Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-042
Prognostic Value of Neutrophil-Lymphocyte Ratio in Chronic Renal Insufficiency Patients Undergoing Percutaneous Coronary Intervention
By Yiting Wu, Enshao Liu, Feng-Yu Kuo
Presenter
Yiting Wu
Authors
Yiting Wu1, Enshao Liu1, Feng-Yu Kuo1
Affiliation
Kaohsiung Veterans General Hospital, Taiwan1
View Study Report
TCTAP A-042
High-Risk Intervention (Diabetes, Heart Failure, Renal Failure, Shock, etc)
Prognostic Value of Neutrophil-Lymphocyte Ratio in Chronic Renal Insufficiency Patients Undergoing Percutaneous Coronary Intervention
Yiting Wu1, Enshao Liu1, Feng-Yu Kuo1
Kaohsiung Veterans General Hospital, Taiwan1
Background
Chronic kidney disease (CKD) is a significant comorbidity of coronary artery disease (CAD), and both are associated with the inflammation response. Treating CAD with percutaneous coronary intervention (PCI) in patients with CKD remained challenging, highlighting the need for developing non-traditional markers to improve outcome prediction. In this study we aimed to evaluate the association between systemic inflammation parameters, including neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and monocytes-to-lymphocyte ratio (MLR), and adverse cardiovascular events in chronic renal insufficiency patients who have undergone PCI.
Methods
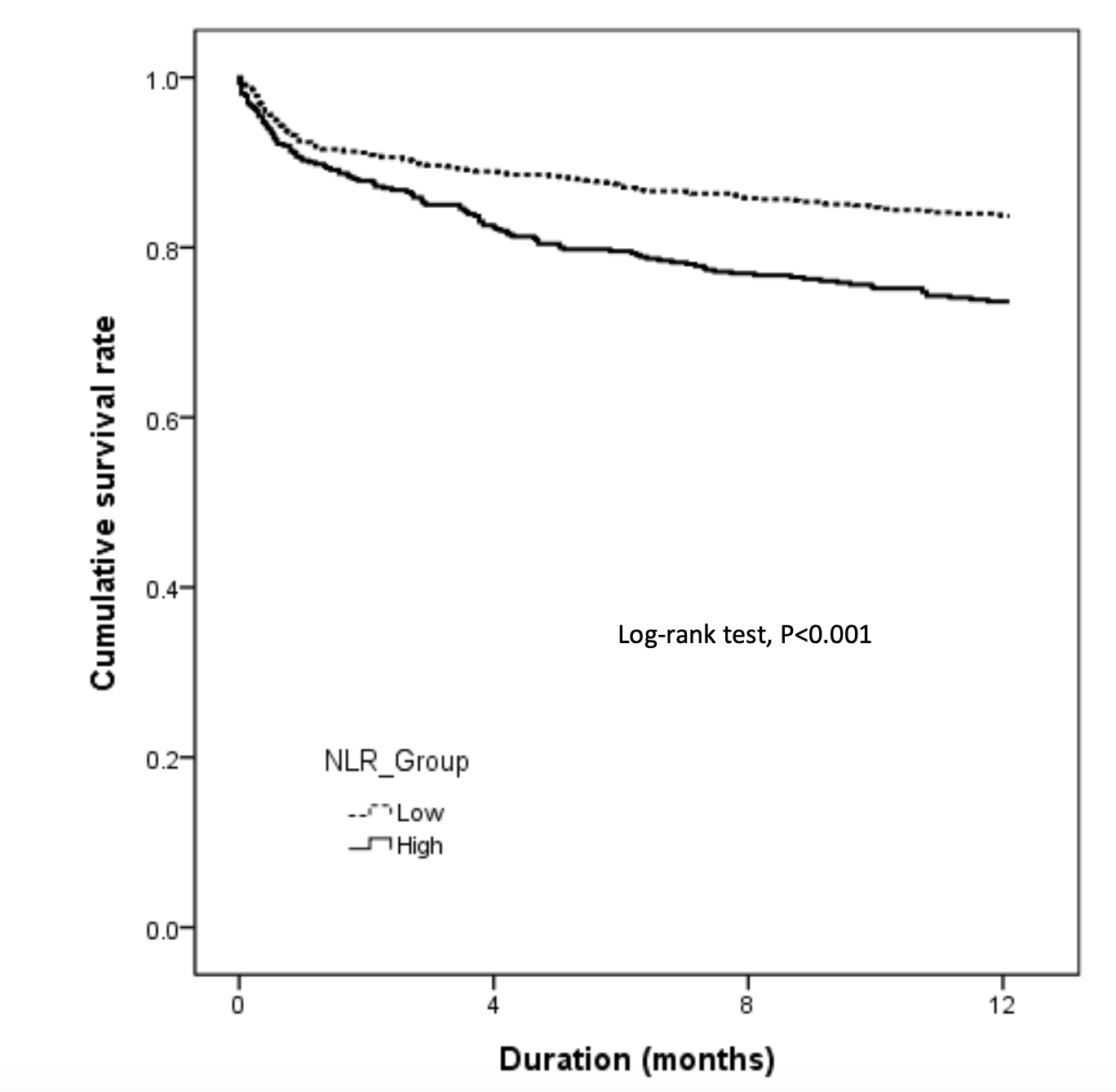
