Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-029
Procedural Aspects, In-Hospital Outcomes, and Long-Term Prognosis in Patients Undergoing Percutaneous Coronary Interventions for Chronic Total Occlusions
By Fazila Tun-Nessa Malik, Prof. Nazir Ahmed, Prof. Dhiman Banik, Md Kalim Uddin, Esmat Ara
Presenter
Esmat Ara
Authors
Fazila Tun-Nessa Malik1, Prof. Nazir Ahmed1, Prof. Dhiman Banik1, Md Kalim Uddin1, Esmat Ara1
Affiliation
National Heart Foundation Hospital & Research Institute, Bangladesh1
View Study Report
TCTAP A-029
CTO
Procedural Aspects, In-Hospital Outcomes, and Long-Term Prognosis in Patients Undergoing Percutaneous Coronary Interventions for Chronic Total Occlusions
Fazila Tun-Nessa Malik1, Prof. Nazir Ahmed1, Prof. Dhiman Banik1, Md Kalim Uddin1, Esmat Ara1
National Heart Foundation Hospital & Research Institute, Bangladesh1
Background
Chronic total occlusions (CTOs) present unique challenges in percutaneous coronary intervention (PCI) due to their complex anatomical and procedural characteristics. This study aimed to evaluate procedural aspects, in-hospital outcomes and 1 year prognosis of patients undergoing PCI for CTO in a tertiary center in Bangladesh.
Methods
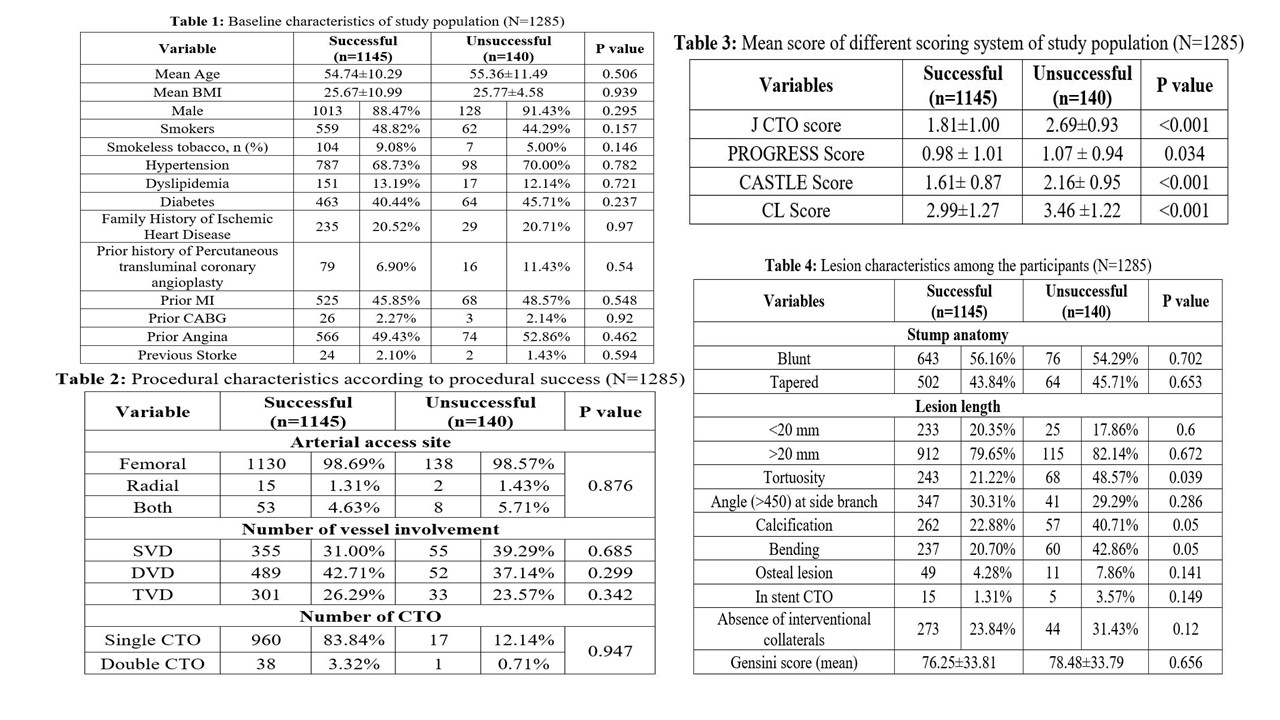
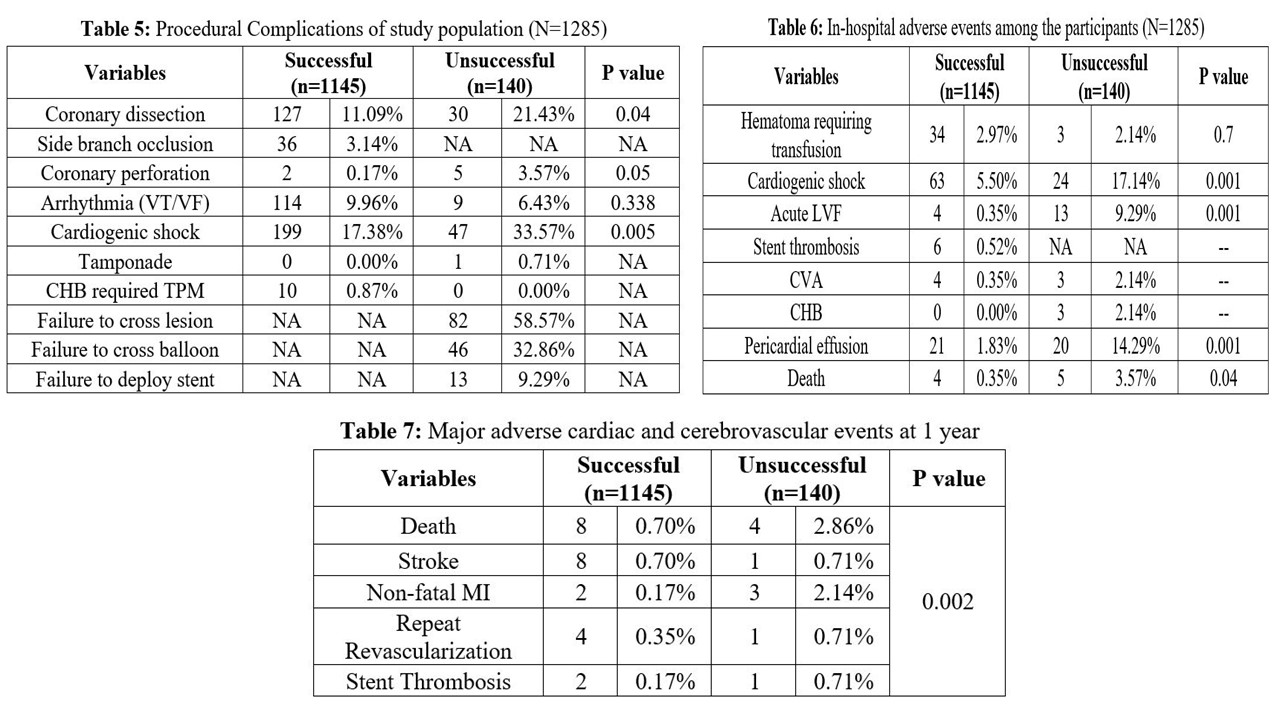
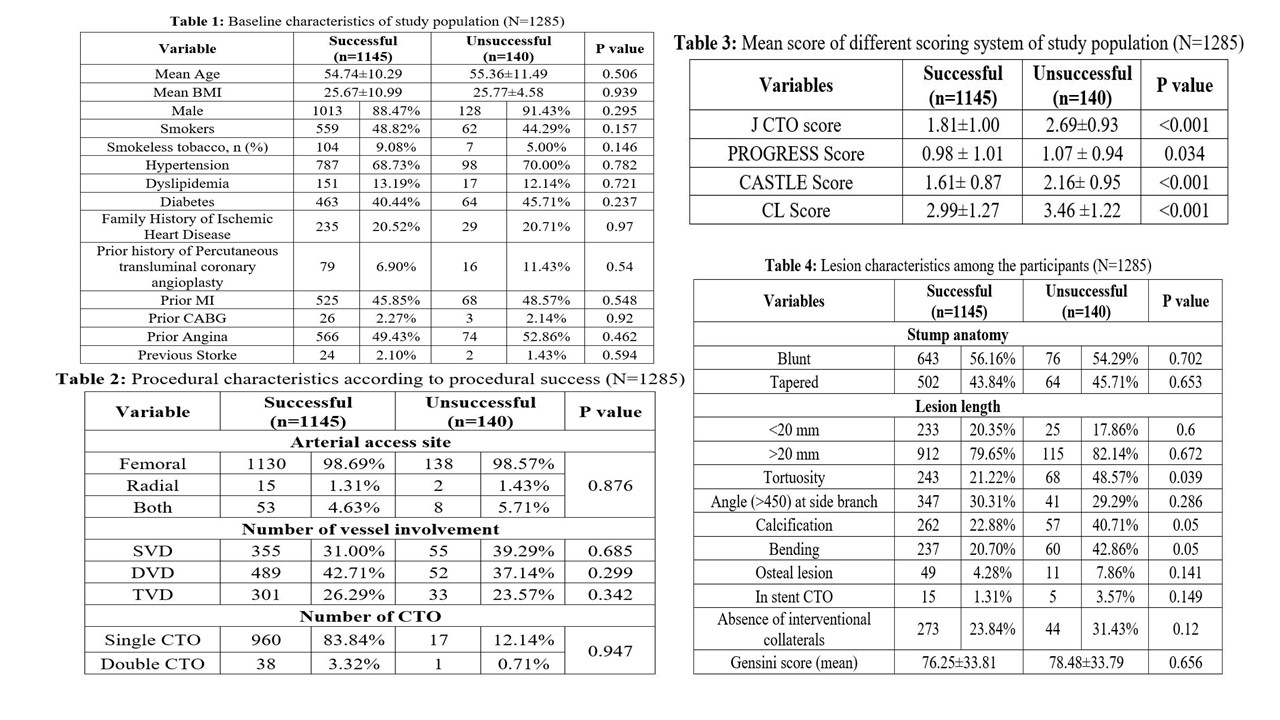
A total of 1285 patients who underwent PCI for CTO between May 2021 and October 2024 were included. Demographic, clinical, and procedural data were collected, including age, sex, cardiovascular risk factors, and scoring system results (J CTO, CASTLE, CL, and PROGRESS). All patients were followed up for one year.
