Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-008
Mid-Term Outcomes of Drug-Coated Balloon Use for Acute Coronary Syndrome
By Nao Yasuda, Takuma Tsuda
Presenter
Nao Yasuda
Authors
Nao Yasuda1, Takuma Tsuda1
Affiliation
Nagoya Ekisaikai Hospital, Japan1
View Study Report
TCTAP A-008
ACS/AMI
Mid-Term Outcomes of Drug-Coated Balloon Use for Acute Coronary Syndrome
Nao Yasuda1, Takuma Tsuda1
Nagoya Ekisaikai Hospital, Japan1
Background
The application of drug-coated balloon (DCB) therapy in percutaneous coronary intervention (PCI) for de novo lesions has been widely reported. However, the efficacy and safety of DCB therapy in lesions associated with acute coronary syndrome (ACS) remain unclear. Recently, the Clinical Expert Consensus Document (CECD) from the Japanese Association of Cardiovascular Intervention and Therapeutics (CVIT) introduced criteria for the appropriate use of DCBs, garnering attention. The purpose of this study was to evaluate the outcomes of DCB treatment for ACS using the CECD strategy.
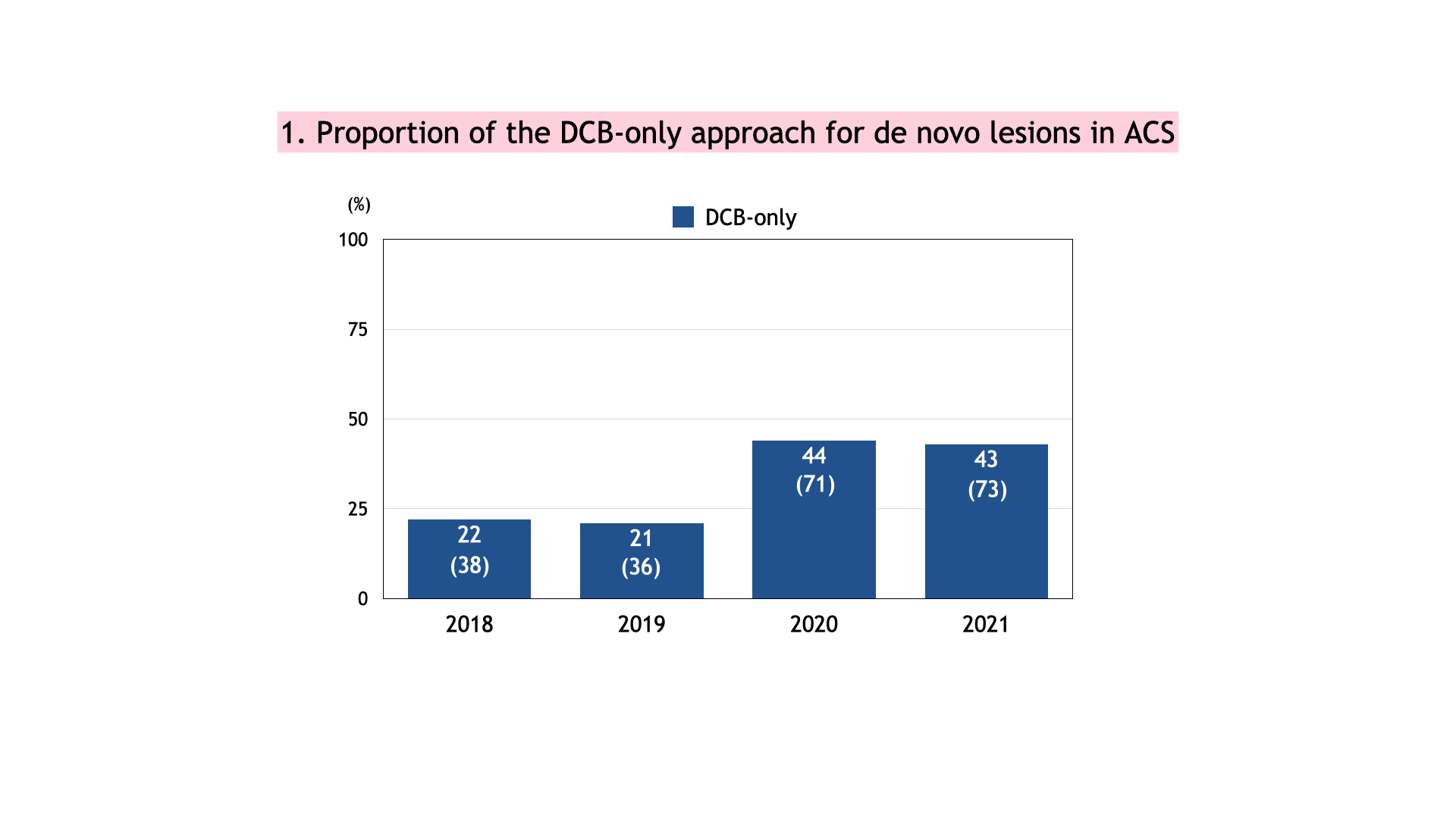
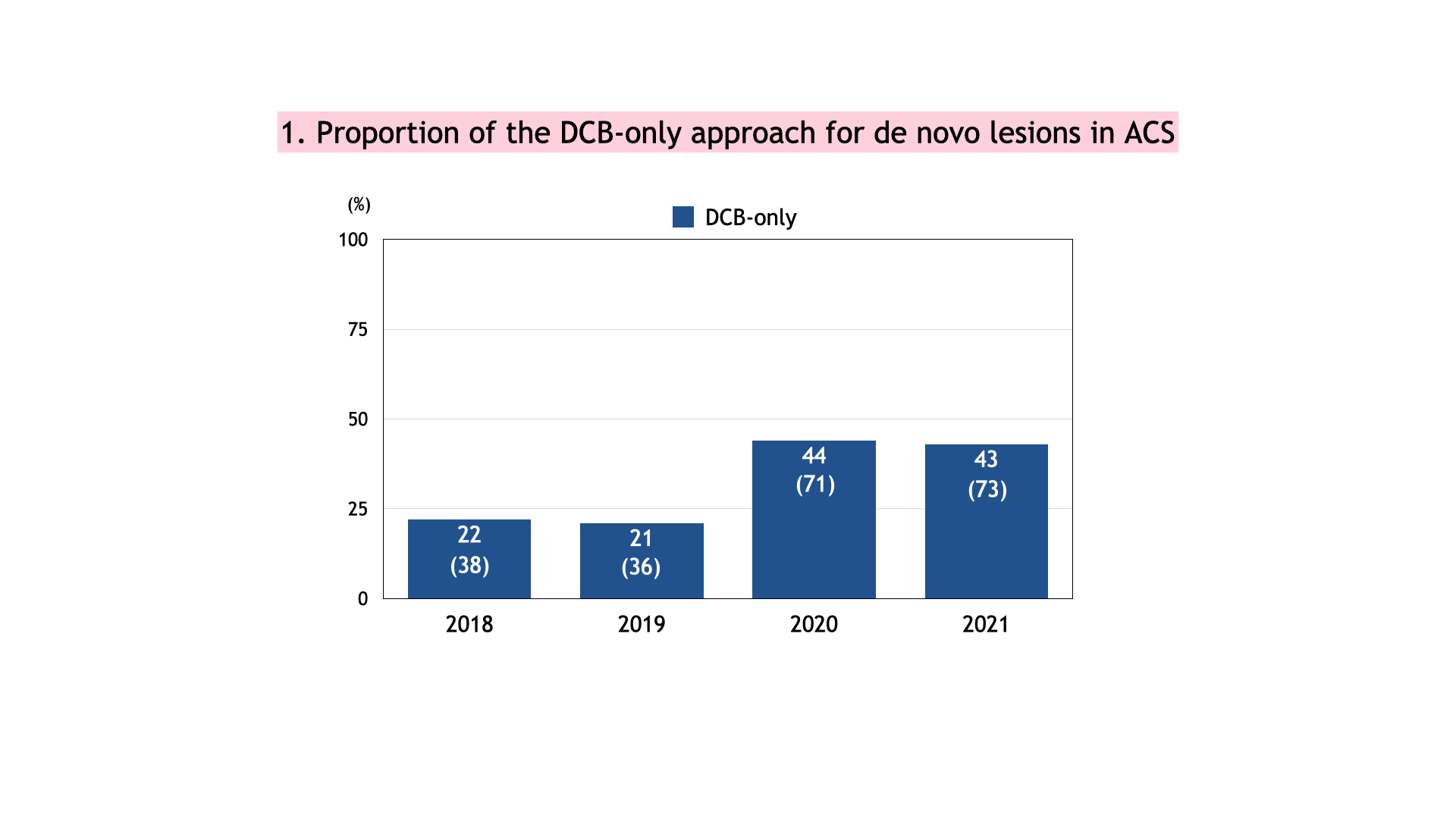
Methods