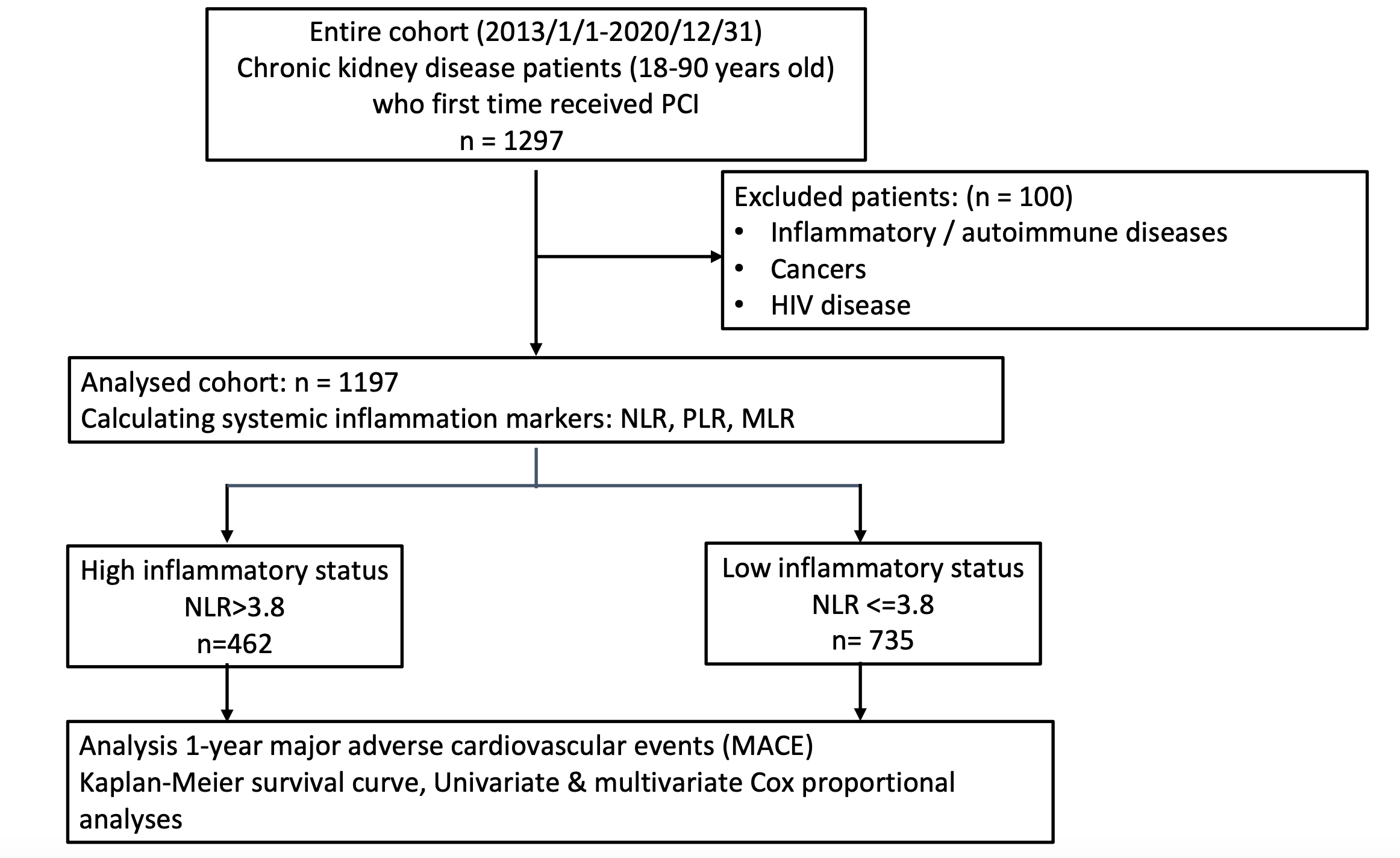
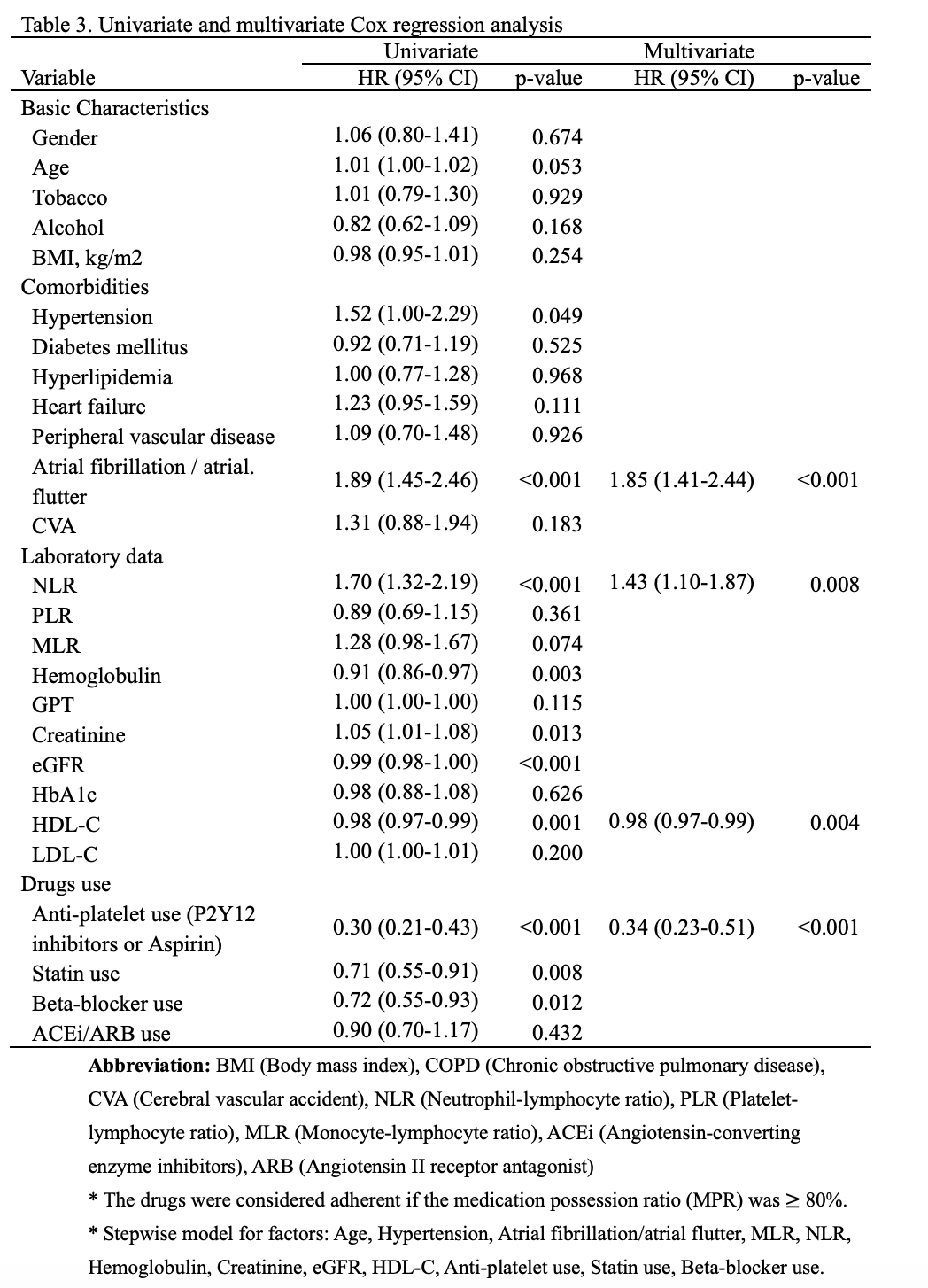
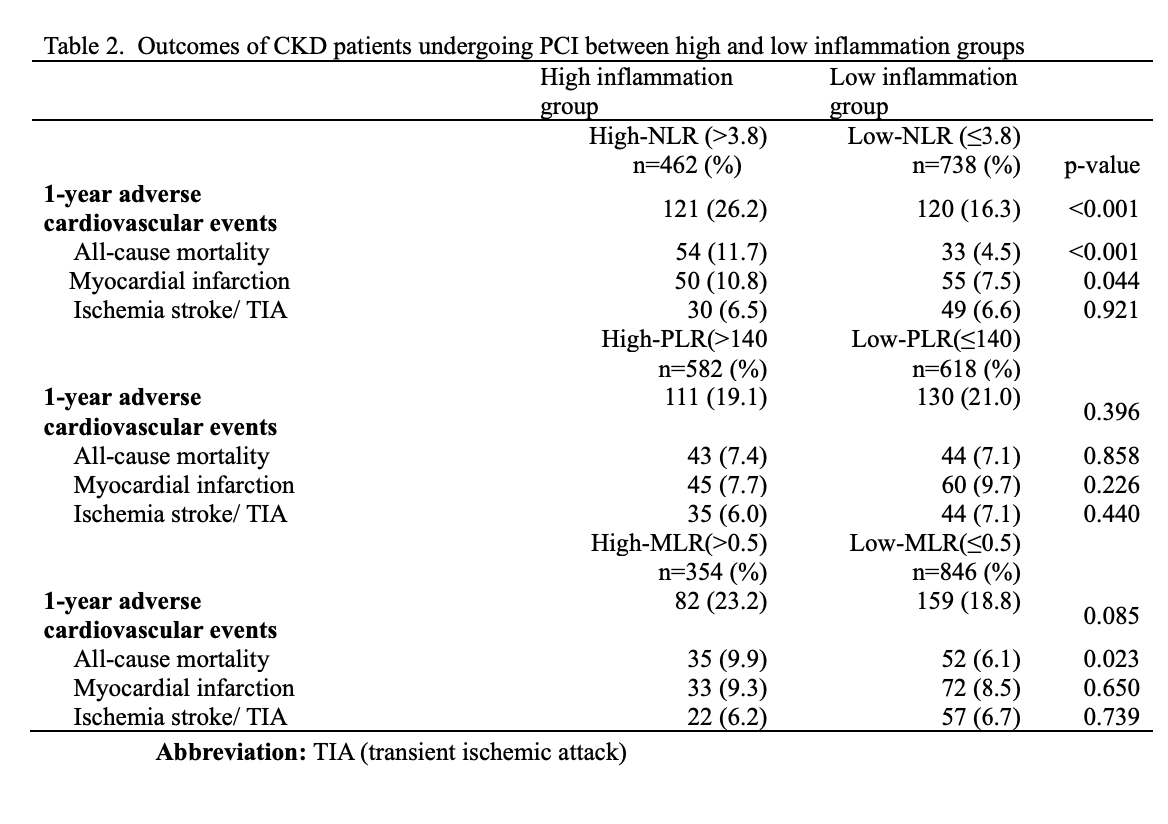
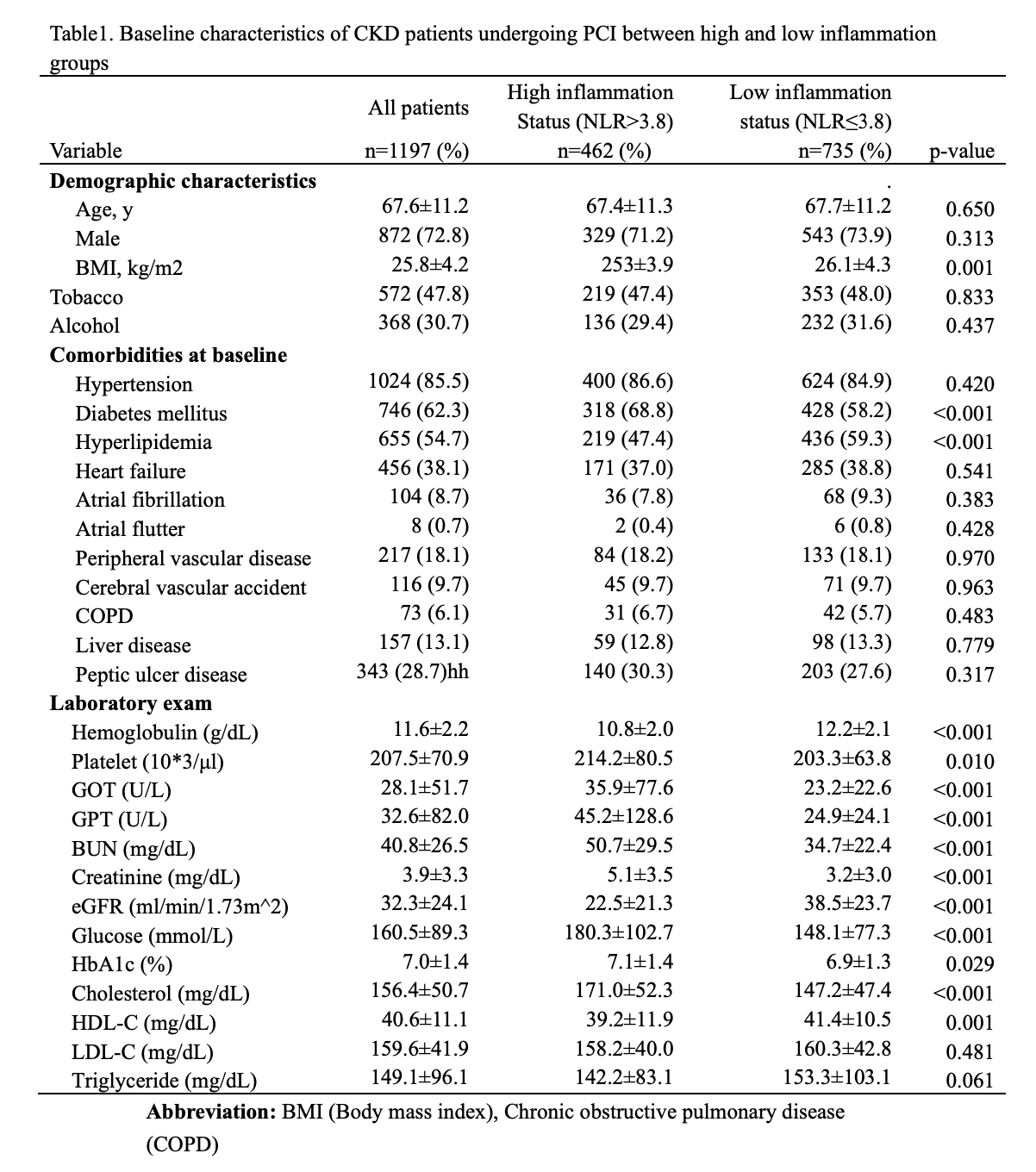
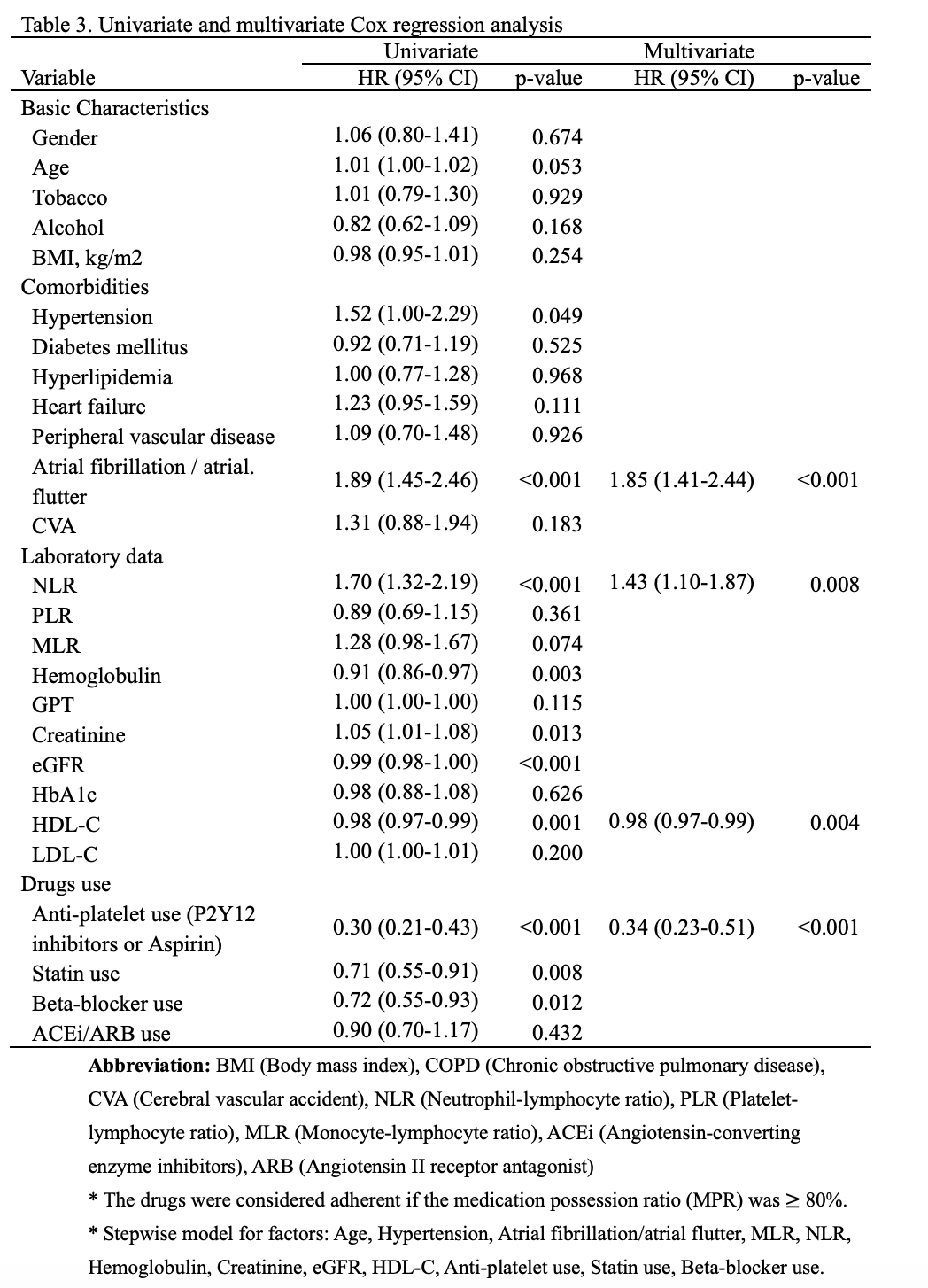
This study retrospectively enrolled CKD patients underwent PCI from cath lab database from 2013 to 2020. The exclusion criteria included patients with extremely young or elderly (<18 or >90 years), unclear CKD diagnosis (lack of eGFR data or CKD diagnosis within 3 years before PCI), or chronic diseases that impose extra inflammatory effects (autoimmune diseases, cancer, or HIV). Systemic inflammation markers (NLR, PLR, and MLR) are calculated as the ratio of different cell counts. The blood samples were obtained at the time of admission before PCI. The primary outcome was adverse cardiovascular events rate at one-year follow-up, which included all-cause death, myocardial infarction (MI), and ischemic stroke. The optimal cut-off values for NLR, PLR, and MLR were determined by receiver operating characteristic curve analysis. The hazard ratios (HR) for adverse cardiovascular events rate were calculated using Cox analysis. Patients were then stratified into the high and low inflammation groups if the inflammatory markers presented significantly in Cox analysis (P <0.05). The Kaplan–Meier method with long-rank tests was performed.