Results
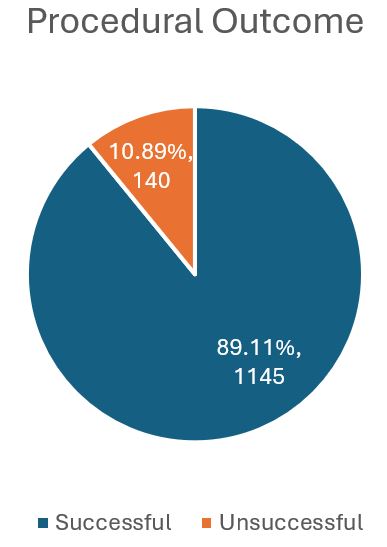
The overall success rate was 89.11% (1145/1285). Baseline characteristics, including age and BMI, were similar between successful and unsuccessful groups. Complications such as calcification (40.71% vs. 22.88%, P=0.05) and vessel bending (42.86% vs. 20.70%, P=0.05) were significantly more prevalent in unsuccessful cases. Scoring systems showed higher mean scores in the unsuccessful group (e.g., J CTO: 2.69±0.93 vs. 1.81±1.00, P<0.001). In-hospital complications, including cardiogenic shock (17.14% vs. 5.50%, P=0.001) and acute left ventricular failure (9.29% vs. 0.35%, P=0.001), were significantly more frequent in unsuccessful cases. One-year follow-up revealed higher mortality (2.86% vs. 0.70%, P=0.002) and non-fatal MI rates (2.14% vs. 0.17%).
