Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-062
Efficacy and Safety of Antiplatelet Therapy After Percutaneous Coronary Intervention Across Different Estimated Glomerular Filtration Rates
By Zhen Cheng Hwang, Kuan-Po Chiu, Donna Shu-Han Lin, Su-Kiat Chua
Presenter
Zhen Cheng Hwang
Authors
Zhen Cheng Hwang1, Kuan-Po Chiu1, Donna Shu-Han Lin1, Su-Kiat Chua1
Affiliation
Shin Kong Wu Ho-Su Memorial Hospital, Taiwan1
View Study Report
TCTAP A-062
Pharmacotherapy (Coronary)
Efficacy and Safety of Antiplatelet Therapy After Percutaneous Coronary Intervention Across Different Estimated Glomerular Filtration Rates
Zhen Cheng Hwang1, Kuan-Po Chiu1, Donna Shu-Han Lin1, Su-Kiat Chua1
Shin Kong Wu Ho-Su Memorial Hospital, Taiwan1
Background
Patients with chronic kidney disease (CKD) are at higher risks of both thrombotic and bleeding events. The aim of this study is to evaluate the efficacy and safety of different antiplatelet strategies after PCI across different estimated glomerular filtration rates (eGFR).
Methods
We searched the PubMed, EMBASE and Cochrane databases for trials which had been published since 2009.Randomized control trials that compared antiplatelet strategies (including standard dual antiplatelet