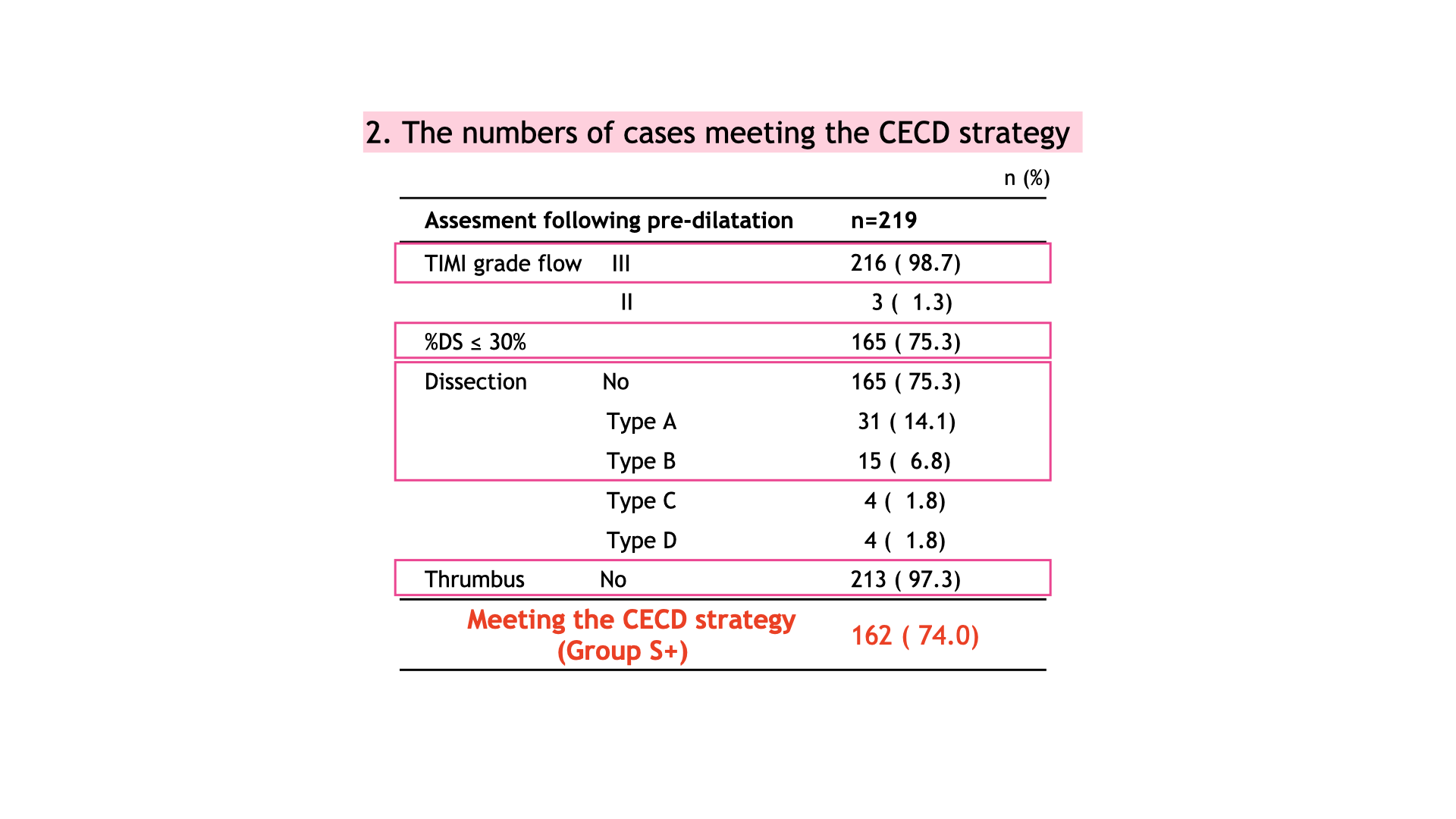
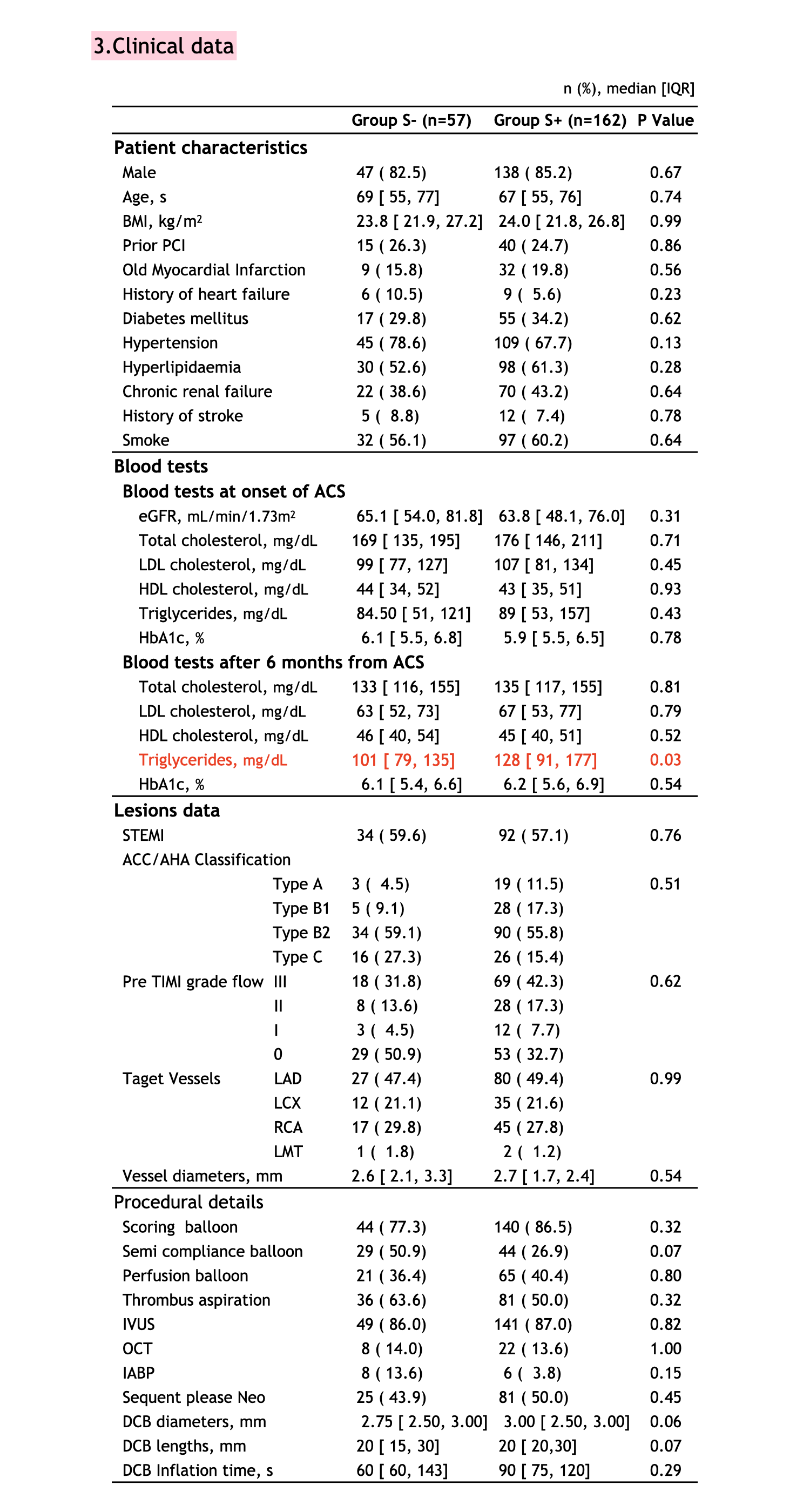
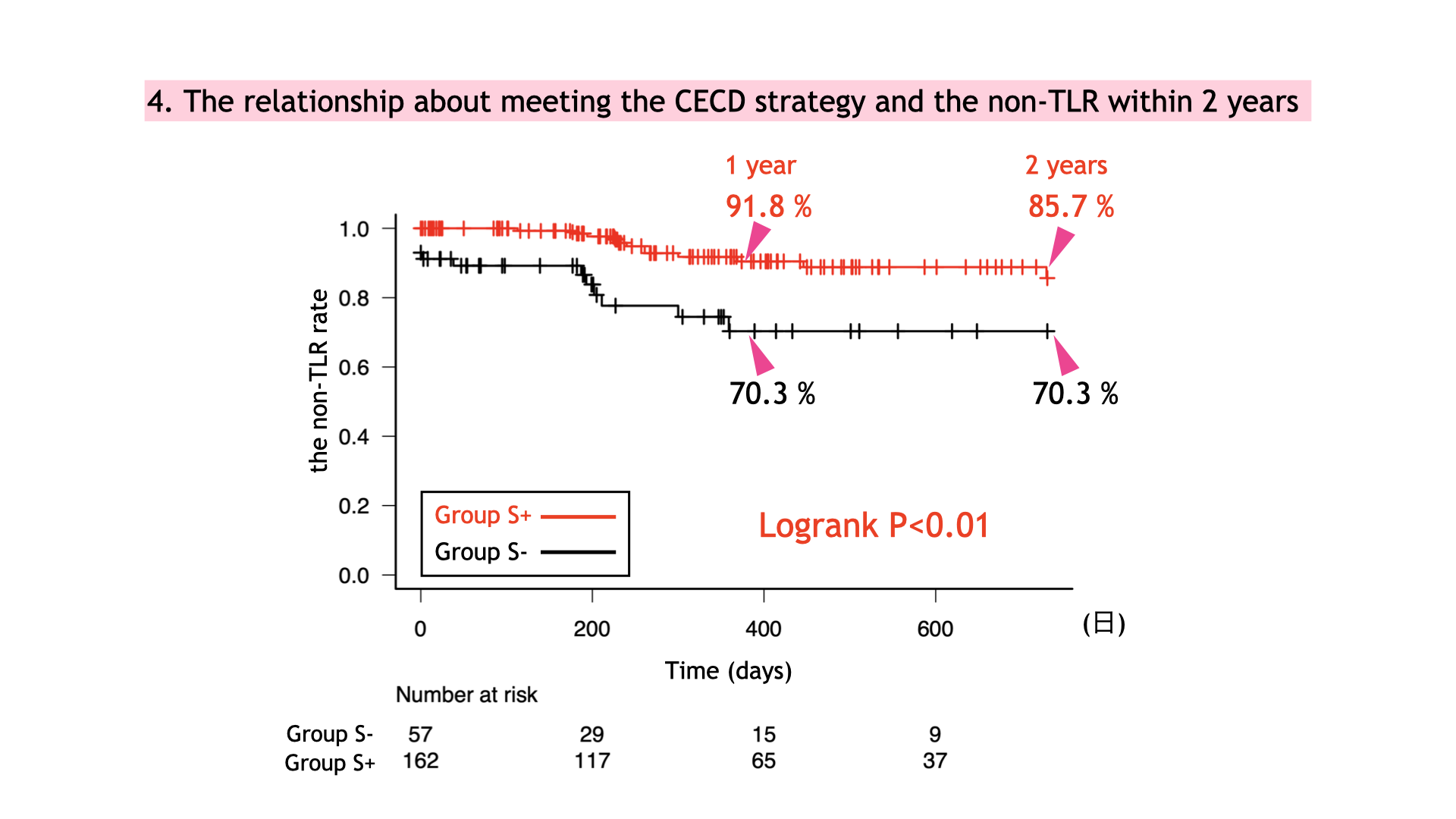
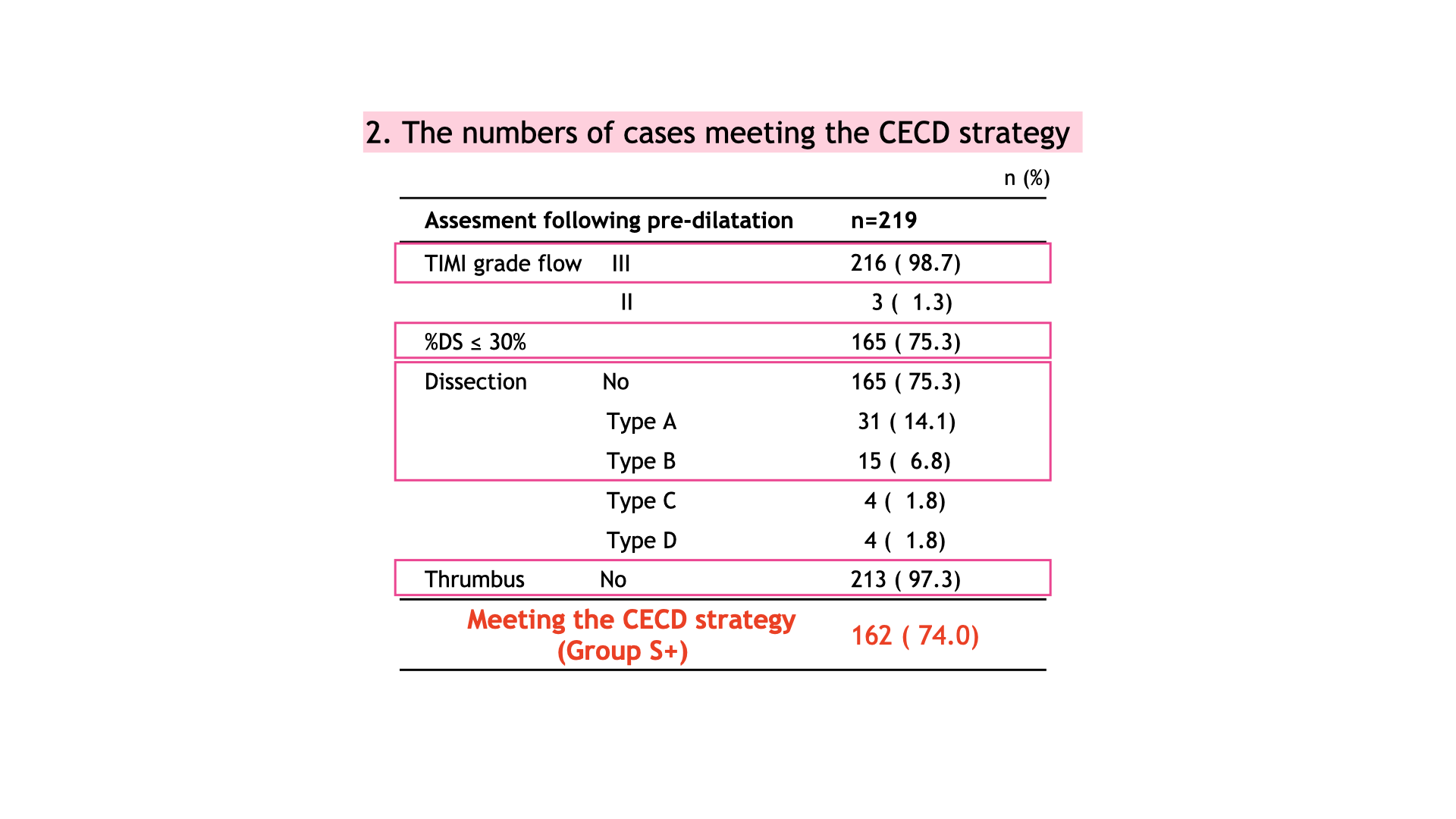
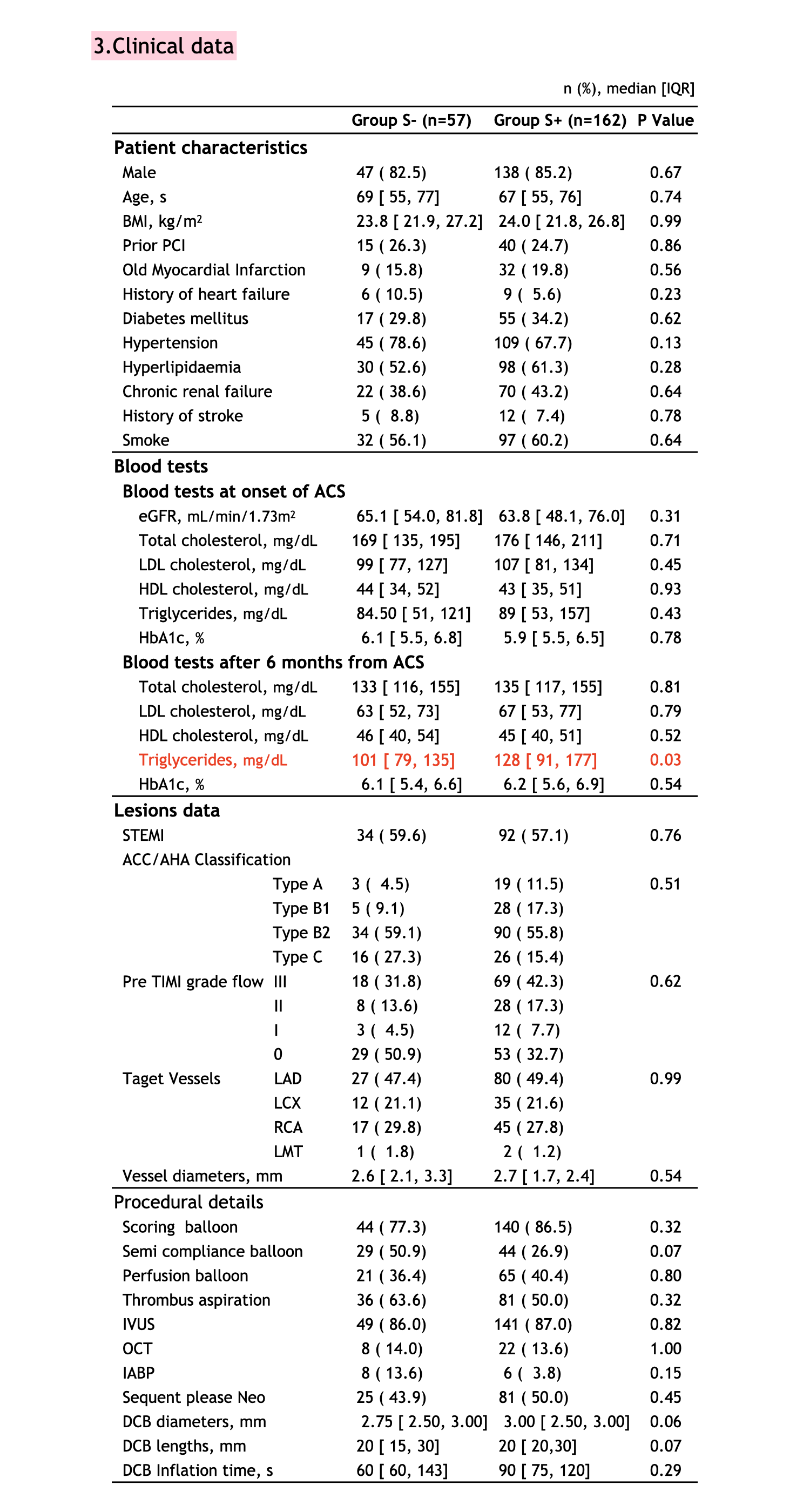
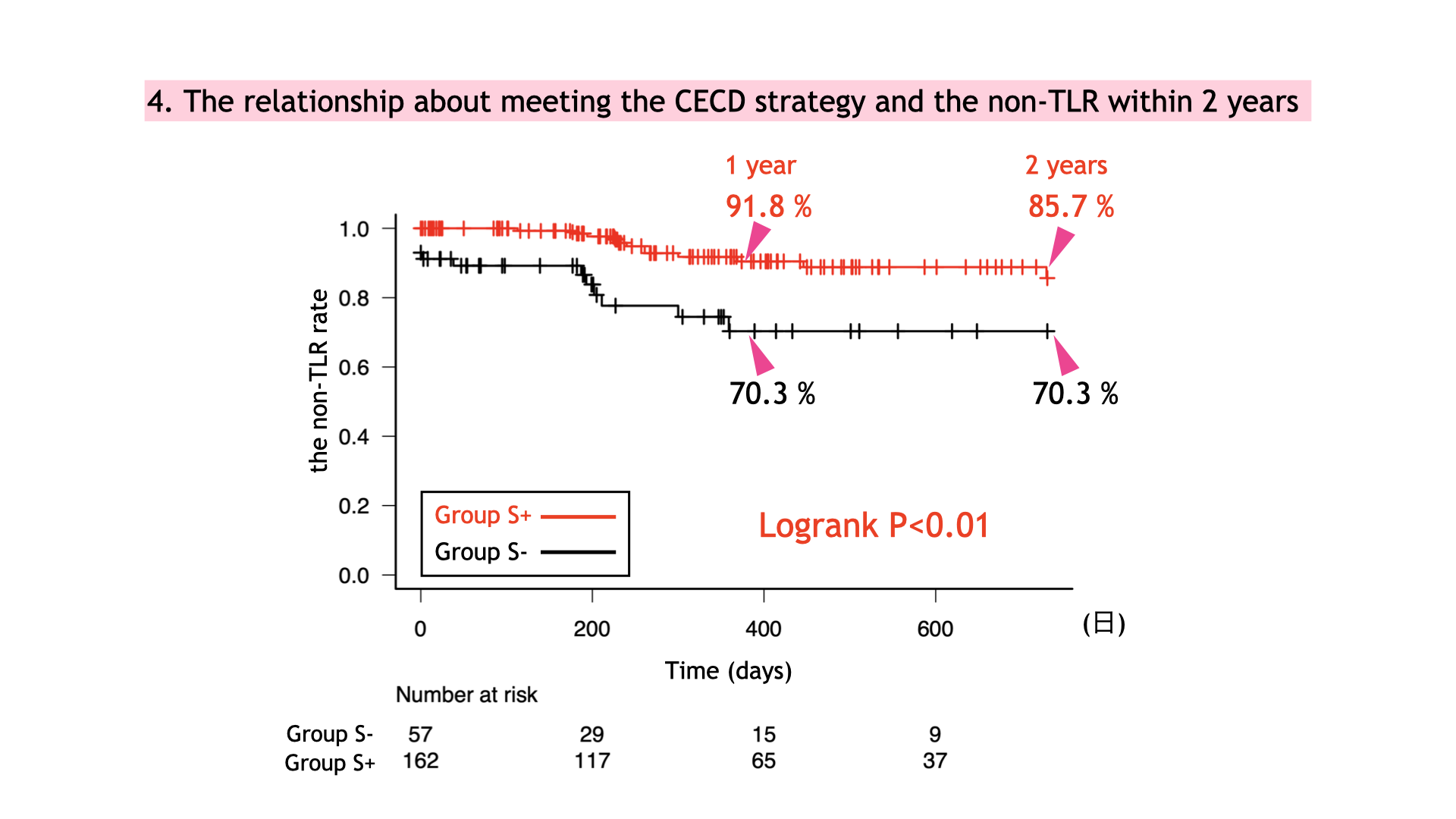
This retrospective study included 219 patients who underwent DCB therapy for de novo lesions in ACS as part of primary PCI at our