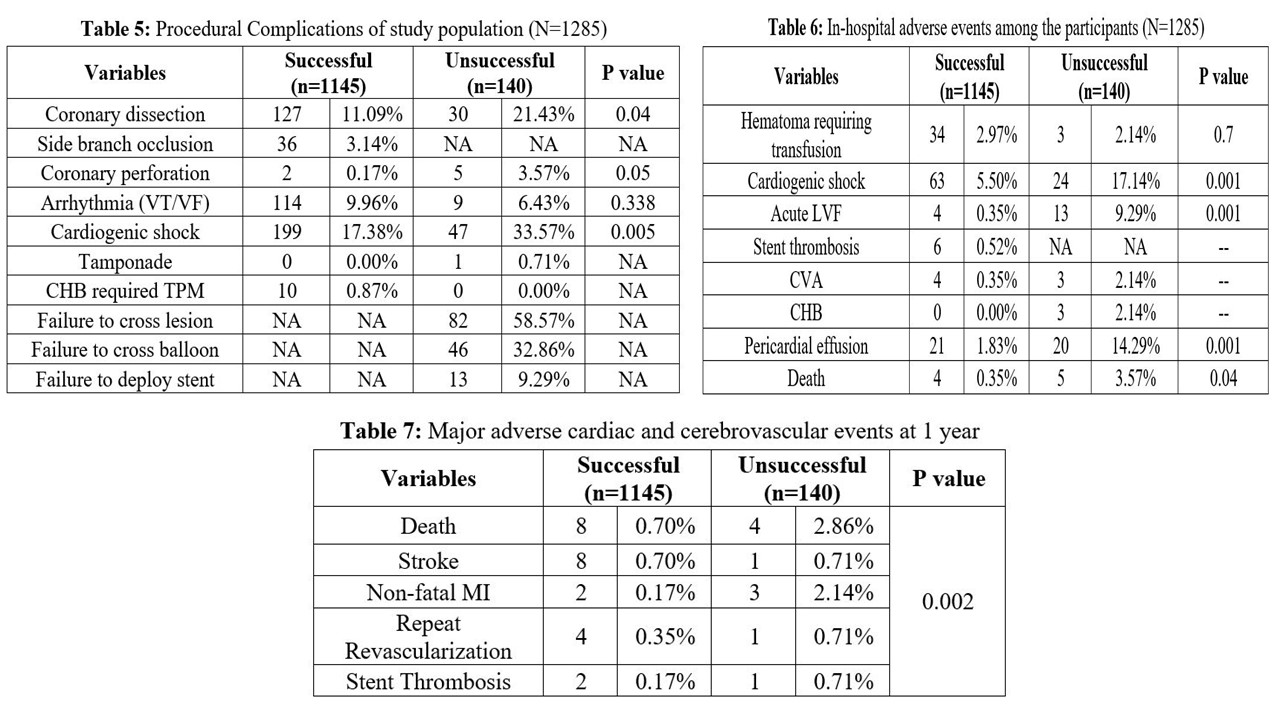
Conclusion
This study underscores the procedural complexity and significant predictors of adverse outcomes in CTO-PCI. Successful interventions correlate with lower rates of complications and improved 1-year outcomes, highlighting the need for strategic planning and risk mitigation, particularly in resource-limited settings.