therapy [DAPT], short DAPT followed by aspirin, short DAPT followed by P2Y12 inhibitors, and DAPT de-escalation) after PCI were screened and studies which reported subgroup data according to kidney function were included. Outcomes of interest included major adverse cardiovascular events (MACE, defined as a composite of cardiovascular death, nonfatal myocardial infarction, and nonfatal ischemic stroke), major or minor bleeding, and net adverse clinical events (NACE, a composite of MACE and bleeding).
Results
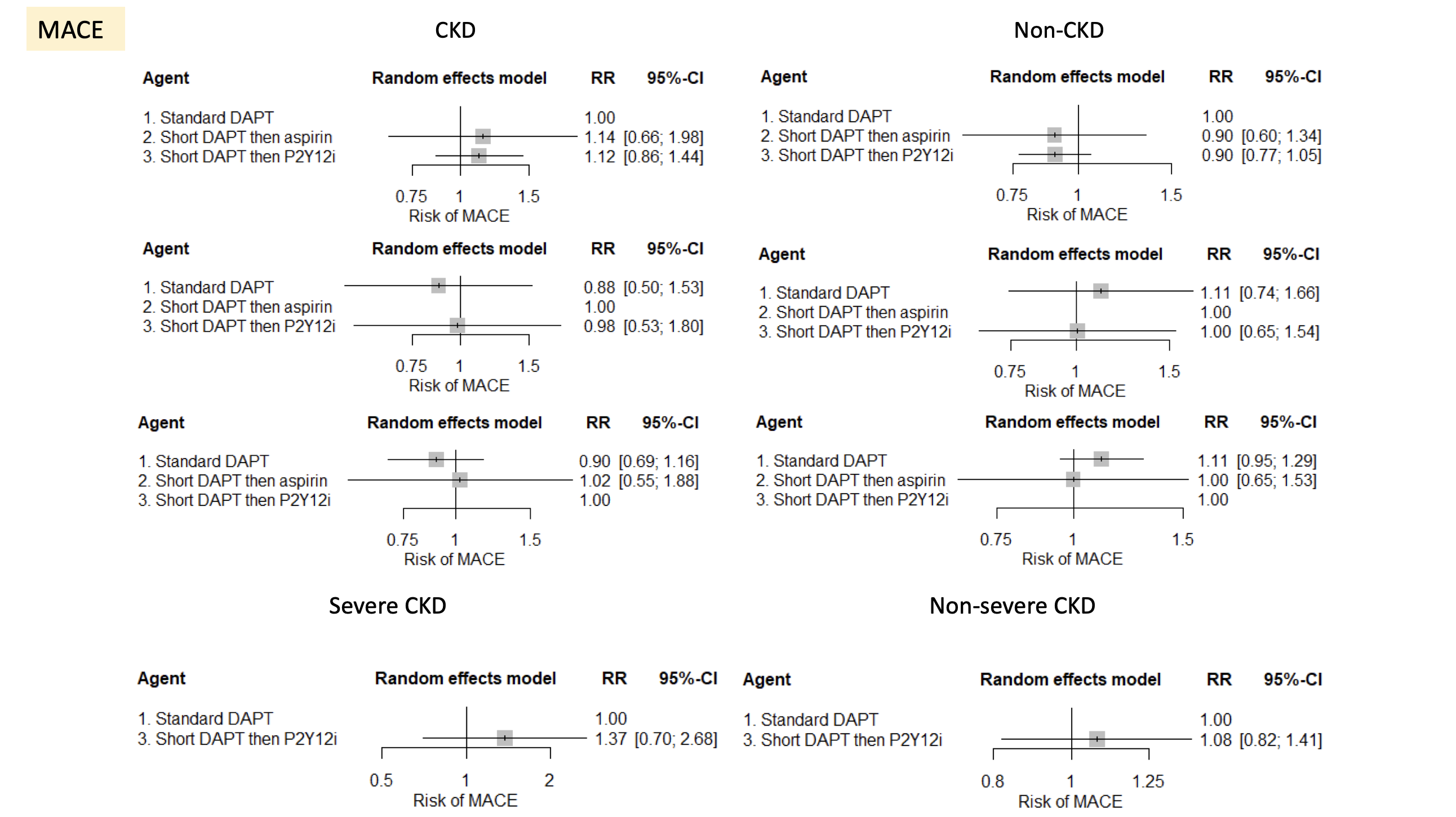
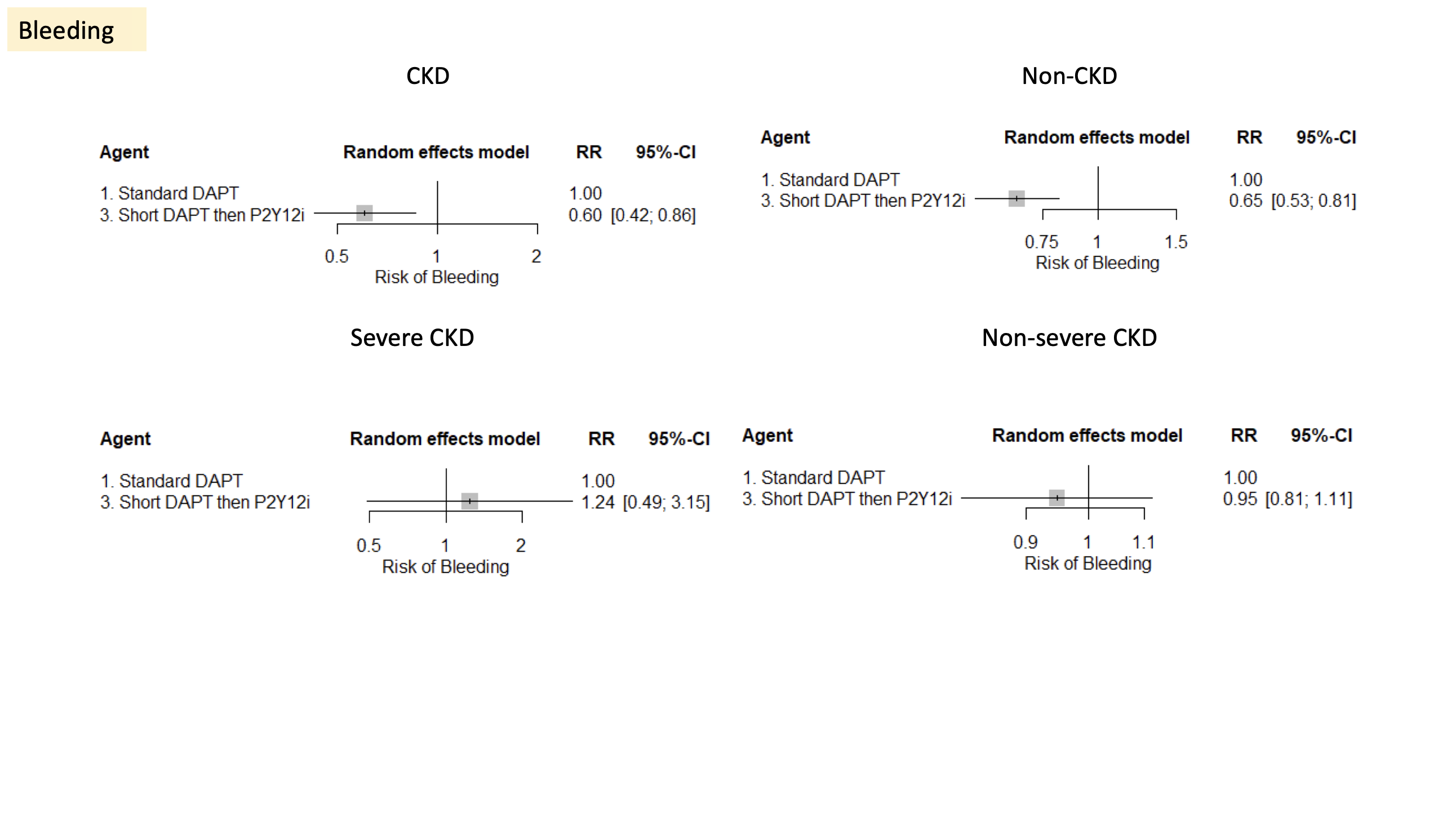
