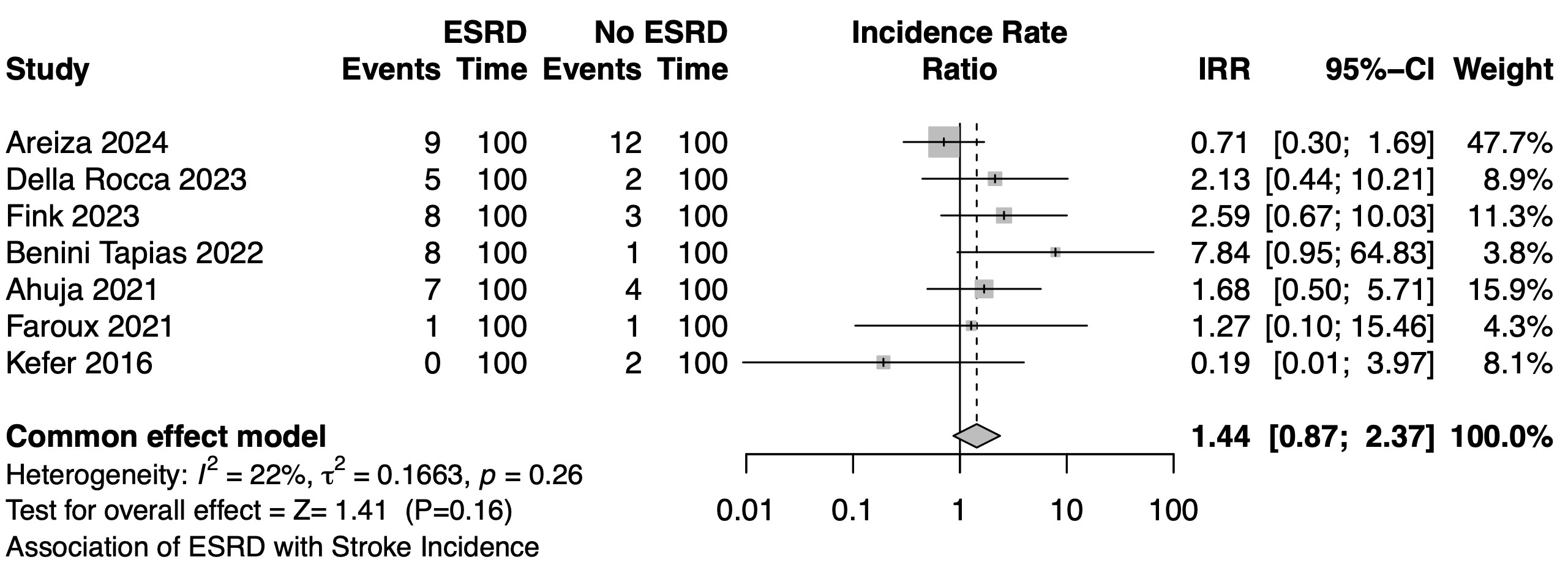
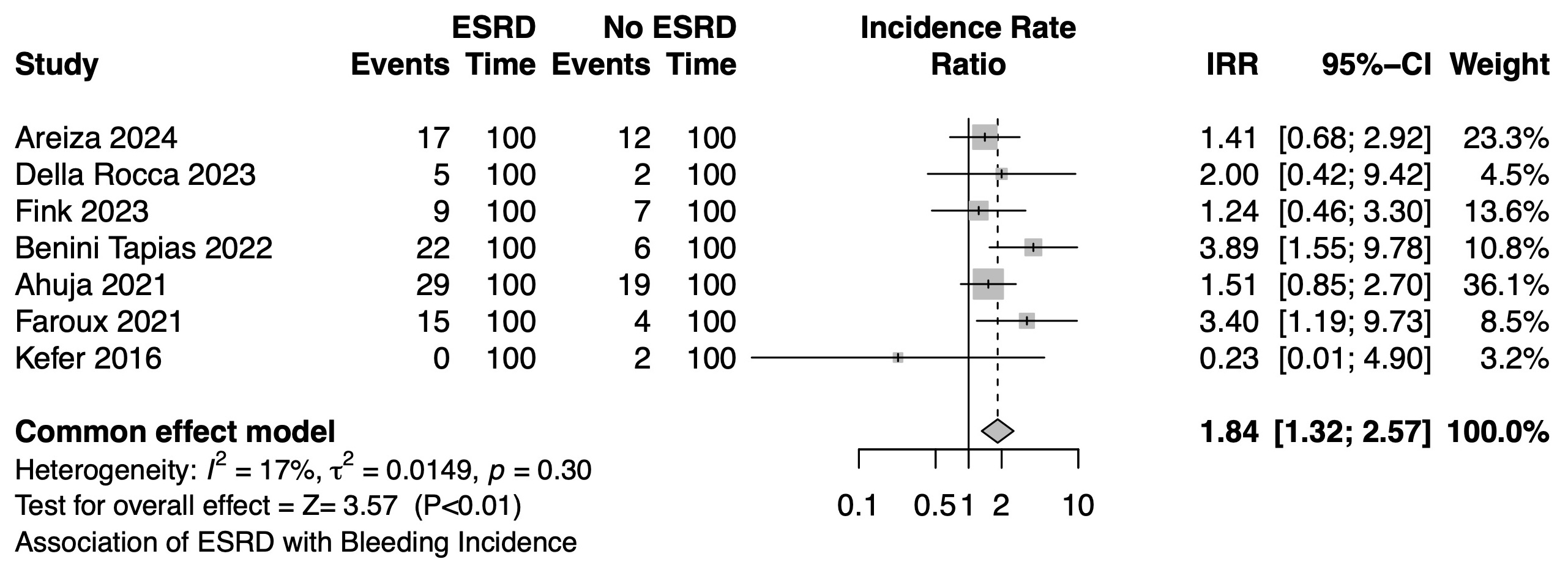
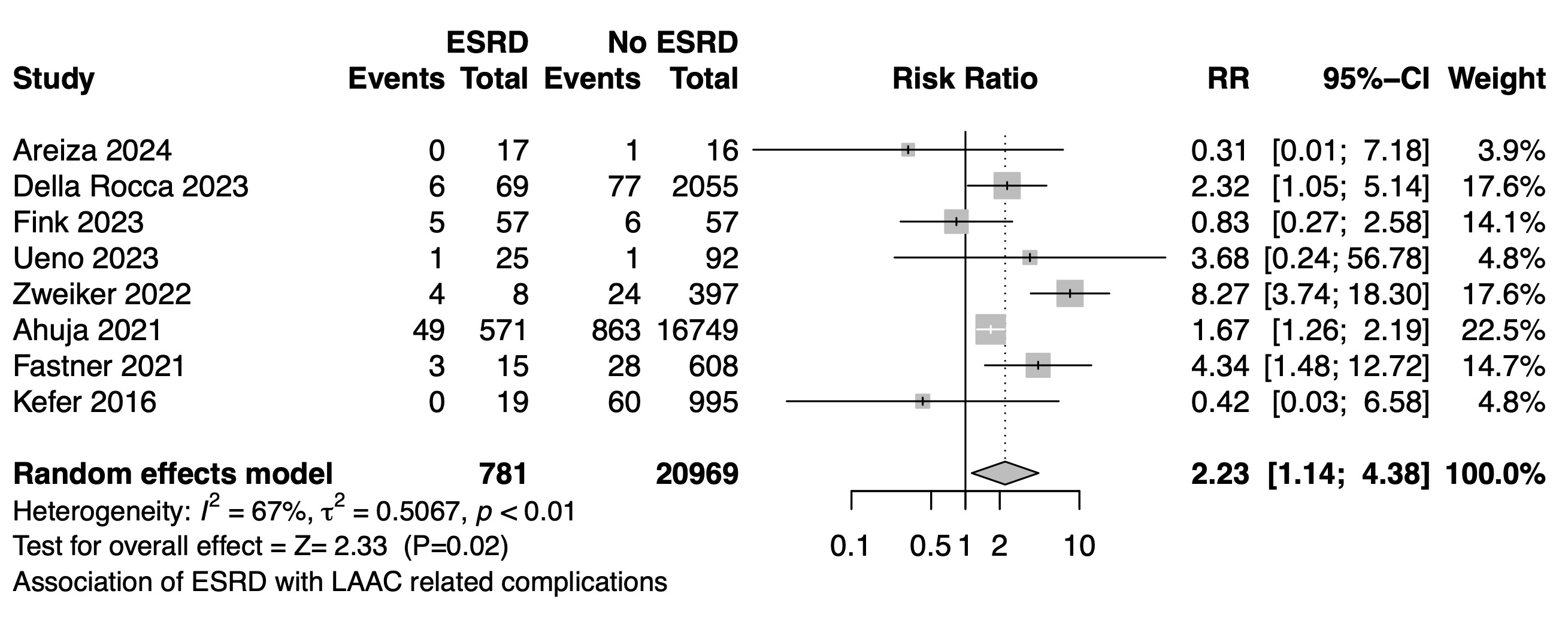
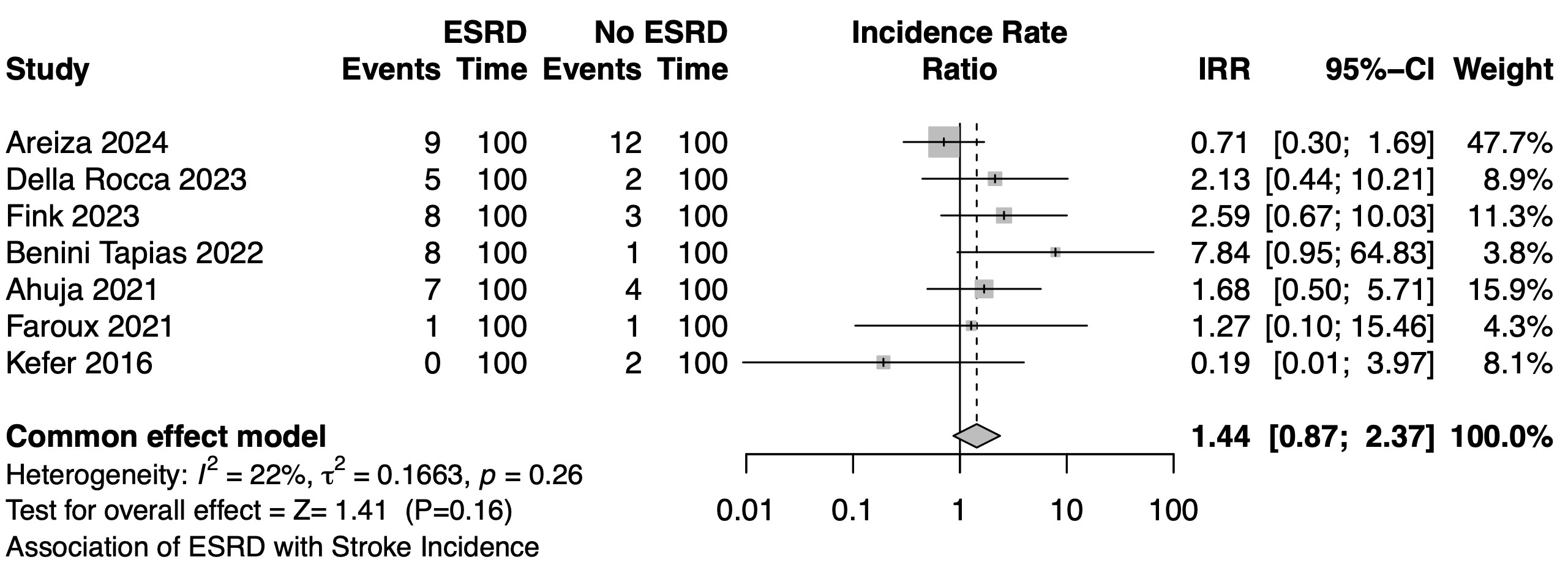
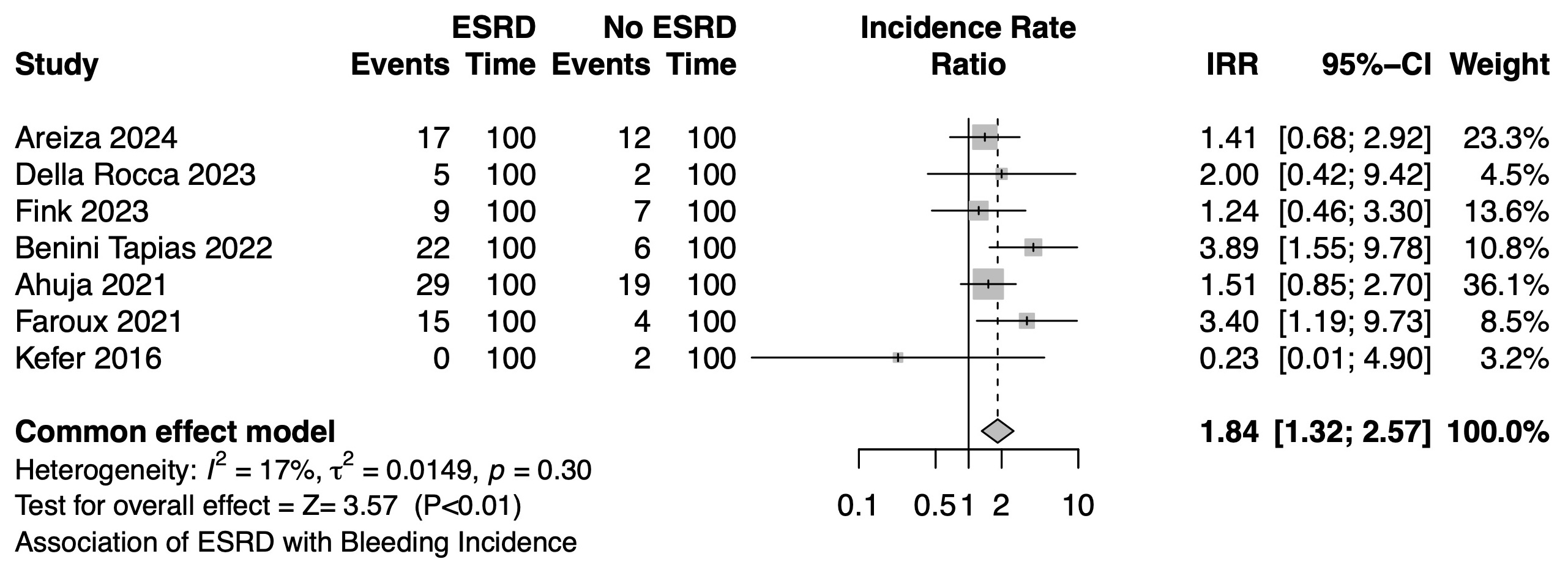
A total of 497 titles and abstracts were screened, 33 studies were fully reviewed, and 13 studies reporting data from 898 ESRD patients and 21,995 non-ESRD patients were included. LAAC was successful in all the patients with ESRD, no differences in the