Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-079
Clinical Characteristics and Outcomes in Patients With Severe Aortic Stenosis Combined With Small Left Ventricle Undergoing Transcatheter Aortic Valve Replacement
By Can Wang, Dejing Feng, Erli Zhang, Xiangming Hu, Yunqing Ye, Haiyan Xu, Yongjian Wu
Presenter
Can Wang
Authors
Can Wang1, Dejing Feng1, Erli Zhang1, Xiangming Hu1, Yunqing Ye1, Haiyan Xu1, Yongjian Wu1
Affiliation
Fuwai Hospital, China1
View Study Report
TCTAP A-079
Other Structural Interventions
Clinical Characteristics and Outcomes in Patients With Severe Aortic Stenosis Combined With Small Left Ventricle Undergoing Transcatheter Aortic Valve Replacement
Can Wang1, Dejing Feng1, Erli Zhang1, Xiangming Hu1, Yunqing Ye1, Haiyan Xu1, Yongjian Wu1
Fuwai Hospital, China1
Background
Background: Clinically, patients with severe aortic stenosis (AS) and a small left ventricle (LV) exhibit prognostic variability after transcatheter aortic valve replacement (TAVR). Limited by a single large-sample registry study, the understanding of this group's clinical profile and outcomes is incomplete. Our study aims to deepen the knowledge of their clinical characteristics, perioperative prognosis, and long-term outcomes.
Methods
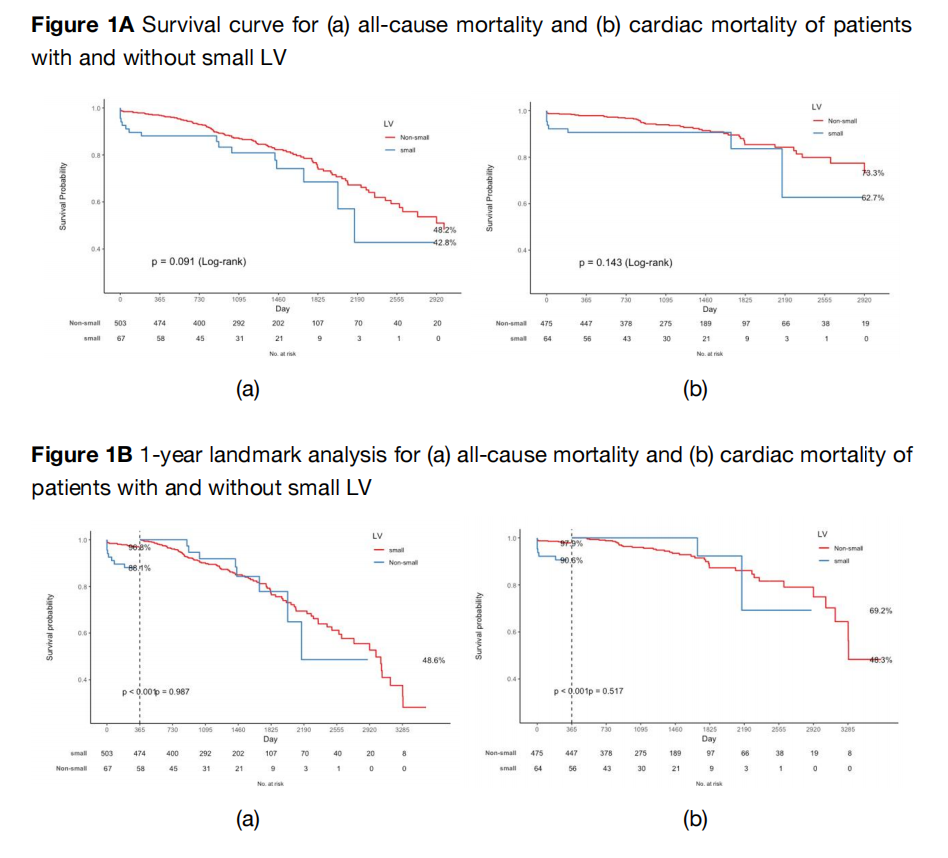
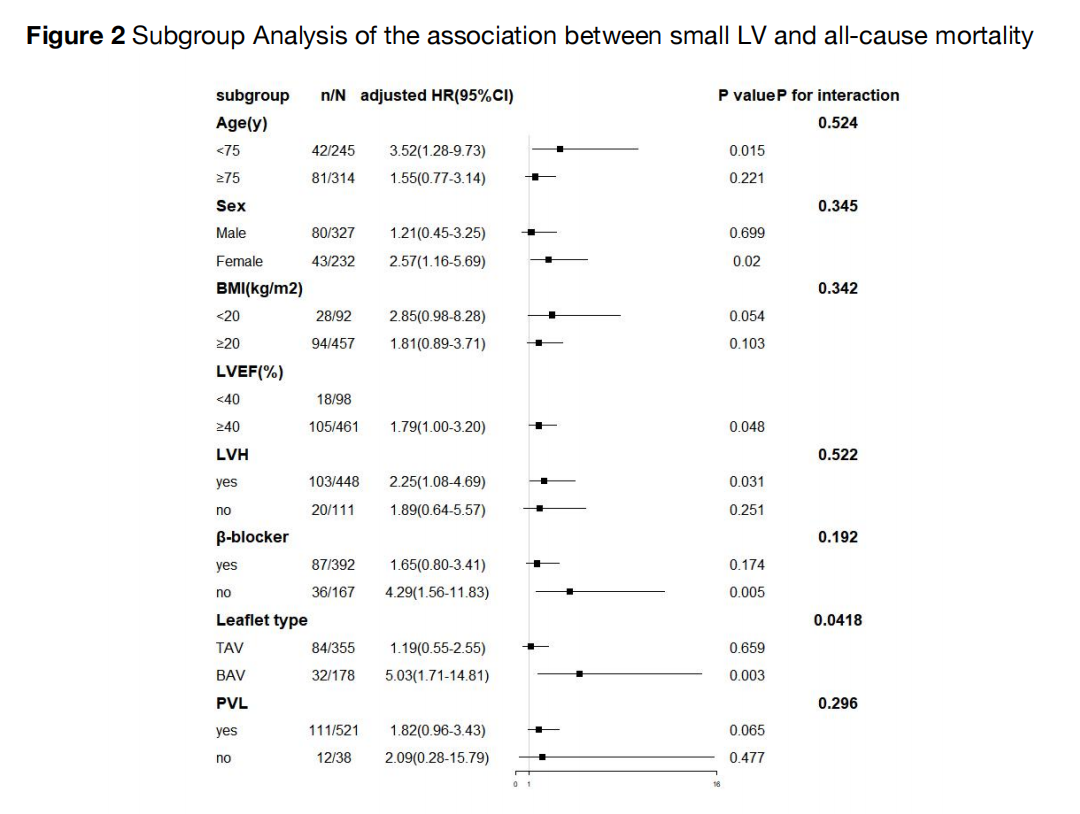
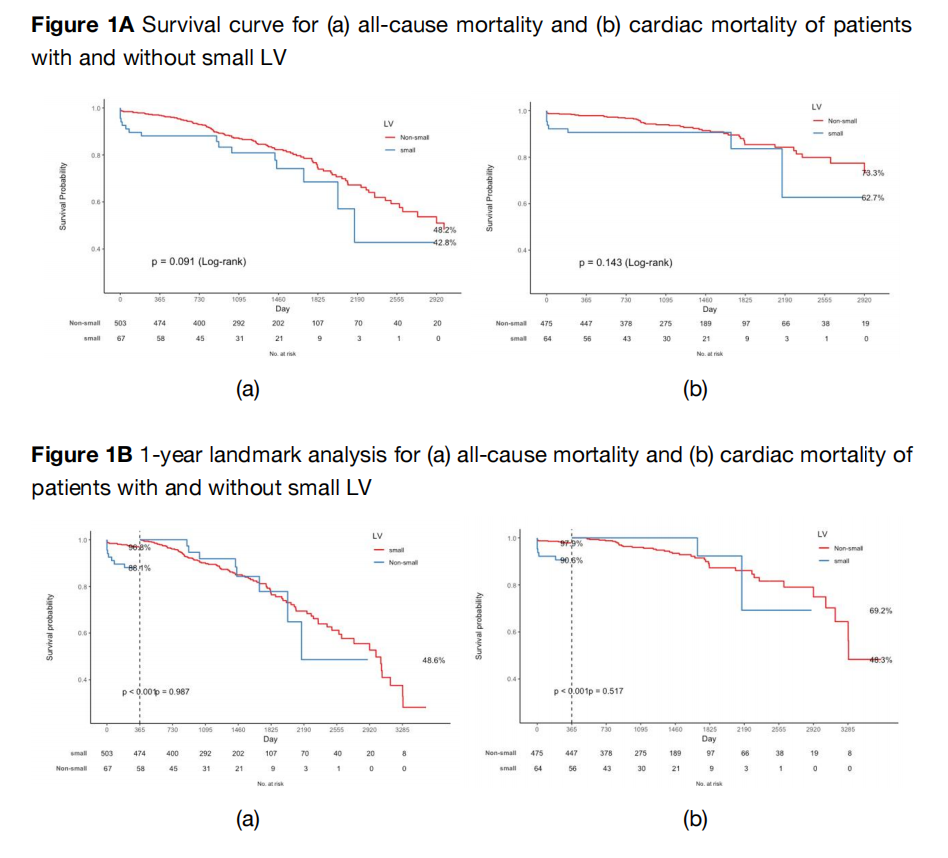
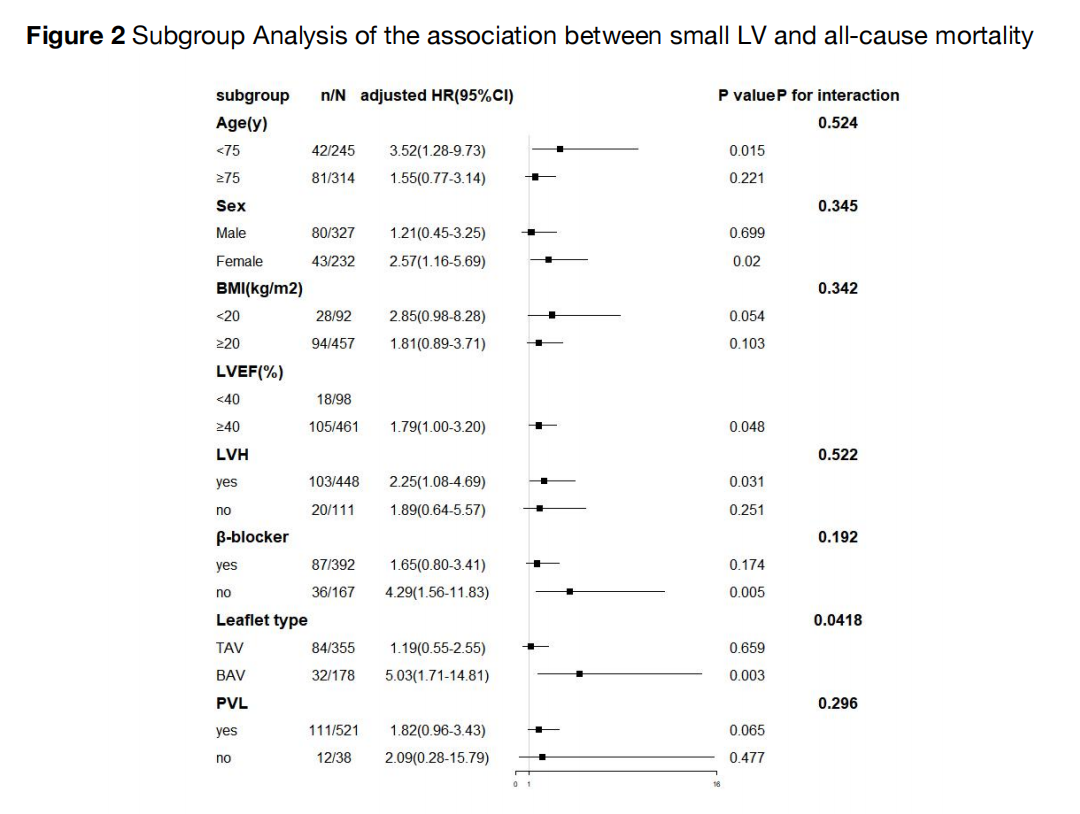
Methods: In this retrospective study, we included 586 severe AS patients who underwent TAVR at Fuwai Hospital from September 2012 to September 2022. Left ventricular end-diastolic diameter (LVEDD) less than 40.0 mm was defined as a small ventricle. Data was collected upon enrollment, at 1, 6, and 12 months post-TAVR, and annually thereafter. Outcomes of interest include perioperative results, long-term survival, and LV remodeling.
Results
Results: The small LV group (n=68) had significantly different baseline characteristics compared to the non-small LV group (n=518), with higher female proportion, lower smoking history, lower NT-proBNP levels, higher left ventricular ejection fraction, lower left ventricular mass index, and increased relative wall thickness. The small LV group showed higher in-hospital mortality (5.9% vs 1.0%, p<0.01), but similar long-term mortality rates. However, one-year mortality rates were notably higher in the small LV group (all-cause: 11.9% vs 3.2%, p=0.002; cardiac-specific: 9.4% vs 2.1%, p=0.005). Echocardiographic data indicated left ventricular reverse remodeling peaks at one month after TAVR.
Conclusion
Conclusions: Patients with small ventricles face higher risks within the first year after TAVR. Smaller left ventricular dimensions may predict poor outcomes, emphasizing the importance of LVEDD as a marker for clinical outcomes.


