Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-065
The Influence of Ascending Aorta Dilatation on Transcatheter Aortic Valve Implantation (TAVI) Outcomes: Unraveling the Risks and Outcomes
By Pandit Bagus Tri Saputra, Wynne Widiarti, Ali Mustofa, Cornelia Ghea Savitri, Johanes Nugroho Eko Putranto, Faisal Yusuf Ashari, Chaq El Chaq Zamzam Multazam, Firas Farisi Alkaff, Mario D'Oria
Presenter
Wynne Widiarti
Authors
Pandit Bagus Tri Saputra1, Wynne Widiarti1, Ali Mustofa1, Cornelia Ghea Savitri1, Johanes Nugroho Eko Putranto1, Faisal Yusuf Ashari2, Chaq El Chaq Zamzam Multazam3, Firas Farisi Alkaff4, Mario D'Oria5
Affiliation
Universitas Airlangga, Indonesia1, University of Manchester, United Kingdom2, Imperial College London, United Kingdom3, University Medical Center Groningen, Netherlands4, University of Trieste, Italy5
View Study Report
TCTAP A-065
Complex TAVR
The Influence of Ascending Aorta Dilatation on Transcatheter Aortic Valve Implantation (TAVI) Outcomes: Unraveling the Risks and Outcomes
Pandit Bagus Tri Saputra1, Wynne Widiarti1, Ali Mustofa1, Cornelia Ghea Savitri1, Johanes Nugroho Eko Putranto1, Faisal Yusuf Ashari2, Chaq El Chaq Zamzam Multazam3, Firas Farisi Alkaff4, Mario D'Oria5
Universitas Airlangga, Indonesia1, University of Manchester, United Kingdom2, Imperial College London, United Kingdom3, University Medical Center Groningen, Netherlands4, University of Trieste, Italy5
Background
The influence and clinical implications of ascending aorta dilatation (AAD) on transcatheter aortic valve implantation (TAVI) outcomes remain ambiguous, largely due to the scarcity and inconsistency of available data. AAD is frequently observed in patients with aortic stenosis and may pose additional procedural challenges, potentially heightening the associated risks. This meta-analysis aims to provide a comprehensive evaluation of TAVI outcomes in patients with AAD versus those without, with a particular emphasis on peri-procedural complications, long-term mortality, and overall procedural efficacy.
Methods
A thorough literature search was performed across multiple scientific databases, including PubMed, ScienceDirect, Web of Science, Springer, Cochrane, and ClinicalTrials.gov, up to March 2024, in order to identify studies comparing TAVI outcomes between patients with AAD and those without. The evaluated outcomes encompassed mortality rates and procedural complications . Statistical analyses were conducted using relative risk (RR) and mean difference (MD) calculations, with heterogeneity quantified through I² statistics.
Results
Ten studies involving 204,078 patients were included and analyzed. The pooled analysis indicated that patients with AAD had a significantly higher likelihood of experiencing paravalvular leakage (RR 1.56, 95% CI 1.32–1.84, p<0.00001) and aortic dissection (RR 3.55, 95% CI 1.79–7.06, p=0.0003) compared to those without AAD. However, no statistically significant differences were observed in peri-procedural death rates (RR 1.09, 95% CI 0.83–1.42, p=0.53) or one-year survival loss (RR 0.79, 95% CI 0.51–1.23, p=0.30). Furthermore, survival rates at three and five years remained comparable between the groups. The occurrence of other complications, including myocardial infarction, permanent pacemaker implantation, conversion to open surgery, and secondary valve implantation, showed no significant variation, indicating that AAD does not substantially influence long-term survival or procedural safety.
