Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-057
The Prasugrel Reduced-Dose Observation for Measuring Improvement in Safety and Effectiveness in Taiwan (PROMISE-TW) Registry
By Yuchen Wang
Presenter
YuChen Wang
Authors
Yuchen Wang1
Affiliation
Asia University Hospital, Taiwan1
View Study Report
TCTAP A-057
Pharmacotherapy (Coronary)
The Prasugrel Reduced-Dose Observation for Measuring Improvement in Safety and Effectiveness in Taiwan (PROMISE-TW) Registry
Yuchen Wang1
Asia University Hospital, Taiwan1
Background
The Prasugrel Reduced-dose Observation for Measuring Improvement in Safety and Effectiveness in Taiwan (PROMISE-TW) registry aimed to evaluate the clinical effectiveness and safety of reduced-dose prasugrel (initial 20 mg loading, maintenance 3.75 mg) in Taiwanese patients with acute or chronic coronary syndromes. Unlike the higher doses used in Western countries, the reduced dosage used in Taiwan raises questions about its safety and effectiveness, especially in preventing major adverse cardiovascular events (MACEs). Therefore, understanding the potential benefits and risks of this reduced dosage in the Taiwanese population is essential.
Methods
This study was a multicenter, retrospective cohort study conducted between January 2018 and November 2022 across 13 hospitals in Taiwan (Figure 1), enrolling a total of 1,167 patients treated with prasugrel. Eligible patients were those aged 18 or older, diagnosed with acute coronary syndrome (ACS) or chronic coronary syndrome (CCS), and treated with reduced-dose prasugrel. Data were collected retrospectively from hospital and outpatient records, including demographics, comorbidities, concurrent medications, and angiographic results. The primary outcome was the incidence of MACEs within one year, specifically focusing on cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke. Secondary