Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-021
The Antiplatelet Therapy in Chinese Post Stenting Patients With High Bleeding Risk Patients With Acute Coronary Syndrome: Insights From BRIC Study
By Dandan Li, Yang Zheng, Hui Chen, Juying Qian, Qin Qin, Chunlin Yin, Jiyan Chen, Chengxing Shen, Yundai Chen
Presenter
Dandan Li
Authors
Dandan Li1, Yang Zheng2, Hui Chen3, Juying Qian4, Qin Qin5, Chunlin Yin6, Jiyan Chen7, Chengxing Shen8, Yundai Chen1
Affiliation
The Sixth Medical Center of Chinese PLA General Hospital, China1, The First Hospital of Jilin University, China2, Beijing Friendship Hospital, China3, Zhongshan Hospital, China4, Tianjin Chest Hospital, China5, Xuanwu Hospital, China6, Guangdong General Hospital, China7, Shanghai Sixth People’s Hospital, China8
View Study Report
TCTAP A-021
Clinical Trials & Science
The Antiplatelet Therapy in Chinese Post Stenting Patients With High Bleeding Risk Patients With Acute Coronary Syndrome: Insights From BRIC Study
Dandan Li1, Yang Zheng2, Hui Chen3, Juying Qian4, Qin Qin5, Chunlin Yin6, Jiyan Chen7, Chengxing Shen8, Yundai Chen1
The Sixth Medical Center of Chinese PLA General Hospital, China1, The First Hospital of Jilin University, China2, Beijing Friendship Hospital, China3, Zhongshan Hospital, China4, Tianjin Chest Hospital, China5, Xuanwu Hospital, China6, Guangdong General Hospital, China7, Shanghai Sixth People’s Hospital, China8
Background
The prospective BRIC study revealed the incidence of postdischarge bleeding (PDB) (post)cardiovascular events in Chinese acute coronary syndromes (ACS) patients with real-world. To evaluate the optimal dual antiplatelet therapy (DAPT) in ACS patients with high bleeding risk (HBR), we performed an explorative analysis of BRIC study.
Methods
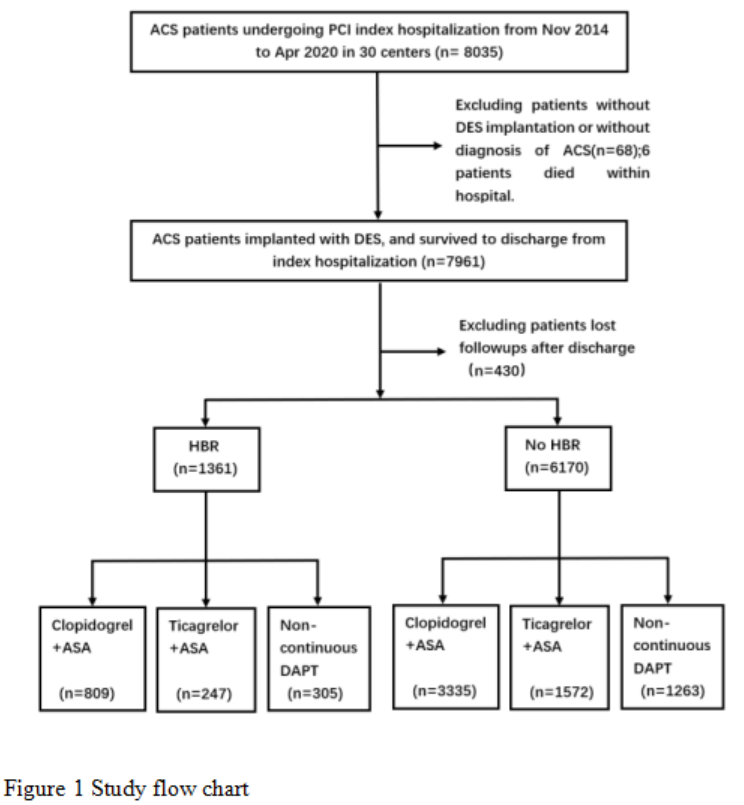
A total of 7531 ACS patients treated with PCI and followed up for 1-year in 30 Chinese hospitals from May 2014 to January 2016 and October 2017 to April 2019 were enrolled, of which 1361(18%)were with HBR.
