Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-060
Association of Baseline Cumulative LDL-C Exposure With Hemorrhagic and Ischemic Events in ACS Patients Within One Year Post-Discharge
By Yani Yu, Xiaodan Tuo, Ying Wang, Dandan Li, Yundai Chen
Presenter
Yani Yu
Authors
Yani Yu1, Xiaodan Tuo1, Ying Wang1, Dandan Li1, Yundai Chen1
Affiliation
The Sixth Medical Center of Chinese PLA General Hospital, China1
View Study Report
TCTAP A-060
Pharmacotherapy (Coronary)
Association of Baseline Cumulative LDL-C Exposure With Hemorrhagic and Ischemic Events in ACS Patients Within One Year Post-Discharge
Yani Yu1, Xiaodan Tuo1, Ying Wang1, Dandan Li1, Yundai Chen1
The Sixth Medical Center of Chinese PLA General Hospital, China1
Background
This study aimed to investigate the association between baseline cumulative low-density lipoprotein cholesterol (LDL-C) exposure at admission and the occurrence of bleeding events, ischemic events, and a composite of both within one year after discharge in acute coronary syndrome (ACS) patients.
Methods
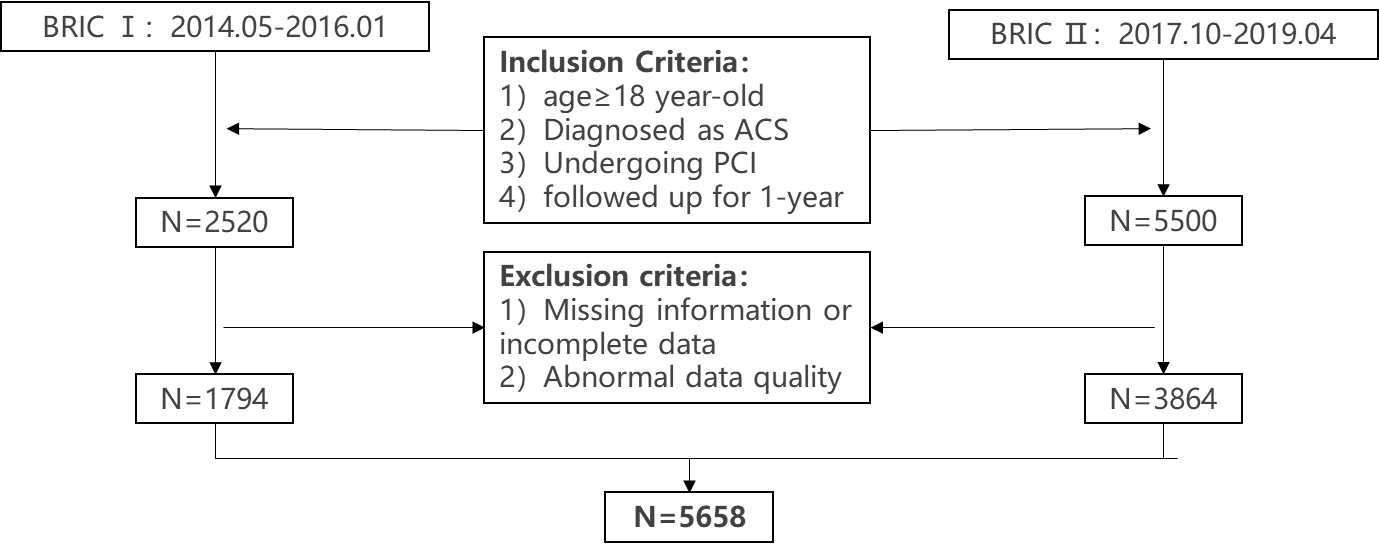
This study is a post-hoc analysis of a prospective cohort study (BRIC study), including ACS patients with percutaneous coronary intervention (PCI) and one-year follow-up from 30 Chinese hospitals. Baseline cumulative LDL-C exposure was calculated as the product of LDL-C concentration at admission and age. Outcome events included BARC type ≥2 bleeding event, major adverse cardiovascular event (MACE), as well as net adverse clinical event (NACE).