outcomes encompassed ischemic and bleeding events, such as MACE plus unplanned revascularization (composite ischemic events), all-cause mortality, ISTH major bleeding, stent thrombosis, and other clinical outcomes.


Results
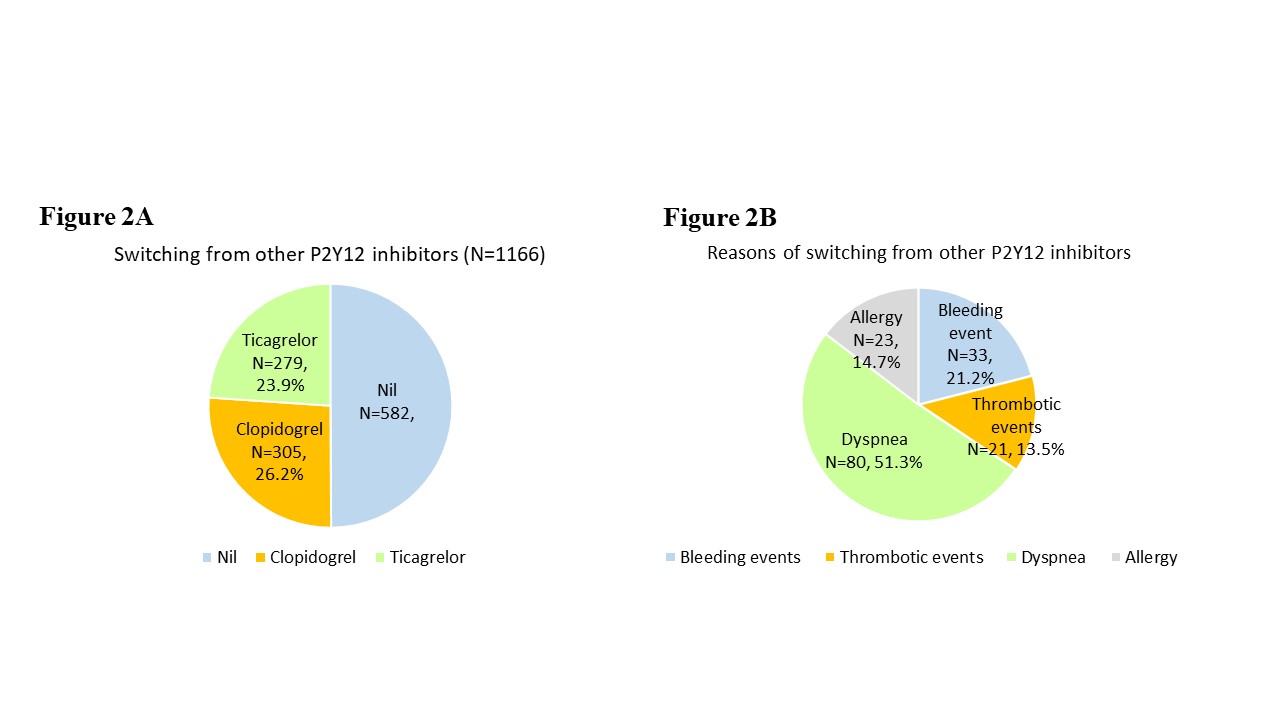
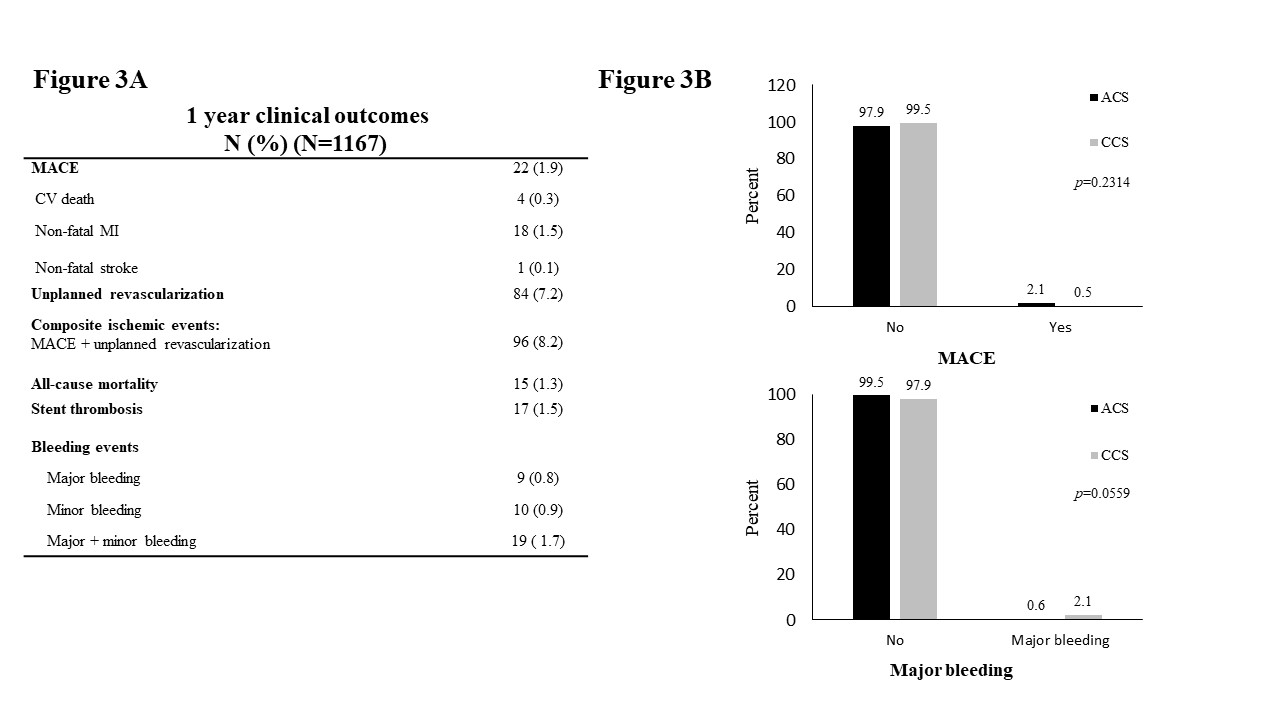
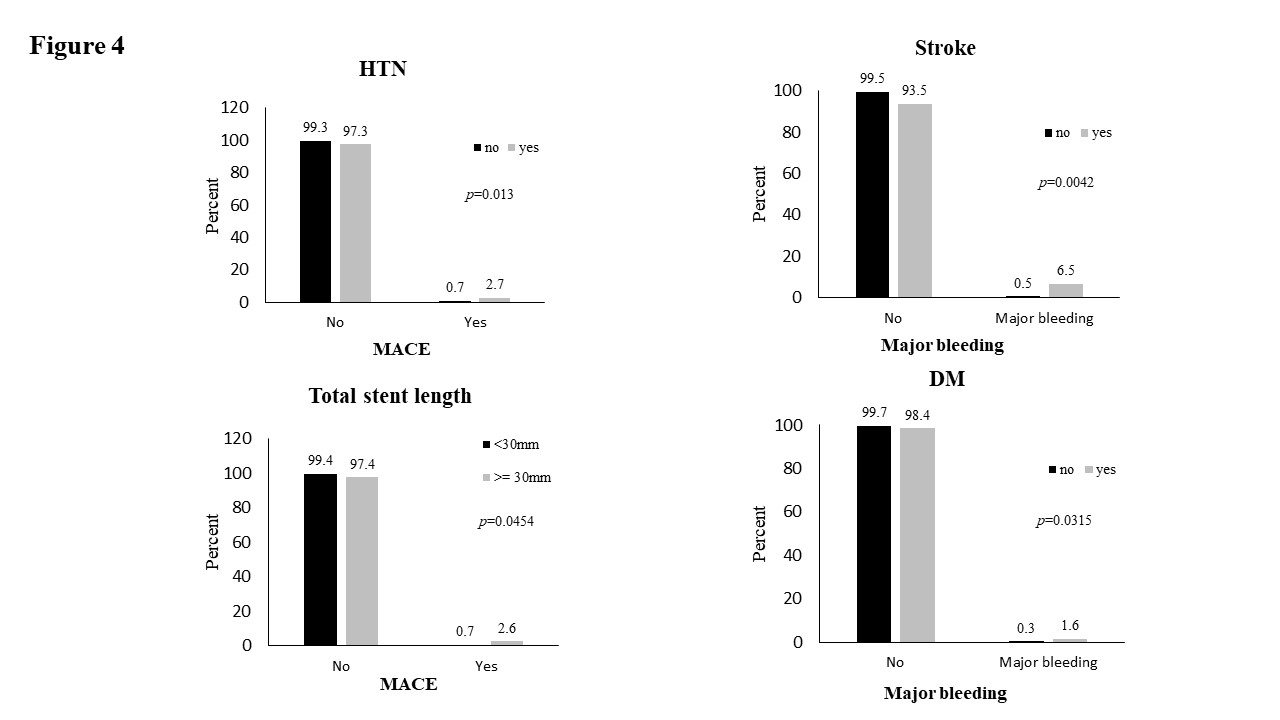
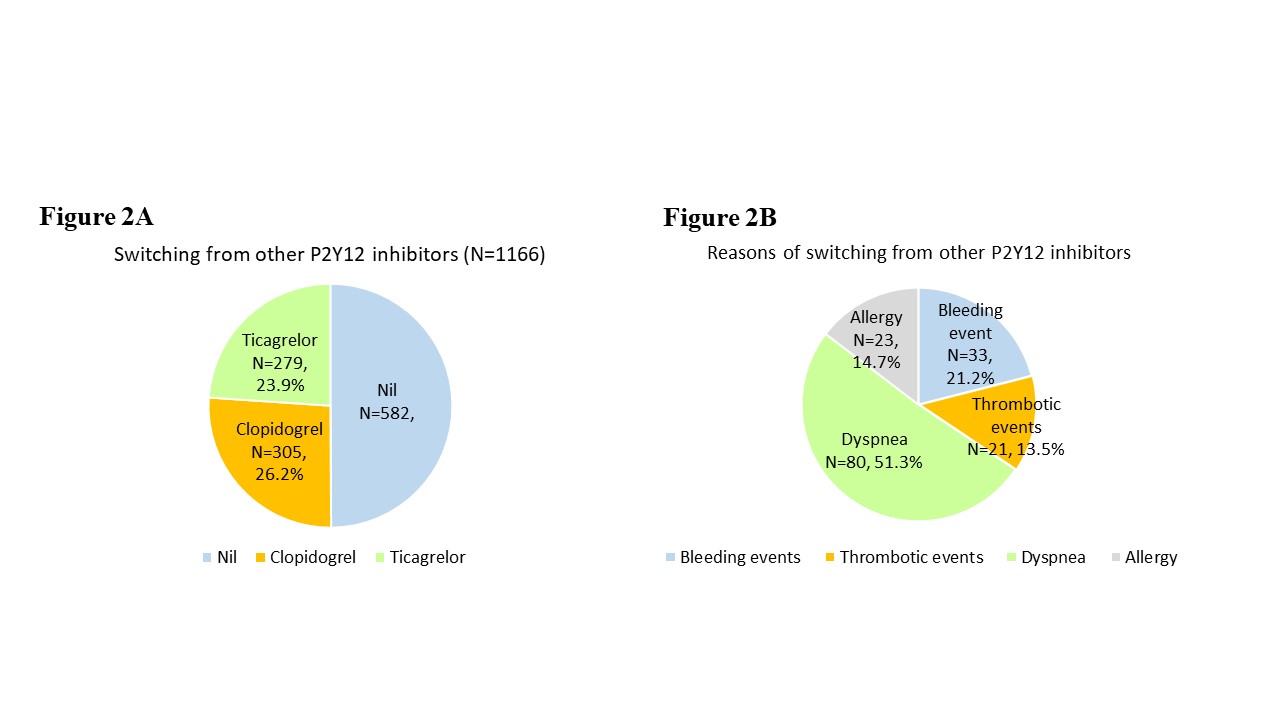
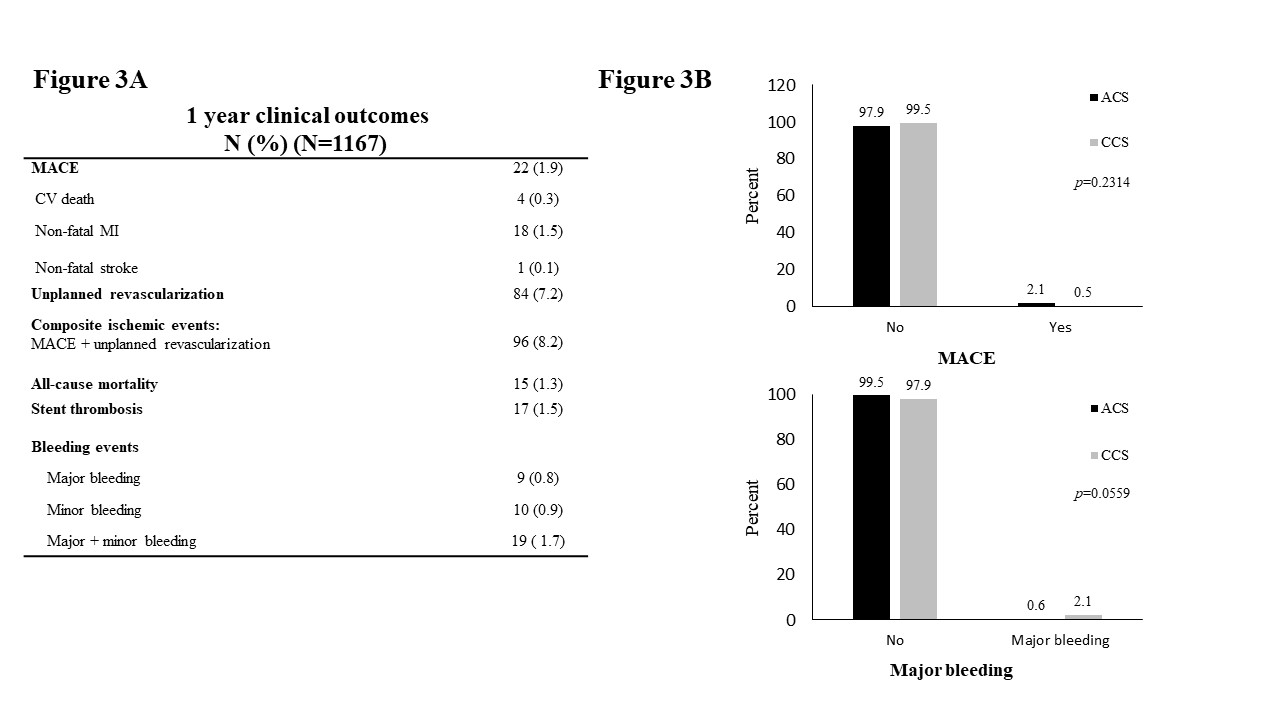
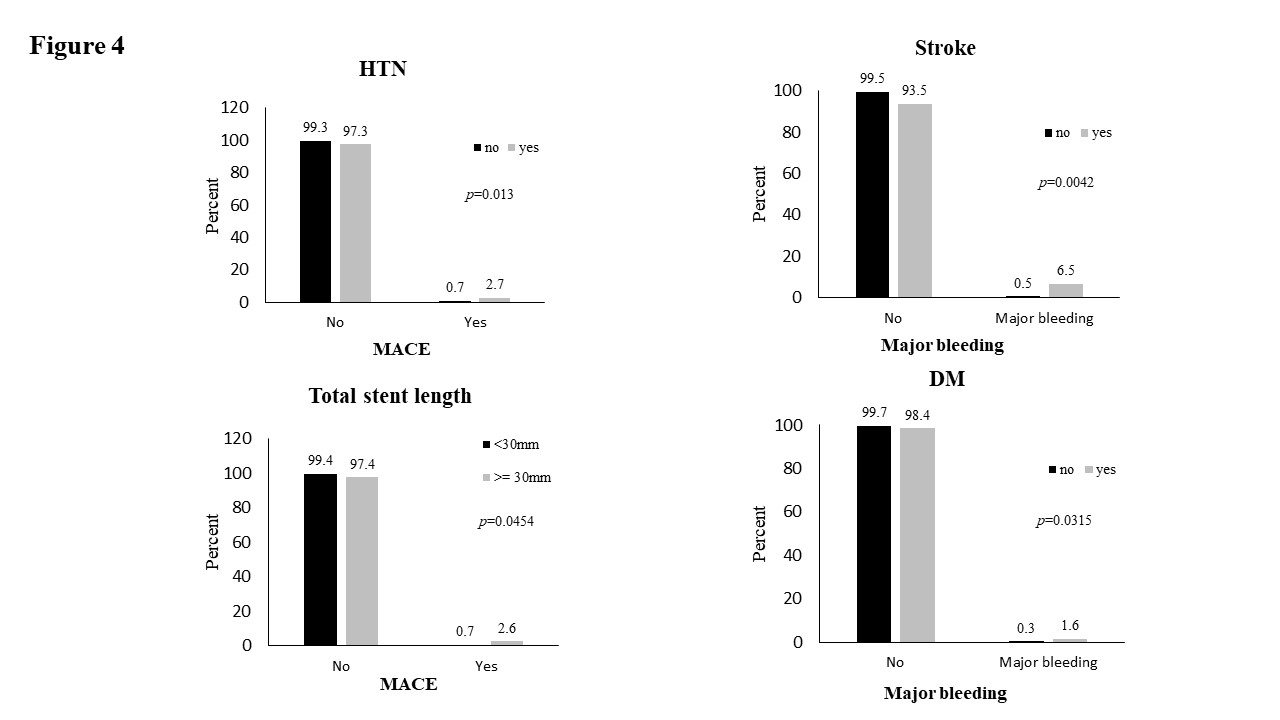
The study enrolled 1,167 patients, of whom 963 (83%) were treated for ACS. Most patients underwent percutaneous coronary intervention (PCI) (90.8%), and prasugrel was administered either alone or in combination with aspirin and/or other anticoagulants. Within the study population, 26.2% transitioned from Clopidogrel, while 23.9% switched from Ticagrelor (Figure 2A). The primary reason for switching was dyspnea (51.3%), followed by bleeding events (21.2%), allergy (14.7%), and thrombotic events (13.5%) (Figure 2B). The one-year clinical outcomes are presented in Figure 3A. The overall incidence of MACEs within one year was 1.9%, comprising cardiovascular death (0.3%), non-fatal myocardial infarction (1.5%), and non-fatal stroke (0.1%). The rate of major bleeding events was 0.8% (9 patients), while the combined rate of major and minor bleeding events was 1.7% (19 patients). Subgroup analysis revealed that patients with ACS had a similar incidence of MACEs compared to those with CCS. However, there was a trend toward an increased incidence of major bleeding in the CCS population (Figure 3B). Additionally, patients with hypertension and those receiving stents longer than 30 mm were found to have an increased risk of MACE. The use of reduced-dose prasugrel appeared effective across other subgroups, including those with high-risk characteristics such as diabetes, chronic kidney disease, and advanced age. Notably, patients with a history of stroke and diabetes showed an increased risk of major bleeding events (Figure 4).
Conclusion
The results of the PROMISE-TW registry suggest that reduced-dose prasugrel may be a viable option for Taiwanese patients with ACS or CCS, providing an acceptable balance between efficacy in preventing MACEs and safety in terms of bleeding risk. The incidence of major bleeding events was relatively low, supporting the feasibility of using reduced-dose prasugrel in populations with higher bleeding risk, such as East Asian patients. These findings could potentially inform local clinical guidelines and patient management strategies, helping to tailor antiplatelet therapy to the specific needs of the Taiwanese population. Future studies are warranted to further investigate the long-term effects and explore subgroup analyses to optimize treatment strategies.


