Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-026
Long-Term Clinical Outcomes of Successful Chronic Total Occlusion Revascularization in Patients With Reduced Left Ventricular Ejection Fraction
By Jihun Ahn, Seung-Woon Rha
Presenter
JIHUN AHN
Authors
Jihun Ahn1, Seung-Woon Rha2
Affiliation
Eulji University Daejeon Hospital, Korea (Republic of)1, Korea University Guro Hospital, Korea (Republic of)2
View Study Report
TCTAP A-026
CTO
Long-Term Clinical Outcomes of Successful Chronic Total Occlusion Revascularization in Patients With Reduced Left Ventricular Ejection Fraction
Jihun Ahn1, Seung-Woon Rha2
Eulji University Daejeon Hospital, Korea (Republic of)1, Korea University Guro Hospital, Korea (Republic of)2
Background
Background: The benefits of revascularization in chronic totalocclusion (CTO) patients with reduced left ventricular ejection fraction (LVEF)still remain conflicting.
Methods
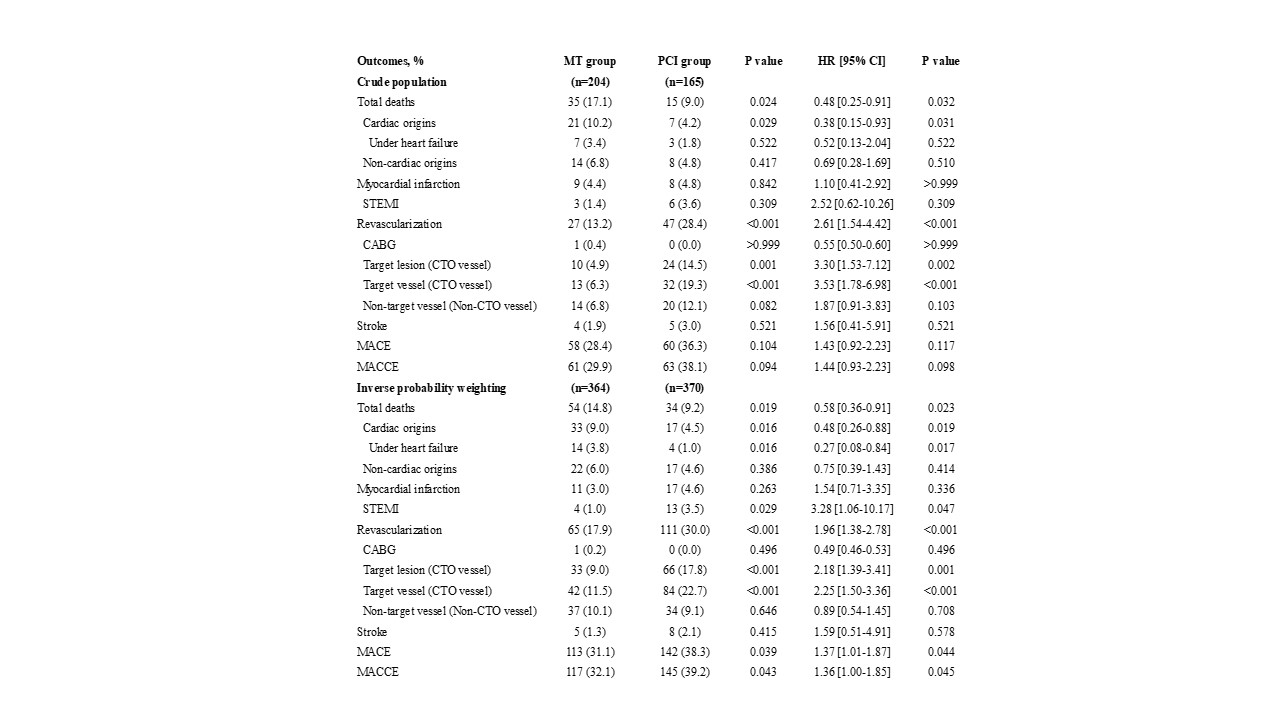
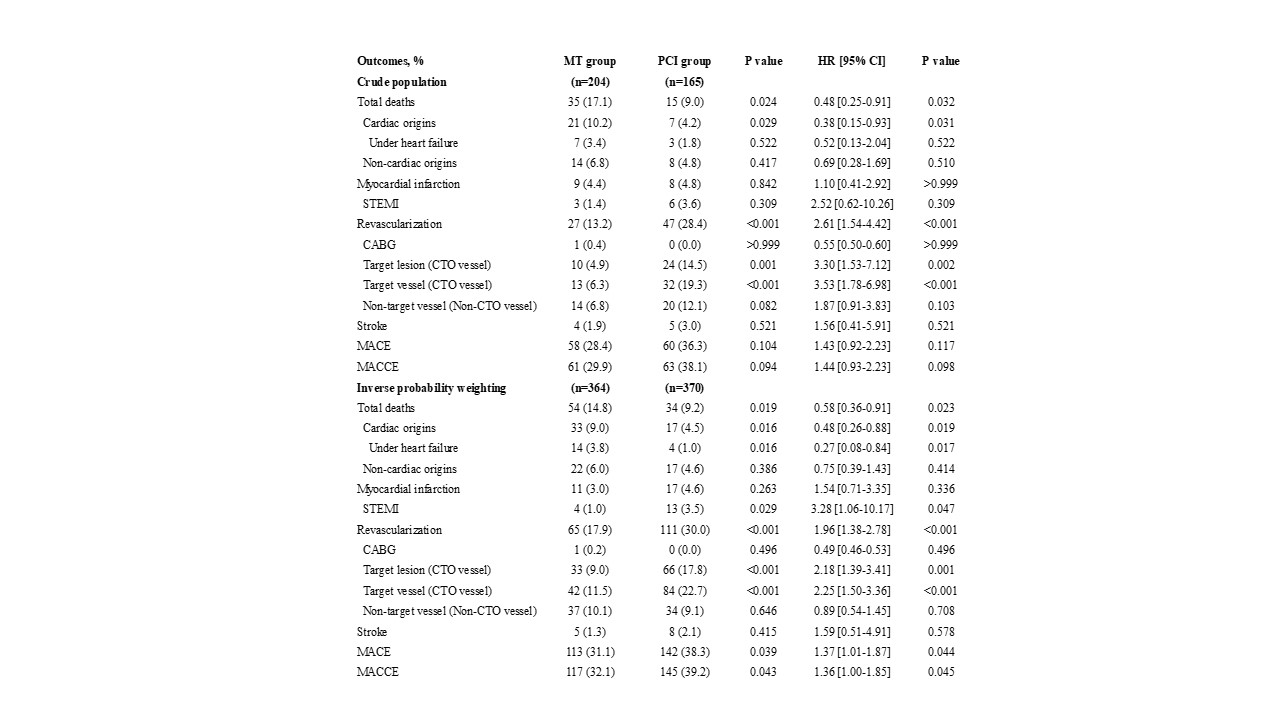
Atotal of 369 consecutive patients who were diagnosed with CTO by coronary angiographywere allocated to either the group medical treatment (MT, n = 204) group orpercutaneous coronary intervention (PCI, n = 165) according to treatmentstrategies. The 5-year clinical outcomes were compared between the two groups. Primary endpoint was a cardiac death or a targetvessel revascularization (TVR) for CTO lesion.