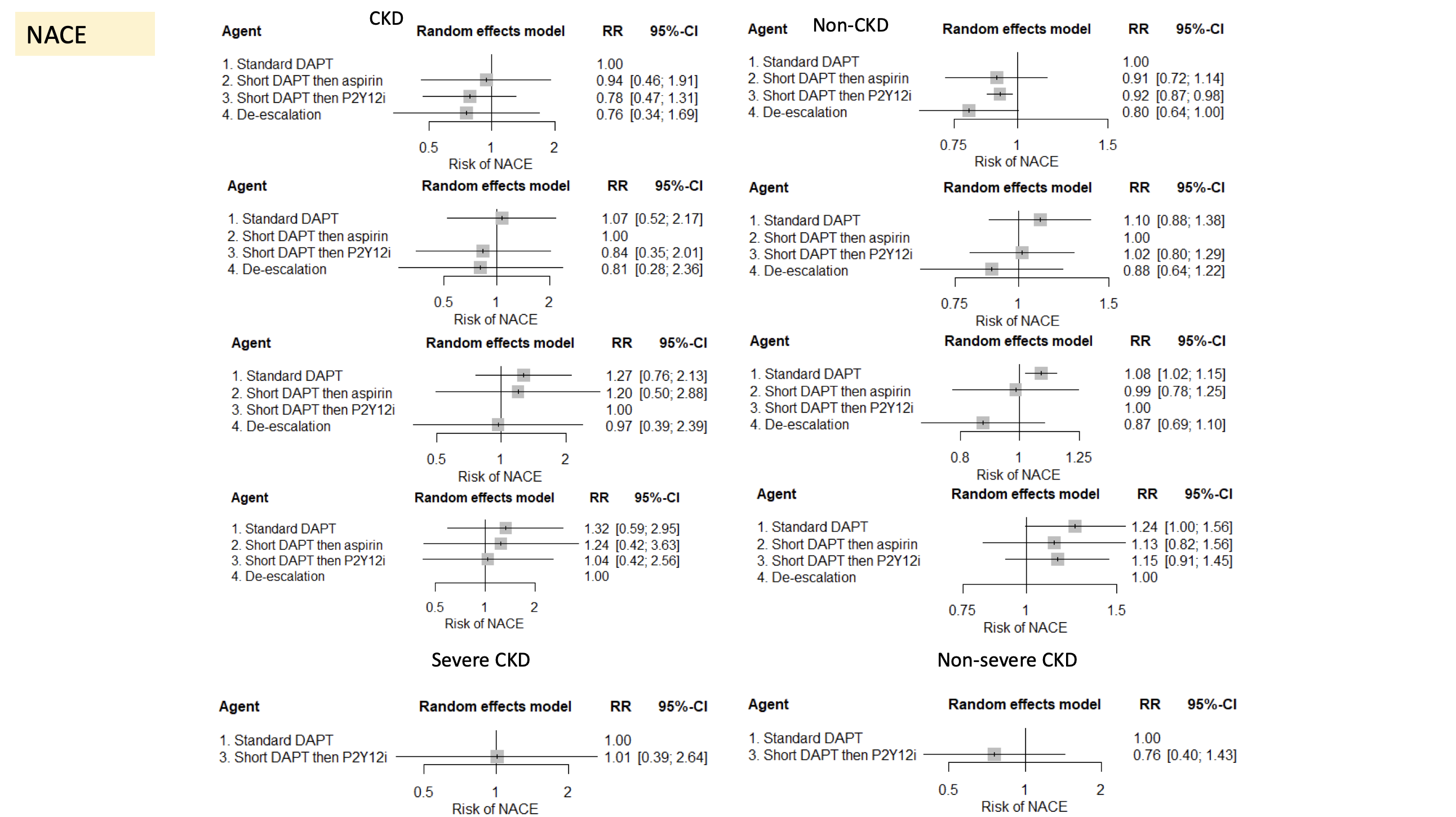
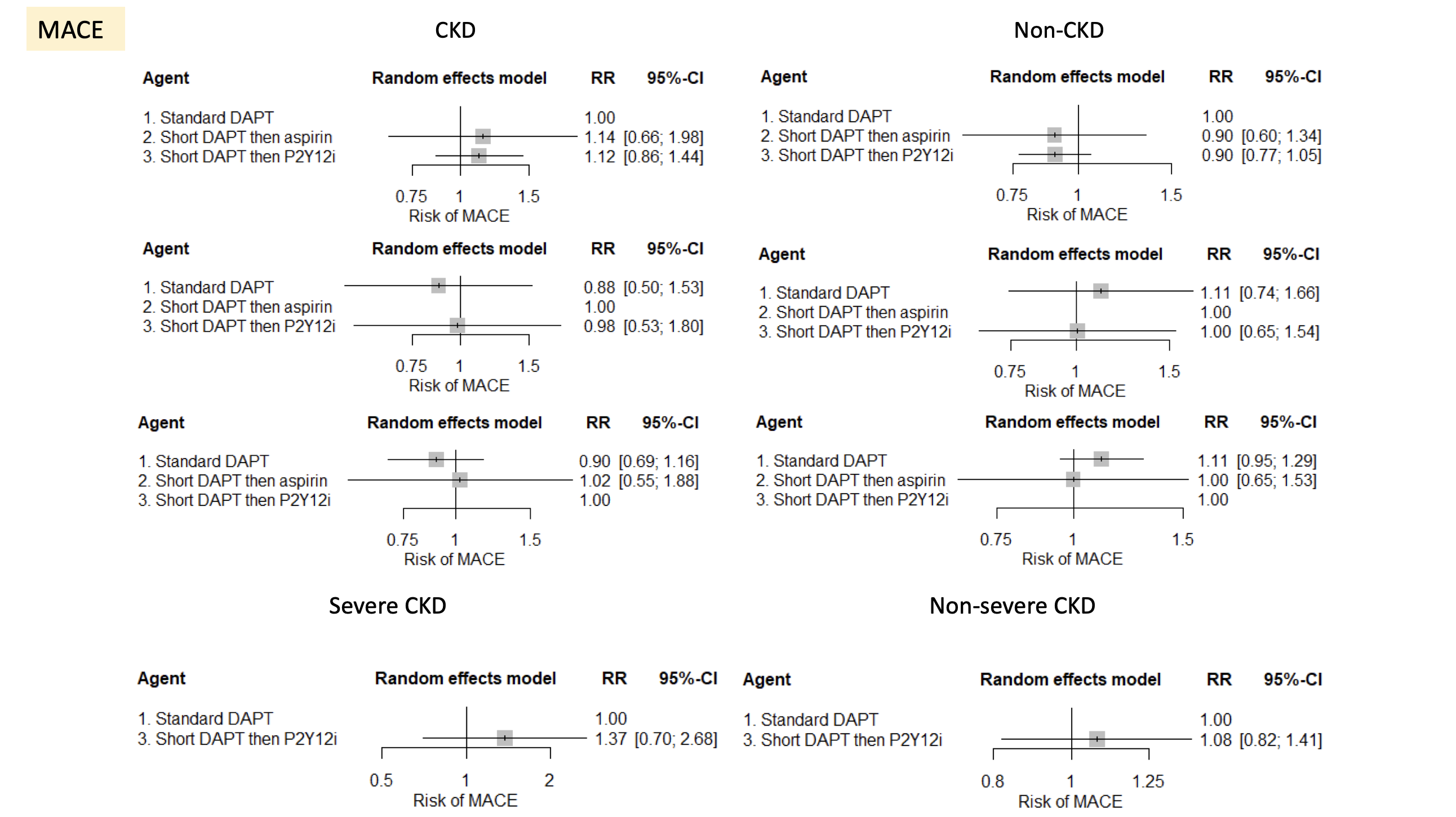
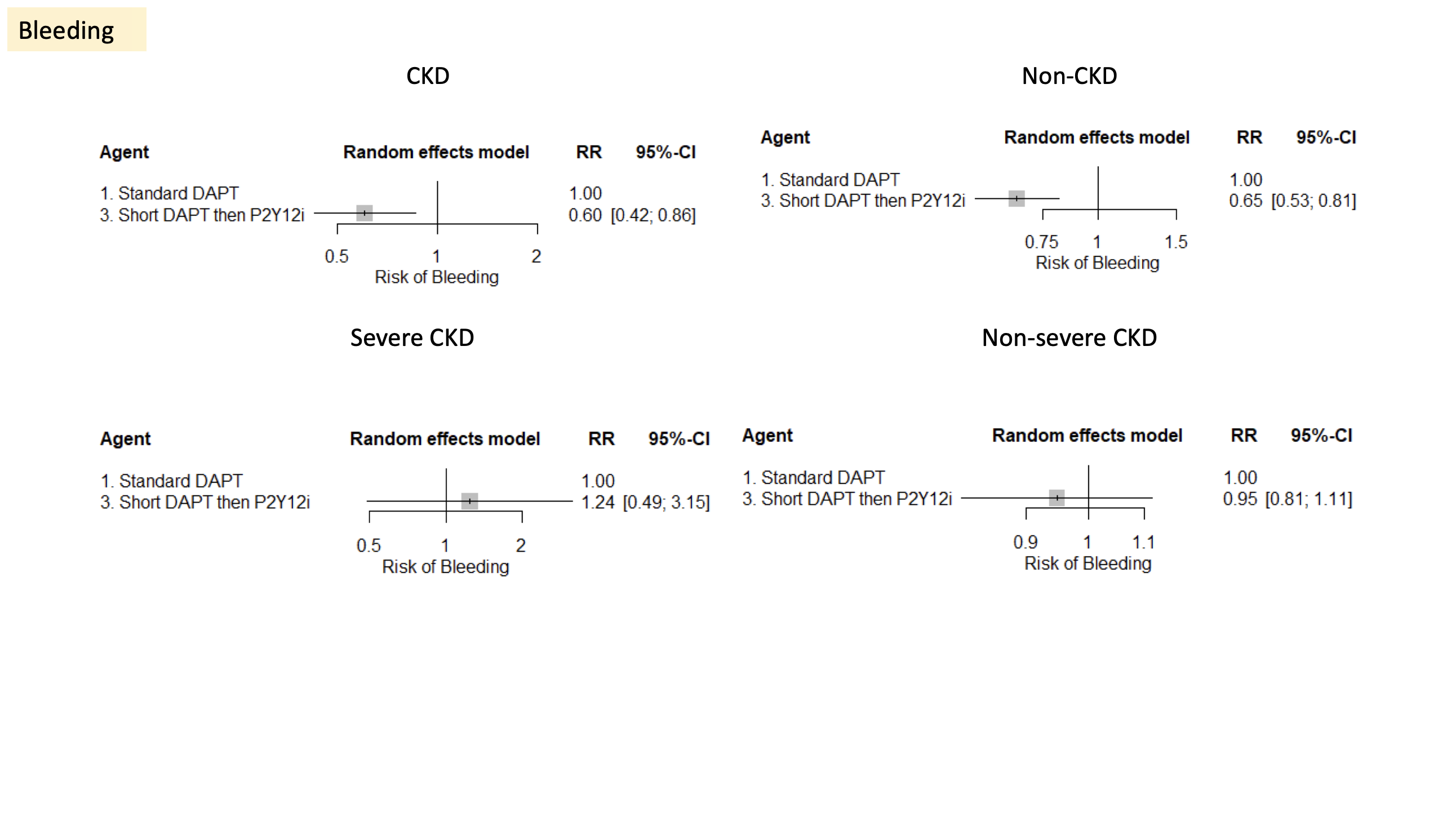
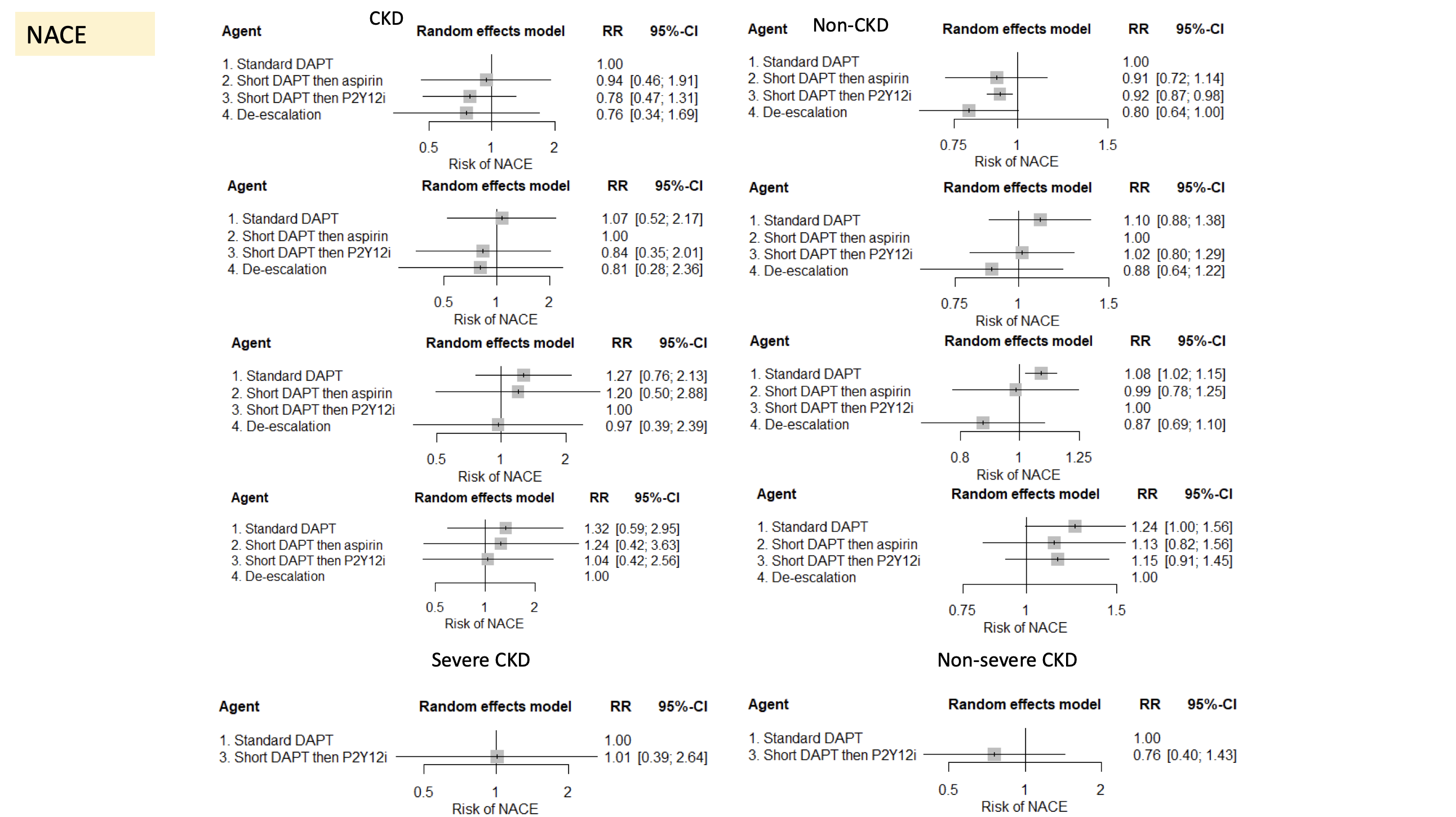
This meta-analysis included 13 randomized controlled trials with 61717 patients.Among these,7508 patients had CKD.Short DAPT strategies were associated with increased risks of MACE in patients with CKD compared to standard DAPT (short DAPT followed by aspirin: RR: 1.14; 95% CI: 0.66-1.98; short DAPT followed by P2Y12i: RR: 1.12; 95% CI: 0.86-1.44). However, this was not seen in non-CKD patients. In the non-CKD group, both short DAPT followed by aspirin (RR: 