Results
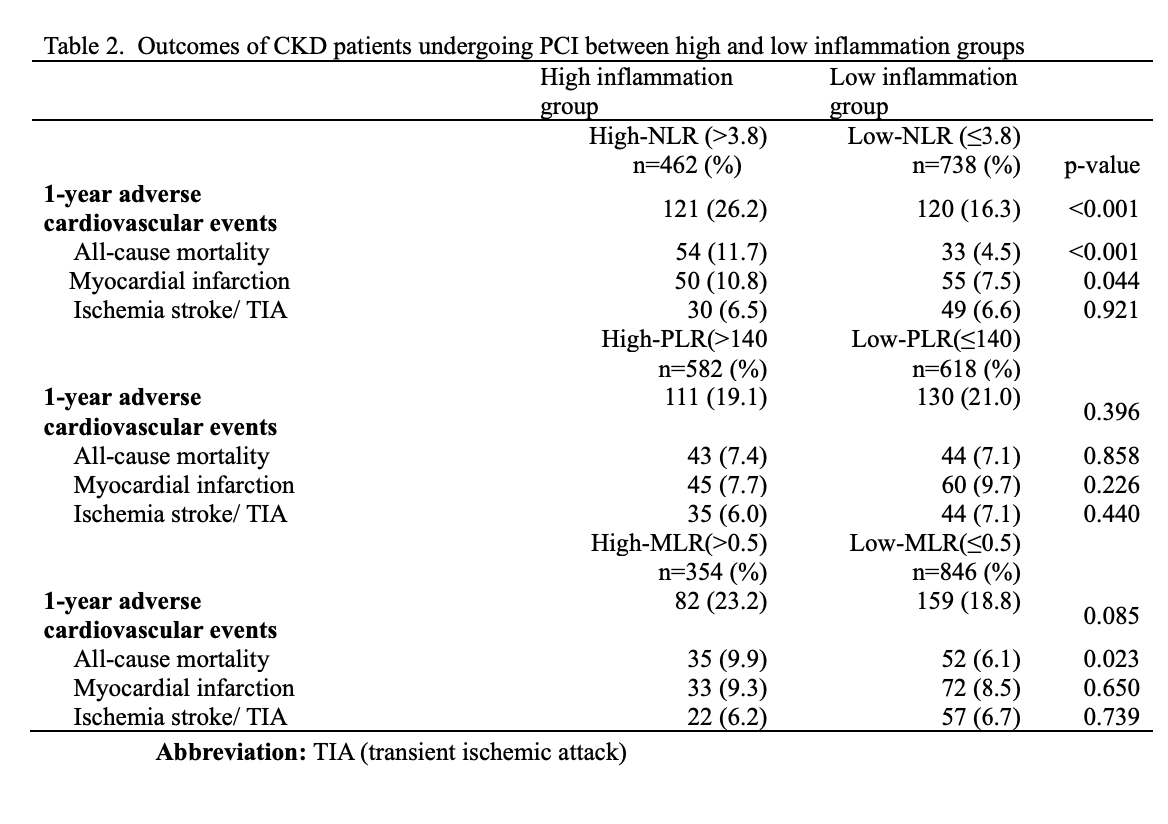
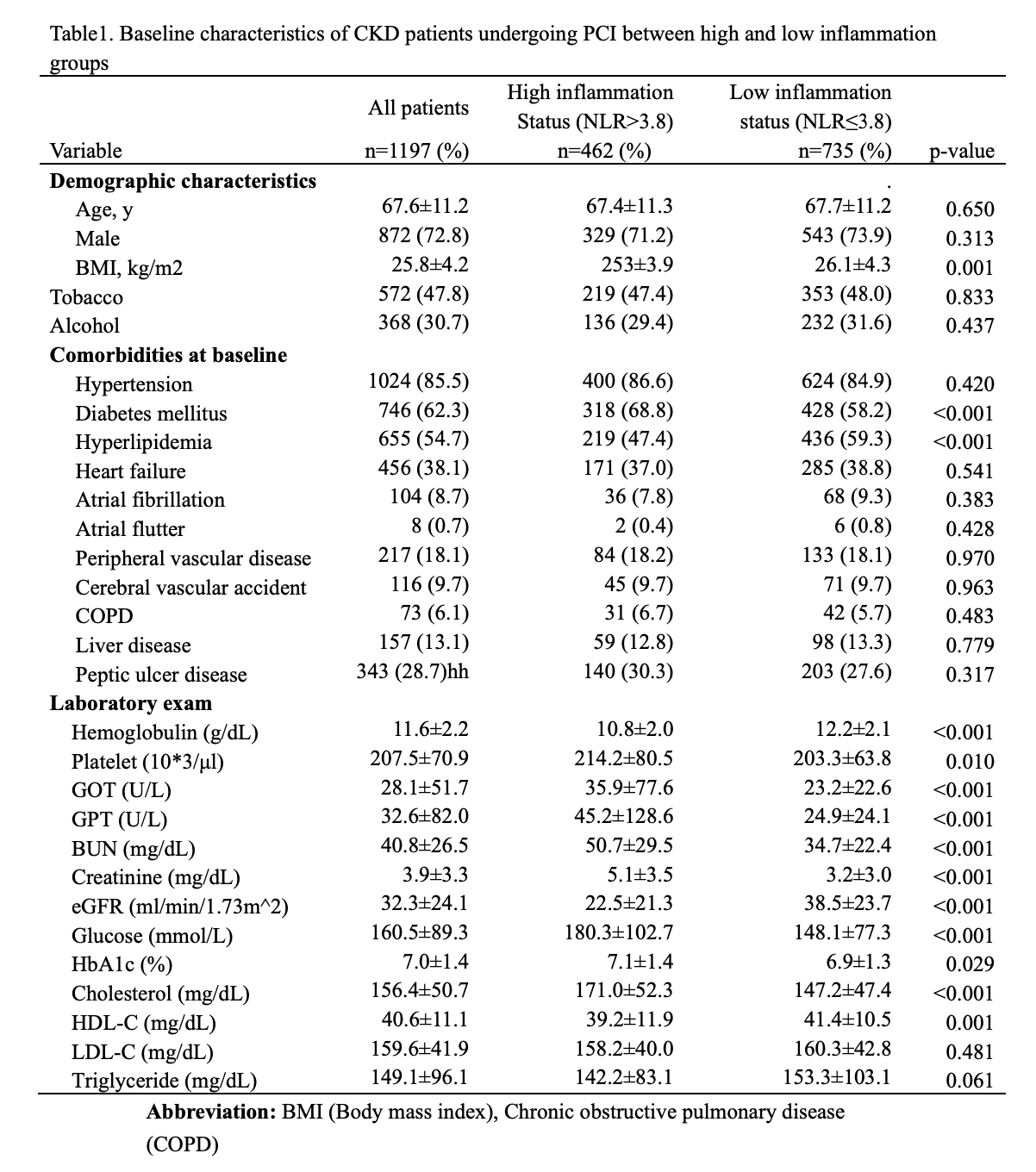
A total of 1197 CKD patients who underwent PCI were identified, with a mean age of 67.6±11.2 years. The majority of these patients carried cardiovascular comorbidities. The NLR, PLR, and MLR cut-off values for MACE were 3.8, 140, and 0.5, respectively. Multivariate Cox regression analysis revealed atrial fibrillation/atrial flutter (HR 1.85, 95% CI 1.41-2.44, P<0.001), NLR >3.8 (HR 1.43, 95% CI 1.10-1.87, P=0.008), anti-platelet use (HR 0.34, 95% CI 0.23-0.51, P<0.001), higher HDL level (HR 0.98, 95% CI 0.98-1.00, P<0.001) were independent predictors of MACE. The NLR >3.8 or not was selected to categorize the patients into high and low inflammation groups. The high inflammation group showed a higher MACE rate (26.2% vs. 16.3%, P < 0.001). The difference in adverse cardiovascular events rate was driven by all-cause death (11.7% vs. 4.5%, P<0.001) and MI (10.8% vs. 7.5%, P=0.044). The Kaplan–Meier curve revealed that the high inflammation group was associated with a worse prognosis. (log-rank P<0.001)
Conclusion
This study demonstrated that NLR is a highly predictive inflammatory marker for cardiovascular outcomes in CKD patients who underwent PCI. Our findings contribute to the development of models that offer individualized estimates of patient-centered outcomes in this high-risk population.