Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-078
Incidence and Temporal Trends in Permanent Pacemaker Implantation (PPI) Following Transcatheter Aortic Valve Replacement (TAVR): A Single Australian Centre Experience
By Christina Mew, Thomas Basso, Kellee Korver, Anthony Camuglia
Presenter
Christina Mew
Authors
Christina Mew1, Thomas Basso1, Kellee Korver1, Anthony Camuglia1
Affiliation
Princess Alexandra Hospital, Australia1
View Study Report
TCTAP A-078
Other Structural Interventions
Incidence and Temporal Trends in Permanent Pacemaker Implantation (PPI) Following Transcatheter Aortic Valve Replacement (TAVR): A Single Australian Centre Experience
Christina Mew1, Thomas Basso1, Kellee Korver1, Anthony Camuglia1
Princess Alexandra Hospital, Australia1
Background
TAVR is a minimally invasive treatment option for patients with severe aortic stenosis. Owing to the anatomical proximity, post TAVR conduction disturbances may occur necessitating PPI and prolong hospital stays. The reported incidence of PPI post TAVR varies with substantial site-level variation. This retrospective study aims to investigate the incidence and temporal trend in PPM rates following TAVR at a single centre.
Methods
A retrospective analysis of all patients who underwent TAVR from January 2016 to February 2024 was conducted. Patient demographics, procedural characteristics, and post-procedure outcomes were analysed. The primary endpoint was PPI incidence within 30 days post TAVR. Risk factors associated with PPI were also assessed.
Results
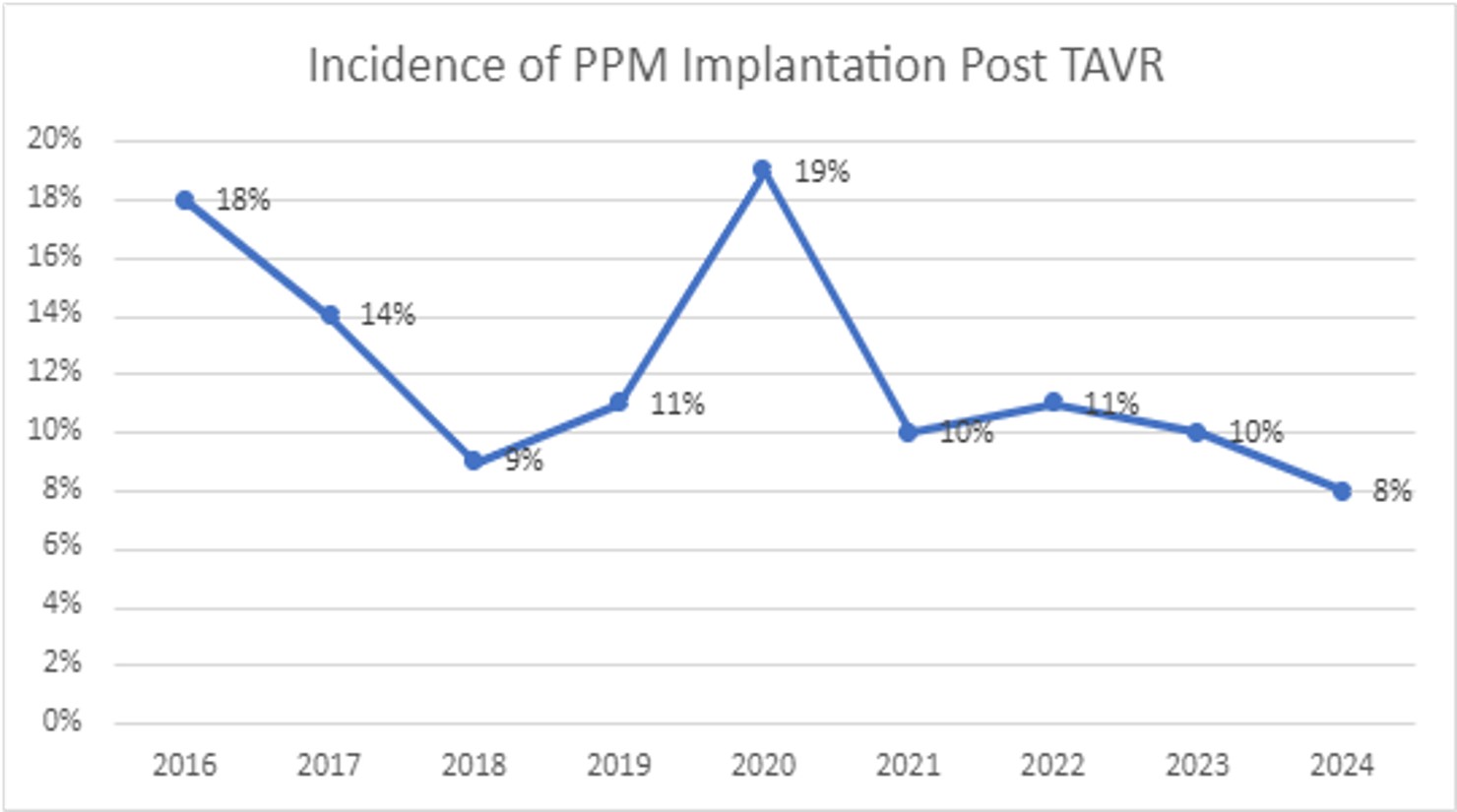