Results
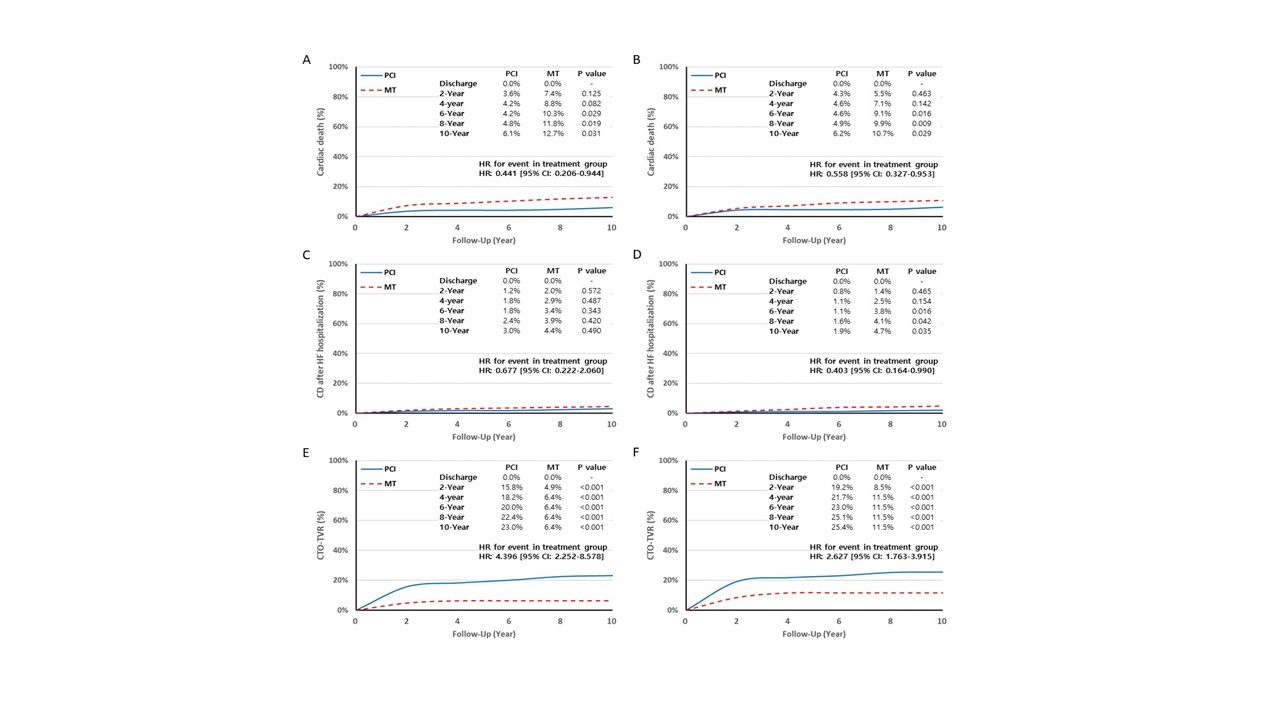
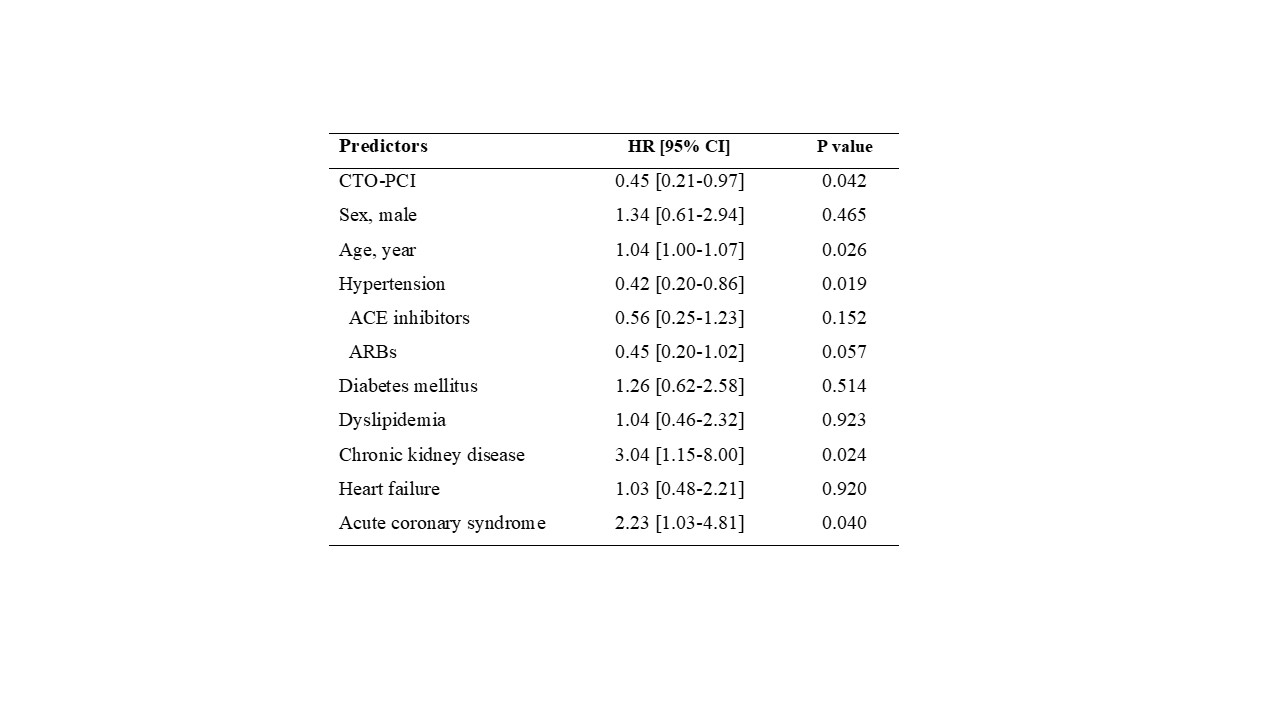
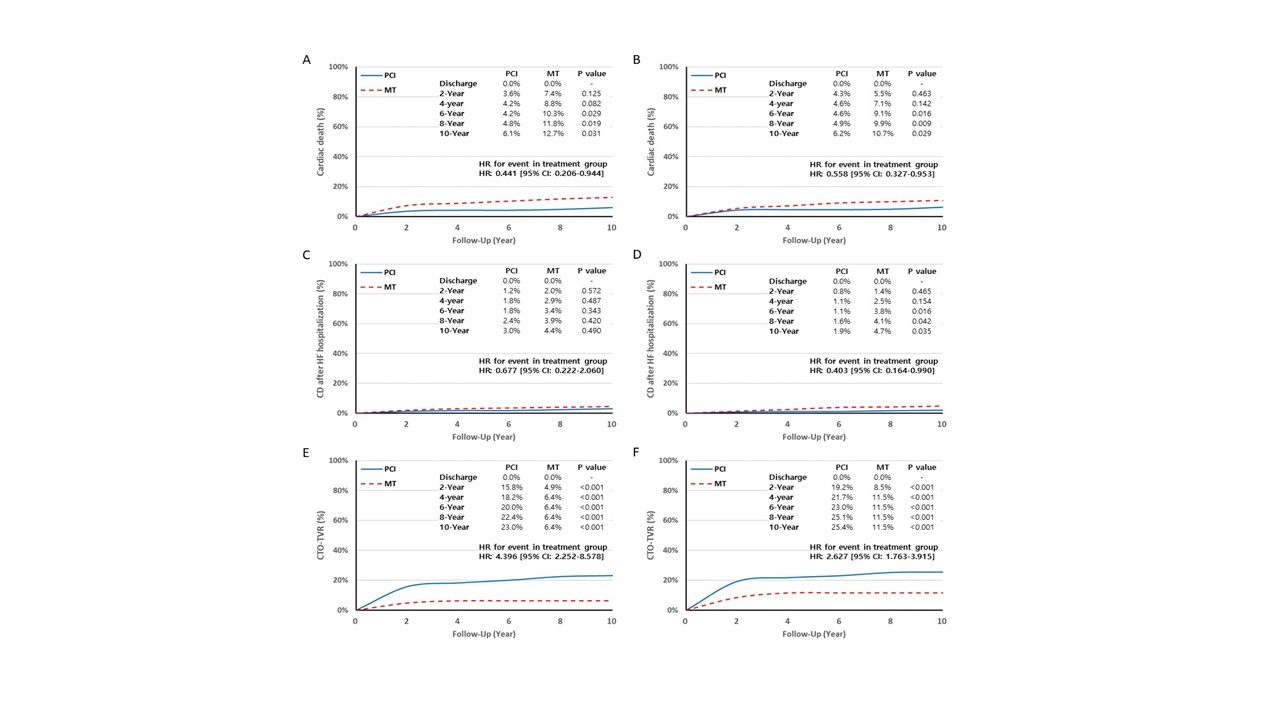
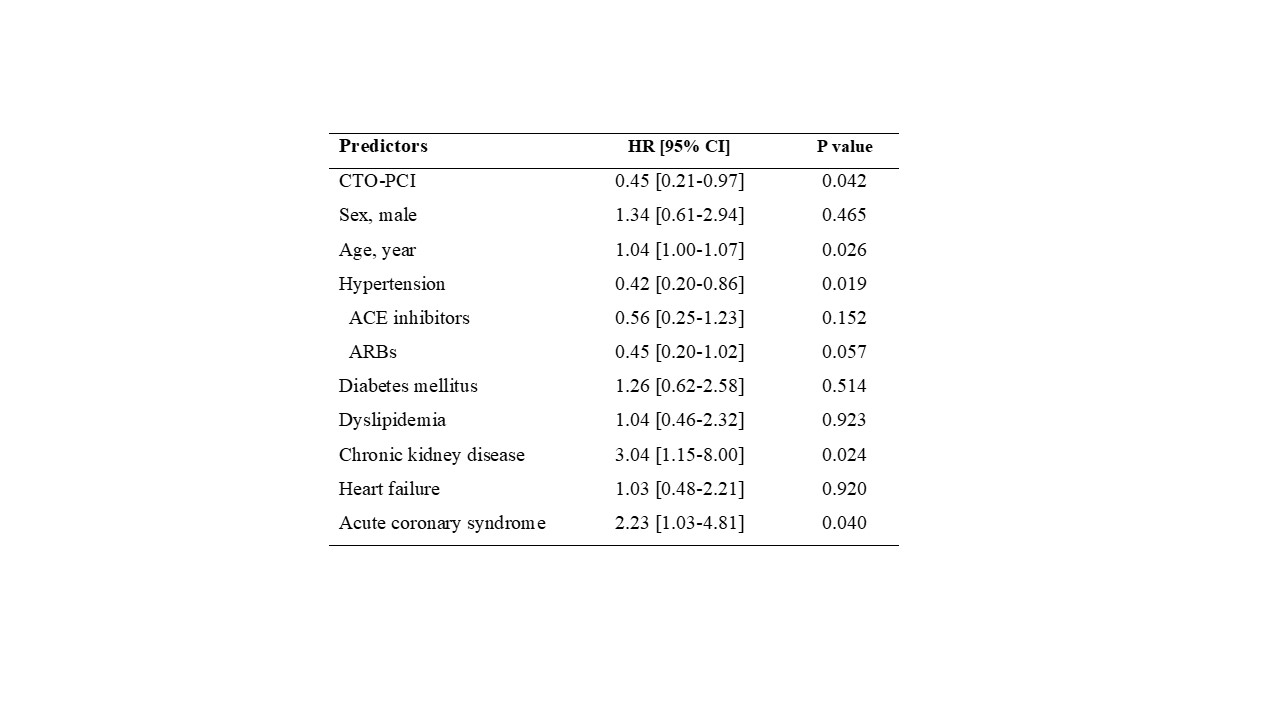
After Inverse probability weighting (IPTW)analysis, the pseudo sample size in the MT group and PCI group was 364 and 370,respectively. After a median 6.0 yearsfollow-up period (interquartile range: 5.0 to 8.1 years), the incidence ofcardiac death (9.0% vs. 4.5%, P=0.019) and cardiac death under heart failurehospitalization (3.8% vs. 1.0%, P=0.017) were higher in MT group, but the incidenceof TVR for CTO lesion was higher in PCI group (11.5%vs. 22.7%, P<0.001). Based onlogistic regression analysis, patients with CTO revascularization had survivalbenefits for cardiac death (HR: 0.558 [95% CI: 0.327-0.953] ) and cardiac deathafter heart failure hospitalization (HR: 0.403 [95% CI: 0.164-0.990] ).
Conclusion
Inour study, In patients with LV systole dysfunction (EF < 50%), successfulCTO revascularization is related to long-term survival benefits. These resultssuggest that a successful CTO revascularization is associated with a reductionin cardiac death after heart failure hospitalization.