Results
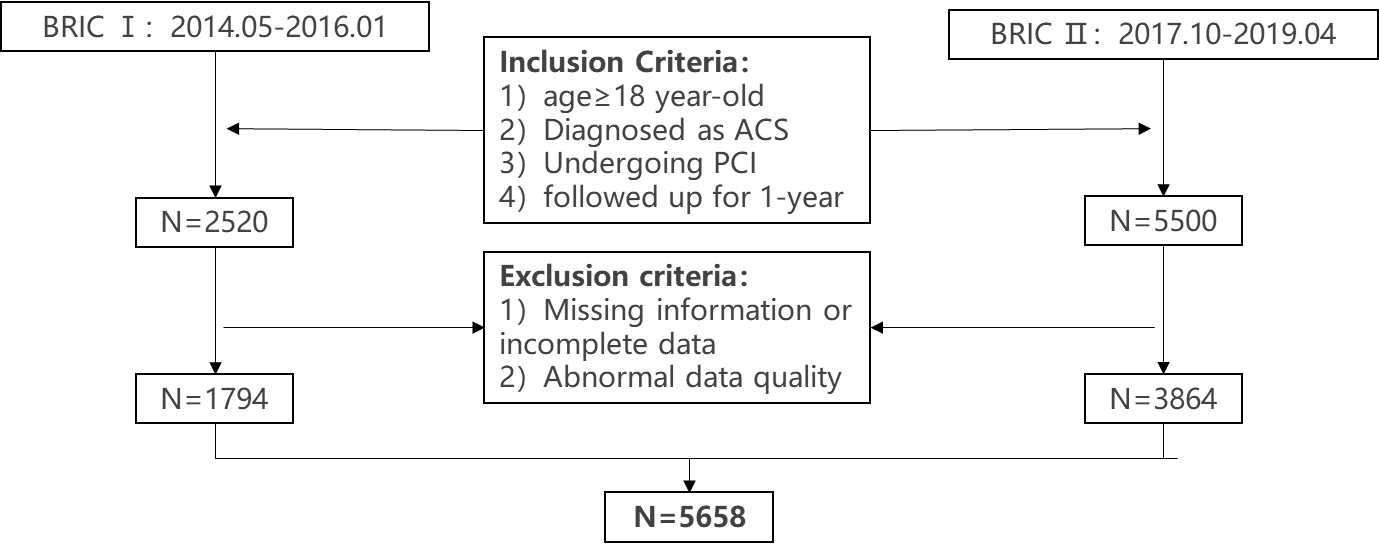
Of the 5658 patients, 309 suffered BARC ≥2 bleeding event, 156 suffered MACE, and 454 suffered NACE. Kaplan-Meier survival analysis revealed a positive correlation between baseline cumulative LDL-C exposure and the risk of MACE and NACE (P=0.002), but not bleeding (P=0.055). After adjusting for confounders, higher LDL-C exposure was