success rates between ESRD and no-ESRD patients were documented (RR, 1.0; 95% CI, 0.97-1.04; I2 = 0%; p = 0.79). Patients with ESRD presented a higher rate of complications (RR, 2.23; 95% CI, 1.14-4.38; I2 = 67%; p = 0.02) Figure 2. Among four studies comparing 105 patients with ESRD and 513 patients without ESRD, device-related thrombosis rates were comparable in both groups (RR, 0.59; 95% CI, 0.11-3.04; I2 = 26%; p = 0.53). During follow-up, there was no significant difference in stroke incidence between ESRD and non-ESRD patients after LAAC (IRR, 1.44; 95% CI, 0.87-2.37; I2 = 22%; p = 0.16) (Figure 3). ESRD patients, however, had higher rates of post-procedure major bleeding (IRR, 1.84; 95% CI, 1.32-2.57; I2 = 17%; p < 0.01) (Figure 4) and mortality (RR, 1.88; 95% CI, 1.28-2.75; I2 = 0%; p <0.01).
Conclusion
To the best of our knowledge, this is the largest meta-analysis in this field and the first to compare stroke and bleeding as time-dependent outcomes. Our results support the feasibility of LAAC in ESRD patients, demonstrating comparable success rates and an acceptable complication rate. However, the complication rate was higher than in non-ESRD patients. Finally, while LAAC provides comparable protection against thromboembolic events in both ESRD and non-ESRD patients, those with ESRD have a significantly higher risk of major bleeding and overall mortality.