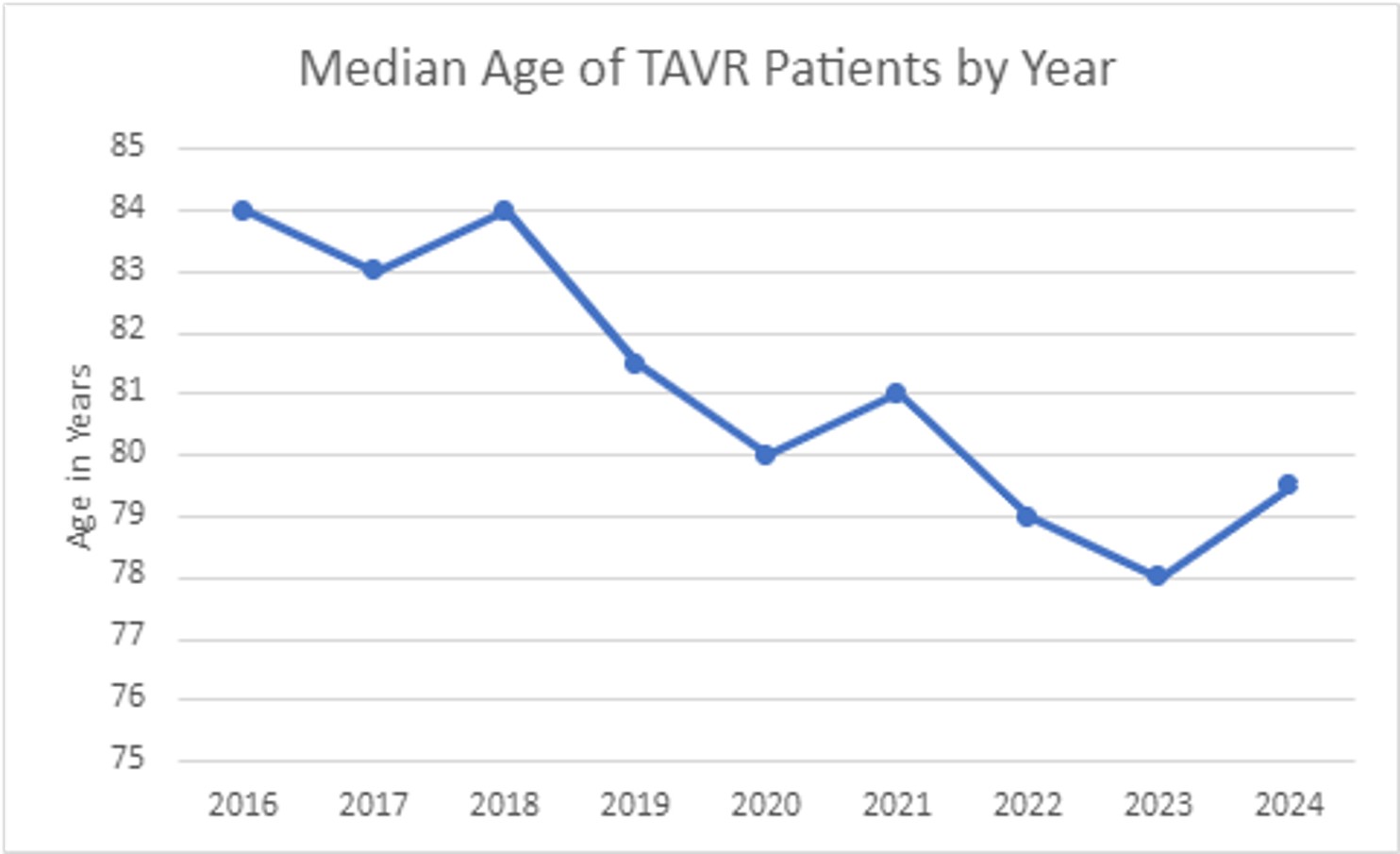
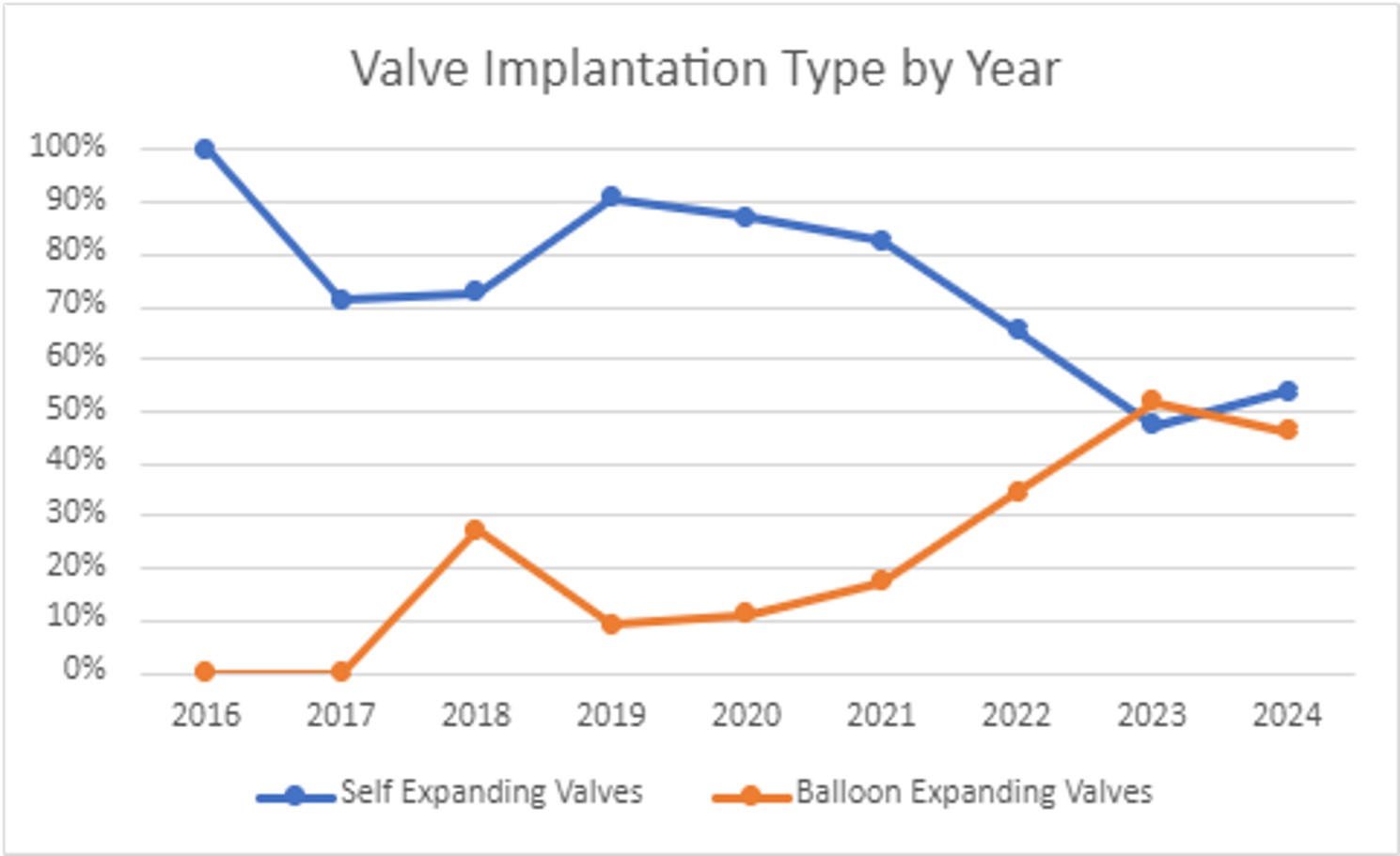
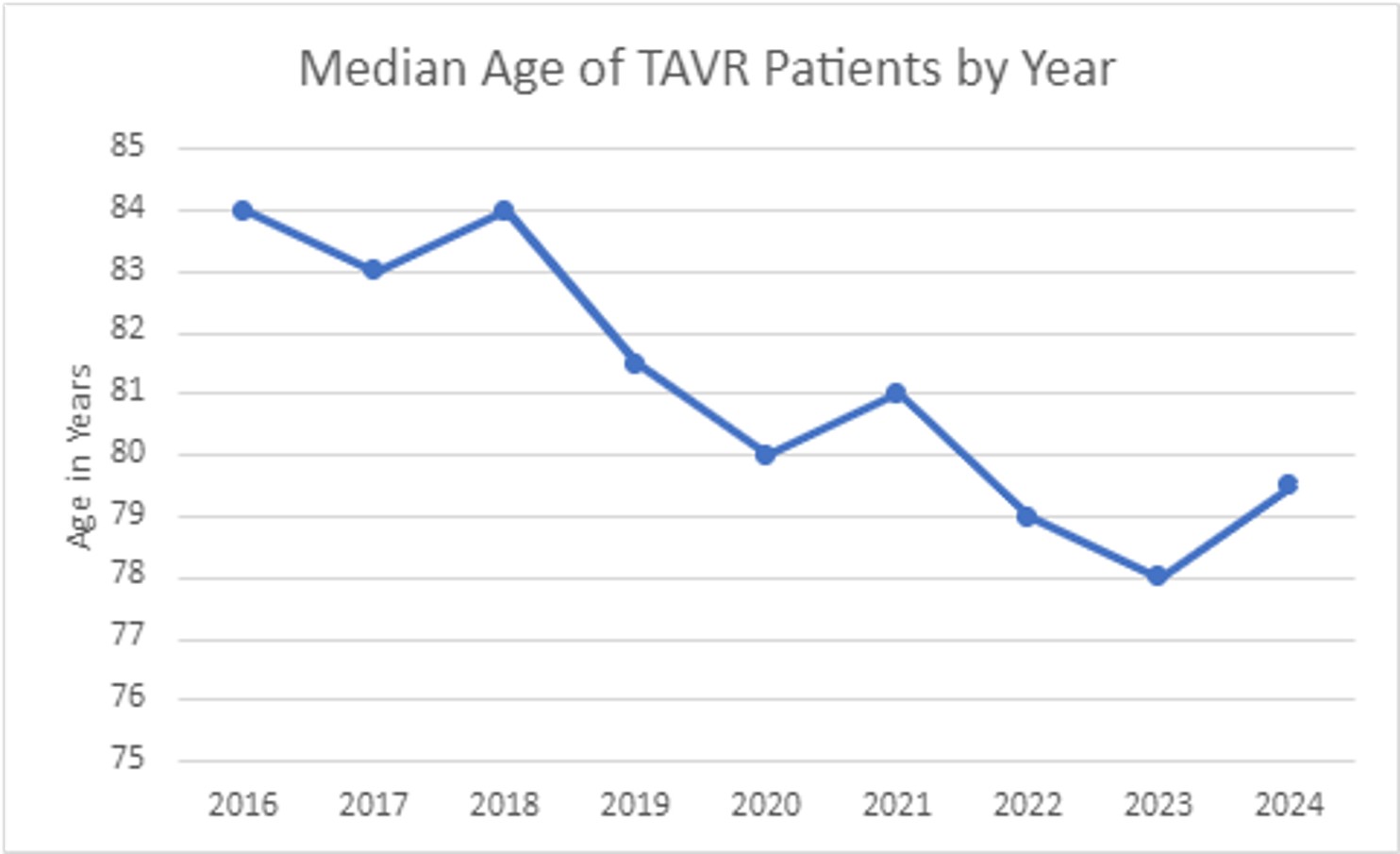
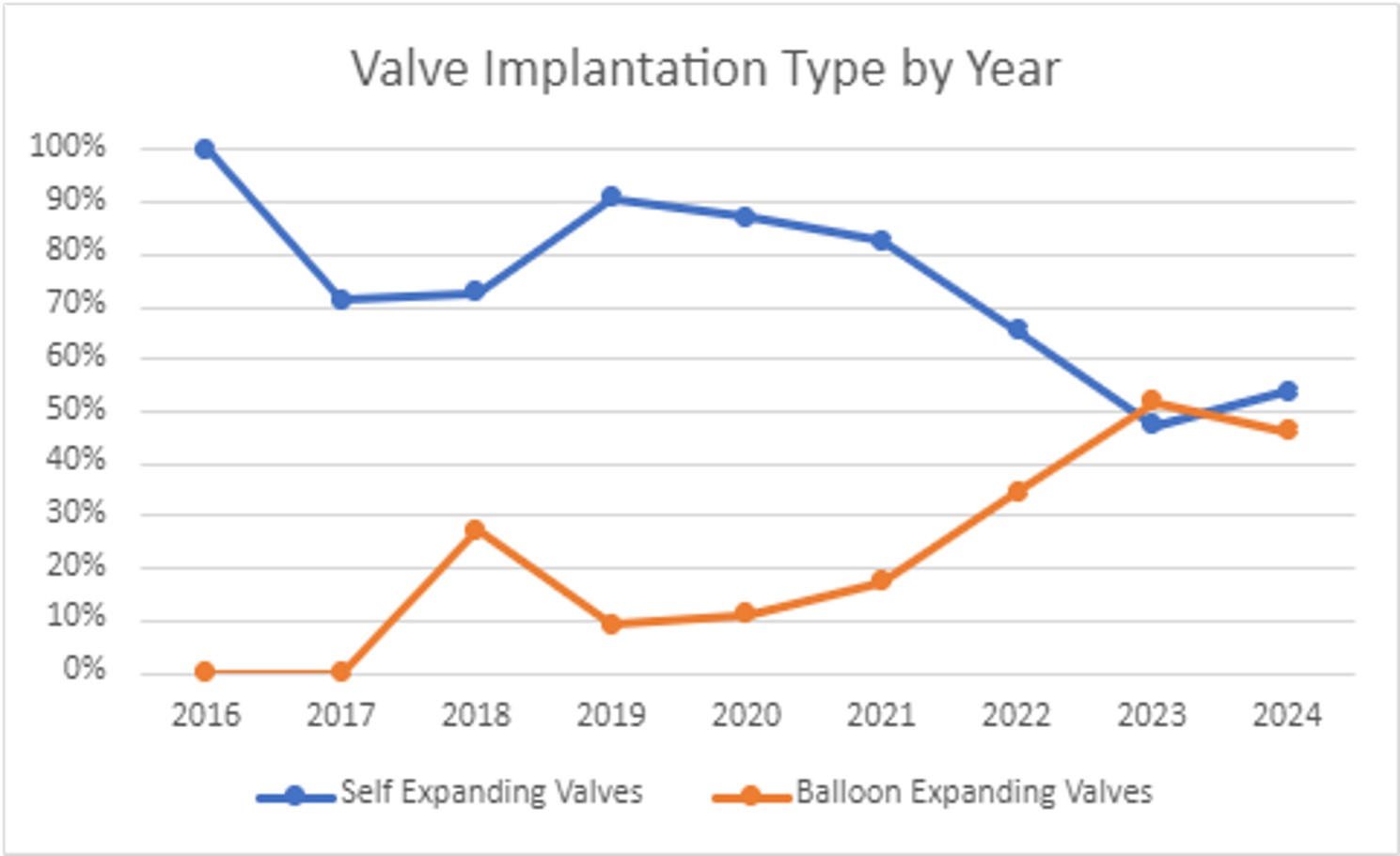
526 patients underwent TAVR during the study period. The overall PPI incidence was 12% (n = 59) with a downward trend from 2016 to 2024 (figure 1). The median age of TAVR patients also trended down and the use of balloon expanding valves trended up (figure 2 and 3). Relevant baseline conduction disease was present in 40% of the PPI group (RBBB 8%, RBBB + LAFB 12%, PR interval >200ms 14%). The average time between TAVR and PPI was 3 days. The mean length of stay was 6.2 days for PPI patients compared to 5.5 days for those not needing PPI. Two patients required hospital readmission for PPI.
Conclusion
Our single centre experience aligns with current literature which shows PPI rates of 9-26%. The downward trend of PPI at our centre is postulated to relate to a younger cohort, increasing use of balloon expandable over self expandable valves, and operator experience.