associated with increased MACE and NACE risks (HR=2.369, 95% CI: 1.440-3.898, P<0.01; HR=1.389, 95% CI: 1.053-1.832, P=0.02), whereas the risk of BARC type ≥2 bleeding was non-significant (HR=1.160, 95% CI: 0.831-1.618, P=0.383). Restricted cubic spline analysis did not reveal a nonlinear relationship between LDL-C exposure and bleeding but confirmed a linear association with MACE and NACE.
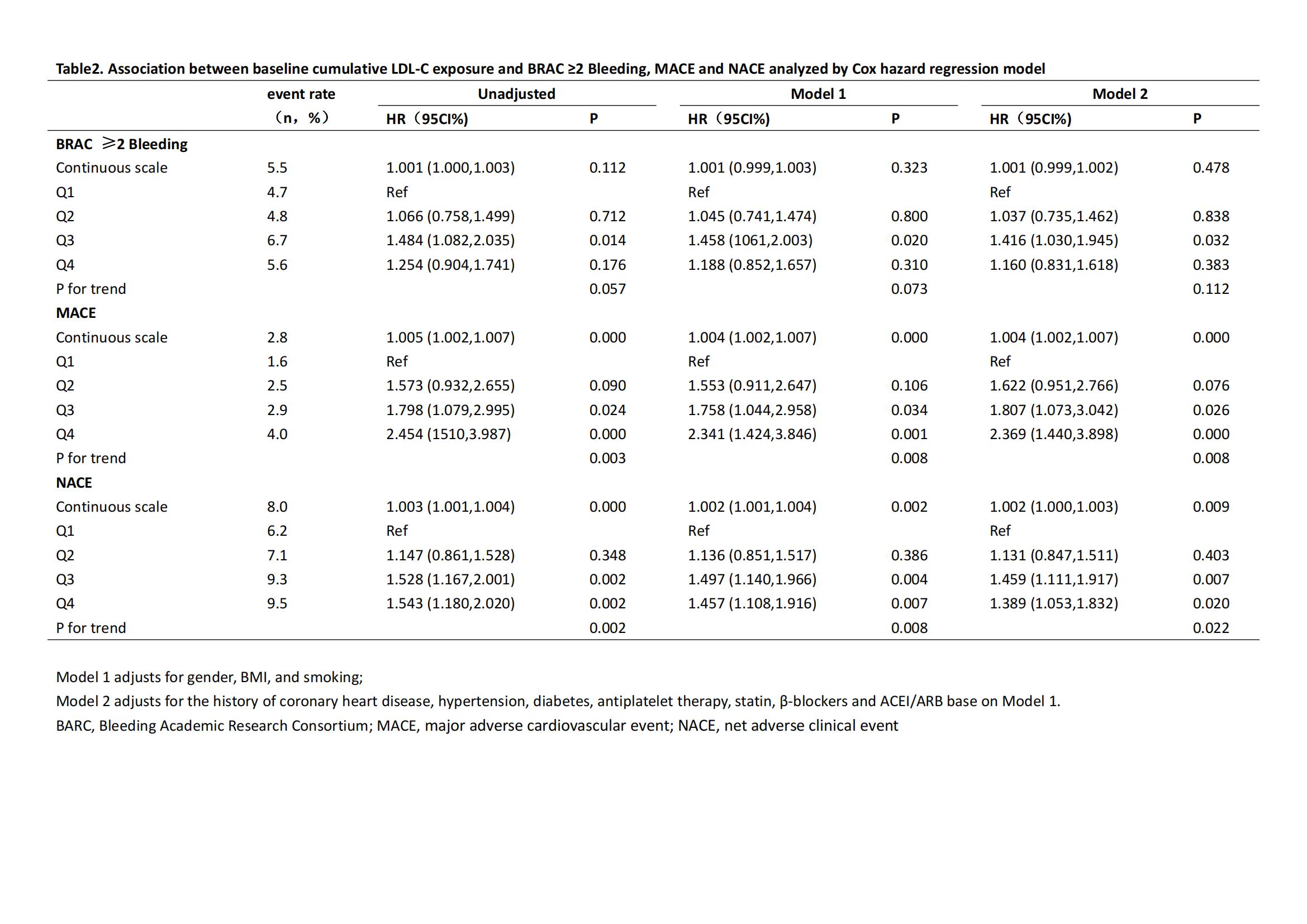
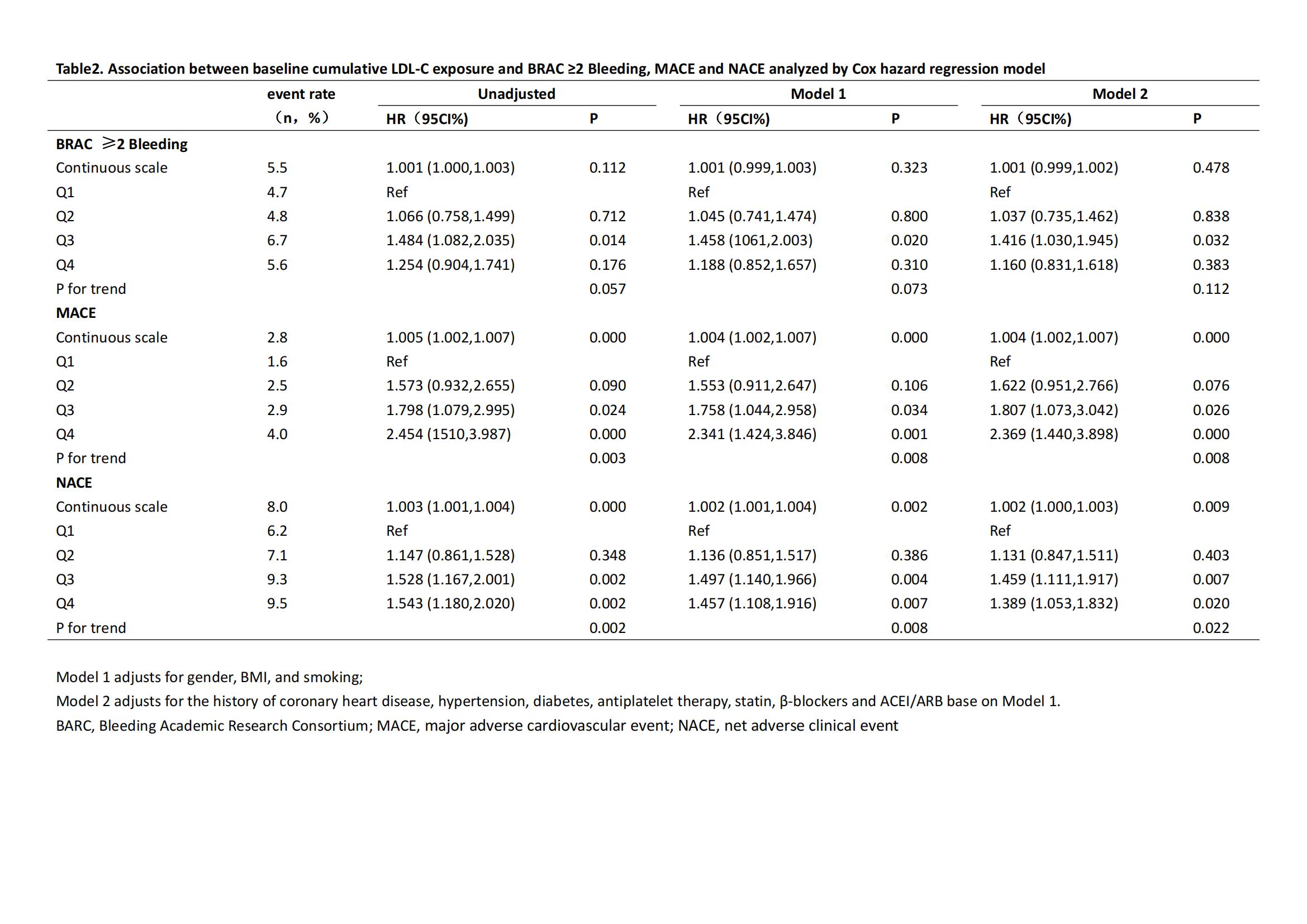
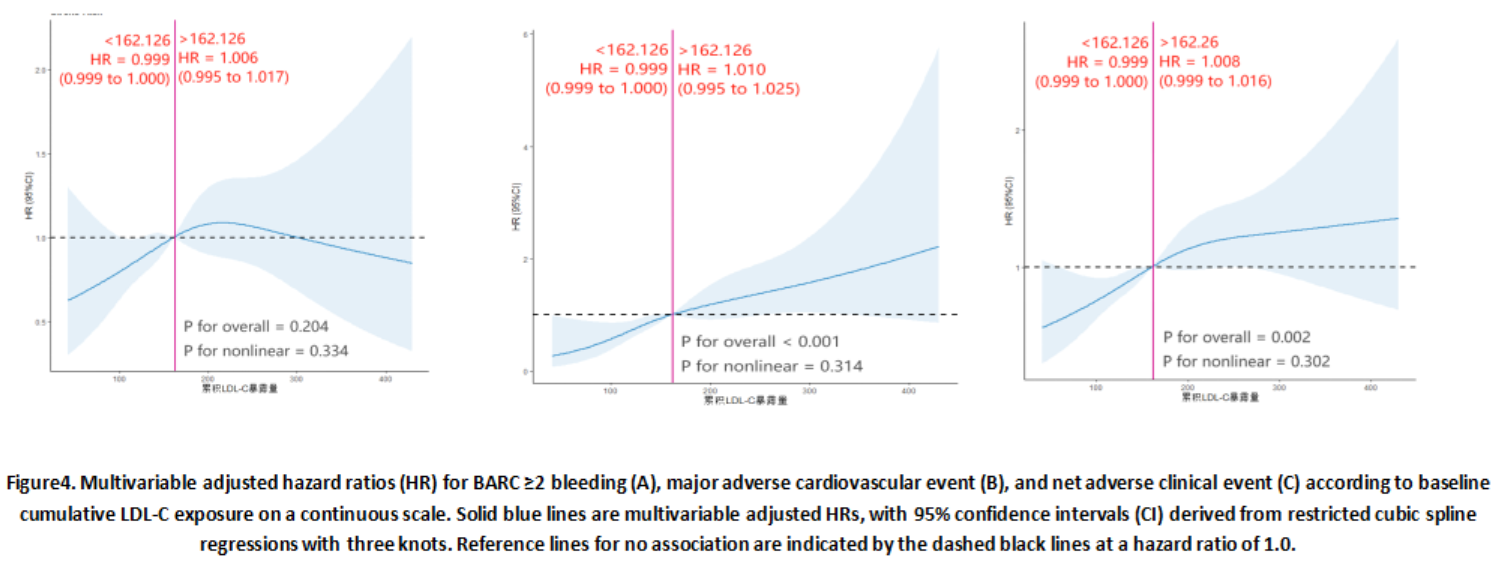
Conclusion
Baseline cumulative LDL-C exposure is associated with the risk of MACE and NACE within one-year post-discharge in ACS patients, with higher exposure indicating a higher risk, but no significant correlation with BARC type ≥2 bleeding.