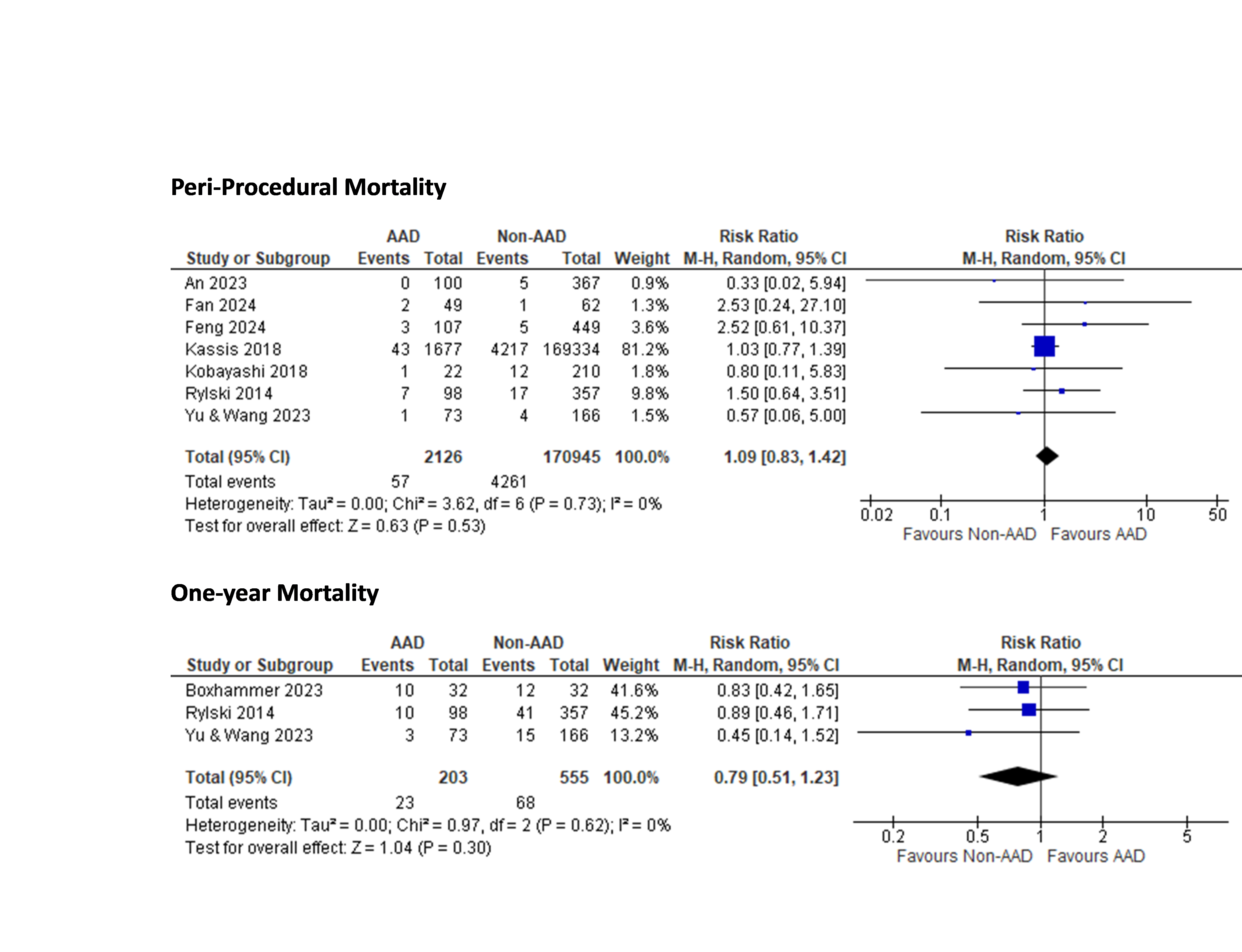
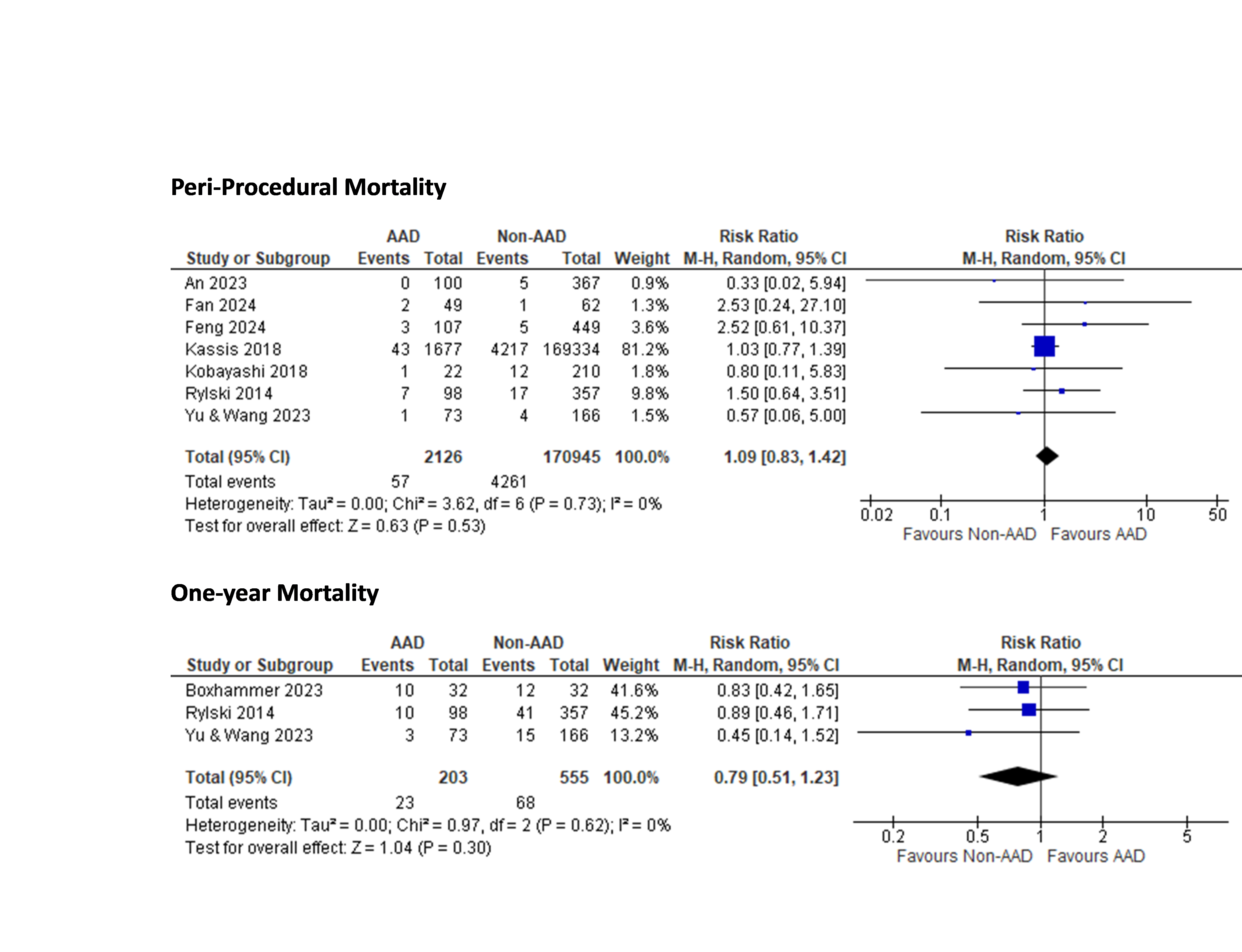
Conclusion
Although patients with AAD experience a higher incidence of aortic dissection and paravalvular leakage, these complications do not translate into an increased risk of short-term or long-term mortality. This finding underscores the robustness of TAVI as a safe and effective treatment strategy for individuals with AAD. Furthermore, advancements in procedural techniques, valve technology, and perioperative management have contributed to improved outcomes, minimizing the impact of anatomical complexities associated with AAD. Given the comparable survival rates between patients with and without AAD, TAVI remains as a viable option, offering a minimally invasive alternative with significant benefits in terms of recovery and quality of life.