Results
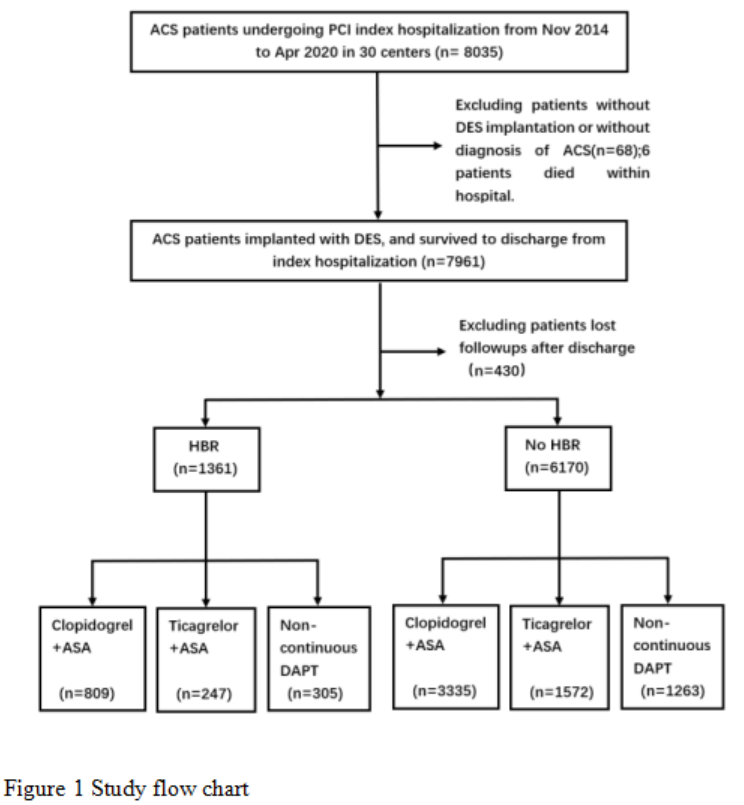
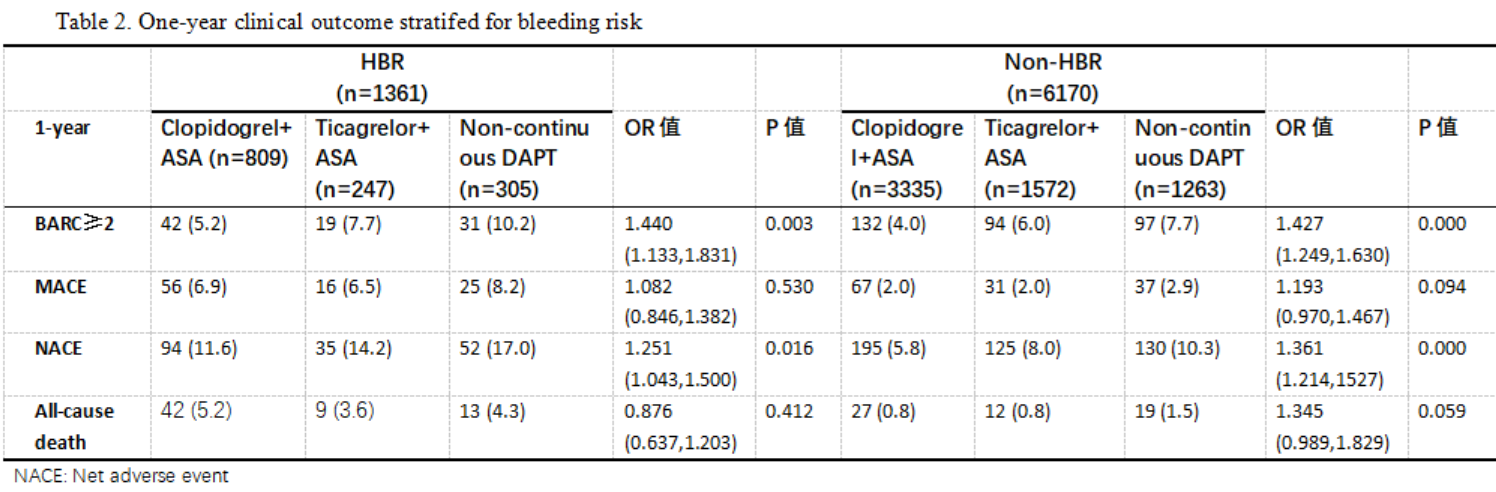
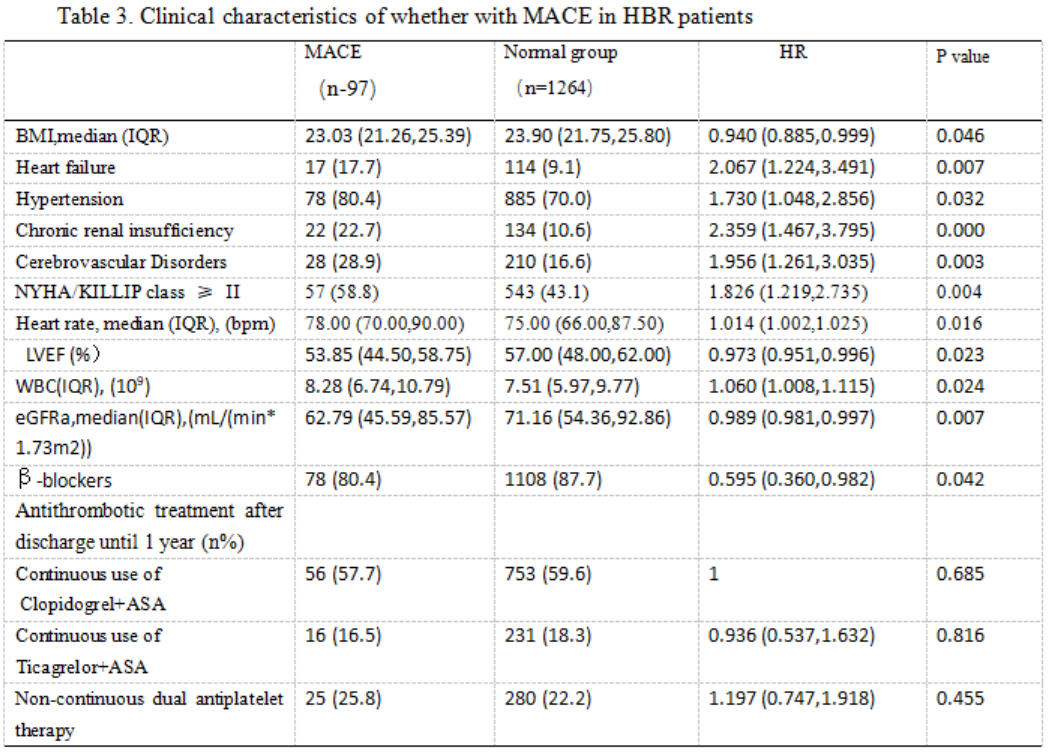
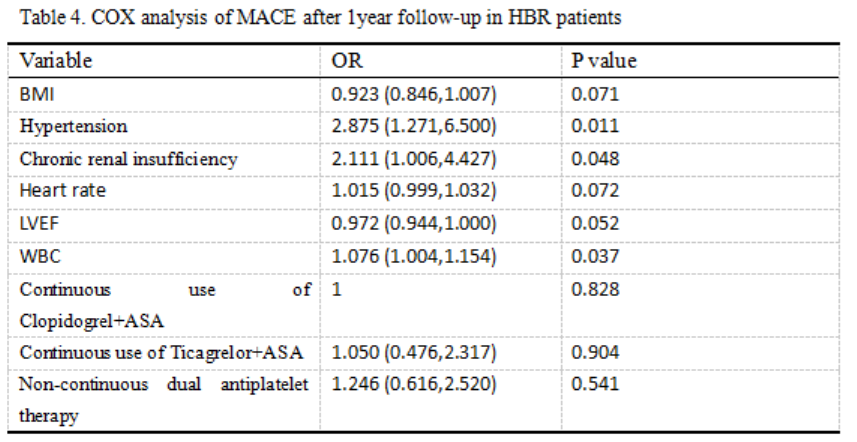
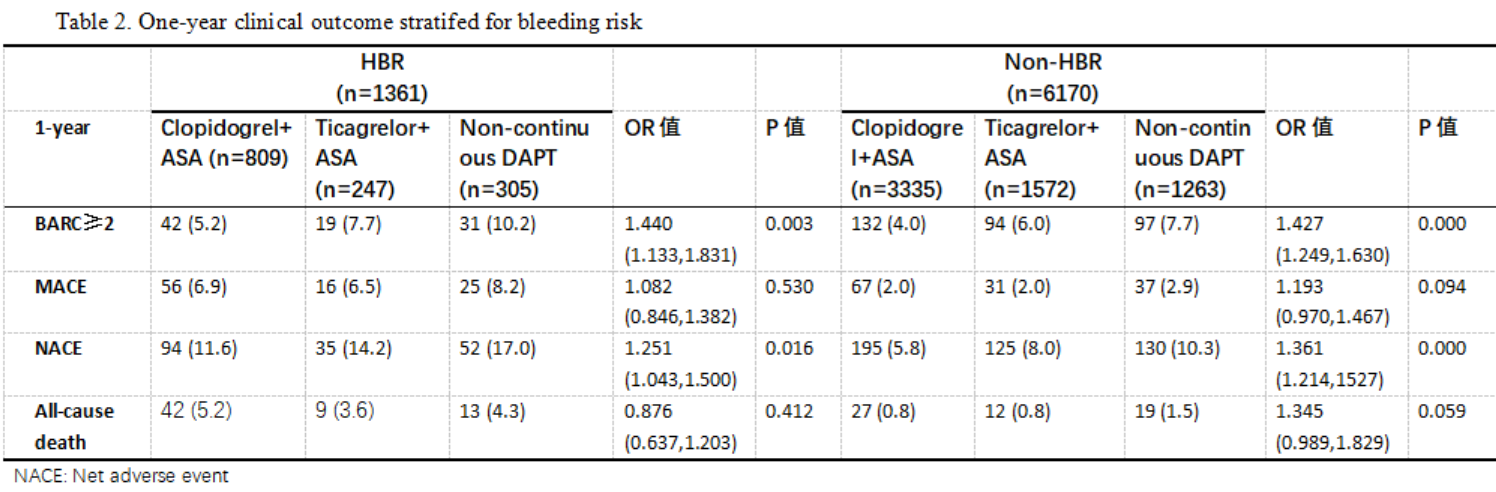
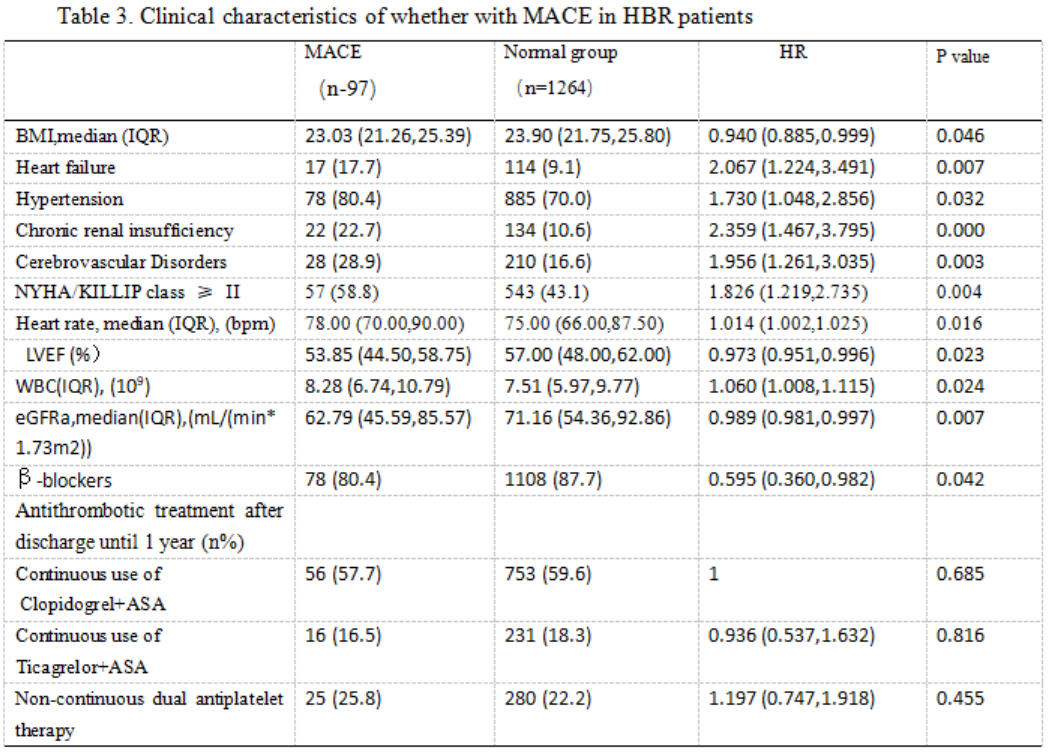
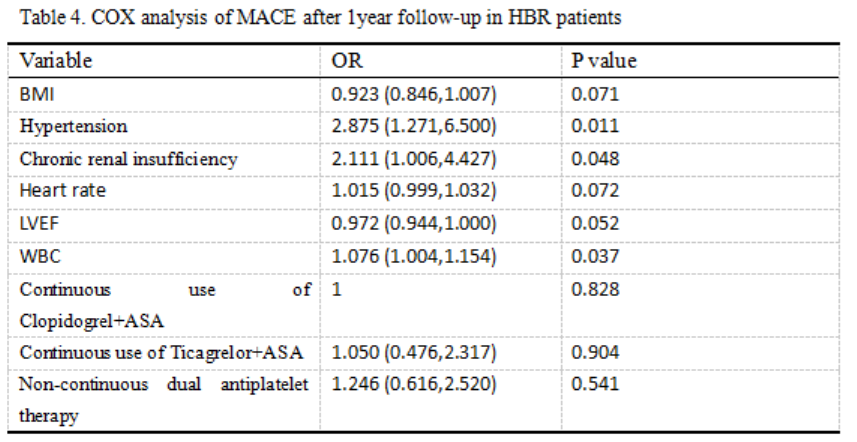
Compared with non-high bleeding risk (NBHR) patients, HBR patients were more frequently developed postdischarge bleeding(BARC type≧2)(6.8% VS 5.2%,95% confidence interval [CI]:0.895-1.255; P=0.000) and main adverse cardiovascular events (MACE) (a composite of all-cause death, myocardial infarction, ischemic stroke, or urgent coronary revascularization) (7.1% VS 2.2%, 95% confidence interval [CI]:2.259-3.574; P=0.000). BMI, Hypertension, chronic renal insufficiency, heart rate, LVEF and White Blood cell count (WBC) were the risk factors in HBR ACS patients who face MACE risk. The incidence of NACE (net adverse clinical events:PDB and MACE) in Clopidogrel DAPT group was significantly lower than that in Ticagrelor group in HBR ACS patients (11.6% VS 14.2%,OR=1.251, [CI]:(1.043,1.500) ;P=0.016).
Conclusion
In Chinese ACS patients with HBR, the incidence of PDB and MACE were both higher than non-HBR patients. Among HBR patients, 13.3% had NACE events within 1 year after PCI,and DAPT with ticagrelor increased the NACE events rates.


