Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-093
Role of Cardiac Myosin Inhibitors in the Treatment of Hypertrophic Cardiomyopathy: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials
By Naiela Ennaji Almansouri, Ahmed Ibrahim, Ahmed Samir Mujahed, Ahmad S. Ghattas, Mahmoud Sayed Ahmed, Omar M. Ramdan, Ahmed A. Lashin, Suhaina Amir, Ismail A. Ibrahim
Presenter
Naiela Ennaji Almansouri
Authors
Naiela Ennaji Almansouri1, Ahmed Ibrahim2, Ahmed Samir Mujahed2, Ahmad S. Ghattas3, Mahmoud Sayed Ahmed4, Omar M. Ramdan5, Ahmed A. Lashin6, Suhaina Amir7, Ismail A. Ibrahim8
Affiliation
Libyan Biotechnology Research Center, Libya1, Alexandria University, Egypt2, Helwan Medical School, Egypt3, Cairo University, Egypt4, Al-Azhar University, Egypt5, Benha University, Egypt6, Dow University of Health Sciences, Pakistan7, Fenerbahce University, Turkey8
View Study Report
TCTAP A-093
Vascular Heart Disease and Cardiomyopathies
Role of Cardiac Myosin Inhibitors in the Treatment of Hypertrophic Cardiomyopathy: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials
Naiela Ennaji Almansouri1, Ahmed Ibrahim2, Ahmed Samir Mujahed2, Ahmad S. Ghattas3, Mahmoud Sayed Ahmed4, Omar M. Ramdan5, Ahmed A. Lashin6, Suhaina Amir7, Ismail A. Ibrahim8
Libyan Biotechnology Research Center, Libya1, Alexandria University, Egypt2, Helwan Medical School, Egypt3, Cairo University, Egypt4, Al-Azhar University, Egypt5, Benha University, Egypt6, Dow University of Health Sciences, Pakistan7, Fenerbahce University, Turkey8
