Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-046
Poor Cardiac Function Plays a Key Role in Cholesterol Paradox in Patients With Acute Myocardial Infarction: A Large-Scale Multi-Center Cohort Study
By Jiawen Li, Menglu Liu, Kailun Yan, Kexin Zhang, Jinqing Yuan, Xueyan Zhao
Presenter
Jiawen Li
Authors
Jiawen Li1, Menglu Liu1, Kailun Yan1, Kexin Zhang1, Jinqing Yuan1, Xueyan Zhao1
Affiliation
Fuwai Hospital, China1
View Study Report
TCTAP A-046
ACS/AMI
Poor Cardiac Function Plays a Key Role in Cholesterol Paradox in Patients With Acute Myocardial Infarction: A Large-Scale Multi-Center Cohort Study
Jiawen Li1, Menglu Liu1, Kailun Yan1, Kexin Zhang1, Jinqing Yuan1, Xueyan Zhao1
Fuwai Hospital, China1
Background
Recent studies have revealed a phenomenon known as the "cholesterol paradox", wherein low low-density lipoprotein cholesterol (LDL-C) levels are associated with adverse outcomes, but the underlying mechanisms are not fully understood. This study aimed to explore the effect of cardiac function on this paradox in acute myocardial infarction (AMI) patients.
Methods
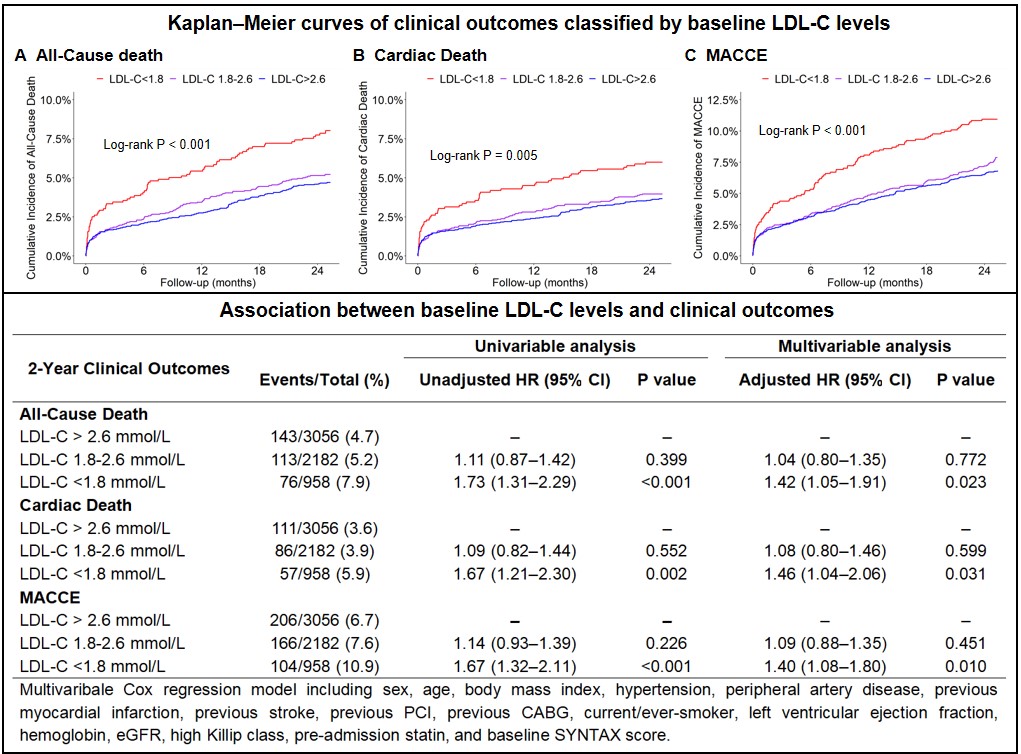
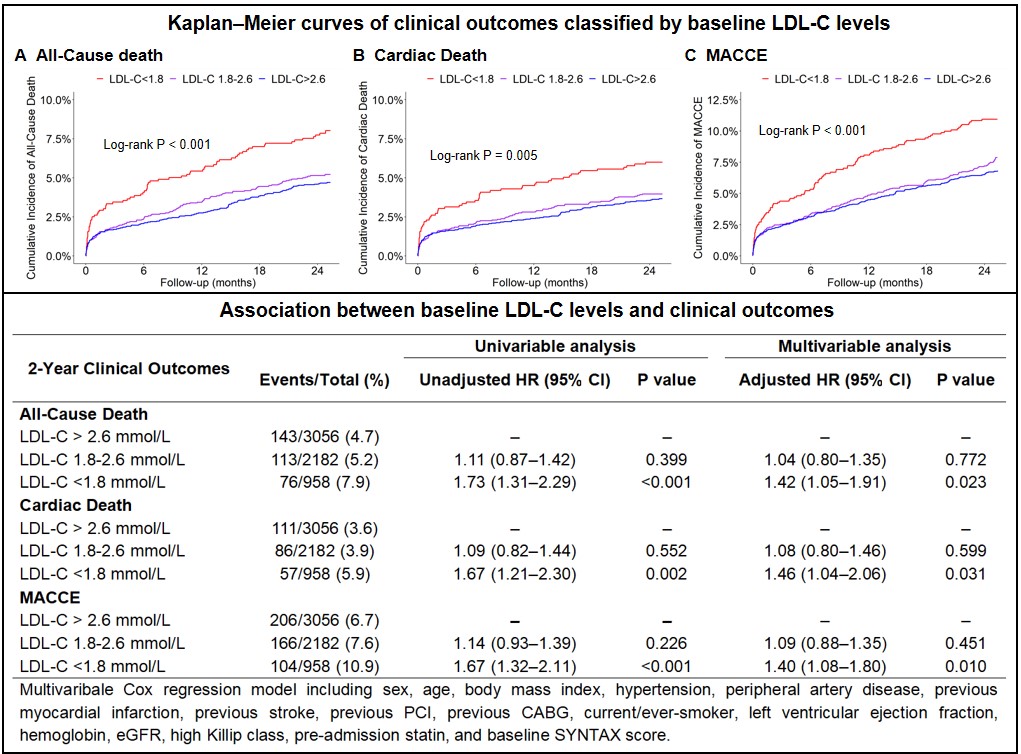
Of 18701 patients enrolled in a multi-center cohort of coronary artery disease from January 2015 to May 2019, we identified 6196 AMI patients with complete baseline data and a 2-year follow-up. The primary outcome was all-cause death. Secondary outcomes were cardiac death and major adverse cardiac and cerebrovascular events (MACCE).