0.90; 95% CI: 0.60-1.34) and short DAPT followed by P2Y12i (RR: 0.90; 95% CI: 0.77-1.05) were associated with decreased risk of MACE compared to standard DAPT.When patients were stratified by an eGFR of 30 mL/min/1.73m2 into severe or non-severe CKD, the usage of short DAPT after PCI were both associated with numerically higher risk of MACE compared to standard DAPT. Although not reaching statistical significance, the magnitude of risk seemed greater in the severe CKD group.Bleeding risks were decreased with short DAPT followed by P2Y12i in both CKD (RR: 0.6; 95% CI: 0.42-0.86), non-CKD group (RR: 0.65; 95% CI: 0.53-0.81) compared to standard DAPT, with the magnitude of risk accentuated in the CKD group. However, in patients with severe CKD, short DAPT strategies were associated with increased risks of bleeding compared to standard DAPT.In both CKD patients, short DAPT followed by P2Y12i (RR: 0.78; 95% CI: 0.47-1.31) and DAPT de-escalation (RR: 0.76; 95% CI: 0.34-1.69) were both associated with lower risks of NACE compared to standard DAPT. The benefits of short DAPT followed by aspirin seemed marginal. The reduction of NACE associated with short DAPT followed by P2Y12i use and DAPT de-escalation in patient without CKD seemed smaller in magnitude compared to those with CKD. However, in the subset of patients with severe CKD, there were no differences in terms of NACE compared to standard DAPT (RR: 1.01; 95% CI: 0.39-2.64).
Conclusion
Short DAPT therapy followed by either aspirin or P2Y12i has shown limited efficacy in patient with CKD after PCI. However, it demonstrates promising bleeding safety, particularly in patients with less severe CKD. For patients with severe CKD, careful consideration is needed. Overall, alternative DAPT strategies should be tailored individually based on the patient's kidney function.