Background
Hypertrophic cardiomyopathy (HCM) is the most prevalent hereditary cardiac condition globally. The existing pharmaceutical therapy choices are limited. Cardiac myosin inhibitors (CMIs), including mavacamten and aficamten, address the primary underlying pathophysiology of HCM. However, the degree of their effectiveness and safety remains uncertain owing to the restricted population examined.
Methods
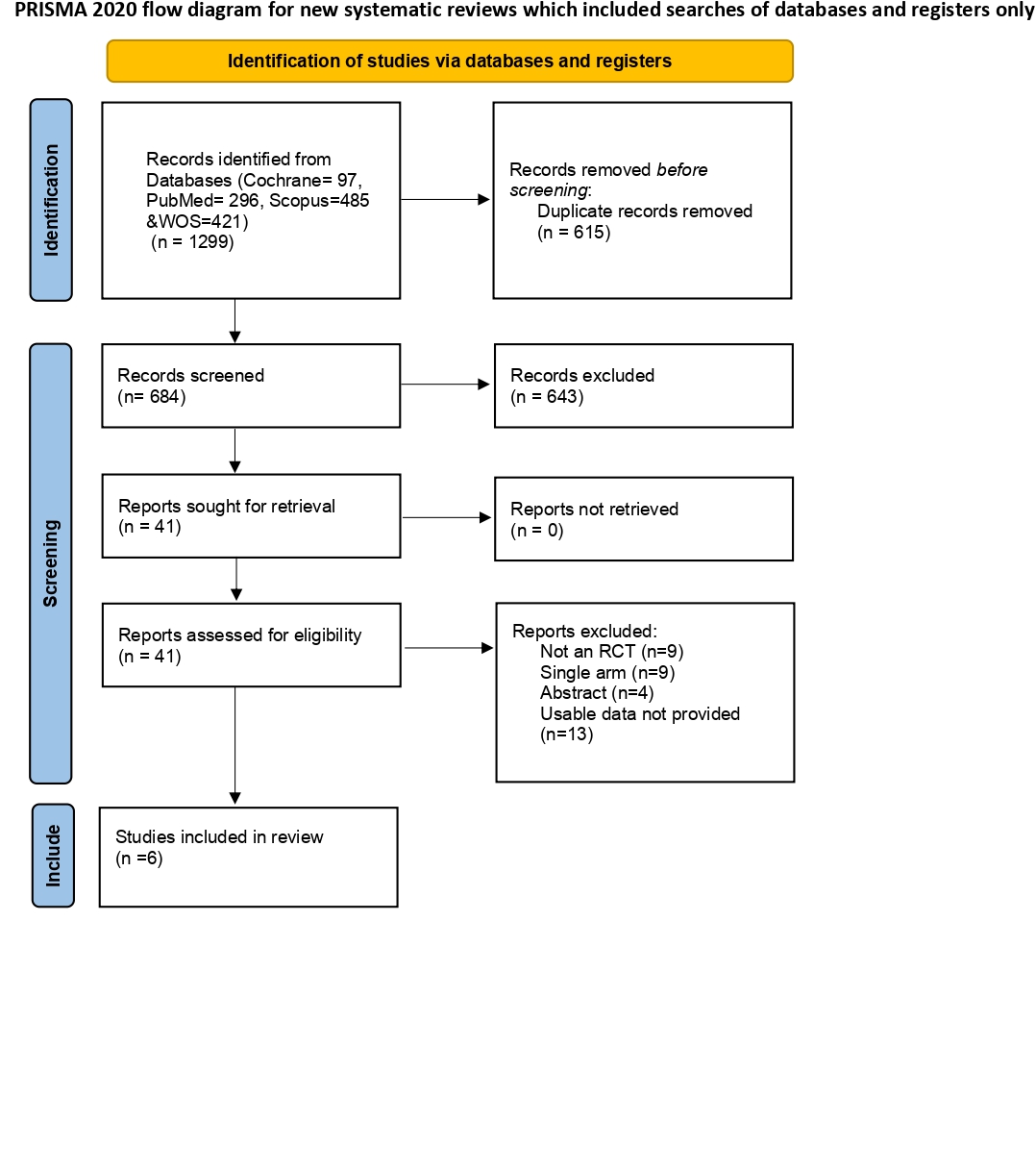
Following Prisma guidelines ( Figure 1), we executed an extensive search on several electronic databases, including PubMed, Scopus, Cochrane, and Web of