Results
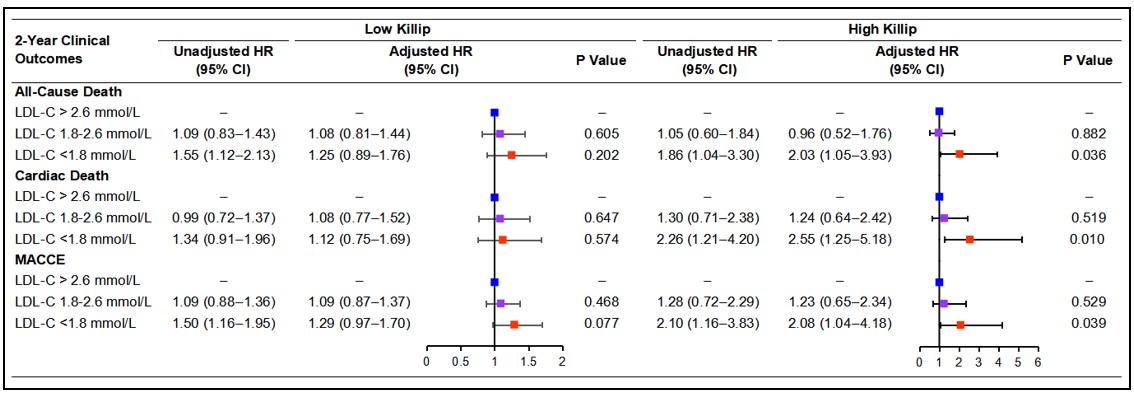
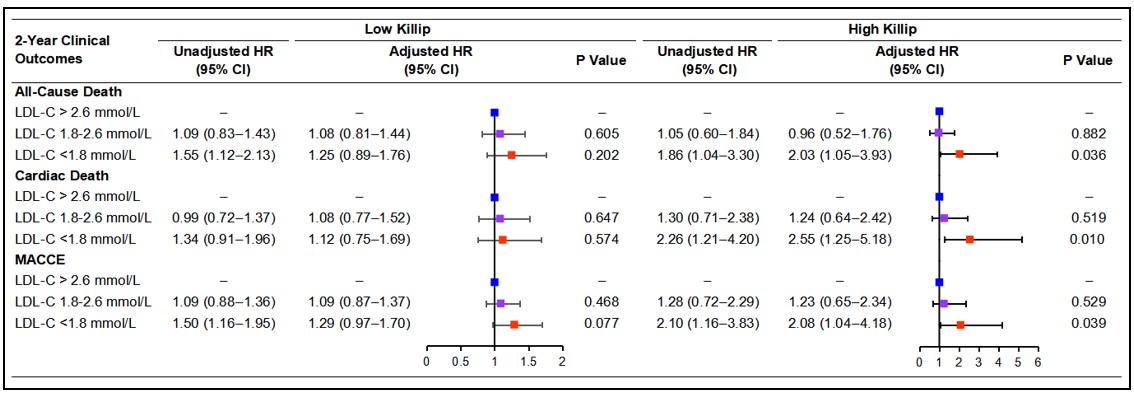
Over a median follow-up of 2.1 years, 324 (5.2%) all-cause deaths, 254 (4.1%) cardiac deaths, and 476 (7.7%) MACCE occurred. Multivariable Cox analysis demonstrated that low baseline LDL-C levels (< 1.8 mmol/L) were independently associated with increased risks of all-cause death (HR: 1.42, 95% CI 1.05–1.91), cardiac death (HR: 1.46, 95% CI 1.04–2.06) and MACCE (HR: 1.40, 95% CI 1.08–1.80) relative to LDL-C > 2.6 mmol/L in patients with AMI. However, stratification by Killip classifications revealed that the increased risks associated with low LDL-C levels were significantly only in patients with high-Killip (Ⅲ-Ⅳ), but not in those with low-Killip (Ⅰ-Ⅱ).
Conclusion
We first reported low baseline LDL-C levels in AMI patients significantly increased long-term cardiovascular events, mainly attribute to poor cardiac function. This may partly explain the LDL-C paradox in patients with acute myocardial infarction.