hospital from April 2018 to March 2022. Based on lesion condition following pre-dilation, patients were divided into two groups: those meeting the criteria of the CECD strategy (TIMI grade 3 flow, residual stenosis ≤ 30% on angiography, absence of major dissection [types C-F on angiography, or medial involvement or hematoma on IVUS/OCT], and absence of thrombus) as the S+ group, and those not meeting these criteria as the S- group. Clinical data and target lesion revascularization (TLR) within two years were evaluated over a mean follow-up period of 340 ± 242 days.
Results
The S+ group comprised 162 cases, while the S- group included 57 cases. No significant differences were observed between the groups in terms of patient demographics, target vessels, vessel diameters, procedural details, or DCB sizes. The incidence of TLR within two years was higher in the S- group, with the non-TLR rate within two years being 85.6% in the S+ group and 72.8% in the S- group (log-rank p=0.002). Notably, in the S- group, there were four cases of acute occlusion within 24 hours and one case of occlusion within two days, whereas there were no instances of acute occlusion in the S+ group.
Conclusion
DCB therapy for ACS demonstrated favorable mid-term outcomes when performed in accordance with the CECD strategy from CVIT. However, cases not adhering to the CECD strategy showed higher rates of restenosis, underscoring the importance of optimizing case selection for the use of DCB in ACS management.