Science, to find RCTs that assessed the effectiveness and safety of CMIs in HCM. A meta-analysis using the Netmeta package in R studio 4.3.2 was performed. Continuous data were pooled using mean differences (MD) whereas dichotomous data were analyzed using risk ratios (RR) with 95 % confidence intervals (CIs).
Results
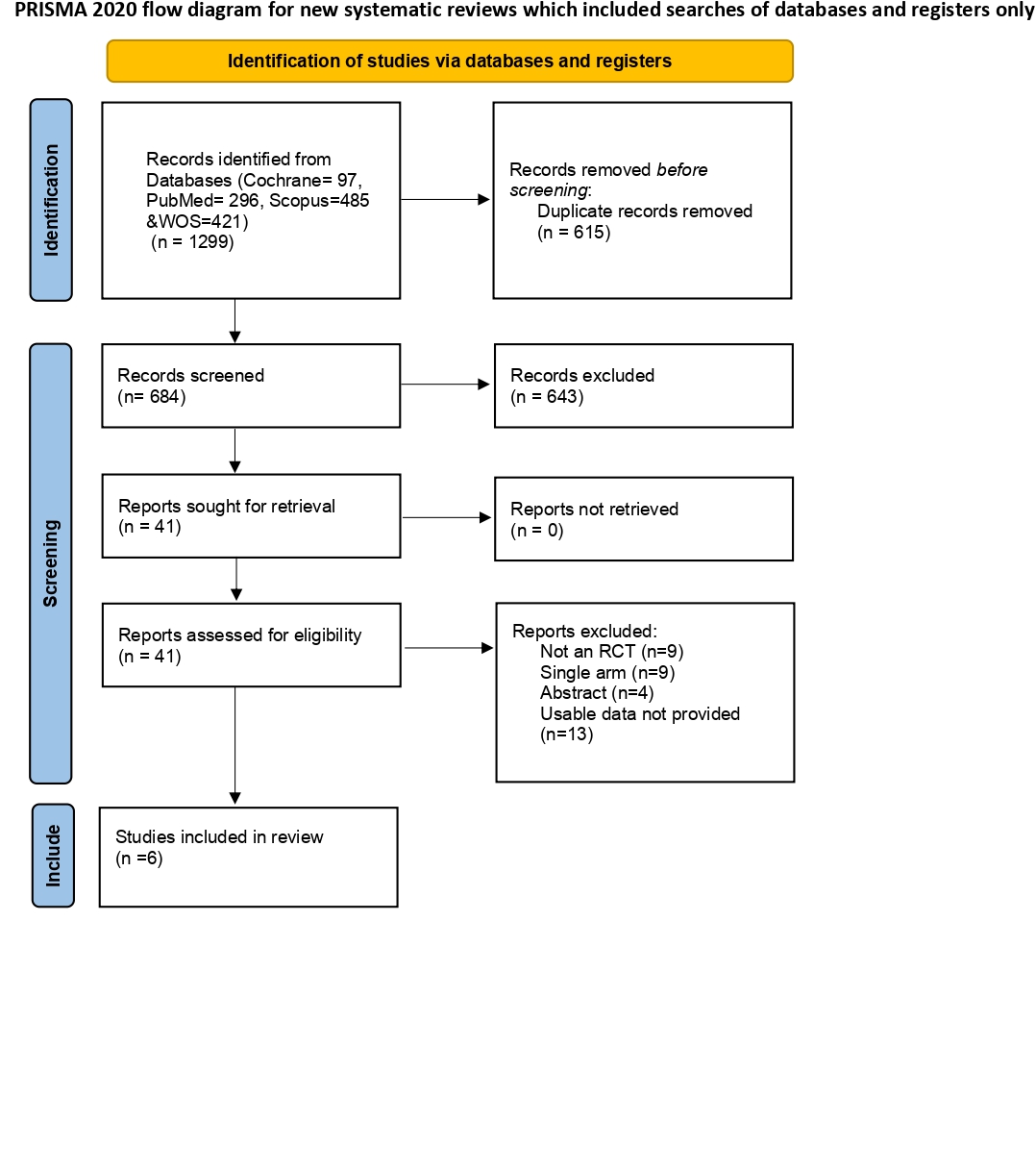
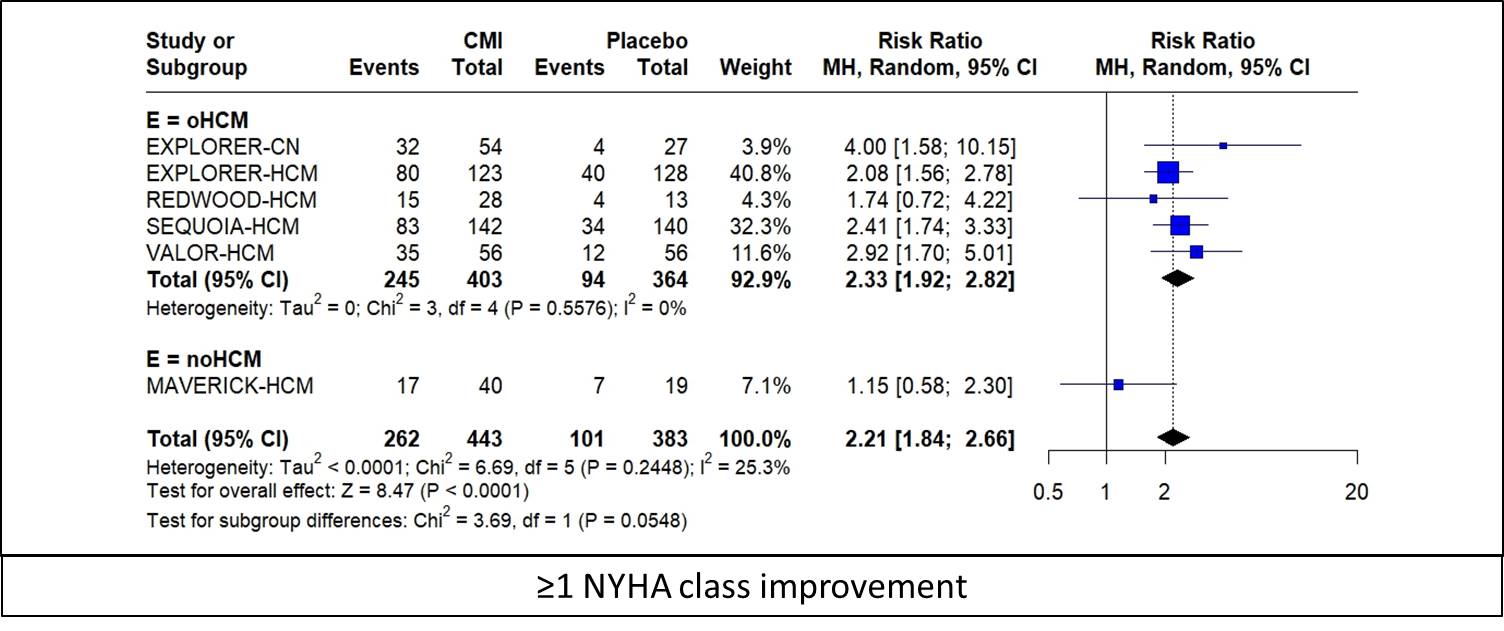
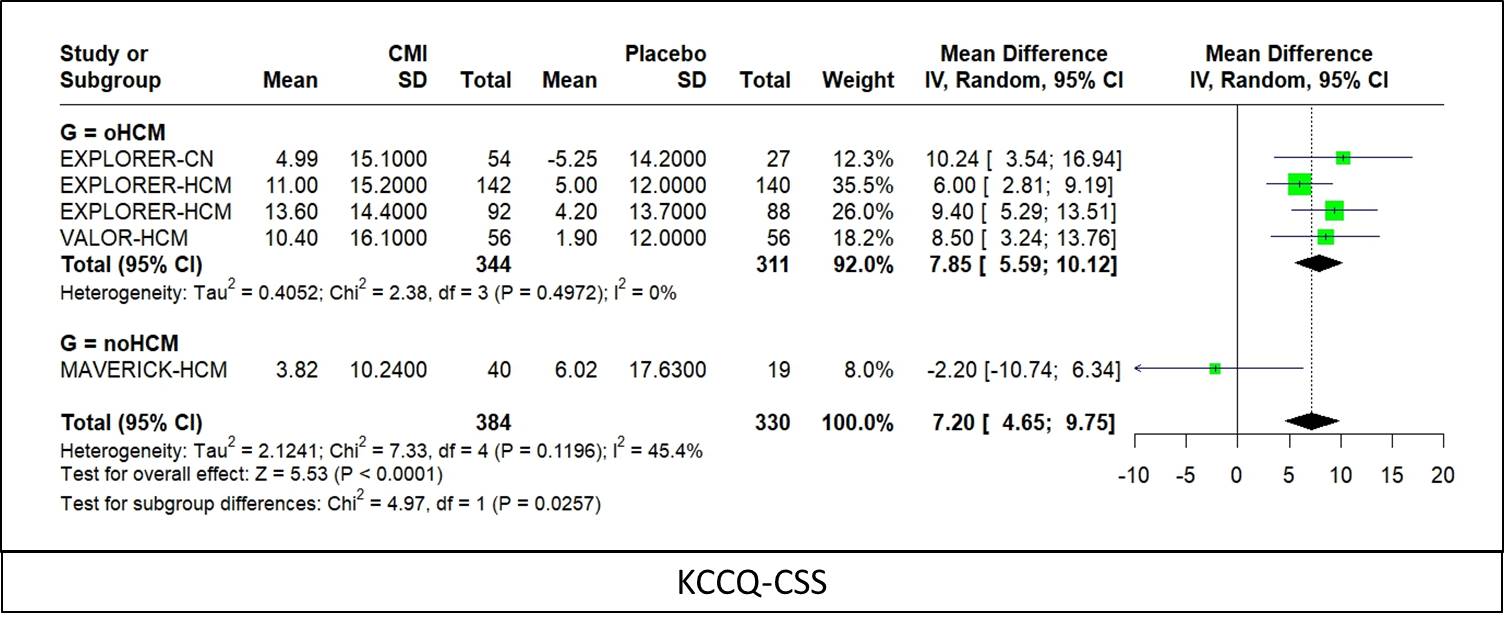
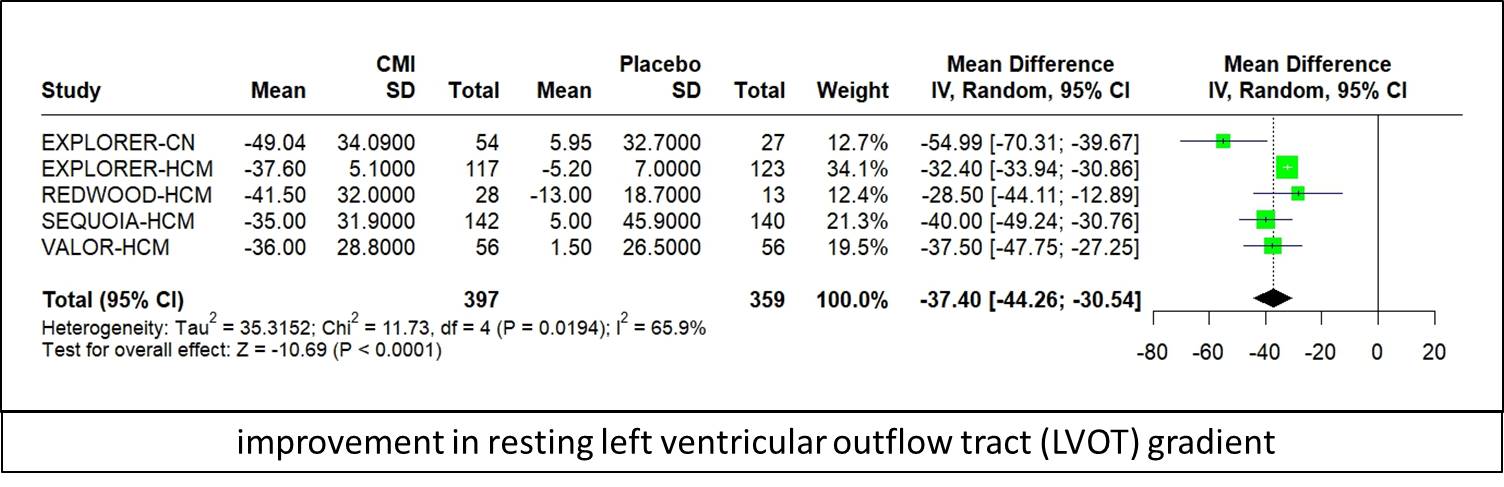
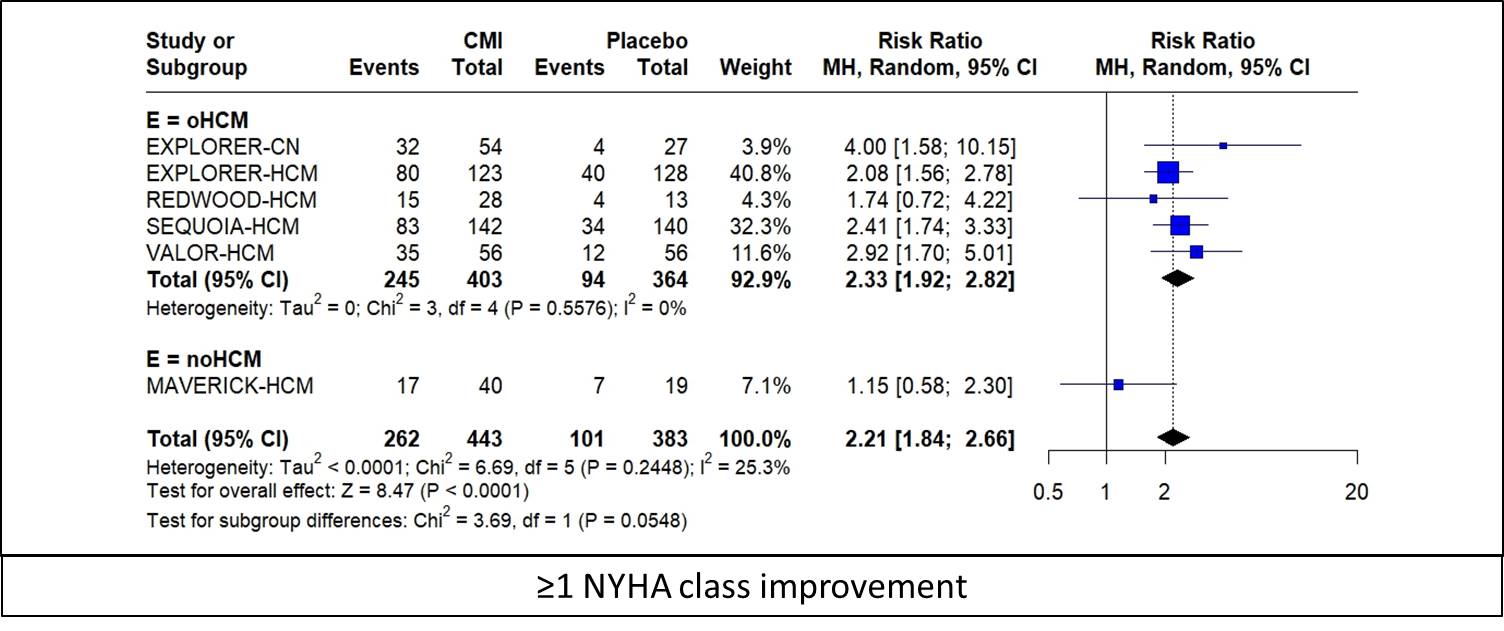
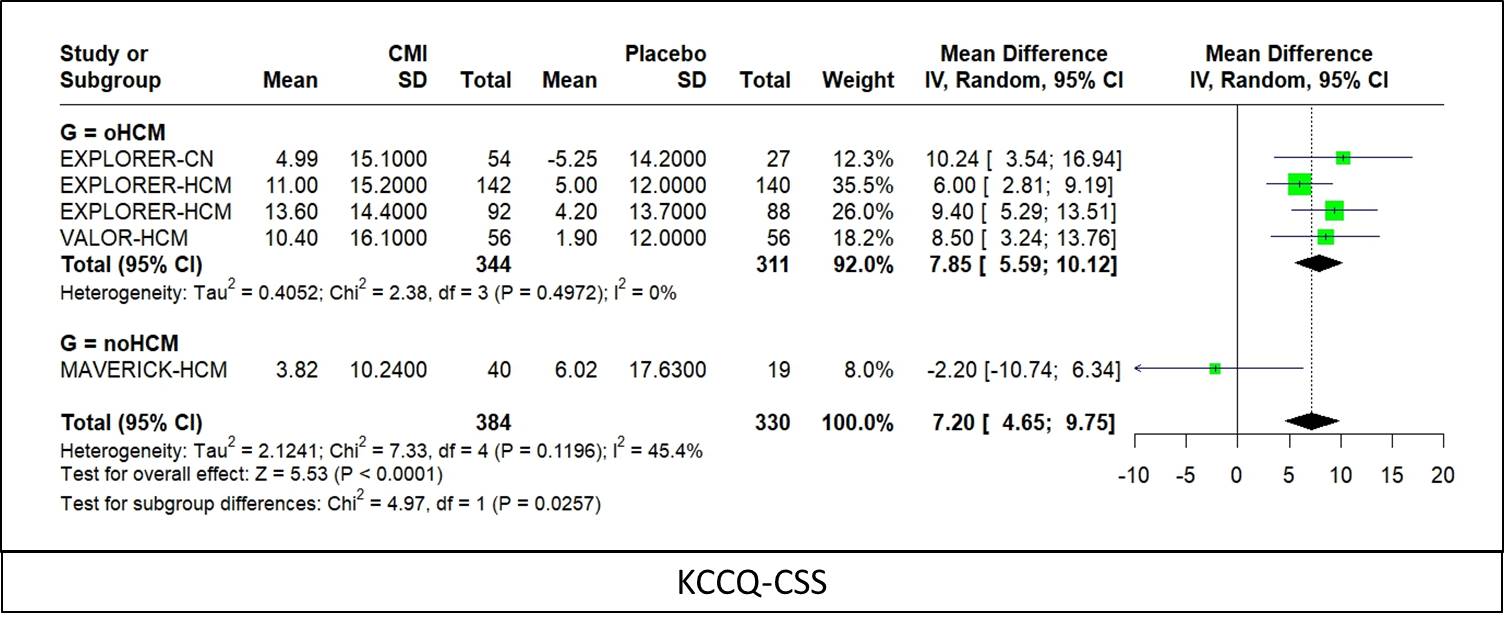
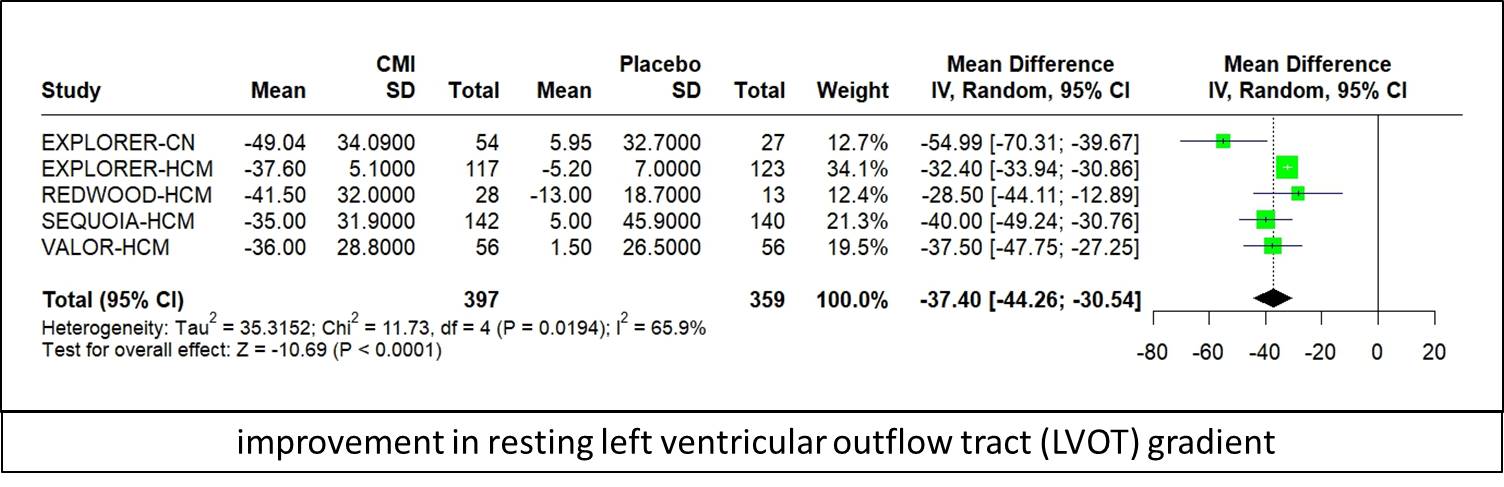
Six RCTs with 826 patients participated, 53.6 % (443) were assigned to the CMIs group and 46.4 % (383) served as controls. Four trials focused on mavacamten, while two concentrated on aficamten. Notably, five trials involved patients diagnosed with hypertrophic obstructive cardiomyopathy (oHCM), whereas one included only patients with hypertrophic non-obstructive cardiomyopathy (noHCM). CMIs were linked to a significantly higher rate of ≥1 NYHA class improvement compared to placebo (RR: 2.21, 95 % CI: 1.84, 2.66; p < 0.0001; I2= 25.3 % ; Figure 2), and change from baseline in Clinical Summary Score of the Kansas City Cardiomyopathy Questionnaire score (KCCQ-CSS) (MD: 7.20, 95 %CI: 4.65, 9.75; p = 0.025; I2= 45.4 % ; Figure 3). In sub-group analysis, patients with oHCM attained higher rates of ≥1 NYHA class improvement (RR:2.33, 95 % CI: 1.92, 2.82) and improvement in KCCQ-CSS scores (MD: 7.85, 95 %CI: 5.59, 10.12) compared to noHCM patients. CMIs were also linked to improvement in resting left ventricular outflow tract (LVOT) gradient (MD: -37.40, 95 % CI: - 44.28, - 30.53; p < 0.0001; I2 = 65.9 % ; Figure 4 ), Valsalva LVOT gradient(MD: - 47.44, 95 % CI: - 59.85, - 35.04; p < 0.0001; I2= 84.3 %), postexercise LVOT gradient (MD: - 37.11, 95 % CI: - 44.34, - 29.87; p <0.0001; I2 = 0 %), Left ventricular mass index (LVMI) (MD: - 16.83, 95 %CI: - 30.28, - 3.38; p = 0.014; I2 = 87.5 %), and lower rates of Septal reduction therapy (SRT) (RR: 0.30, 95 % CI: 0.22, 0.40; p < 0.0001; I2 = 0 %), but also there was a decline in left ventricular ejection fraction (LVEF) (MD:- 4.15, 95 % CI: - 5.20, - 3.10; p < 0.0001; I2 = 42.5 %). There were no significant differences between CMIs and placebo in the composite functional outcome, ≥1 treatment-emergent adverse event, ≥1 serious adverse event, atrial fibrillation, and any score LVEF < 50%.
Conclusion
Our meta-analysis demonstrated that CMIs (mavacamten, aficamten) improved NYHA class, KCCQ-CSS scores, LVOT gradients, and LVMI. Simultaneously lowering the frequency of SRT in patients with HCM. There was a significant decline in LVEF. New large-scale multicenter RCTs are required to confirm or refute our findings and provide more reliable results.


